Introduction
With increasing rates of declining mental health in Australia, there is a commensurate rise in the need for appropriate support. E-health, defined as technology-based health services and information delivery at the intersection of medical informatics, public health and business1, has been proposed as one such support mechanism. It can be provided through a broad range of devices and strategies such as telehealth (eg video-conferencing or web resources), wearable devices, smartphones and shared electronic records2,3. While some consumers may prefer face-to-face service, e-health is becoming increasingly accepted as a supplement to care that may also encourage autonomous and proactive consumers4. It is purported that e-health is cost-effective, provides efficient, real-time automated monitoring and convenient 24-hour access5. With the introduction of the Australian Digital Health Agency and National Digital Health Strategy the Australian Government has prioritised e-health initiatives to improve service delivery and population health outcomes6.
However, despite increasing interest in e-health models in policy and practice settings and Australians becoming more digitally connected7, uptake of initiatives has been underwhelming8,9. For example, in the initial rollout phase, only 2.7% of Australians registered for a personally controlled electronic health record, which led to the decision to use an ‘opt out’ approach in the latest rollout6,10. Further, in an Australian study of residents in a rural community in New South Wales, only 20% suggested that they would consider using e-mental health in the future11. Poor uptake is related to misalignment of e-health initiatives with end-user requirements, such as access, ease of navigation, complexity, appropriateness, capacity, self-efficacy, attitudes toward the internet and computers, privacy and confidentiality concerns9,12,13.
Understanding internet use
A range of relevant factors have been proposed to explain internet use. First, issues that are extrinsic to the individual, which may be considered thematically as ‘equity’14, include adequacy of environmental conditions, geographic location, availability and reliability of the internet (access), possession of suitable hardware, an appropriate connection and suitably designed software15,16. There are also important personal variables, such as age and gender7. For example, males are more likely to engage with new technology, including for seeking mental health information, and do so earlier than females17. Younger people usually have had greater exposure through schooling and social interactions and are generally more motivated to actively use the internet in comparison to older generations18,19. Some older people may lack interest or see limited value in the internet20,21.
Other important determinants include marital status, with some evidence that people living alone are more likely to use e-health22. Income is positively related to internet use, with higher income presumably allowing access to appropriate equipment19. Employment produces similar results, as computer skills are a prerequisite for many occupations16,23. Conversely, lower education levels are associated with less, and less proficient, internet use8,18,24. In relation to e-health access specifically, education is a stronger predictor than income24. In terms of e-mental health services, higher usage is reported by females, those with higher educational attainment and those who are socioeconomically advantaged25.
A key intrinsic factor for internet use is motivation. For example, perceived usefulness and perceived ease of use are consistently strong predictors26,27. Technological self-efficacy and facilitating conditions are also valuable contributors8. A further fundamental motive for e-health use specifically is trust, which is influenced by past experiences with the internet, health systems and professionals, or concerns with surveillance28,29. One source suggested that while increasing numbers of consumers may be using the internet to search for health information, only 6% find sources they trust30. Subsequently, trust is a critical success factor for the National Digital Health Strategy6.
Rural mental health consumers: a case study in internet use
A review by the Australian Government has led to a plan to develop a mental health portal, aligning with the aims of the National Digital Health Strategy. The goal is to optimise innovative technologies in guiding consumers toward the most appropriate services including high quality apps and services6,31. A key population affected by such reforms is people living in rural areas. Rural Australians are more likely to face the additional challenges of socioeconomic disadvantage (lower employment and income), higher health care costs, greater travel demands and a scarcity of health infrastructure and professionals5,32-34. Consequently, if accepted, e-health initiatives have the potential to allow higher numbers of rural mental health consumers to receive support, across greater distances, at lower cost5,6. However, current evidence suggests that internet use among people with mental illness is relatively low and variable. Internationally, rates of between 55% and 80% have been cited for general use, with 69% noted for specific health use18.
Summary
Policymakers and service providers are acutely interested in leveraging internet use to facilitate positive health outcomes. However, it would appear that the first step remains a more fulsome appreciation of barriers to and enablers of internet use. Assessing these factors using quantitative methods allows for consideration of both the direct and indirect relationships at play that could help to target future decision-making. Such evidence may inform the efficient allocation of resources and the appropriate design of initiatives to produce innovative solutions. As these developments would appear to be particularly advantageous to rural mental health consumers, the goal of the current study was to assess the factors associated with internet use in general and for health purposes specifically.
Methods
Participants
Data were provided by 208 rural South Australians sourced from a pool of consumers who had recently accessed a rural local health network (LHN) mental health service (MHS). This is a government-funded service for people with serious and severe mental illness. Those who had been under a community treatment order (level 1–2), a detention and treatment order (level 1–3) or guardianship during this period were excluded. The sole criterion for inclusion in final analyses was that participants nominated themselves as internet users.
Procedure
Variables (described in Table 1) were sourced from both the LHN MHS clinical database and a questionnaire constructed. Potential participants were given a unique identifier by a LHN MHS employee, who then posted recruitment packages to those selected. This included an introduction to the study, information sheet, consent form and reply-paid envelope. The return of a signed consent form allowed the authors access to identifying information, with a questionnaire mailed to consenting participants. Follow-up reminders were then posted at appropriate intervals. As 200 is the commonly cited sample size requirement for structural equation modelling (SEM) to be appropriately tested35,36, recruitment continued until this goal was achieved. A larger sample size was beyond the scope of available resources.
Table 1: Measures of study variables 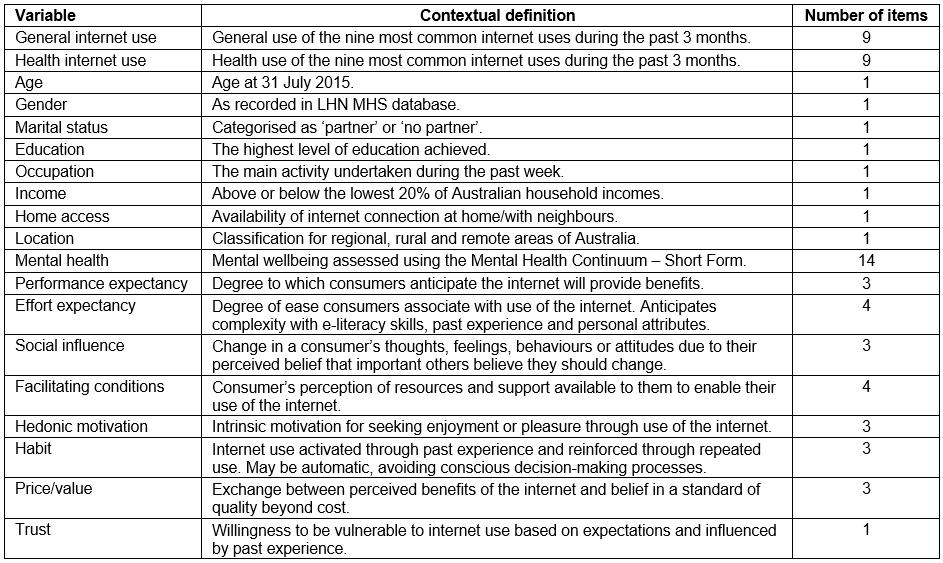
Variables
Internet use: Level of general internet use (range 0–45, α=0.83) was quantified using a six-point scale ranging from ‘never’ (0) to ‘several times a day’ (5) in response to the question ‘How often during the last three months have you used the internet for each purpose listed below?’. Nine common internet uses were then listed37: information seeking (eg Google), email, classic (eg for news, sports, travel plans), socialising (eg Facebook, Twitter, Instagram), shopping and banking (eg selling, buying, paying bills), accessing information/activities for school and work, entertainment (eg watch or download movies, TV programs, music), using an online telephone and creative (eg post a video, story or other creative work). The same information was then sought to determine ‘How often during the last three months have you used the internet to access something to do with either your physical or mental health?’ (health internet use, 0–45, α=0.85).
Sociodemographic variables: Participants were asked whether they had internet access in their residence (‘yes’ or ‘no’), and their age, gender, marital status (‘partner’ or ‘no partner’), education (‘secondary school or less’ or ‘additional education or training’), employment (‘any employment or student’ or ‘unemployed, disability pension, retired’) and household income (‘below $30,212’ or ‘above $30,212’, in line with Australian Bureau of Statistics data)38,39. Location was identified using the LHN MHS clinical management database. Categories (regional, population ≥50 000; rural, population 5000–50 000; rural, population <5000; remote) were informed by the Modified Monash Model40, which is commonly used to classify metropolitan, regional, rural and remote areas of Australia.
Mental health: The Mental Health Continuum-Short Form (MHC-SF) is a measure of general wellbeing41. Responses are recorded on a six-point scale from 0 (never) to 5 (every day) across 14 items comprising emotional (three items, range 0–15), social (five items, range 0–25) and psychological wellbeing (six items, range 0–30). In the present research, only the total score is reported (range 0–70, α=0.95).
Motives: Participants responded using five options (‘strongly disagree’ to ‘strongly agree’) to items from the United Theory of Acceptance and Use of Technology – Revised (UTAUT2)27, a motivational framework that has been successfully applied to internet use. Example items for each motive are ‘I find the internet useful in my daily life’ (performance expectancy, three items, range 3–15, α=0.85), ‘I find the internet easy to use’ (effort expectancy, four items, range 4–20, α=0.95), ‘People who are important to me think I should be using the internet’ (social influence, three items, range 3–15, α=0.92), ‘I have the knowledge necessary to use the internet’ (facilitating conditions, four items, range 4–20, α=0.80), ‘Using the internet is fun’ (hedonic motivation, three items, range 3–15, α=0.93), ‘Using the internet has become a habit for me’ (habit, three items, range 3–15, α=0.85), and ‘The internet is good value for money’ (price/value, three items, range 3–15, α=0.95).
Trust: The single item ‘I am able to find information I trust on the internet’ was used to measure trust on a five-point scale from ‘strongly disagree’ to ‘strongly agree’42.
Statistical analyses
Data were analysed using the Statistical Package for the Social Sciences (IBM; http://www.spss.com). Bivariate hypothesis tests comprised Pearson correlation coefficients, t-tests and one-way ANOVA. Multivariate analyses were conducted within an SEM framework using automated model order selection algorithms. SEM is a generic term for a suite of multivariate techniques, including confirmatory factor analysis, regression analysis, discriminant analysis, canonical correlation, latent variable analysis and path analysis, that take advantage of the covariances among the components of a proposed model43. The value of SEM over other multivariate techniques is the ability to consider more than one variable as an ‘outcome’ in a single analysis. A further advantage is the ability to provide a visual diagram to aid in the interpretation of the presented results.
In the present context, the relatively simple procedure of path analysis was used to examine the hypothesised associations between multiple ‘predictor’ variables of general internet use and internet use for health purposes, respectively, while general internet use is also purported to be a predictor of internet use for health. Trust and motivation were proposed as predictors of both forms of use, with trust hypothesised to precede motivation. Age and equity were proposed as exogenous variables, being potential predictors of all other components of the model.
The goal was to evaluate whether this model had theoretical sense, reasonable parsimony and an acceptable correspondence to the data44. A range of goodness-of-fit indices are reported as is the usual recommendation, with their associated thresholds for acceptable model fit considered ‘rules of thumb’36. Path coefficients are standardised. Non-significant paths evaluated for inclusion and demonstrated not to contribute to the model have been removed to improve interpretation, as have error terms for endogenous variables.
Ethics approval
Ethics approval for this research was granted by the South Australian Health Human Research Ethics Committee (14/SAH/180) and the Flinders University Social and Behavioural Research Ethics Committee (OH-00045).
Results
Tables 2 and 3 summarise all variables, highlighting those found to be related to internet use (for general and health purposes, respectively) in univariate analyses. Higher levels of general internet use were associated with being younger, having stronger motivation (all motives except social influence), having greater trust, a higher education level, being employed, having a higher household income, and having home access to the internet. For health internet use, the identified significant associations were generally more modest and included only being younger, having stronger motivation (all motives), and greater trust. Gender, marital status, mental health and location were associated with neither form of internet use.
Prior to SEM the large number of observed variables was reduced. Individual motives were correlated between 0.21 and 0.68, with model results likely to be both influenced by multi-collinearity and provide minimal discrimination between individual motives. Therefore, the seven motives were subjected to a principal components analysis with the first component saved as ‘motivation’ using the regression algorithm (mean=0, standard deviation (SD)=1). Positive scores denote levels of motivation above the sample mean. The seven categorical equity variables (home access, marital status, gender, education, occupation, income, location) were treated similarly (‘equity’: mean=0, SD=1), with higher scores denoting greater social advantage.
With respect to the resultant model (Fig1), final indices were suggestive of very satisfactory fit. The model χ2 was non-significant (χ2(6) = 8.50, p=0.204; χ2/degrees of freedom=1.42), and the normed fit index, comparative fit index and Tucker–Lewis index were all excellent at 0.99. The root-mean-square error of approximation was 0.039 (confidence interval=0.000–0.094). The model indicates no direct predictors of internet use for health beyond use of the internet for general purposes. General internet use itself, however, was strongly influenced by motivation, and age and equity to a lesser extent. Motivation was influenced by trust, age and equity, and trust was also influenced by age and equity. Therefore, while there were no significant direct effects, all model components provided significant indirect paths to health internet use.
Table 2: Summary of continuous study variables and their associations with internet use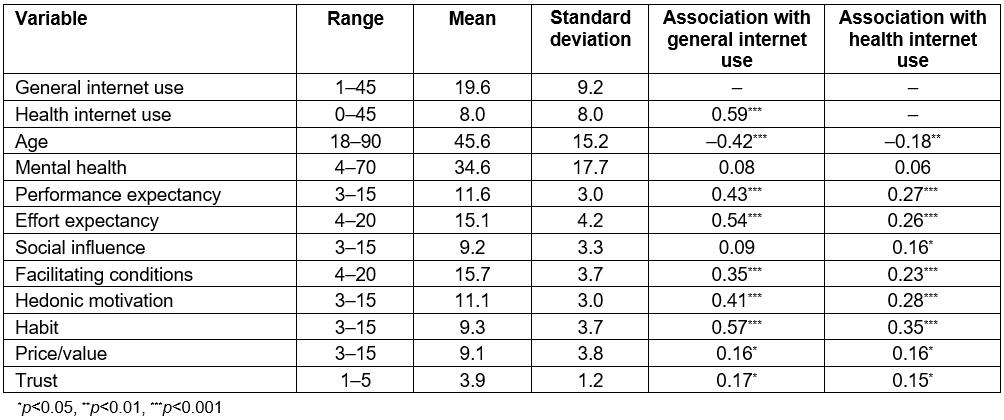
Table 3: Descriptive data for categorical study variables (measures of equity) and tests of difference with general and health-specific internet use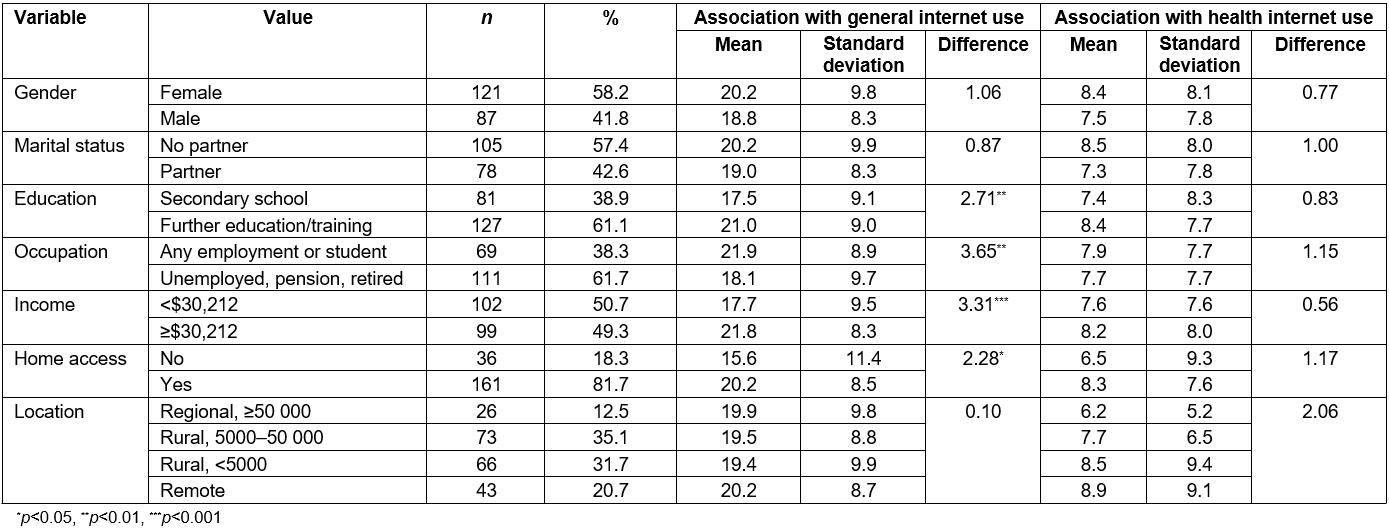
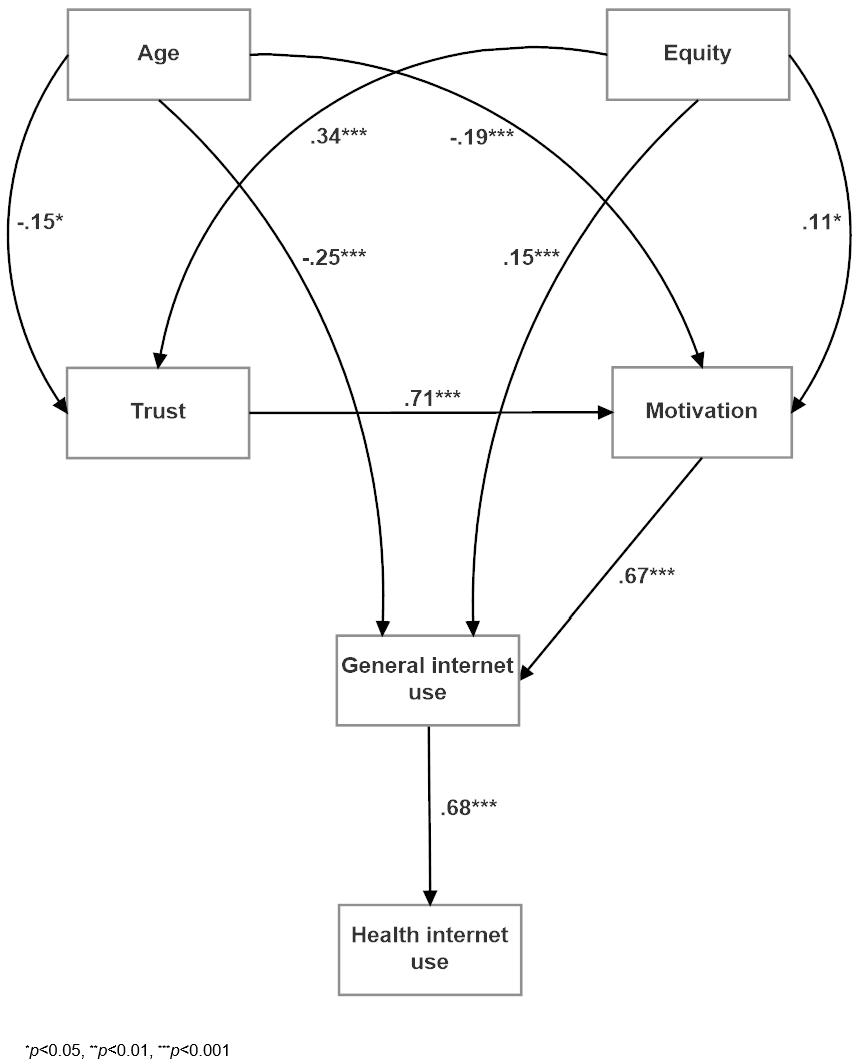 Figure 1: Structural equation model demonstrating the hypothesised paths leading to general and health-related internet use.
Figure 1: Structural equation model demonstrating the hypothesised paths leading to general and health-related internet use.
Discussion
Recent government initiatives have emphasised the future reliance on e-health initiatives to address resource gaps in the provision of mental health care31. However, existing programs have been challenged by poor uptake8,9. Walker noted that rural digital inclusion policies need to address the interactions that occur between ‘infrastructure, adoption and usage of ICT in rural areas’ (p. 263)45. This quantitative investigation sought to describe the barriers to and enablers of internet use generally, with the premise that before people will use the internet for health, they need to be prepared to use it for general purposes.
The unique contribution of this study is a move toward filling the gap between the e-health initiatives being introduced at a policy level, and at a micro-level the environmental context for individuals and their capacity and willingness to engage with these initiatives. In their study of online health-related activities, Chae concluded that how individuals make use of the internet will have implications for their health outcomes46. The present article progresses this notion as it allows an exploration of not only the factors affecting internet use, specific to a cohort of rural mental health consumers (a vulnerable, often under-explored population), but also an understanding of the direct and indirect relationships between these factors and health internet use. The participants in this study are a cohort for whom the context is complex; understanding this context through a psychosocial model such as that presented here offers benefits for informing the efficient allocation of resources and implementation of e-health initiatives for rural communities.
Within a rural mental health context, the proposed theoretical model provided support for the hypothesis that motives and equity influence general use of the internet, but only indirectly affect health use. Interestingly, intrinsic motivational factors were more strongly associated with internet use than more extrinsic, equity-related factors. Such findings suggest that to design successful e-health initiatives the initial focus must be on consumers’ individual capacity and willingness to use the internet generally.
In line with previous research, findings from this study suggested that general internet use was associated with younger age, higher education and current employment17-19,23. It is likely that such characteristics reflect increased opportunity to engage with the internet and subsequently stronger skills27. This familiarity may also contribute to the higher levels of motivation and greater trust in the internet recorded among the sample. Similarly, consistently high socioeconomic status and access have been linked with internet use, reinforcing the notion that higher household income often permits access, as people are more likely to be able to afford the equipment required to enable frequent use19,25.
Despite a strong association between general and health internet use, overall there were low levels of health use among the sample. Factors affecting likelihood to engage included younger age, greater trust and stronger motivation. Nevertheless, when considering the overall model, these elements had only indirect effects on the likelihood of using the internet for health purposes. This suggests that there may be other factors at play in predisposing to use the internet for health, such as health literacy, attitudes and self-efficacy12,13. Alternatively, the specific nature of the sample may have contributed, with previous studies noting low to moderate intention or actual use of e-health initiatives among cohorts in rural areas and those with mental illness11,18.
The model proposed in the present research offers preliminary insights into some of the factors that may influence rural mental health consumers’ use of the internet for both general and health purposes. However, given the cross-sectional nature of the study, the findings should be considered indicative rather than definitive. Future research should thus not only test this thesis with a larger sample but could advance this inquiry by comparing differences in motives and equity among both users and non-users of the internet within rural and metropolitan sites. Further, it is important to consider that South Australia has the poorest rates of digital inclusion (calculated based on access, affordability and digital ability) across Australia23, thus future studies may consider patterns of use within different parts of the country. With respect to equity, it must also be noted that due to the aggregate method employed, the specificity of individual equity variables was lost in the present study. For example, gender, which has previously been shown to be important7,17,25, was subsumed within the broader measure of equity, and this may have masked its importance. Against this, it must be recognised that in the initial univariate analyses gender was not related to either measure of internet use. Nevertheless, the reduced number of variables offered greater convenience in model construction, providing the opportunity to investigate the influence of constructs that had not previously been assessed simultaneously.
Interestingly, mental health played no significant direct role in predicting internet use. However, it must be acknowledged that given the self-selecting nature of recruitment, it is possible the sample was biased against those who were particularly unwell at the time of the survey, who may have been disinclined to participate. Further, in a recent review on mental health consumers’ use of smartphone apps, Torous and colleagues described how low motivation is a symptom of a number of mental illnesses, thus mental health may have had an indirect effect within the model9. Future studies may therefore look more specifically at mental health variables, including diagnoses and treatment, to assess their influence on use. Moreover, future research may strive to attain a more nuanced understanding of how trust influences acceptance and use of technology by developing new comprehensive measurement tools. Additional studies may also consider alternative variables likely to influence internet use for health, including micro-level factors such as health literacy and digital literacy, and macro-level factors such as the rollout of the National Broadband Network (which has been shown to improve access) and National Digital Health Strategy23,47.
Implications for practice and policy
Previous applications of the UTAUT and UTAUT2 cite evidence for motives as predictors of adoption of different technologies27, and the present research offered further support. When viewed holistically, motivation was a key driver of internet use. The measured motives, drawn from expectancy-value theories, reflect a range of perspectives that influenced behaviour. For internet users, habit was key, as were ease of use (effort expectancy), perceived benefit of use (performance expectancy) and perceived enjoyment (hedonic motivation). These predominantly intrinsic motives were more strongly linked with internet use than extrinsic elements such as facilitating conditions, social influence and price. In association with the finding that motives had a greater influence on internet use than equity measures, it seems that appealing to internal characteristics to initially trigger, guide and sustain internet use will be critical in introducing e-health initiatives.
For practitioners seeking to enact e-health models of care in rural and remote areas, understanding the factors that will affect their patients’ likelihood to engage is invaluable. Findings from this study will assist practitioners to identify consumers who are most likely to accept e-health as part of their care. Practitioners may consider their patients’ socioeconomic status, motivation and level of trust to ascertain their propensity for using the internet, before suggesting they enrol in e-health programs. Trust is affected by experience with the internet, health systems and health professionals28,29, thus practitioners must also acknowledge their role in encouraging e-health uptake. At a practice level, it may be possible to look at methods to improve general internet use before implementing e-health initiatives. Active consumer input into the design of initiatives, education and training sessions may be a useful strategy to promote improved literacy, provide information on the benefits of the internet and harness willingness to engage9,47.
It is understood that rural areas face challenges in terms of access to health care generally and mental health supports specifically5,32-34, and while e-health has been suggested as a remedy for this situation, there are environmental challenges that will affect the likelihood of success17. The finding that equity was associated with general internet use within the present sample reinforces the potential digital divide that has been alluded to in previous studies and the National Digital Health Strategy6,23. First-level digital divide relates to digital maturity and environmental factors such as infrastructure and physical access to software and hardware, while second-level digital inequity relates to human factors such as intellectual access and efficacy. This may result in digital exclusion of vulnerable groups16 – those who are most in need of support may be those least likely to have access to the technologies that will enable them to benefit from e-health initiatives47. Without addressing this inequity, e-health could be advantageous only to those with more resources and thus serve to disenfranchise both non-internet users and non-proficient users48.
Conclusion
At a policy level, the National Digital Health Strategy is currently being implemented. However, its effectiveness is likely to be challenged by digital inequity. Digital inclusion is strongly affected by equity-related variables such as income, education, employment and geography23. Consequently, consideration needs to be given to broader contextual factors before rolling out initiatives unlikely to be adequately utilised by the community. The internet presents an opportunity to improve health outcomes for those with the means, capacity and motivation to use available resources. A concerted effort should therefore be made to improve structural deficits, particularly in the areas of improving infrastructure and access, while research continues the search to identify factors relating specifically to use of the internet for health.
References
You might also be interested in:
2008 - Clinical placement and rurality of career commencement: a pilot study
