Introduction
Blindness and visual impairment are significant public health problems worldwide1-3. Through eye health system strengthening, strategies have been developed in the Pacific region to tackle the burden of blindness and visual impairment. One approach is to increase human resources in eye care and to supply medical and ophthalmic supplies4-6. However, few studies have examined the impact of eye care training programs7-9 on the state of eye health systems where mid-level eye care workers are remotely deployed, especially regarding the availability and use of medical technology.
This lack of data is not without significance. In low-resource countries, ophthalmologists are scarce and mainly practise in urban centres, which leaves remote areas with important deficits in eye care services5. For many years, efforts have been made to train and increase the number of mid-level eye care workers, to be deployed in the predominant rural areas. As this strategy has been applied throughout the Pacific region, there is a need to assess indicators of the current eye health system, such as medical products and technologies, one of the WHO building blocks of health systems10.
In 2006, the Fred Hollows Foundation New Zealand (FHFNZ) implemented a Postgraduate Diploma in Eye Care (PGDEC) for qualified nurses, developed with regionally relevant competencies and aligned with the eye care burden in Papua New Guinea (PNG) and Pacific Island countries and territories (PICT)11. Participants travel for 1 year from their places of employment, in order to train in two regional universities (Divine Word University in PNG and the Pacific Eye Institute at Fiji National University), which deliver training in ocular health assessment, refraction, operating theatre skills and public health8,12,13. By 2015, FHFNZ had supported over 150 trainees from more than 15 countries. Students are supported financially by FHFNZ through scholarships and standardised long-term ophthalmic equipment loans to complement existing equipment in the workplace, if any. Graduates thus have access to standardised equipment upon graduation. This mainly includes refraction equipment (visual acuity charts, retinoscope, lens rack, trial lens frame and set, Jackson cross-cylinder) and ocular health assessment equipment (ophthalmoscope, pen torch, visor loupe). However, over time, many factors (malfunction, theft, lack of spare parts) may affect the availability of certain items. Eye care workers are encouraged to signal repair needs to FHFNZ for repairs to be facilitated or to apply for ad hoc replacement equipment grants from FHFNZ.
In this context, the present study aims to describe the availability, use and comfort level with use of ophthalmic equipment and medications by mid-level eye care workers in PNG and PICT, as indicators of the state of eye care in the Pacific.
Methods
FHFNZ is the principal organisation supporting local development of human resources in eye care in PNG and PICT. Program monitoring data were used to depict the state of eye care in the Pacific. To assess the region’s workers’ professional integration, FHFNZ developed a post-training, in-country workforce support system, previously described14. After eye care workers graduate, FHFNZ periodically sends one of ten Pacific-based local consultants for workforce support (WFS) visits, offering mentoring and support, while gathering monitoring and evaluation data on professional integration. WFS are performed every 2 to 3 years, depending on resources available. WFS data are also used to define content for local continuous professional development (CPD).
WFS visits include a questionnaire for workers to document the availability and comfort level for use of ophthalmic equipment as well as availability of and comfort prescribing ophthalmic medications. Availability of equipment and medications are documented with yes/no items. Frequency and comfort of use are graded using five-point Likert scales (1 = rarely/not comfortable, 5 = frequently/very comfortable). WFS visits considered for this study occurred from January 2013 to December 2016, in eight countries (Fiji, Papua New Guinea, Vanuatu, Samoa, Solomon Islands, Kiribati, Tonga and Tokelau).
FHFNZ’s WFS data were transferred to a spreadsheet database and depersonalised before transmission to the investigators. Analyses were conducted using JASP v0.10, (University of Amsterdam; https://jasp-stats.org) to extract descriptive statistics. Median Likert scores and interquartile ranges (IQR) were calculated for all items with skewed distribution.
Ethics approval
Ethics approval was granted by the University of Montreal ethics committee for health research (CERES, certificate 16-099-CERES-D). The graduates all signed an agreement with FHFNZ to partake in the WFS program, which includes a clause to partake in eye health events and share information with FHFNZ. Furthermore, before organizing a WFS visit, FHFNZ obtains the participant’s employer’s permission.
Results
A total of 66 eye care workers had WFS visits and surveys completed during the study period (2013–2016). Ten respondents were visited more than once during the study period; only the most recent data were retained. Demographic, professional and geographic characteristics of respondents are presented in Table 1. Given the regional training model of FHFNZ, results for individual PICT were combined (n=31) and are compared to those of PNG (n=35). Wherever mentioned, access to equipment pertains to functioning items.
Table 1: Demographic, professional and geographic characteristics of respondent Pacific mid-level eye care workers (n=66)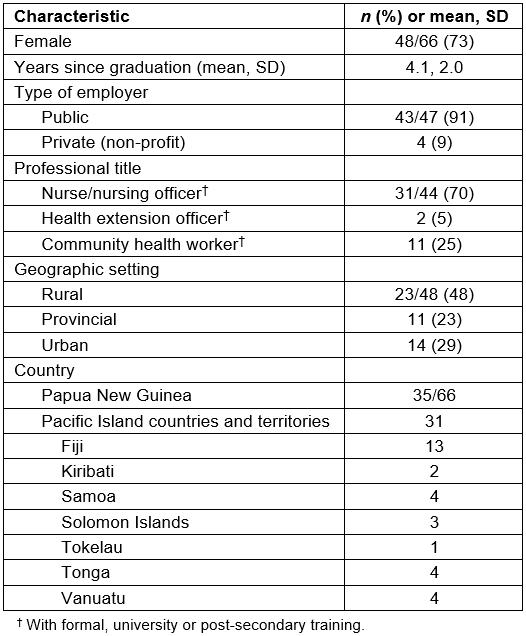
Access to and levels of use and comfort for refraction
Table 2 presents access, levels of use and levels of comfort for refraction and ocular health assessment. Access to equipment for spherical refraction (detecting myopia, hyperopia and astigmatism) is 97–100% across both regions, for visual acuity charts, retinoscopes and trial lens sets. The range of median Likert scores for frequency of this equipment is 4.0–5.0 (out of 5). Score range for frequency and comfort of trial lens sets and visual acuity charts is 4.0–5.0. Median score for frequency of retinoscopy is 1.5 (IQR 2.8) in PICT and 4.0 (IQR 3.0) in PNG. Score for frequency of use and Jackson cross-cylinders (specific to the measurement of astigmatism) in PICT is 2.0 (IQR 4.0) and 5.0 (2.0) in PNG.
Access to and levels of use and comfort for ocular health
To assess anterior segment health, all graduates have access to either a slit lamp or pen torch (Table 2). For the slit lamp, median Likert scores for frequency and comfort of have a range of 4.0–5.0. Some 80% of PICT and 43% of PNG respondents reported having access to tonometers. For tonometry, median Likert score for comfort of use was 2.0 (IQR 3.0) in both regions, and score for frequency of use of tonometry was 1.0 in both regions.
Table 2: Equipment for refraction and ocular health assessment: access, levels of use and comfort for mid-level eye care workers in the Pacific (n=66)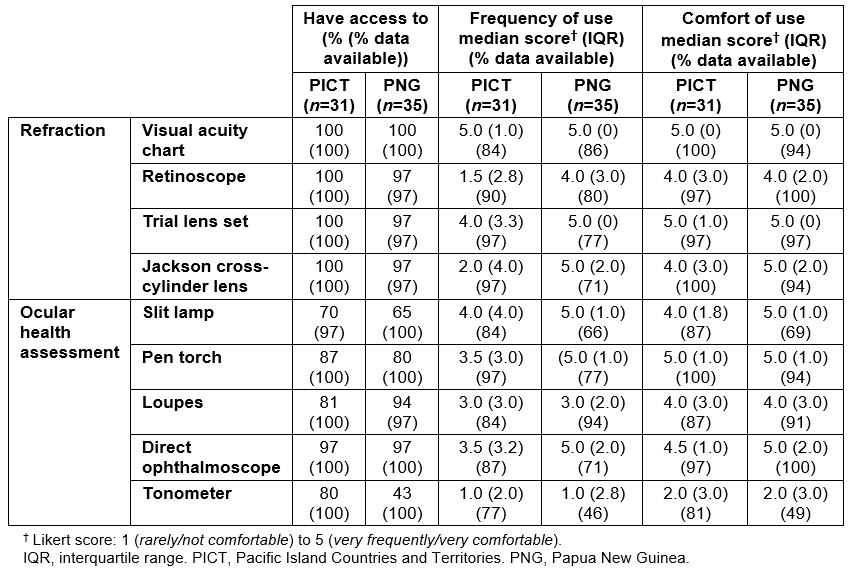
Access to and levels of use and comfort for medications
Regarding diagnostic agents, respondents reported access to at least one type of anaesthetic eye drop in both regions (PICT 73%, PNG 74%) as well as to sodium fluorescein (PICT 76%, PNG 77%). Range for access to mydriatic drops was 58–69% and for access to cycloplegics was 65–77% (Table 3).
For antibiotics, access to chloramphenicol is reported at 100% for PICT and 97% for PNG. Ciprofloxacin is reported to be available to all respondents in PNG and to 54% in PICT. Median Likert scores for comfort using chloramphenicol were 5.0 (IQR 1.0) in PICT and 5.0 (IQR 0) in PNG. Scores for reported comfort with use of ciprofloxacin were 3.0 (IQR 4.0) in PICT and 5.0 (IQR 1.0) in PNG.
In PICT, 63% of respondents reported having access to prednisolone acetate, while in PNG 63% did. Dexamethasone was reported to be accessible to about half of respondents in both regions (PICT 58%, PNG 51%). Reported comfort with using prednisolone acetate scored 2.0 (IQR 2.0) in PICT and 3.0 (IQR 2.0) in PNG. PICT score for comfort using dexamethasone was 2.5 (IQR 2.0), while in PNG this score was 4.0 (2.0).
Access to econazole was reported by 66% of PNG respondents and 42% of PICT respondents. Access to acyclovir, a topical antiviral drop, was reported by 54% of PICT respondents and 63% in PNG. Median scores for comfort using econazole were 2.0 (IQR 2.0) in PICT and 5.0 (2.0) in PNG.
Range of reported access to glaucoma medications across both regions was 40–58%.
Table 3: Levels of access and comfort of use for ophthalmic medications for mid-level eye care workers in the Pacific (n=66)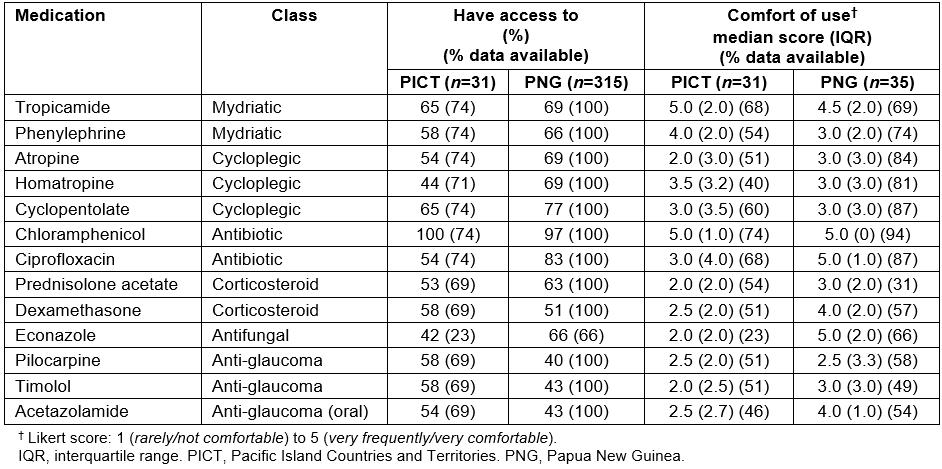
Discussion
Knowing the availability, use and comfort with ophthalmic equipment and medication by mid-level eye care workers allows for a better understanding of the state of the health system.
Current strengths for Pacific mid-level eye care workers
First, resources required for detecting and treating uncorrected spherical refraction error are present. Overall, eye care workers in PNG and PICT have excellent access to refraction equipment, with visual acuity charts, retinoscopes and trial lens sets nearly ubiquitous in the region. Considering the epidemiological importance of uncorrected refractive error and visual impairment3, this is certainly beneficial. The frequency of use of refraction equipment is higher in PNG than in PICT. This correlates with the 39% of PICT respondents who reported performing refractions less than 20% of the time they dedicated to eye care (against 6% in PNG, data not shown). This is likely explained by the fact that, despite their training, eye nurses in Fiji (20% of respondents) are not yet able to prescribe spectacles independently, contrary to other PICT states and PNG. Nurses in Fijian hospitals have a workload that typically includes a high proportion of operating theatre duties, more so than in other countries surveyed (additional workforce support data, not shown).
Comfort levels for refraction techniques show no regional differences; encouragingly, almost all respondents reported being very comfortable using a trial lens set, the main technique used for subjective refraction in this region. Fewer reported being very comfortable with retinoscopy and Jackson cross-cylinder refraction for astigmatism, possibly due to the complexity of the techniques and their steeper learning curves15. Additionally, in the authors’ experience, the prevalence of strong astigmatic refractive errors in the region was relatively low, reducing opportunities to practice and maintain the Jackson cross-cylinder skills acquired during the PGDEC training. Furthermore, while some WFS data were collected on the availability of spectacles and practices regarding optical dispensing, insufficient uniformity of the data prevented their inclusion in this study.
Second, given the importance of enabling mid-level eye care workers to detect cataracts and manage low-morbidity anterior segment conditions, access to equipment for assessing ocular health seems adequate in the region. As head-mounted loupes and pen torches are part of the graduates’ equipment package and replacement torches are inexpensive and easily sourced locally, almost all respondents possessed one or the other or both (Table 2). These are positive findings, as eye care workers need to access, and be comfortable with, these low-cost alternatives to slit lamps. Throughout the region, access to slit lamps was impressive at 67%. Considering that most graduates start working in clinics without slit lamps and that these are not included in the FHFNZ equipment package, efforts were made by FHFNZ to source second-hand and refurbished slit lamps from optometrists and optical suppliers from New Zealand and Australia. Although donated equipment is often prone to certain difficulties (unfit to local needs, inadequate support for installation or repairs, etc.)16,17, donated slit lamps, within a framework such as the WFS program, can help initially equip eye care workers for diagnosis and treatment of eye conditions and suitable peri-surgical care for cataracts. However, efforts to transfer to local health authorities the procurement and maintenance of ophthalmic equipment would be a long-term goal to aim for in a health systems strengthening approach.
Furthermore, an encouraging majority of respondents reported access to topical diagnostic agents (over 70% for anaesthetics, mydriatics and fluorescein), which are important for diagnosing anterior segment conditions. Notably, large-spectrum antibiotics such as chloramphenicol, helpful for mild conditions or prophylaxis, were accessible to almost all respondents.
Current challenges for Pacific mid-level eye care workers
Overall, access to and confident use of some medications, especially those needed to treat higher morbidity conditions (microbial or fungal keratitis, uveitis, trauma) constitutes a challenge. Notably, these study data yielded some positive results that, given the difficulties related to the procurement of medications in developing countries, exceeded the authors’ expectations. However, there were higher numbers of incomplete data for certain medications. Since these may represent unavailable items (rather than an absence of data collection), this may overestimate the reported accessibility of some agents. As in any low-resource regions, improvements in the procurement of medications in PNG and in PICT are elaborate and long-term endeavours18,19. They must aim to improve the complex in-country systems of pharmaceutical purchasing, management and distribution, which, unlike the case of ophthalmic equipment procurement, lie beyond the scope of a WFS program. Access to more potent antibiotics such as fluoroquinolones was not as widespread in PICT (54%) compared to PNG (83%). Considering the need to adequately treat potentially blinding conditions, this is an area for improvement in national essential medicines lists. Topical corticosteroids seem fairly accessible to eye care workers (50–70% have either prednisolone acetate or dexamethasone), but graduates report low confidence in their clinical use. This may be explained by some PICT jurisdictions not allowing nurses to prescribe steroids and by the fact that graduates who practise in jurisdictions where steroid use is allowed are encouraged to first consult with those in ophthalmology.
Another area highlighted as needing improvement is the identification and management of glaucoma. Tonometers are fairly accessible in the region, but comfort levels using them were reported as low. This was to be expected: currently, in the PGDEC, tonometry is a complementary competency only taught to the students most proficient in slit lamp techniques. Unsurprisingly, anti-glaucoma agents were infrequently used. Glaucoma is not a strong area of focus in the PGDEC curriculum and there is a dearth of recent data on the epidemiology of glaucoma in the region20. Should new data indicate an important prevalence of glaucoma, improving diagnosis and treatment of glaucoma would become a necessary but complex endeavour. It would necessitate to not only improving drug availability and comfort of use, but also refining techniques such as tonometry and ophthalmoscopy, as well as investing in regional centres equipped with perimetry and nerve fibre layer imaging technology.
Potential improvement through continued professional development
Continued support of graduates is a way to improve some of the shortcomings in technical skills and confidence levels through continued professional development (CPD) workshops and site visits. Through its WFS program, FHFNZ has an established record of this14, despite the continued challenges such as the financial and human resources required and the complex logistics of dealing with a widespread eye care workforce.
The data presented in this study highlighted some specific areas that could be addressed in CPD. Despite limited access to custom-made spectacles to manage astigmatic cases, Jackson cross-cylinder (astigmatic) refraction represents a skill that could be improved though workshops. Also, given that tonometry is key in quality diagnosis and treatment of glaucoma and anterior segment disease, tonometry technique and equipment procurement could be addressed. Finally, if competent steroid use by mid-level eye care workers becomes a higher priority in this context, CPD should also include training on how to control risk of inadequate diagnosis and treatment of steroid responders.
Study limitations
Limitations to this study include that data collection was not intended to sample eye care workers in a representative way, but gathered for monitoring and evaluation purposes. While the WFS program’s policy is to visit every eye care worker within 2 years after graduation and every 3 years thereafter, limitations in staff and finances restricted the number of WFS to 66 during the study period, out of a total of 155 graduates (41%). However, the distribution of these WFS data likely represents a reasonable cross-section of eye care workers, covering eight out of twelve countries in the Pacific region (excluding Australia and New Zealand), in clinical installations of various sizes. No other major factor in selecting sites for WFS visits (time since graduation, class of graduation, years of experience in eye care, etc.) were identified that could differentiate graduates who were or were not visited during the study period. The data are prone to inter-observer variability, although efforts were made to standardise the WFS procedures between the WFS consultants when collecting questionnaire data14. Lastly, as many responses were self-reported, the likelihood of a response bias by social desirability cannot be excluded.
Conclusion
These data give an impression of access to and use of eye care equipment and medications in the Pacific, as indicators of the regional eye health systems. Overall, trained mid-level eye care workers who have benefited from FHFNZ training and workforce support programs have good access and comfort with equipment for ocular health and spherical refraction assessments. Comfort using equipment for astigmatic refraction and tonometry are areas for CPD.
Access to ophthalmic medications appears generally acceptable in the region for low-morbidity anterior segment conditions, although additional confirmatory research is warranted and efforts to support local health authorities to improve procurement and distribution of medication should be pursued.
Author declaration
BS is a paid employee for Fred Hollows Foundation New Zealand. MGP, BT, GN and JB are past consultants for Fred Hollows Foundation New Zealand.
References
You might also be interested in:
2016 - Health promotion and empowerment in Henganofi District, Papua New Guinea