Introduction
Based on recent global estimates, one in every 9 children aged less than 5 years dies as a result of a form of diarrhoea1; and the annual under-five prevalence rate is about 42%2. Within developing regions, the burden of diarrhoea is more tragic among children (<5 years) in urban informal settlements3. In Kenyan urban informal settlements, about 100 children die every day from diarrhoea4. Reports elsewhere reveal that children from poor resource settings often have inadequate access to improved water, sanitation and hygiene (WASH) facilities2,4, and are therefore extremely vulnerable to poor hygiene practices and disease transmission5,6. As a result, children from these settings account for the highest child morbidity and mortality rates worldwide7-9. For instance, studies showed that in the Korogocho urban informal settlement of Nairobi, the 2 weeks’ prevalence rate was 35.6%4, in Burundi it was 32.6%10, whereas in Papua New Guinean urban informal settlements, in the south-west Pacific region, the prevalence rate was 24.0%11.
In the Solomon Islands, diarrhoea is the second leading cause of under-five mortality12,13; with about one in every 10 children dying from it before reaching 5 years14. In 2005, the country recorded the highest number of under-five diarrhoeal cases among the nine Pacific Islands countries with available data15,16.
Other studies have revealed that drinking untreated water4,17,18, poor sanitary facilities, the presence of stagnant wastewater6,11, observed flies and scattered solid waste near households4,6, plus the low altitude and near distance of under-five households to exposed areas such as garbage dumpsites6,11,19 were associated with under-five diarrhoea.
Globally, nearly 2 billion people are currently without suitable water and sanitation facilities3. In addition, many urban informal settlements are built without municipal approval and are often built in ill-suited locations that predispose residents to diarrhoeal disease transmission11,20. In Pacific Island countries, urban areas such as Nuku’alofa, Suva and Lautoka have informal settlements that are located on former mangrove swamps, leaving people vulnerable to storm flooding, waterborne diseases and sanitation problems. In Port Moresby, Madang and Honiara, informal settlements are located on town garbage dump sites, steep slopes, near rivers and coastal areas7,21,22. With relatively low monthly earning and high family size, dwellers of urban informal settlements often face numerous challenges associated with living in poor environmental conditions2,4,6,8,10,23,24.
Children under 5 years are often at high risk of diarrhoeal infection1,16,23-25. This is because, within this age group, or at least after age 6 months, children start to be weaned from breast milk and its disease-protective properties. Crawling and walking commences within this age group and the risk of picking up contaminated materials is often high4. Further, 3–4 years is the school enrolment age, whereby children start to be exposed to the wider environment. This suggests that under-five children should be given optimal care11,26.
Efforts to combat diarrhoea infection and to improve child health worldwide include the inclusion of rotavirus vaccines as one of the necessary components of the WHO and UNICEF Integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea among member countries27. WHO and UNICEF have developed hand hygiene guidelines as for health educators worldwide28. The importance of children’s health and the ability to survive childhood are also incorporated into the United Nations Millennium Development Goals and Sustainable Development Goals29,30, which are global health indicators for all nations.
In the Solomon Islands, the National Health Strategic Plan 2016–2020 has prioritised the health of children, especially children from disadvantaged communities31. This is necessary to make schools and communities, and households, important settings in which to protect and promote the health of children32. The WASH accessibility approach is important to reduce the gap between WASH facility accessibility among urban rich and poor residents3, and further reduce the rate of open defecators6. Community health education among caregivers is important in order to increase knowledge about the causes, effects, mode of transmission and prevention of under-five diarrhoea33. It is reported that about one-third of under-five diarrhoeal deaths in developing countries are due to consumption of contaminated water34. However, through preventative efforts, 30–40% of yearly mortality cases worldwide could be avoided33,34.
To reduce the tremendous burden of diarrhoea among children under 5 years in Honiara, Solomon Islands, it is important to identify the associated risk factors in order to design effective intervention strategies to prevent diarrhoea and to promote diarrhoea awareness among caregivers. This is the first documented study that aims to identify risk factors in the Solomons; no previous baseline studies have been conducted in the Solomon Islands. The aim of this study was to assess the environmental factors associated with under-five diarrhoeal prevalence in the Mataniko informal settlements, Honiara, Solomon Islands.
Methods
Study design and setting
A community-based cross-sectional study was conducted at Mamana Wata, Lord Howe and Koa Hill settlements, situated along the Mataniko River corridor, in Honiara, Solomon Islands, from June to July 2016. Honiara is the capital city of Solomon Islands, with an estimated population of 64 609 people, as of the 2009 census7,22. Three out of the six settlements along the Mataniko River corridor were randomly selected (Figs1,2).
 Figure 1: Map of Mamana Wata (left) and Lord Howe settlement (right) showing the surveyed under-five households.
Figure 1: Map of Mamana Wata (left) and Lord Howe settlement (right) showing the surveyed under-five households.
 Figure 2: Map of East Koa Hill settlement showing the surveyed under-five households.
Figure 2: Map of East Koa Hill settlement showing the surveyed under-five households.
Sampling and sample
The potential households in the three settlements were selected on the basis of having at least one child under 5 years. The source population, therefore, were caregivers who were responsible for taking care of children every day. In this study, some households had more than one caregiver and some caregivers had more than one child (<5 years). In the analysis, a caregiver with more than one child was treated the same way as a caregiver with only one child. However, in a situation where a caregiver had two or more children (<5 years) and only one experienced diarrhoea, only the case child was considered in the analysis.
Data collection tool and procedure
Instruments employed to collect the study variables were global positioning system (GPS) technology and a questionnaire. A pilot testing exercise was carried out to validate the data collection tools prior to the actual survey.
The outcome variable was collected based on a 2-week recall of diarrhoea episodes, and cases were verified using each child’s medical record. A 2-week recall period was used because it is reasonable for memory and limits recall bias35. To avoid double-counting, each surveyed household was geo-referenced (assigned x and y coordinates) using GPS. The definition of diarrhoea was translated into a commonly spoken dialect known as Pidgin English, in a way that maintained the original meaning of diarrhoea.
A voluntary informed consent form was issued to each child’s caregiver. Data were collected by two research assistants and a callback visit was made for caregivers who were not available at the time of the first household visit, including those caregivers whose children (<5 years) had diarrhoea and were unable to participate in the first visit.
Data analysis
Data were entered and analysed using the Statistical Package for the Social Sciences v23 (IBM; http://www.spss.com). In the univariate analyses, categorical variables were displayed as counts and percentages, and continuous variables were expressed as mean±standard deviation. Binary logistic regression was used to measure the strength of association between under-five diarrhoea and the independent variables by calculating the odd ratios (OR) and 95% confidence intervals (CIs). A p-value less than 0.05 was considered as statistically significant (p<0.05).
Ethics approval
This study was approved by the responsible Research and Ethics Committee of the Fiji National University and the Solomon Islands Ministry of Health and Medical Services.
Results
A total of 205 caregivers with at least one child under 5 years participated in the study. This was all households in the study area that had a child under 5 years, so the response rate was 100%. As Table 1 shows, the mean ages of caregivers and the under-five children were 30.7 (±8.2 SD) years and 2.6 (±1.5 SD) years, respectively. Among 205 caregivers, 94 had reported that their children (<5 years) had suffered with at least one episode of diarrhoea within the 2 weeks prior to the survey. This gives a prevalence rate of 45.9% (Table 1).
Table 1: Under-five diarrhoea occurrence within 2 weeks prior to the survey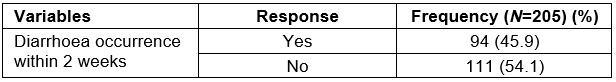
Environmental characteristics of households
Table 2 demonstrates that 56.6% of the participants did not have access to safe water and 73.2% of them did not own a toilet facility. The study also showed that there were stagnant wastewater (7.3%), flies (48.3%), scattered solid waste (71.2%) and water-filled containers (34.1%) near some under-five households. Of all under-five households, many (61.0%) were built on low altitude areas (≤19 m above sea level); and nearly three-quarters (70.6%) were built near (≤125 m) the river.
Table 2: Environmental characteristics of households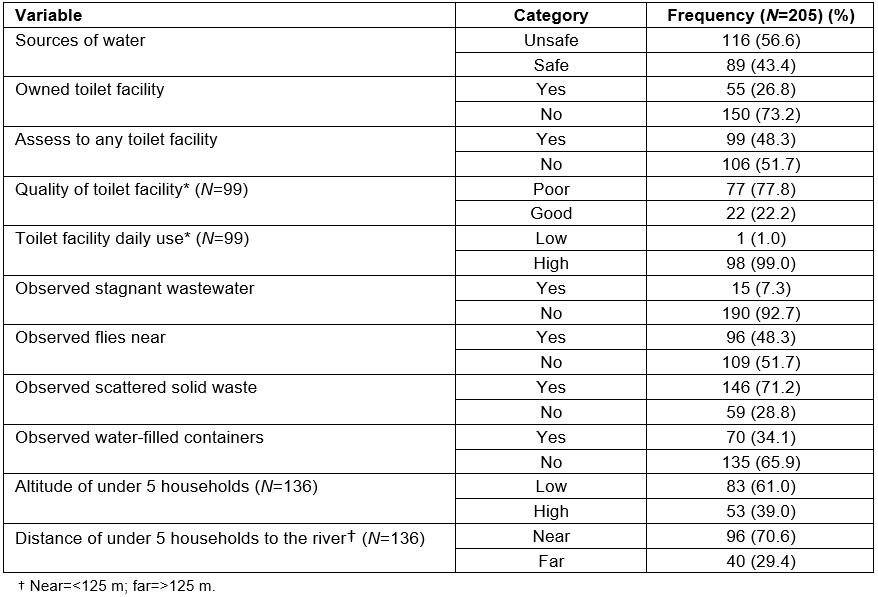
Association between environmental factors and under-five diarrhoea
The presence of stagnant wastewater, flies, solid waste and water-filled containers near households, and the distance of under-five households to the river, were found to be significantly associated with under-five diarrhoea in Mataniko informal settlements (p<0.05). These results are summarised in Table 3.
Key findings revealed that the chance of having diarrhoea increased by 3.6 times (OR=3.55, 95%CI: 1.09, 11.53) among children from households with observed stagnant wastewater, 1.9 times (OR=1.89, 95%CI: 1.08, 3.29) among children from households with observed flies and 2.0 times (OR=2.00, 95%CI: 1.07, 3.76) among children from households with observed solid waste, compared to their respective counterparts. In addition, children from households situated far (>125 m) from the river were 2.6 times less likely to have diarrhoea.
Although access to safe water and sanitation facilities were not associated with under-five diarrhoea, results revealed that the likelihood of having diarrhoea increased by 47% and 66% respectively, among children whose caregivers did not have access to safe water sources and toilet facilities.
Table 3: Environmental characteristics of caregivers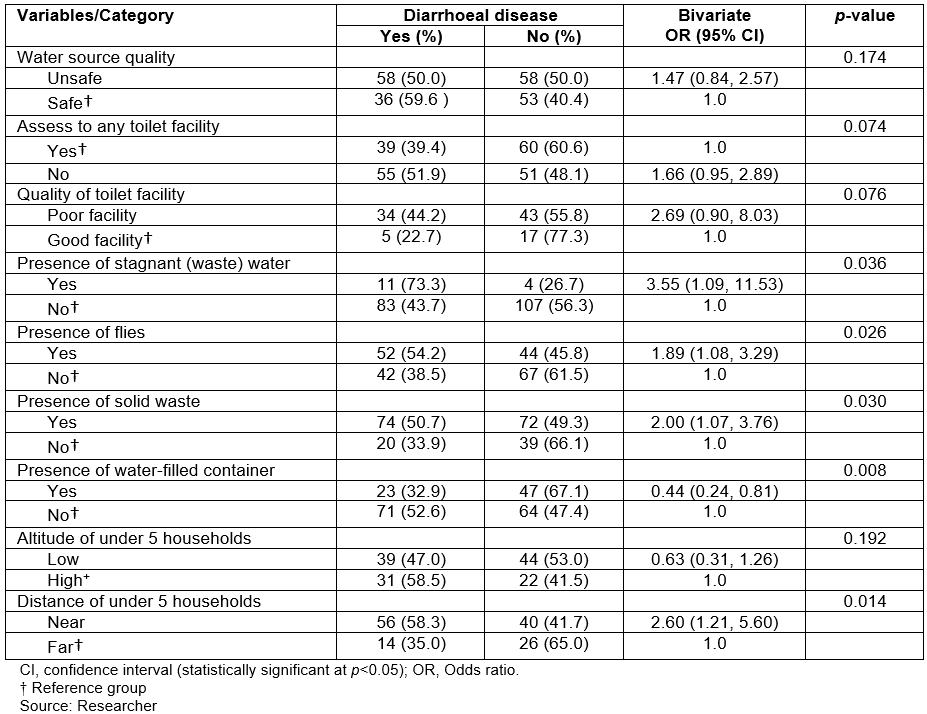
Discussion
This study has identified the prevalence of diarrhoea among children (<5 years) in Mataniko informal settlements and some of the related environmental factors. This is the first documented prevalence study of under-five diarrhoea in Honiara, Solomon Islands. The 2-weeks’ diarrhoeal prevalence rate (45.9%) was higher than the national prevalence rate (9.4%) cited in the Solomon Islands Demographic and Health Survey16, and studies conducted in other developing regions in Africa, including in Nairobi (35.6%)4, Burundi (32.6%)10, Southern Ethiopia (11.0%)24, and Papua New Guinean urban informal settlements (24.0%)11. The high prevalence rate (45.9%) in the context of the Mataniko informal settlements was mainly due to the fact that caregivers and children (<5 years) were frequently exposed to the contaminated Mataniko River. The river has been used by business houses and informal settlers situated along the Mataniko River corridor to dispose their solid and liquid waste, including human waste. The high prevalence rate was also due to the high proportion of younger children (≤2 years) in the study who are at high risk of diarrhoeal infection. Further, about half (49.3%) of participants were younger caregivers (≤29 years), who often have little experienced in child care36. The scope of study also influenced the results because it covered only a subset of the urban informal settlements. Nonetheless, such an alarming rate indicates an urgent need for public health prevention intervention.
In this study, results revealed that poor access to a safe water source was not significantly associated with under-five diarrhoea (p>0.05). This is in agreement with one other study4. In this study, this non-significant relationship could be influenced by the fact that some households without access to a safe water source had the practice of boiling their drinking water. Boiling drinking water can kill germs and prevent under-five diarrhoea4,10. It could be also influenced by the fact that younger infants (≤6 months) in the analysis were breast fed at the time of study and were thus unlikely to drink water. Nevertheless, since the majority (61.7%) of cases were reported by caregivers from households without access to a safe water source, the study supports the broad conclusion that children coming from households obtaining their water from protected sources were less likely to have diarrhoea2,4,18.
Other studies have revealed that poor access to improved toilet facilities is significantly associated with under-five diarrhoea4. In this study, the statistical significance of access to a toilet facility was p=0.074, which was slightly above the cut off (alpha) of p<0.05. This suggests that although not meeting statistical significance, access to good toilet facilities appears to be a factor influencing diarrhoeal infection. A majority of toilet facilities were not regularly cleaned (57.6%) and most (81.8%) were classified as poor toilet facilities, which were characterised by poor running water systems, overflowed sewage during heavy rain and often a bad smell. The fact that only a few families (22.2%) had access to good toilet facilities indicates that children from households with access to poor toilet facilities were also at risk for diarrhoeal infection because of the poor status of their toilets. As mentioned earlier, the majority of under-five children in this study were aged ≤2 years (58.5%), and thus were incapable of using the toilets by themselves. This suggests that they were more likely to be infected with diarrhoeal pathogens from within and around the household environment, and also through poor hand hygiene by their caregivers after using the toilets or changing diapers. This emphasises that access to cheap and good quality toilet facilities is necessary to ensure appropriate disposal of human waste4. It should be noted that in this study the likelihood of having diarrhoea was about 2.7 times higher (OR=2.69, 95%CI: 0.90, 8.03) among children whose caregivers did not have access to good toilet facilities. Other studies have revealed that children from households using modern toilet facilities were more than 60% less likely to experience diarrhoea6.
As in other studies, this study observed that stagnant wastewater, flies, solid waste and presence of water-filled containers near under-five households were associated with under-five diarrhoea (p<0.05). Regarding the presence of stagnant wastewater, these results are consistent with a study by Uwizeye et al, which revealed that stagnant wastewater near households, due to poor drainage systems, was associated with diarrhoeal prevalence6. This study showed that the likelihood of having diarrhoea was increased by a factor of 3.6 among children (<5 years) from households with observed stagnant wastewater.
In this study, many of the diarrhoea cases were reported by caregivers with the presence of flies (55.3%) and scattered solid waste (78.7%) near their households. These findings were statistically significant (p<0.05), and are consistent with other studies11,36 where flies observed in close proximity to households due to uncollected garbage, as well as scattered faecal waste on footpaths and near households, were associated with under-five diarrhoea prevalence4,4. This indicates that children (<5 years) were also infected with diarrhoeal pathogens from their surrounding household environment, where they often played. This suggests that government bins should not be placed too near households, as children potentially have contact with them.
Results further revealed higher reported diarrhoeal cases from under-five households located in low altitude areas (55.7%) compared to those located in high altitude areas (44.3%). However, such differences were not statistically significant (p<0.05). This may be due to the physical landscape of the settlements. For instance, Mamana Wata and Lord Howe settlements are located on low-lying coastal areas, whereas Koa Hill is located further inland near a hillside. It is also possible that it was due to small sample size.
These findings are not consistent with other studies that have found that altitude of households was significantly associated with disease occurrence6,19. Diarrhoea prevalence among dwellers is often dependent on household location; specifically households built in high altitude areas were less likely to experience diarrhoea6. In another study to estimate leptospirosis seroprevalence in American Samoa, Lau et al also found that altitude and location of backyard piggeries were significantly associated with leptospirosis seroprevalence19.
Lastly, the results demonstrate that the distance of under-five households to the river was statistically associated with under-five diarrhoea (p<0.05). In addition, a majority (80.0%) of under-five households with reported cases within 2 weeks were near the river (≤125 m), in comparison to those far (>125 m) from the river (20.0%). This significant difference was not likely due to chance (p<0.05). The results (OR=2.60, 95%CI: 1.21, 5.60) illustrate that children from households located near the river were 2.6 times more likely to experience diarrhoea. Children from households near the river were highly exposed to river pollutants. Other related studies also support this finding and argued that household location, such as distance to exposed areas like garbage dump sites and poor drainage areas, are influential factors for diarrhoea prevalence6,11.
Strengths and limitations
This is the first ever prevalence study in Honiara informal settlements and there are no previous studies or data in Honiara for comparison. This study is important for a number of reasons. First, it has identified the burden of diarrhoea among children (<5 years) in Honiara informal settlements and environmental factors that are associated with under-five diarrhoeal transmission. Second, it compares and discusses the recorded diarrhoeal prevalence rate (45.9%) with studies carried out in similar settings elsewhere in developing countries. Third, the study findings may be useful for strengthening policies and activities of the Health Promotion Department, other public health agencies, and other sectors with similar interests in identifying, managing and addressing public health determinants. In addition, it has added useful performance information to guide planners and policy-makers of the Solomon Islands Ministry of Health to tailor their future approaches according to the identified exposures, since water and food-borne disease reduction are among the Solomon Islands Ministry of Health national indicators.
There are some limitations in this study that need to be considered. The study was conducted in three informal settlements along the Mataniko River corridor, in Honiara, and therefore did not represent the entire population of children (<5 years) in Honiara’s informal settlements. There is also a limitation in the targeted age group (<5 years) since all age groups are at risk of diarrhoea.
The high prevalence rate among the Mataniko settlements may have been influenced by the time frame of data collection, which followed a national diarrhoea outbreak in Solomon Islands. The initial week of field data collection (household interviews) was carried out at least 4 weeks after the national diarrhoeal outbreak finished. For confirmatory purposes, the study needs to be repeated at several time points to exclude the possibility that the results were influenced by the previous outbreak.
In addition, courtesy bias may have been introduced due to the methodology of the study, and information bias may have resulted from personal knowledge questions. The study focused on diarrhoea occurrence, and did not consider different types of diarrhoea such as acute, watery or bloody diarrhoea in the analysis. The chance of over-reporting diarrhoea cases is high, because some symptoms of other childhood illnesses, such as anaemia, can overlap. The study directly involved primary caregivers instead of under-five children who were at a speaking age. This means that some practices of children, including the number of watery stools per day, can be over-reported by caregivers. In this situation there were no children around to verify the responses concerning them. Although other WASH facilities, such as water source, were classified as safe sources, due to limited funds, no microbiological and chemical analyses were conducted to determine the true quality of drinking water sources.
Conclusion
Diarrhoea is a major public health problem among children under 5 years in the Mataniko informal settlements, as indicated by a prevalence rate of 45.9%. Results showed that under-five diarrhoea is associated with the presence of stagnant wastewater, flies, solid waste and water-filled containers near households, plus the distance of under-five households from the river. To address these exposures, relevant programs and projects should be designed and implemented, especially in areas such as family planning, household economic empowerment and political commitment to a total WASH coverage initiative. Awareness and advocacy programs on environmental hygiene, food hygiene and potential health risks about the river should be ongoing at the community level.
Acknowledgements
We really appreciate the support rendered by the community leaders, key informants and research assistants (Philemon Tohunoni and Dudley Kunu). We thank the Solomon Islands Government as funder of this project and Mrs Sabiha Khan for her advisory input and encouragement. We also thank Professor Peter Crampton for valuable editing assistance.
References
You might also be interested in:
2017 - Gene therapy renews hope to lower the global rural sickle cell disease burden


