Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer and the third leading cause of cancer death for both men and women in the USA1. The prevention and early detection of CRC through screening has led to a large reduction in CRC incidence and mortality1. The US Preventive Services Task Force recommends screening average-risk adults aged 50–75 years for CRC using fecal occult blood testing (FOBT) every year, sigmoidoscopy every 5 years, or colonoscopy every 10 years2. However, over 30% of adults aged 50–75 years have not been screened for CRC according to national guidelines3. In particular, rural residents have been found to be less likely to receive timely CRC screening according to these guidelines than their urban counterparts4-6. Identifying barriers to increase CRC screening, especially for rural residents, should be a research priority. This article aims to review recent studies to identify barriers for CRC screening in rural populations so that appropriate interventions can be designed to improve CRC screening.
Most studies on CRC screening have focused on urban populations,, and the factors related to CRC screening have been found at multiple levels. Individual-level factors include demographic characteristics, socioeconomic status, personal or family health risks, and indicators of access to medical care7,8. Provider-level factors include primary care provider’s gender, medical training, workload, and practice history9. Clinic-level practices related to CRC screening include a protocol to reach patients due for CRC screening, patient or provider reminder systems, and provider performance feedback on CRC screening10-12. Recent studies also indicate that contextual factors such as area-level socioeconomic conditions, poverty, medical resources, and insurance coverage are also related to an individual’s CRC screening behavior13-16. An increasing number of studies focus on examining factors related to CRC screening in rural areas, where the patients may have more access barriers and limited medical resources. Of these rural studies, some examine perceived CRC screening barriers of the rural populations, others study rural clinics or providers from rural sites, and others conduct rural–urban comparisons for barriers to CRC screening specific to rural populations17-20. To inform effective policies or interventions that cater to the special characteristics of rural residents, it is essential to understand the barriers to CRC screening that are specific to rural populations. However, there has been limited effort in systematically reviewing the literature on barriers or facilitators to CRC screening for rural residents.
This systematic review will help distill information from the vast literature on CRC screening barriers and identify the most important barriers specific to rural areas. The review results will also inform and facilitate the design of targeted interventions for improving CRC screening rates among rural residents in the USA and guide future research.
Methods
Databases used, search strategies, and selection criteria
The literature search was started with Medline (via PubMed) using a combination of the keywords 'barriers' , 'rural', and 'colorectal cancer screening', 'colonoscopy', 'FOBT' or 'sigmoidoscopy'. A similar search was replicated using CINAHL, Embase, and Scopus databases, to retrieve articles not available in MEDLINE. The literature search was conducted in December 2017 on the literature published in the past 20 years (1998–2017) (Fig1). Complementing the database search, a manual search was conducted through journals, internet resources, and bibliographies of retrieved articles. Only empirical studies that examined the factors related to CRC screening or perceived barriers for a rural population in the USA were included. Studies excluded from this review were review studies, studies without empirical data analysis, intervention studies to promote CRC screening, studies outside of the USA, and studies focusing on cancer patients or cancer survivors. A total of 81 unduplicated titles were obtained using the listed keywords. Two additional articles were added through manual references search. Two authors independently reviewed the abstracts or the full-text articles of each of the 83 articles, discussed and came to an agreement about whether each article met the inclusion criteria. Out of these 83 articles, a total of 27 articles published from 2002 to 2017 were included in the systematic literature review. The Preferred Reporting Items for Systematic Reviews and Meta Analyses framework were followed when reviewing the articles included in this study21.
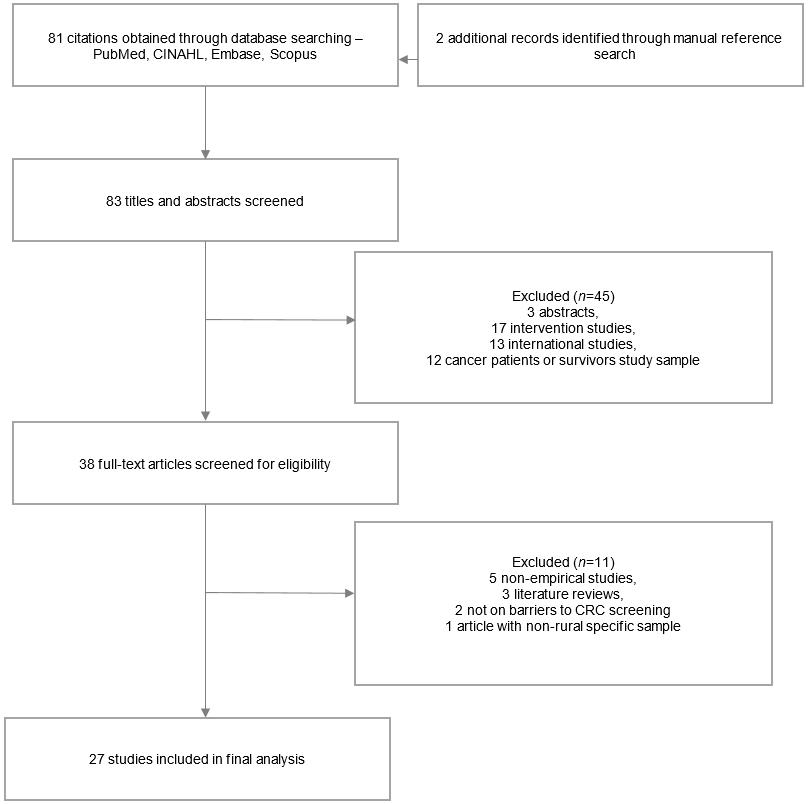 Figure 1: Flowchart of process for identification of literature relating to colorectal cancer screening in rural populations.
Figure 1: Flowchart of process for identification of literature relating to colorectal cancer screening in rural populations.
Analysis
The articles were categorized into three groups based on study methodology: studies using focus groups or in-depth interviews with rural patients or providers on perceived barriers for CRC screening, studies surveying patients or providers to assess perceived barriers and/or factors associated with CRC screening in rural areas, and studies examining factors associated with CRC screening behaviors using electronic medical record or survey data in rural areas. The factors identified in quantitative studies that are negatively associated with CRC screening behaviors were considered manifested barriers to CRC screening.
The systematic review examined perceived barriers and manifested barriers separately when summarizing the findings. For studies reporting perceived barriers, two authors recoded the barriers identified to ensure consistent interpretation of the barriers reported and generated a full list of all barriers identified in reviewed articles. The authors reviewed the identified barriers and counted the total number of studies that identified a specific barrier and compared it to the total number of studies that examined this barrier. For qualitative studies, it was assumed all possible barriers were included in the study analysis as participants were not restricted in their perception of CRC screening barriers. For quantitative studies using surveys with a list of barriers for participants to choose from, barriers not included in the list were considered as not examined in the study. For studies that focused on examining a particular factor and did not report other barriers identified in their study, only the identified factor was reported and counted as examined in the study. Factors negatively associated with CRC screening in either a bivariate analysis or a multivariate regression analysis were considered as manifested barriers. Factors that were statistically associated with CRC screening status after controlling for other covariates in a multivariate analysis were marked in a summary table.
Results
Table 1 summarizes all 27 articles that investigate the barriers to CRC screening among rural populations. Of the 27 articles, 10 reported only perceived barriers: five using focus groups20,22-25, three using in-depth interviews26-28, and two using survey methods17,19. Eight articles reported both perceived barriers and manifested barriers: six using surveys18,29-33 and two using surveys and focus groups34,35. Nine articles reported only manifested barriers: seven using surveys36-42 and two using electronic medical records43,44. Out of these articles, 14 studies examined rural populations in general17,18,22-24,26,29-31,34,37,41-43 and 13 studies focused on specific demographic groups in rural areas, such as women, minority populations, and patients with multiple diseases19,20,25,27,28,32,33,35,36,38-40,44. While most of these articles studied barriers or factors related to CRC screening in general, five studies discussed perceived barriers specific to FOBT as compared to endoscopies17,19,25,30,34.
Table 1: Summary of studies examining barriers to colorectal cancer screening in rural populations
Summary of identified barriers
As shown in Table 1, perceived barriers by rural residents included individual-level structural barriers, barriers related to screening procedures, and individual-level perception/knowledge barriers, and barriers at the provider level. Structural barriers for rural residents included high cost of screening procedures18,20,22-26,28-34, or lack of insurance coverage19,20,22-24,26,28,34, and lack of time18-20,26,29,31,32,34. Barriers related to screening procedures included embarrassment or discomfort17-20,22-29,31,32,34, fear of the test18,24,26,28,29,31, fear of finding cancer17-20,22,24,25,31-34, and fear of burdening family20,24. Additional barriers identified at the individual level included lack of knowledge on screening test options and guidelines17,20,22-26,28,30,34, lack of perceived need when there is no symptom19,23,25,26,28,30,31,34, and misperception that CRC is a male disease and CRC screening is more important for men22,25,26,28,35. Provider-level barriers included lack of provider recommendation17,19,20,22,23,25,29-31,33-35, distrust of providers or health care system20,23-26, inadequate supply of specialists (sometimes even primary care physicians19,20,23,24,28, and lack of reminder system19,25,28. In particular, there was some discussion on rural-specific attitudes and issues including lack of prevention attitude23-25,28-30, lack of privacy23,26,28, and distance/transportation to screening facilities20,23,24,26,28,29,32. Rural residents from several studies reported that they did not see a doctor regularly and would go to a doctor only when they were sick23-25,28,30. Rural residents also reported lack of privacy or confidentiality as a barrier of CRC screening and the fact that they know the medical staff exacerbated the embarrassment in several studies23,26,28.
High cost of screening and other financial barriers
The high cost of the CRC screening procedure was one of the most frequently identified barriers in this review. Of the 14 studies that examined high cost, all found it to be a barrier to CRC screening to some extent18,20,22-26,28-34. A study found that rural residents who were not up to date on CRC screening were more likely to agree with the statement that CRC screening cost is high than those who were up to date with CRC screening (p<0.001)31.The high cost of the procedure was cited as a barrier to CRC screening implementation by both patients and physicians29. Focus groups with providers also revealed that they were sometimes reluctant to recommend colonoscopy to patients because the out-of-pocket costs were too prohibitive23. High cost was consistently reported as a barrier by patients, providers, and key players in social networks in rural areas26. Focus group discussions with low-income rural residents in North Carolina also revealed that the high cost of the tests and follow-up care was one of the major barriers to CRC screening24.
When discussing financial barriers, lack of insurance coverage was often specified as the cause or a contributing factor of financial barriers. Eight out of 10 studies specified lack of health insurance as a barrier19,20,22-24,26,28,34. A considerable percentage (59%) of physicians in rural central Pennsylvania reported economic issues as a barrier and specified that under-insurance or uninsurance status contributed to the problem28. Not only lack of insurance but also the lack of insurance coverage on preventive tests by many insurance plans was a barrier to CRC screening28. Rural patients felt that their providers would not recommend CRC screening tests if they believed that the patient’s insurance will not cover it23. Rural patients also expressed their concern that providers would not recommend screening because of lack of financial incentive23.
Embarrassment and other barriers related to screening procedures
Embarrassment or discomfort related to CRC screening test was identified as a barrier in all 15 articles that included this factor in their study17-20,22-29,31,32,34. The percentage of respondents agreeing to CRC screening is embarrassing was significantly different between respondents who were current and those who were not current with CRC screening in a sample of rural respondents in Georgia (p=0.033)31. It emerged as a barrier for both rural men and women in one study24. For men, it was a sense of violation and, for women, embarrassment. In rural areas, the embarrassment caused by the procedure was worsened by the likelihood that the patient might know the medical staff conducting the procedure26. This was found to be especially relevant for rural women who were embarrassed about who else is in the room for colonoscopy28.
Discomfort related to the screening procedure and fear of the screening test were also frequently discussed and reported in these studies. The rural populations considered preparation for the test an uncomfortable process and worried about the pain associated with the test. Rural patients hoped that a less invasive test would soon become available23,25. Many studies reported about patients’ fear of the screening procedure as barriers for CRC screening24,26,28-31. Participants reported that they were afraid of possible bleeding or tearing of the colon31.
Other reasons for not undergoing screening were patients’ worry about finding out that they had CRC (11 out of 14 studies)17-20,22,24,25,31-34. The severity of CRC was perceived to change the life of the patient24 and many rural residents viewed cancer as a death sentence23. In one study, participants reported that, once symptomatic, they would start writing their last will25. This fatalistic attitude of patients was found to significantly reduce the likelihood of undergoing CRC screening42.
Risk perception and other barriers related to knowledge about colorectal cancer screening
Barriers related to lack of knowledge about CRC screening (10 out of 11 studies)17,20,22-26,28,30,34 and lack of perceived need (8 out of 12 studies) 19,23,25,26,28,30,31,34 came up frequently in the literature. Some rural residents felt that CRC screening was unnecessary unless they exhibited harmful symptoms30,31, which pointed towards a general lack of knowledge about CRC and the screening guidelines. A study found that patients thought there was no good cure to cancer and were unclear about the need for CRC screening, had concerns about effectiveness of treatment, and found the instructions on the screening test to be unclear25. Rural patients also reported the lack of conclusiveness associated with the screening test in identifying cancer to be a barrier23. A study reported that rural residents were less likely to receive education about the FOBT test as compared to urban residents17.
Lack of physician recommendation and other barriers related to providers
A total of 12 out of 15 studies reported the lack of physician’s recommendation to be a barrier to CRC screening17,19,20,22,23,25,29-31,33-35. Two additional studies reported that physician’s recommendation was a facilitator to CRC screening24,26. In a study of Federal Qualified Health Centers in northern Louisiana, rural participants were found to be less likely than urban participants to have ever received physician recommendation17. Rural patients also reported that CRC screening was not as commonly recommended by physicians as other tests such as mammogram, pap smear, and cholesterol check-ups, and was only recommended if the patient had a family history or was symptomatic23.
Other physician-related barriers included not having a regular doctor24, not seeing a doctor regularly30, and the lack of specialists to conduct the screening procedure19,20,23,28. In a study of patients from rural clinics in Nebraska, patients were found less likely to be up to date on CRC screening if they lived in a county with no gastroenterologist, and patients were more likely to be up to date if they had a primary care provider who was aware of clinic CRC screening protocols or who manually checked patient CRC screening status during the patient visit43. Although it may not be related to physicians directly, some studies reported a lack of trust in the medical establishment25 and avoidance of engaging with the healthcare system26 as barriers to CRC screening.
Manifested barriers
Manifested barriers examined in the quantitative studies focused on individual characteristics and socioeconomic factors. The most frequently reported factors associated with being up-to-date on CRC screening in rural areas included older age (11 out of 11 studies)18,29-32,34,36,37,39,42,43, insurance coverage (six out of seven studies)31,32,34,36,39,42,43, family history of CRC (four out of five studies)30,31,34,37, perceived risk of having CRC (five out of five studies)18,30,31,34,37, and physician recommendation (five out of five studies)18,29,31,34,35. Not having health insurance was consistently found as a barrier to CRC screening in six out of the seven studies that examined the relationship31,32,34,36,39,43. The study that did not find a significant association between insurance and CRC screening compared Medicare to other types of insurance coverage42. Physician recommendation, family history of CRC, and perceived CRC risk were all found to be positively correlated with CRC screening status. Other factors frequently found to be associated with CRC screening included marital status (four out of five studies)29-31,36,42 and race/ethnicity (five out of eight studies)29-32,37,39,41,43. Having a usual source of care (three out of six studies)18,31,35,36,39,42, gender (2 out of 10 studies)18,29-32,34,35,37,42,43, income (one out of four studies)30,34,39,42, and education (four out of nine studies)29-32,34,36,37,39,42 were relatively frequently examined and the results were not consistent.
Barriers specific to fecal occult blood testing
In contrast to endoscopies, FOBT is non-invasive, less expensive, and less sensitive, thus barriers related to FOBT may be different. Several articles explored barriers specific to FOBT and shed light on the differences in barriers among test modalities17,19,25,30,34. Similar to endoscopy tests, lack of information/knowledge25,30,34 and lack of physician recommendation17,25,30 were perceived as main barriers to have FOBT. Rural residents did not know that FOBT was recommended every year17,30,34, believed that instructions and rationale for FOBT need to be more explicit25, and indicated that their doctors did not tell them to have FOBT17,25,30. In addition, rural residents had doubts on the effectiveness of FOBT and perceived it as an ‘outdated test’ that was not as accurate or as thorough as colonoscopy25,34. Some physicians also indicated their preference for colonoscopy as compared to FOBT and considered FOBT ‘a substandard screening tool’19,28. Few rural residents reported barriers to completing an FOBT or had concerns over the test procedures17. However, only a slightly higher percentage of rural residents had concerns of pain/discomfort (16% v 11%) and financial concerns (21% v 18%) for colonoscopies than for FOBT30.
Rural-specific barriers
Five studies examined barriers to CRC screening for both rural and urban residents and compared the rural–urban differences17-20,22. While many barriers were common in both rural and urban areas20,22, rural residents were more likely to report embarrassment and discomfort, fear of finding cancer, lack of physician recommendation, lack of knowledge, and lower level of recognition on the benefits of CRC screening17,19,20. Hughes and colleagues’ study also confirmed that rural residents were more likely to report fear of the screening test and high cost of screening as barriers18. Lack of nearby clinic or screening facilities or specialists in rural areas were rural-specific barriers reported in several studies, as well as feelings of lack of privacy as a result of knowing the medical staff, and lack of prevention attitude resulting from the rural culture20,23,24,26.
Barriers identified among specific demographic groups
Gender-specific barriers were found, such as the belief that CRC affects mainly men28,39. Barriers related to race/ethnicity groups were also discussed in several studies. Poor quality of patient-provider communication was identified to be a major barrier to CRC screening for African Americans35. Besides other common barriers, lack of clinic staff who can speak Spanish was reported to be a barrier for Spanish rural populations20,32. Providers of the Indian Health Services revealed a lack of local capacities and providers as healthcare system-level barriers to CRC screening in remote and rural areas19. For patients who had multiple morbidities, the competing demands (both physical and financial) from the other conditions relegated cancer screening to lower priority27. Patients going through chronic opioid therapy for chronic non-cancer pain had significantly lower likelihood of receiving CRC screening44. Among religious groups, Amish adults were found to have a significantly lower CRC screening rate as compared to non-Amish adults in Ohio Appalachia38. Immigrants were also found to be less likely to receive CRC screening in rural areas40.
Discussion
The systematic review suggested that financial barriers, embarrassment/discomfort of undergoing the screening procedure, lack of knowledge thus lack of perceived need, and the lack of a physician’s recommendation were most commonly perceived barriers to CRC screening in rural populations. The association of these perceived barriers with CRC screening behavior was confirmed in a number of quantitative studies using bivariate or multivariate analysis. Lack of physician recommendation and its negative association with CRC screening status were supported in several quantitative studies18,29,31,34,35. The relevance of insurance coverage was also documented in a number of quantitative studies whereby it was revealed that those who did not have insurance coverage were less likely to be up to date on CRC screening31,32,34,36,39,43. In addition, increased risk as measured by family history of CRC or high perceived risk of CRC were also found to be positively related to CRC screening status and vice versa30,31,34. One study examined the association of embarrassment with CRC screening status and found that rural residents who felt the test was embarrassing were less likely to adhere to screening guidelines18. Efforts to improve CRC screening in rural populations need to first address these four most frequently identified barriers.
The findings from this literature review suggest that future interventions targeting rural populations focus on the individual-level barriers, by alleviating the structural barriers and finding ways to reduce screening test costs or increasing insurance coverage. Most of the studies included in this review took place before the enactment of the Affordable Care Act, thus the results may not fully capture the impacts of full insurance coverage of preventive CRC screening tests. However, several recent studies still indicate that patients and providers may not clearly understand the insurance coverage on screening tests and that some insurance companies may treat a screening test as diagnosis test and not cover the full cost43,45. Additional efforts in increasing insurance coverage and promoting information related to the increased insurance coverage on these tests would prove helpful for rural residents. Exploration of ways to promote alternative tests that are not cost prohibitive such as FOBT and promoting the use of such tests will also be needed46.
Findings across studies suggest that lack of knowledge on CRC and screening guidelines and lack of perceived need for an asymptotic person were major barriers in rural areas. Primary care providers have inconsistent understanding of the screening guidelines regarding the available tests and the starting age for average-risk patients19. Some providers consider colonoscopy as the most effective CRC screening test and prefer colonoscopy to other types of test19,28. Patients also have doubts on the efficacy of non-endoscopic tests and the benefits these tests can provide. Patients’ misconception that the tests are for people with symptoms and the belief that there is no cure even if CRC is detected early reduces the motivation for patients to initiate CRC screening25. Following the Health Behavior Model, efforts need to be made to educate rural residents to improve their knowledge on CRC and CRC screening, and change their attitudes, before they can actually change their behavior in seeking CRC screening47. Evidence-based strategies to educate patients and physicians to share information on all types of CRC screening test options, efficacies, and CRC treatment options and results would prove to be effective ways in addressing this barrier.
The importance of provider recommendation for adherence to CRC screening guidelines cannot be over-emphasized. Interestingly, physicians/providers surveyed often reported that they always or often recommend CRC screening to their patients. However, patients reported that their providers were less likely to recommend CRC screening compared to other screening tests34. Other provider-level factors (protocol, reminder system, provider assessment, and feedback) were not examined thoroughly in these studies, although these factors were found to be related to CRC screening status in general48-50. Rural residents and providers did report fragmentation of the healthcare system and distrust of healthcare providers as barriers. Patients reported that limited reimbursement for the CRC screening for the providers led to insufficient discussion with patients and inadequate physician referral for having a CRC screening test. Multi-level interventions that target system level barriers such as reimbursement policy as well as physician level barriers to improve the design and use of reminder systems may be most effective in promoting physician–patient communication and the physician recommendation of CRC screening.
Barriers identified in this review may be more pertinent to endoscopy tests as most patients think of colonoscopy when referring to a CRC screening test. While some identified barriers such as the lack of knowledge, lack of physician recommendation, and fear of the test results are applicable to both endoscopy tests and FOBT, some additional barriers are specific to different test modalities. Specifically, financial concerns and embarrassment/discomfort as a result of the invasive test procedure are barriers mainly related to the endoscopies. For FOBT, confusion about the test effectiveness by both rural residents and some physicians seems to be a major barrier. The findings from one study indicate that rural residents have similar concerns (financial concerns and concerns over test procedure) for colonoscopy and FOBT30. This finding suggests that rural residents may not understand all the risks and benefits related to different CRC screening methods. This calls for public health education in rural areas so rural providers and residents are equipped with accurate information to weigh the risks and benefits of different screening methods and find the most effective strategies to improve CRC screening in rural areas.
The systematic review results also suggest efforts taken to address rural-specific barriers such as lack of prevention attitude, lack of privacy, lack of medical facilities/specialist, long distance, and travel time to get screening done. Culturally competent materials will prove helpful for rural residents and underserved populations such as women or minority populations. The barriers at the community or area level are not sufficiently examined in the rural literature, which calls for additional studies to examine multi-level barriers to get a complete picture of factors contributing to low rates of CRC screening in rural areas.
The findings from this literature review are subject to the following limitations. First, studies used various definitions of rural populations, including patients from rural clinics, from rural counties, or rural Appalachian communities. Although the crude measures of rurality still provided valuable information, a more refined and accurate definition of rurality would be helpful in order to understand the rural-specific CRC screening barriers. Second, this review included both qualitative and quantitative studies on perceived barriers and manifested barriers. The manifested barriers revealed by studies investigating factors associated with CRC screening were in line with the perceived barriers identified in qualitative studies. However, the number of quantitative studies on the barriers specific to rural populations were very small (n=17) and many examined CRC screening barriers using simple bivariate comparisons. Those studies that conducted both bivariate and multivariate regression analysis seemed to suggest some factors that were statistically significant in the bivariate analysis but lost significance after adjusting for other factors. Last, this review was limited to published, peer-reviewed, English-language articles in the specified databases and results from studies not indexed in these databases may have been under-represented.
Conclusions
These limitations withstanding, the systematic review results suggested that the major barriers identified for the rural populations are not essentially different from those identified for the urban populations. Many individual-level characteristics were associated with CRC screening in rural areas, and the identified factors were in line with those found for urban adults in general. However, a few rural-specific barriers were identified including privacy and confidentiality issue, lack of prevention attitude, and structural barriers related to availability of specialists and distance to screening facilities. These factors need to be considered when identifying effective strategies to promote CRC screening with rural populations. Additional research on rural–urban differences in CRC screening barriers is needed to further delineate the extent to which the identified barriers, such as insurance and distance to a medical facility, are differentially associated with CRC screening in rural and urban areas. It will be helpful to carry out studies distinguishing barriers specific to FOBT as compared to endoscopies. The literature review findings suggest strategies providing public health education, reducing costs, and increasing access to specialists may be most effective in rural areas to promote CRC screening. An evaluation of these strategies and their impact on CRC screening can help inform policy interventions in rural areas.
References
You might also be interested in:
2015 - Determinants of an urban origin student choosing rural practice: a scoping review
2012 - Psychogeriatric care: building rural community capacity


