Introduction
Telehealth allows individuals to receive health care remotely via video-teleconference equipment1. In the past decade, the use of telehealth has been rapidly growing for medical consultations and other clinical services such as teleradiology, telepsychiatry, telepsychology, and teleneurology1. One of the primary benefits of telehealth is that it allows for the provision of specialist assessment and intervention to previously inaccessible and remote populations. Studies examining the use of clinical diagnostic interviewing, including patients with dementia, cognitive impairments, neuropsychiatric conditions and healthy controls, have shown good agreement between traditional face-to-face and telehealth conditions 1-5. In regards to sleep, the American Academy of Sleep Medicine Taskforce on Sleep Telemedicine supports telemedicine use for diagnosing sleep disorders6. A telehealth service for diagnosing or following up on sleep disorders, such as insomnia and sleep apnea, was found to be effective for consultations and management7. In addition to increasing access to assessment, telehealth has been used effectively to provide psychological therapy to cancer survivors in rural Australia, provide emotional and symptom support to improve quality of life among patients with cancer, increase access and speed at which young adults with cancer were able to receive psychosocial services, and provide support groups for rural minority groups8-11.
The use of telehealth has only begun to be applied to increase research participation. Historically, studies that use objective assessments requiring that the researcher and participant be face to face often only recruit individuals from a limited geographic region located near the city in which the study is being conducted. This limits the number and variety of individuals that can be included in the study. Telehealth is one approach that could be used to increase both sample size and representativeness. Others have made similar arguments for the use of telehealth in research, stating that telehealth could improve access to patients from rural, regional and other underprivileged settings; increase recruitment, which could lead to shorter study timeframes; and lead to better cancer care, which could reduce discrepancies in cancer outcomes in geographically diverse populations12. However, to the best of the authors’ knowledge, no study to date has assessed telehealth use in the research area of cancer, sleep, and cognition.
The present analysis aims to evaluate the experience of individuals diagnosed with breast or prostate cancer who participated by telehealth in studies investigating the effects of cancer treatment on sleep and cognition. Evaluation of participants’ experiences will highlight potential benefits of using telehealth and identify ways to improve the process for future studies and assessments.
Methods
Participants
Participants were recruited from one of two larger studies investigating the role of sleep disturbance in the first year of treatment on the development of cognitive impairment in newly diagnosed men with prostate cancer and women with breast cancer. The inclusion criteria of the larger studies required that individuals be English-speaking, aged greater than 18 years, for men to have intermediate or high risk adenocarcinoma of the prostate gland and be scheduled to receive radiation therapy with or without androgen deprivation therapy, or for women to have a diagnosis of stage I–III breast cancer and be scheduled to receive either adjuvant hormonal therapy or chemotherapy and hormonal therapy, and have not previously been treated for cancer or are not already undergoing cancer treatment. Exclusion criteria of the larger studies included that individuals must not have another sleep disorder, besides insomnia, that is not adequately treated, not have another psychological disorder that is not stable and/or would impair the ability to participate in the study, and must not have a score lower than 24 on the Mini-Mental State Examination, suggesting a severe cognitive impairment. The additional inclusion criteria for the current study is that individuals must have participated in the study via telehealth for at least one assessment to date.
Procedure
Larger studies: Prostate and breast cancer oncologists identified and screened eligible participants from clinical charts and provided them with information about the study. To confirm eligibility, such as treatment type and stage, patients’ medical charts were assessed. Interested patients spoke to a research team member on site about additional details of the study. Research team members scheduled an appointment with potential participants at their convenience.
For the assessments, a research team member was present at the Dr H. Bliss Murphy Cancer Centre, in St John’s, NL, Canada, and the participant was present at the nearest hospital or health clinic to their residence that had telehealth equipment. Telehealth is a secure system provided by region health authorities of Eastern, Central, Western, and Labrador-Grenfell Health of Newfoundland and Labrador. There was a technician on site to set up the teleconference equipment for participants. Informed consent was obtained, after which a medical, psychological, and sleep disorders screen and the Mini-Mental State Examination were administered to assure participants met the inclusion and exclusion criteria. Once eligibility was confirmed, participants completed a baseline assessment of sleep and cognition, followed by further assessments at 4, 8 and 12 months.
In addition to the collection of baseline demographic information the following sleep and cognitive measures were assessed: Insomnia Severity Index, Pittsburgh Sleep Quality Index, Controlled Oral Word Association Test, Letter-Number Sequencing, and Hopkins Verbal Learning Test-Revised (HVLT-R)13-16. The HVLT-R requires a 20–25 minute break before moving on to the next step, thus some self-reported questionnaires were verbally asked via telehealth. An actigraph (a wrist-worn device that measures sleep), a sleep diary, consent forms, and some self-report questionnaires were mailed to participants with a postage-paid envelope that was provided for return.
Present study: Participants who participated via telehealth in the larger studies were organized into the four regional health authorities of Newfoundland and Labrador: Eastern, Western, Central, and Grenfell-Labrador (n=45). Participants of varying ages and communities were then purposively chosen, to increase representativeness, to be contacted about participating in a telephone interview about their telehealth experience. For individuals who were interested, a time was scheduled at the patient’s convenience. Recruitment continued until saturation was achieved. The telephone interviews were conducted by a research team member, at the Sleep, Health, and Wellness Lab at Memorial University, and were approximately 5–10 minutes in duration. Participants were asked questions concerning what they liked and disliked about their experience participating in the study via telehealth, and invited to give suggestions for improvements (Box 1). Telephone interviews were recorded, and transcribed verbatim. All recordings were uploaded to a computer in the secure laboratory, where they were password-protected. Transcriptions were also password-protected on the laboratory computer.
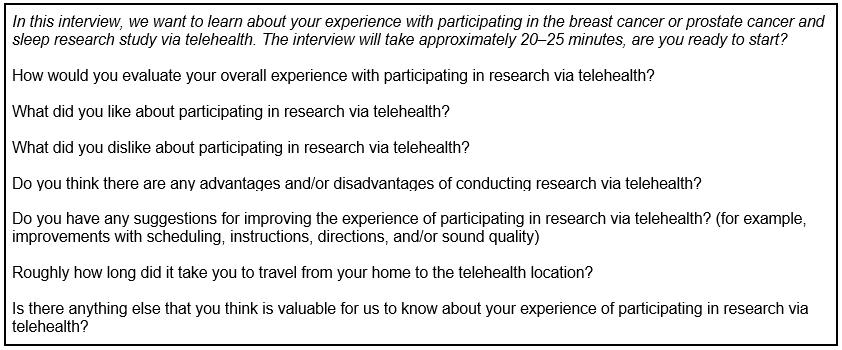 Box 1: Interview script and questions
Box 1: Interview script and questions
Statistical analysis
Demographic information was used to characterize the sample; the Statistical Package for the Social Sciences v25 (IBM; http://www.spss.com) was used. Interview transcripts were coded using a thematic analysis approach. One research team member began the coding process, developed a coding manual, and coded all interview scripts. Another research team member used the coding manual and coded 20% of the interview transcripts (two interview transcripts from individuals with breast cancer and two from individuals with prostate cancer) and inter-rater reliability was calculated (92% agreement). Any coding discrepancies were resolved by consensus.
Ethics approval
Both the larger studies and the present study received ethics approval (HREB# 2016.092 and #2016.145) from the Health Research Ethics Board of Newfoundland and Labrador. The larger studies obtained written consent, and the present study obtained verbal consent.
Results
In total, 13 individuals with breast cancer and 10 individuals with prostate cancer were approached. One individual was not interested in participating, and two individuals were too busy at the time to take part. The final sample included 12 individuals with breast cancer and 8 individuals with prostate cancer (Fig1).
Demographic information is presented in Table 1. Including telehealth as an option in the overall study allowed for a 55% sample size increase for participants with breast cancer and a 44.8% sample size increase for participants with prostate cancer. The average travel time from participants’ homes to the telehealth locations was 19 minutes (<10 minutes, 60%; 11–30 minutes, 20%; 31–59 minutes, 10%; >60 minutes, 10%). No individual described their overall experience as negative or unsatisfying; individuals described their overall experience as good/great (70%), fine (10%), a positive experience (5%), overall satisfying (5%), professional (5%), and insightful (5%). The themes that emerged could be classified in two categories: positive aspects of using telehealth and potential for improvement with telehealth.
Table 1: Demographic information about participants (n=20)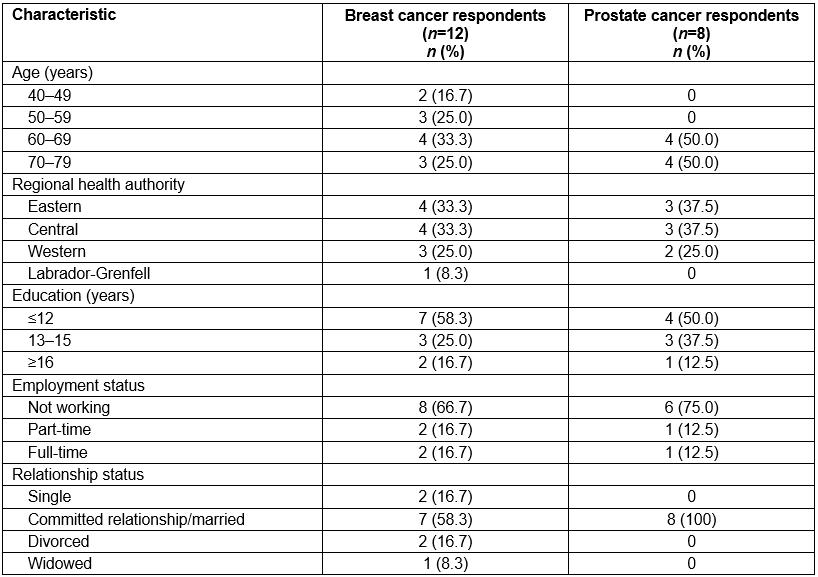
 Figure 1: Participant locations across Newfoundland and Labrador.
Figure 1: Participant locations across Newfoundland and Labrador.
Positive aspects of using telehealth
Convenient: Participants (80%) reported using telehealth made their participation in the study more convenient. Three subthemes emerged under this theme: travel, setup of equipment, and scheduling.
Participants noted the convenience of having a short distance to travel to the telehealth location, which saved time and money:
Just convenience, like overall convenience for whomever it is participating in the study. The fact that you’re in your home town, your rural community, there’s no time constraint. For me to have gone into town (St. John’s), [interviewer’s name], it would have been a 3-hour extra drive. You know what I mean, so just a time thing, it frees up more time that’s all. You know without having to take the extra time off work, and like I said to drive. So not only is it time consumption, it’s money involved too. For most people who have had cancer, a lot of people do not continue to work, whether through the diagnostic process or in fact if they are getting chemo or what not. And like they can’t afford to take … Like personally myself, I’m a single person okay, and I’ve missed quite a bit of work because of what I had to go through, and you know you’re always concerned with how much a place of employment can put up with, you know what I mean with regards to having an employee gone for so long. So, the fact that that makes it more convenient, and it makes it less stressful. (breast cancer, age 51)
And it’s very convenient because I, well you know I only have to travel like 20 minutes down to Lewisport … (prostate cancer, age 64)
Participants appreciated that the appointments and telehealth equipment for the study were set up for them, which made participation more convenient:
I mean it was pretty convenient for me, everything was set up … It was just a matter of me going into the hospital here and participating. (breast cancer, age 44)
Yes, everything was set up for me, so therefore it wasn’t a bit stressful. (prostate cancer, age 70)
Participants reported that the scheduling of study assessments was done at their convenience, with the researchers always trying to find a time that worked best for the participant:
For scheduling, I’ve had some stuff going on in my personal life … and you guys always worked around me. (breast cancer, age 55)
I found it good, you could decide your own time … you could do it at your own convenience really. (prostate cancer, age 70)
Increases access: Participants (50%) reported that a big advantage of using telehealth is that it allows individuals to participate in research, when they would not be able to otherwise due to their location outside of the city and/or in rural areas:
Well I guess it can reach people in faraway places, more conveniently, you know I would never be able to take part in the study if it wasn’t that way. (breast cancer, age 71)
I wouldn’t be able to do it if I had to come in to St. John’s, I wouldn’t be able to do that … I mean you know that’s a lot of travel and time you know … yeah no you wouldn’t get anyone to do it. (prostate cancer, age 73)
Personable: Participants (30%) reported that using telehealth for research made their experience more personable. Having the opportunity to be face to face while completing the study allowed participants’ experience to be more real and enjoyable, compared to if the study was over the phone, or filling questionnaires out on their own:
I can see it being an advantage, you know just for the contact itself, like the visual contact. If it was something that took place over the phone, I don’t see that as being as effective. For me I really enjoyed coming in and seeing you guys on the screen, and you see me, and kind of reading your body language, and I guess you guys kind of reading mine … it made it a little more personal. (breast cancer, age 44)
You can see the person who is asking you the questions … I think it’s an advantage because like I said it’s more personable. (prostate cancer, age 69)
Helping others: Participants (35%) reported that participating in the study via telehealth gave individuals the chance to help others in the future who are going through the same or similar cancer treatment:
Well the only reason why I participated is if it can help somebody else out – well why not … and like I said research is a good thing, you know if you can find out things that can help other people down the road somewhere then great. (breast cancer, age 69)
It’s hope, right, you know maybe something that I am doing might be able to benefit somebody else, right … and that’s what it felt like … ah I got 5 boys, and my fiancé’s got 5 boys, so you know prostate is a problem … so if I can do something to enhance that research then so be it … (prostate cancer, age 70)
Helping self: Participants (45%) described that the study helped them personally, with three subthemes emerging: memory, health, and being cared for. Participants indicated that by participating in the memory assessments, individuals were able to note where they stand, by comparing their memory performance at different time points. Other participants reported that the memory assessments acted as an exercise for their brain:
I thought it was good because it seemed like it helped strengthen my memory … (breast cancer, age 79)
Yeah I sort of looked forward to it because I had to benchmark myself … like you know, how I did like in my own mind, how did I do from the last time that I did it … yeah, it sort of put my mind at ease to see whether I am going ahead, or backwards … (prostate cancer, age 70)
Participants explained that by participating in the research study, individuals had the opportunity to be informed about different aspects of their health:
I find it helpful in the fact that if I was having problems with my medication, with some of the questions you guys would ask. I could relay them to my doctor, like you guys have even said, you think I have sleep apnea, and I could relay that to my doctor because of you guys … other than that research I would have never clued in to that maybe there is something wrong. (breast cancer, age 55)
Well I think it sort of helped me get to know the things about my health a little bit more, more aware of how I’m feeling or how I’m thinking … (breast cancer, age 65)
One participant highlighted that living in a rural area can be lonely at times, and that participating in the study via telehealth made her feel cared for:
It gives you a chance to talk to somebody, where you’re rural, and if you’re like me living alone all the time … and it makes you believe there’s someone else in the world who cares about you. (breast cancer, age 79)
Potential for improving the telehealth experience
Sound quality: Most individuals who participated in the study reported that the sound quality was good; however, for three participants the sound quality was not always favorable:
I mean sometimes we might have misunderstood each other a couple of times, you know something like that, but which is to be expected you know, but really there was no problems. The sound sometimes … when you were trying to remember the things she was saying, I think I might have misunderstood a couple of times a little and she may have misunderstood me, but you know. (breast cancer, age 55)
There were a few times that the sound wasn’t great, but we got over that. (breast cancer, age 79)
Access still an issue: For the most part, telehealth increased access to participating in the study; however, a couple of individuals who lived in rural areas reported that distance was still an issue. One individual suggested that telephone or skype could be a better option for those who experience access issues:
But you know the thing is I live off the grid, which means in the winter when the snow comes, we have to use skidoos to get to our vehicles … that put a block up against me being able to participate during the winter months. (breast cancer, age 63)
The only thing is the travel from home to the video conference … Because you know there’s a cost involved in that right? … if you’re going to keep on doing it the way you’ve been doing it, with secure video, maybe you should have a nominal fee in there for the people for gas money and stuff like that because some people are in areas like where there’s no public transportation … I think maybe, I don’t know just about, if it could be done by telephone or skype or something like that. (prostate cancer, age 70)
Discussion
This is the first study to date to examine the experience of individuals with breast and prostate cancer participating in a research study via telehealth. Individuals reported having an overall positive experience, and discussed many positive aspects of using telehealth for research purposes, as well as areas that could be improved. A primary theme identified was the convenience of the telehealth experience due to the reduction in travel time and cost, the ease of use with the telehealth equipment setup for participants, and scheduling accommodations. Similarly, a systematic review focusing on survivors of cancer found that telehealth interventions were perceived as convenient due to flexible scheduling and by reducing disruptions to daily routines, travel time, cost, and associated stress17. Previous research investigating the benefits of an outpatient telemedicine program that included 11 281 patients found that using telehealth resulted in a total travel time savings of 8.96 years, and a total cost savings of US$2,882,05618. Notably, Australia, which is sparsely populated similar to Canada, has incorporated telehealth into cancer care programs to increase access, leading to reduced costs, and high patient and physician satisfaction19.
In order to not place additional financial burden on participants, researchers need to find novel ways to reduce travel costs. Similarly, with large sample sizes often needed for research, it may not be feasible for studies to reimburse participants for travel costs. Furthermore, requiring participants to travel long distances would be an inconvenience imposed on individuals who are already dealing with many stressors. A study that investigated the factors that influence participation in clinically focused research found that researchers perceived reducing the time burden on participation as a key component20. Specifically, additional required travel time is viewed as an inconvenience to participants, and can often result in participants declining to take part in research20. Individuals also highlighted the convenience of participating in the study and that barriers to participation were removed, such as having readily available assistance to access telehealth equipment. Participants noted that the research assistants were very accommodating in scheduling the telehealth study assessments. For those who live in rural communities outside of the city where the study staff are located, telehealth is clearly a beneficial option in terms of convenience for participants.
Participants explained that using telehealth gave individuals the opportunity to participate in research that they would not have had otherwise. Newfoundland and Labrador, with a land area of 370 510.76 km2, has a population of 519 716, with a population density of 1.4 persons/km221. Forty-three percent of residents live outside of the metropolitan area21. In the present study, telehealth increased participation for individuals with breast cancer by 55%, and individuals with prostate cancer by 44.8%. The present sample included individuals from all four regional health authorities: Eastern, Central, Western, and Labrador-Grenfell. One way of improving research in the area of cognitive dysfunction and sleep in patients with breast and prostate cancer is to increase sample sizes and representativeness, and telehealth targets these issues.
Participants described their telehealth experience as personable, because of being able to see the researcher face to face. Some participants noted that using telehealth for research purposes was preferred instead of participating by telephone, or independently filling out questionnaires. For individuals living outside the city region, the personal touch of visual contact thanks to telehealth seems to keep participants more engaged and satisfied with the research experience. Similarly, telehealth has been found to allow for personalized relationships between cancer survivors and service providers due to individuals being able to communicate with healthcare personnel in their chosen environment, and feelings of more time to express their concerns, as opposed to hospital settings, where they would feel more rushed18. Additionally, one study highlighted a personalized approach, such as consistent interviewers throughout the study, as contributing to the retention of participants22. In contrast, some studies have found that individuals perceive telehealth as impersonal and lacking human contact, with some individuals noting a preference to know the healthcare practitioner before disclosing personal and sensitive information18. Thus, when using telehealth for research and health care, taking time to develop a relationship may be beneficial before inquiring about any personally sensitive information.
Although the present study was intended to focus specifically on aspects of the telehealth experience, individuals also communicated factors that they enjoyed about the overall study. Participants explained that participating in the study was important to them because they were hoping to help others in the future who would be going through a similar experience of receiving treatment for breast or prostate cancer. This is consistent with the literature, with one study reporting that a main reason for participation in clinical research is altruism, such as the desire to help future patients20.
Many participants explained that participating in the study allowed them to help themselves. Participants explained that the study helped with memory by being able to judge their own performance on the memory assessments at different time points, and with the memory assessments acting as an exercise for their brain. Individuals could be informed about different aspects of their health, which they reported as an aspect of the study they appreciated. This is consistent with other reports that research participation can have personal benefit. By participating in research, women with ovarian cancer reported that they received educational benefits about their health, and individuals with cardiovascular problems reported access to more continuous care23,24. Furthermore, studies including survivors of cancer found that telehealth provided an educational opportunity to improve or manage their symptoms, and raised awareness of potential issues to look out for in regards to cancer17.
Some participants identified that the sound quality was not always ideal during the study assessments; however, these individuals did not report that it hampered their overall experience or participation. Some studies have found similar findings, such as telehealth being a barrier to engagement among individuals with hearing difficulties, and that technical issues at times prevented connections being made17. When sound quality is not ideal, one potential solution suggested is to turn off the audio of telehealth, and to communicate with individuals via telephone25. This solution would allow researchers to maintain visual contact, while also improving communication.
Although telehealth improves access to participation in research for individuals living in rural areas, it is important to recognize that access still remains an issue for some individuals. One study compared therapy for individuals with diabetes being delivered face to face in clinic to internet video-conferencing via skype, and found no difference in treatment effects between conditions26. Future studies should investigate the generalizability of using skype or similar mediums for use with rural and remote participants.
Limitations
The findings of this study are based on a qualitative analysis, thus there exists a possibility of bias when interpreting participants’ attitudes and opinions. Every effort was made to assure the accuracy of results, including verbatim transcription of the interviews, having multiple coders, and performing an analysis of inter-rater reliability, which yielded a 92% agreement.
Additionally, it is possible that individuals who participated in the interviews encountered a different experience of participating in research via telehealth than those who were not interviewed.
Conclusions
Telehealth is an effective method to engage research participants and can aid in addressing methodological issues such as sample size and representativeness. Participants reported an overall positive experience, with telehealth allowing for greater convenience, more personable interactions, increased access, and an opportunity to help others and themselves. Identified areas for improvement were improving sound quality, and access for those who still face barriers of commuting to telehealth locations. Furthermore, although this study investigated the use of telehealth in a sample of individuals with cancer, telehealth would likely improve research and access to research and services in other health areas.
Acknowledgements
The authors thank the Dr H. Bliss Murphy Cancer Centre, Joy McCarthy MD, Erin Powell MD, Renee Lester MD, Melanie Seal MD, Jinka Sathya MD, Asim Kamran MD, Oliver Holmes MD, Dolores Rice and all the nursing staff; the telehealth site coordinators, Alice Nolan and Donna Foote; and research assistants of the larger study, Nicole Rodriguez, Kayla Wall, Hilary Rowe, and Megan Van Wijk.
References
You might also be interested in:
2012 - 'It's a regional thing': financial impact of renal transplantation on live donors

