Introduction
Pre-eclampsia is a condition that is part of a spectrum of conditions that can arise as a result of pregnancy-induced hypertension. The word ‘eclampsia’ stems from the Greek word for ‘lightning’, such as a seizure, that can happen very quickly and unexpectedly if the condition of pre-eclampsia is not recognised and controlled. Globally, half a million women and newborns still die each year as a direct result of pregnancy complications. Hypertensive disorders account for 12% of all maternal deaths1. In addition, pre-eclampsia is associated with short and long-term morbidity2. In the UK, pre-eclampsia affects up to 6% of pregnant women, with severe cases progressing to eclampsia in up to 2% of these pregnancies3.
Early identification of pre-eclampsia and its appropriate management before the onset of eclampsia is recognised as a way to mitigate the worst outcomes for mothers and newborns1. It is important that midwives and other healthcare practitioners, wherever they are located, have the knowledge and skills to identify and manage pre-eclampsia.
Providing emergency maternal care in Scottish rural and remote settings can be challenging. The National Health Service (NHS) Highland is the largest Health Board area (by land area) in the whole of the UK4. Yet, while it encompasses a land mass that is larger than Belgium, with a population of 333 000, which is smaller than that of most UK cities, 70% of the Highland population (233 100 people) live in small, isolated communities across the mainland and 93 inhabited islands. Highland Scotland is a popular tourist destination and a further 350 000 tourists are estimated to be drawn to the area each year, mainly to remote locations, mainly in the summer months of June through to September5, some of whom may be pregnant. There are unique challenges to delivering maternity services in this region.
Research by Harris et al found that providing midwifery care in the rural and remote regions of Scotland can be challenging6. Midwives’ perception of ‘rural’ can vary from the semi-urban to very remote locations where the added challenges of ambulance response time, ferry times and the weather prevail6. Other researchers have contended that rural and remote midwifery care can only be determined by those who live and/or work in these regions because they have the local knowledge of travel times across different weather conditions and modes of transportation7. This infers that professional and personal knowledge about care provision need to be specific to local conditions.
Midwifery practice in rural communities in Scotland and New Zealand has been described as regionally specific and underpinned by the resourcefulness and resilience of midwives serving these regions8. The ability to practise effectively in rural regions requires bespoke education and training to address this requirement. A Scottish government report9 noted:
Each of the remote, rural and island areas have different education and training support needs. However, these areas share an urgent and ongoing need to redesign the community and hospital workforce to ensure delivery of improved and sustainable services.
This article reports on a study undertaken in Highland Scotland and explores how pre-eclampsia outcomes might be further improved through rural midwives adopting a novel m-learning/m-health toolkit10. The demographics and geography of Highland Scotland are challenging for any providers of health care in the region. It has been reported that good communications between rural maternity care providers improve safety11. It can be construed that any technology that supports and improves communication in this area would be beneficial. However, it is unclear what is needed and wanted from such a technology for it to be acceptable and of value to rural midwifery practice. The aim of this study was to investigate whether a mobile health (m-health) intervention would be acceptable and useful to rural midwives in detecting, managing and making timely referrals of women presenting with possible pre-eclampsia and whether such technology would offer any advantage and/or improvement over current practice10.
Several studies have found that m-health interventions using apps and e-books on smartphones and tablets are useful to healthcare professionals11,12. There is some published evidence that midwives and community health workers in developing countries find these technologies support practice, reducing morbidity and mortality11. However, there is a lack of published literature on how such technology would support midwives in the early identification of women with pre-eclampsia in developed countries in rural and remote settings. Moreover, Speciale and Freytis highlighted how most m-health interventions lack theoretical underpinning or involve users in their planning13.
Engmann et al contend that political will needs to co-exist with sufficient investment and a well-trained workforce to create an environment where policymakers as well as healthcare professionals are aware of the transformative potential of mobile devices and interventions such as apps and interactive e-books to alter the way that maternal care is sought and delivered14. Furthermore, Tripp et al argue that it is important for healthcare professionals to be in tune with this trend15.
Methods
The study sought to understand the experiences of rural midwives, particularly in relation to implementation of an m-learning/m-health toolkit intervention into their practice. A qualitative descriptive approach was adopted16 and data were gathered from focus groups with rural practising midwives.
Midwives were recruited from three geographically and demographically diverse rural and remote Scottish locations. Participants took part in one of three focus groups, one in each of the areas where they worked (Table 1). The study drew from practice experiences of 18 midwives across the three focus groups. Scotland has a diverse geography, with each rural location having unique issues and concerns related to healthcare provision. When deciding upon locations for the study, different locations were selected to avoid any bias towards a particular topography, such as remote islands, or remote mountainous areas on the mainland. Therefore, each focus group brought a different dynamic to the conversations around the aim of the study17.
Inclusion criteria included midwives working at rural locations more than a 1-hour drive from towns with a population of 10 000 and at semi-rural locations that were within a 30-minute drive from towns with a population of 10 000 or more. Any midwives working in only urban environments were excluded from the study. Table 1 describes the three locations and an overview of the geographical logistics for the midwives.
Whilst most of the midwives who participated in the study were familiar with and had used a range of consumer health and wellbeing apps such as Apple Health and Fitbit, none had used an m-health intervention in their professional practice. The emphasis at each focus group was on the potential use of an m-health toolkit into their practice and whether it might offer any advantages over their current practice in respect of how they manage and support women presenting with pre-eclampsia.
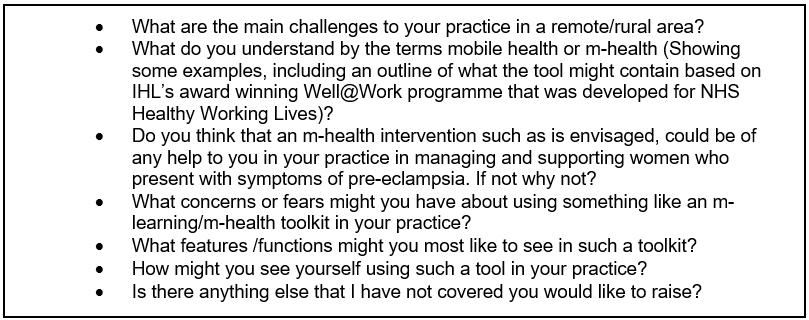
The focus groups took place at NHS Highland premises at the three locations (Table 1). Suitable times were mutually agreed with participants within their working days. The locations were anonymised. Not doing so could easily identify participants who work in a region where individual healthcare providers are highly visible and well known. The sample size was 18 out of a population of 332 midwives. The midwives who had agreed to participate in the study regularly experience geographical and logistical challenges. Not all were able to attend the focus groups in person and several needed to join virtually. All participants were familiar with using NHS Highland’s video-conferencing system within their rural practice roles. This enabled 10 midwives from the more remote locations to join the focus groups. Indicative questions were used in the focus groups to provoke a dialogue around the aim of the study (Box 1).
The focus groups were recorded, and the data transcribed, systematically coded and thematically analysed using Braun and Clarke’s thematic framework18. Codes and themes were developed through an iterative process with the research team until consensus was reached. The themes and coding were subsequently refined through presentation of the findings to a group of peers independent of the research team.
Table 1: Distribution of focus groups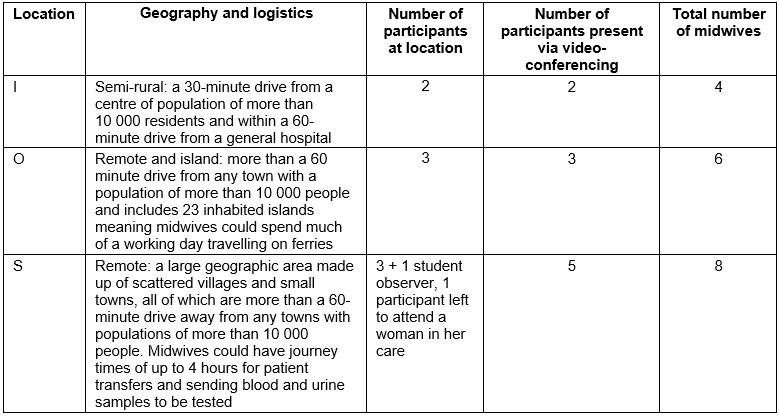
 Box 1: Indicative focus group questions
Box 1: Indicative focus group questions
Ethics approval
Ethics approval was granted by Robert Gordon University’s School of Nursing and Midwifery Review Panel (SERP) (10.08.2016) and NHS Highland Research Development and Innovation (224895 : 01/04/2017). The primary author was granted an NHS Research Passport (a mechanism for non-NHS staff to obtain an honorary research contract or letter of access when they propose to carry out research in the NHS). All the participants were provided with a participant information sheet prior to recruitment. The data were anonymised, using numeric pseudonyms. Participants were given the opportunity to ask questions about the study. Consent from participants was obtained prior to commencement of focus group conversations.
Results
Five main themes and 10 subthemes were identified in the transcribed focus groups data (Table 2). Each theme is presented with supporting data from the transcribed focus group recordings.
Table 2: Themes and subthemes of transcribed focus group data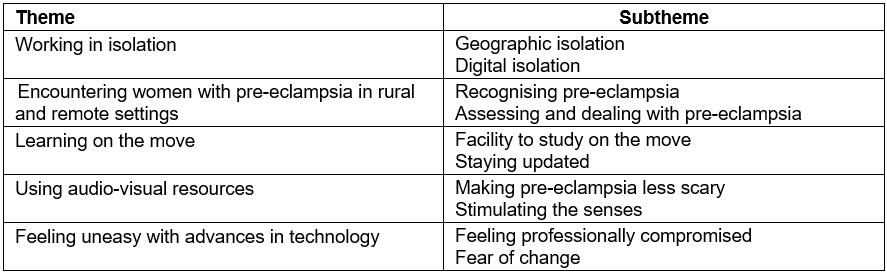
Working in isolation
Working in isolation can be described as a social phenomenon but it also reveals the potential for professional isolation. This theme highlights that midwives were concerned about working at a distance from specialist obstetric clinicians’ support without robust internet connectivity, This sense of distance and disconnection was revealed through two subthemes: geographic isolation and digital isolation.
Midwives working in rural and especially in remote locations have challenges over and above those faced by their peers who work in or close to urban centres. In particular, these include lengthy journey times associated with the distance from hospitals, extreme weather and variable road conditions. A midwife described how this affects decision making in her practice:
Decision making is a big challenge because it’s not just about your clinical assessment you’re making. It’s all of these elements, you know, yeah, the best made plans, you want to get her from here to here but it’s all of these elements that you have to take on board to make that happen and it could be that your road’s closed and you're having to go another 60 miles along a diverted route, and our colleagues in the referral centres don’t get that concept and the geography of and, so that’s a challenge. (Midwife 3, focus group O)
This is exacerbated by a perception among the midwives that their colleagues in urban-based specialist centres have little personal experience of these challenges and do not fully understand the clinical implications that might arise as a consequence. Another rural midwife described her experience in communicating with clinicians:
Yeah, I’d also add that it’s difficult sometimes to communicate your concerns effectively to the clinicians that you’re talking to on the phone. Obviously you’ve got the patient in front of us and we’re telling them what our findings are but sometimes it’s difficult to get across exactly what’s going on to somebody on the phone who doesn’t appreciate it but what kind of area, remote and rural you are. (midwife 4, focus group S)
In addition, ‘geographical isolation’ became more apparent and intense when the need for transfers involved lengthy travel times in severe weather. One of the midwives shared her experience:
Weather, weather is part of the transport challenges, especially if it’s an air transport, they can only fly if the weather’s permitting, they can only land if the weather’s permitting so, obviously that’s a challenge, I mean that can be, and even if they do get in there it’s, you know, we’ll have transfers that are aiming to end up in Glasgow but they end up in Ayrshire and getting transported in by road, which adds to the delay. (midwife 1, focus group O)
Communication pathways are crucial in maternity services because they involve care in the community and at times involve necessary consultation with a multidisciplinary team, particularly pertinent when morbidities arise such as pre-eclampsia. The challenges of communication across rural and remote locations can be problematic for rural midwives when there is inconsistency of mobile phone signals across Highland Scotland. The midwives in the study experienced digital isolation daily. Midwives reported concerns about their mobile phone coverage is ‘at best patchy’ in many locations. A midwife based at another remote location saw advantages in using a tool that was preloaded onto a digital device:
It’s a bit reassuring that this is not something that’s going to have to rely on signal on Wi-Fi or not, because that is a challenge. (midwife 2, focus group O)
This theme has revealed particular challenges around how rural midwives communicate with colleagues in labs and obstetric units based in general hospitals and around lengthy travel times, which can be aggravated by severe weather. These, combined with ‘at best patchy’ mobile phone connectivity, can have implications when rural midwives encounter pre-eclampsia. Having access to up-to date information without the need for constant connectivity was viewed as helpful by some of the midwives.
Encountering women with pre-eclampsia
This theme explores how midwives diagnose and manage women with pre-eclampsia in rural and remote settings. Although there have been no recent deaths as a result of pre-eclampsia, there are challenges in communicating and maintaining women’s care needs particularly if they are visitors to the region10. There is at present an expectation that women undergoing treatment and intending to travel will carry their paper maternity records with them. This approach relies upon women remembering to carry their records and not losing them. A midwife reflected on her experience:
The scariest cases I’ve had have been with holiday makers, they just pitch up and they-re usually the ones that have got fulminating preeclampsia, you’ve never met them before, try to find things in their notes, they maybe don’t have their notes with them, so I think that certainly highlights it’s good to have a national set of guidelines. (midwife 5, focus group O)
This can put extra demands on rural midwives. In some instances, rural midwives recognise, assess and manage pre-eclampsia in remote and rural settings, requiring seamless communication pathways and access to information to provide effective timely care. Midwives described how it may be possible that such an assessment and management situation could be enhanced using a m-learning/m-health toolkit:
… because we’re not located within a hospital environment, we sometimes worry that we’re not always hearing the updated information, policies and procedures change or management of things, like pre-eclampsia – updated information is not filtered through … We're going paper light and not carrying round lots of folders when we’re dealing with something. Obviously pre-eclampsia we are fairly used to dealing with but other more unusual things, maybe we haven’t dealt with them for some time and we’ve got to get back to base to log onto the computer to look it up. Some kind of preloaded device with current guidelines would potentially be very helpful when we’re out and about in community to have at our fingertips. (midwife 8, focus group S)
This midwife is suggesting that she and her colleagues need to be kept up to date and be able to access up-to-date information as a rural midwife in the same way her urban based colleagues can.
The theme of encountering women with pre-eclampsia reveals some instances of how midwives recognise, assess and manage pre-eclampsia in remote and rural settings. It may be possible that assessment and management practice are enhanced using an m-learning/m-health toolkit as discussed during the focus groups.
Learning on the move
Healthcare information, guidance and protocols are continually changing. Participants could see the advantage of a mobile device that held information that could be accessed without any need to connect to the internet. Having access to up-to-date information without the need for constant connectivity was viewed as helpful by some of the midwives:
I think it’d be useful for us when we’re on the road and, you know, just having something that is just in our hands that was current and up to date rather than trying to come back to the unit and access the intranet, you know. (midwife 3, focus group S)
It is also a requirement of the UK Nursing and Midwifery Council that midwives undertake regular continuous professional development (CPD). Highland midwives currently must work on this by logging on to the LearnPro or NHS Scotland’s new Turas learning management systems on NHS computers either at their practice bases or at home. The m-learning/m-health toolkit could enable them to work on their CPD away from any connection to the internet. Participants welcomed the idea of using a mobile device that requires no internet connectivity for supporting their CPD requirements:
… a lot of things are on LearnPro, and with the best will in the world it’s very time consuming, the amount of time you have to spend doing that. Now, if you had some of that actually available on your phone so that, actually, when you were sitting on a train, sitting on a ferry, you could do that and have it then signed off and it linked into LearnPro then actually it would probably take the pressure off folk for their PDP [CPD]. (midwife 1, focus group O)
This flexibility appealed to the midwives irrespective of their locations and could be useful during the time rural midwives spend travelling on planes to visit island communities or on trains to attend face-to-face meetings and trainings in Inverness (their employing main centre and tertiary hospital).
Using audio-visual resources
Audio-visual resources support the acquisition of knowledge by text and other media. This could include using pictures (still or moving images), voice and music. They do not necessarily have to rely on sophisticated technologies to communicate with learners using mobile devices. The inclusion of audio-visual multimedia resources in the learning materials appeared to be acceptable. Participants discussed how audio-visual multimedia could be tailored to use as an interface between midwives and women who had been diagnosed with pre-eclampsia to facilitate explanations about what was happening.
I suppose, you know, pre-eclampsia can be quite a scary sort of subject when you’re sort of talking to women about it so you using a kind of cartoon format while you’re still giving information maybe makes it a little bit less scary, you know, it’s, you can, you can obviously expand on it through your discussion but, it’s, it’s not quite so sort of intimidating maybe when you’re talking about something that’s potentially quite serious, you know, condition, you know, it may be kind of, you know, doesn’t scare them too much if you’ve got a format like that. (midwife 8, focus group S)
Participants also felt that an m-health intervention with its multimedia content could be helpful in various situations they encounter. Examples include during transfers by ambulance to a general hospital, when women and paramedics could watch a short program together about what a woman diagnosed with pre-eclampsia can expect or having short multimedia modules where users could use the audio-only option to listen and learn whilst undertaking other activities such as driving, cycling, running and walking. Overall, the midwives were positive about a multimedia module on a mobile device that could take account of different situations and learning styles. However, some midwives had reservations about the reliability and usefulness of technological innovation:
As long as it’s [the m-learning tool] reliable and it’s actually … supporting practice, or beneficial to practice rather than just another thing you have to do then, then yes, there’s lots of opportunity, but it has to be reliable and it has to be of benefit. (midwife 4, focus group S)
In general, the midwives in the focus groups were positive about a multimedia module on a mobile device that could take account of all learning styles and provide a useful interface between midwives and the women in their care across various situations.
Feeling uneasy with advances in technology
Although the participants discussed the advantages of having a multimedia module, there was apprehension among some participants about the possible addition of new technology into their professional practice. This also reflected the participants’ unease with the possibility of the introduction of new technology into their professional practice.
I’m sure you would understand that we pride ourselves on actually making sure that we are competent and able to practise. We put a lot of effort into that, that’s a completely different demographic that having worked in a lot of countries, the level of training and learning for a lot of midwives, never mind when you go out to community health workers, so you’ve got to look at the demographics. (midwife 1, focus group O)
This unease appeared to be embedded in the fierce sense of the midwives’ pride in their practice. It may well be that this combination of pride in practice and an apparent unease with advances in technology could present the greatest barrier to the adoption of an m-learning/m-health toolkit:
Despite these reservations, the midwives recognised the utility of m-health technology in managing pre-eclampsia:
… you maybe haven’t dealt with them [woman with pre-eclampsia] for some time and then you’ve got to get back to base to log onto the computer to look up what the guidelines are and everything around it. So, some kind of preloaded device with current guidelines would potentially be very helpful when we’re out and about in community. (midwife 8, focus group S)
Although some resistance to change was evident, the midwives wanted to improve practice in their regions and be proactive in finding solutions:
… we want to be part of something that’s going to make a difference. (midwife 3, focus group O)
Although this study has revealed that geographic and digital isolation are significant challenges, an m-learning/m-health toolkit could be part of a solution to these challenges. Despite there being some reservations and concerns about introduction of new technology into practice, the data do suggest that a new approach to enable ‘learning on the move’ would be very much welcomed. Furthermore, most participants would be willing to try out an m-learning/m-health toolkit, providing they are consulted from the outset about their needs and that they are involved in the development of the toolkit.
Discussion
This study sought to discover whether a solution, such as an m-health intervention, would be acceptable and useful to rural midwives in detecting, managing and making timely referrals for pre-eclampsia. The findings highlight a number of salient and significant issues.
Geographic and digital isolation are daily challenges faced by midwives working at remote and rural locations in Highland Scotland. The mountainous terrain of Highland Scotland will, for the foreseeable future, make the quality and signal strength of line of sight connectivity via mobile phone masts inconsistent. Most participants saw advantages in an m-learning/m-health toolkit that requires no internet connectivity.
The ability to work on CPD whilst on the move is also welcomed and supports the hypothesis that a mobile device, preloaded with an m-learning/m-health toolkit (no internet connection required) could mitigate at least some of the challenges of working on the move in both geographic and digital isolation. The study also aimed to find out whether a solution such as that proposed offers any advantage and/or improvement over current practice, and findings suggest that there is the potential for m-health technology to be helpful to rural midwives. The inclusion of CPD modules might be the most useful feature of an m-learning/m-health toolkit. It could enable midwives to utilise downtime (eg travelling on ferries) rather than needing to wait until they were either online at their base or at home. The ability to stay up to date and ensure CPD can be difficult and Gilkison et al suggest that the ability to practise effectively in rural regions requires bespoke education and training to address this requirement8.
It was unsurprising that a potential mobile e-learning innovation was welcomed by participants. In addition, the possibility of using multimedia as an explanatory interface between midwives and women who have been diagnosed with pre-eclampsia was also welcomed. Conversely, some midwives felt uneasy with advances in technology and that their professional integrity and autonomy might be compromised by the introduction of an m-learning/m-health toolkit, and a few participants considered that rural midwives are not the most appropriate audience for an m-learning/m-health toolkit.
Despite some misgivings about the appropriateness of the technology to their practice, participants were all pleased to have been consulted on their opinions. Crowther and Smythe contended that rural and remote midwifery care can only be determined by those that live and/or work in these regions7. Significantly, the importance of midwives to be involved in the development of such interventions was apparent throughout the data. This, in turn, may help to ensure the feasibility, acceptability and sustainability of any m-health intervention. The importance of involving end users in the design of new m-health interventions is therefore crucial and is congruent with previous studies13,19.
Familiarity with the introduction of technological innovations into practice can also help. Evidence from a recent Canadian study20 suggests that the ubiquity and familiarity with using mobile devices has enabled nurses at remote locations to embrace m-health and m-learning resources to enhance their practice and to strengthen their communities of practice. Familiarity among Highland midwives in using mobile devices might transform the way in which they and other healthcare practitioners work at remote locations but would need to be supported by policymakers in the area of reproductive, maternal and child health.
The findings of this study are consistent with Lee et al’s systematic review that concluded that many m-health interventions lack a sound evidence base21. This study has demonstrated that behaviour change is required, and any intervention needs to be acceptable to the end user. Such challenges need to be resolved for interventions using mobile devices to gain credibility and acceptance among healthcare practitioners, such as rural midwives, who serve scattered communities in remote locations20.
Strengths and limitations
The strength of the study is that it drew from rural midwives’ current practice experiences. It was able to highlight the feasibility of a technology and how this can be developed through consultation and ensure regional specificity. A limitation and strength of the study was that the first author was a layperson with little understanding of clinical midwifery, the professional concerns or the reality of their midwifery practice. However, knowing the technology enabled the researcher to adequately describe the intervention in the focus groups.
This was a small study in one region and participants were recruited from only one health board. The advantage of this was to the ability to collect rich contextual data and identify nuanced understandings of the domain through in-depth analysis that could be transferable to similar locations. There are multiple issues and concerns that the authors could have focused on rather than pre-eclampsia. Pre-eclampsia was an example of subject matter through which the authors were able to demonstrate an appreciation and understanding of what would be involved and acceptable regarding m-learning/m-health technology – knowledge that could be applied to other areas, such as gestational diabetes and foetal growth restriction.
Conclusion
This article reports on a small qualitative descriptive study that explores how midwives working at rural and remote locations in Highland Scotland perceive the idea of introducing a new m-learning/m-health toolkit into their practice and whether it could offer any advantages over their current practice. The study found that such an m-health/m-learning toolkit, which requires no internet connectivity, might offer several advantages in mitigating the negative effects of working in isolation. These advantages may be transferable to other healthcare providers and regions. Perhaps most importantly, the study confirmed that it is essential that those who are expected to use such tools are involved from the very beginning in the concept development, design, subsequent feasibility studies and ultimately the introduction of such tools into mainstream practice.
Future research
The study could potentially inform further research into contexts where partnerships between government, healthcare providers, the private sector and universities might be developed. Such development holds a promise of a future where advances in m-health/m-learning could be ever more closely aligned with transformational advances in the use of mobile devices – a new era when midwives and their other healthcare practitioner colleagues at rural and remote locations could be supported to work more effectively whilst on the move. The current study has led to the development of a prototype of a novel m-learning/m-health toolkit that is being tested in remote parts of Highland Scotland as part of a small feasibility study involving multidisciplinary healthcare teams that include lay volunteers. Service evaluation will follow this feasibility study and seek to ascertain if the standard of care desired is the standard achieved through implementation prior to further upscaling being recommended. Further studies building on this Scottish study are planned in sub-Saharan African regions with a view to ongoing evaluation and upscaling in these regions.
Acknowledgements
Thanks to the midwife participants who contributed to the focus groups for graciously providing professional insights drawn from their rural practice experiences.
References
You might also be interested in:
2013 - Multiple mini-interview scores of medical school applicants with and without rural attributes
