Introduction
Migrant farm or agricultural workers (MAWs) have formed a critical part of many rural economies for decades. In 1966, as a response to agricultural labour supply challenges, the Canadian federal government developed the Seasonal Agricultural Worker Program (SAWP), bringing workers initially from the Caribbean and, beginning in 1974, from Mexico for up to 8 months annually. In 2011, the Canadian government instituted a smaller, general agricultural stream of Canada’s broader Temporary Foreign Worker Program (TFWP), allowing workers to enter from any country with contracts of up to 2 years, with some additional MAWs through TFWP’s general streams for low- and high-wage positions1. These workers now include those from Asia, as well as other Latin American countries. Over 53 000 temporary foreign agricultural worker positions were approved in Canada in 2015, of which nearly 42 000 were through the SAWP2.
Social determinants of health figure prominently in MAWs’ lives3,4. Working conditions include physical hazards (eg outdoor physical labour using farm equipment), environmental factors (such as extreme heat, inadequate lighting, biting insects), farm chemicals (such as pesticides and fertilizers), and mechanical hazards (farm machinery on rough terrain and unsafe transportation), which heighten their risks of specific occupational injuries and illnesses5-7. However, unlike citizen farmers and permanent resident workers, MAWs are precarious workers8,9, under a managed labour migration program in Canada that renders them ‘permanently temporary’, compounding their vulnerability10. Studies in the Canadian and US contexts have demonstrated that MAWs are likely to experience a range of health outcomes: injury and illness from agrochemical and climatic exposures; musculoskeletal injury from repetitive motion, awkward postures, and lifting heavy loads; and motor vehicle and machinery accidents4,11,12. In addition, MAWs are required to live in employer-provided housing, which is typically on farms and is highly variable due to inconsistent application of housing regulations. Studies of migrant worker housing in Ontario and British Columbia have demonstrated numerous housing deficiencies, including insufficient food storage and cooking facilities, over-crowded and poorly ventilated dormitories lacking privacy, insufficient cooling and heating systems, and proximity to pesticides and fertilizers among many other concerns5,13, similar to those in North Carolina14. MAWs lack resources such as transportation4, common among poor people in rural settings. They also may lack dominant language communication capacity15, have different understandings of health and illness, and expect different healthcare treatment, all of which pose intercultural competency challenges to providing care16.
A substantial literature exists on rural health service provision to MAWs in the USA11,12,16-20. As is the case for other rural residents, access to health care, particularly specialists, remains an ongoing challenge for migrant and non-migrant farm workers alike21-23. Yet MAWs often face particular barriers to health and social services utilization11-13,15,24-27. In Canada, MAWs are eligible for provincial health coverage and workers’ compensation systems, and supplementary insurance benefits (for prescription drugs or physiotherapy, for example) are usually in contracts. However, processing delays occur, and health card access is a challenge for some: nearly 20% of 600 Ontario MAWs in one survey had not received their cards5. The SAWP and other TFWP streams create structural vulnerabilities and additional barriers to accessing healthcare systems among MAWs13,25,28. For example, MAWs may not take time off work when sick or injured due to fear of loss of current or future employment or wages. In a survey of approximately 600 MAWs in Ontario, 45% reported working despite illness or injury for fear of telling their employers, and 55% worked in these conditions to avoid losing paid hours5. Indeed, under the SAWP, employers can terminate employment and return workers to their country of origin if MAWs refuse work for any reason, including for medical reasons29,30. MAWs, their families and their providers can encounter challenges of transnational coordination of care across different healthcare systems31,32, particularly when MAWs become ill and injured in Canada and are returned home with their condition not fully investigated, managed or compensated28-30.
Rural health professionals and health services may have limited preparation for responding to both the specifics of MAWs’ challenges and their complexity. They may have limited preparation in evidence-informed management of MAWs33,34 for the determinants of health, the particular health problems, and the range of structural challenges to care which MAWs present. However, unlike those serving other migrants, immigrants and refugees in the US20,35, Canada36, and Europe37, views of health professionals providing services to MAWs in Canada have rarely been documented. Hence, the research reported here asked ‘What are rural health professionals’ perspectives on health care for MAWs, both in sending countries and in Canada?’
Methods
Design
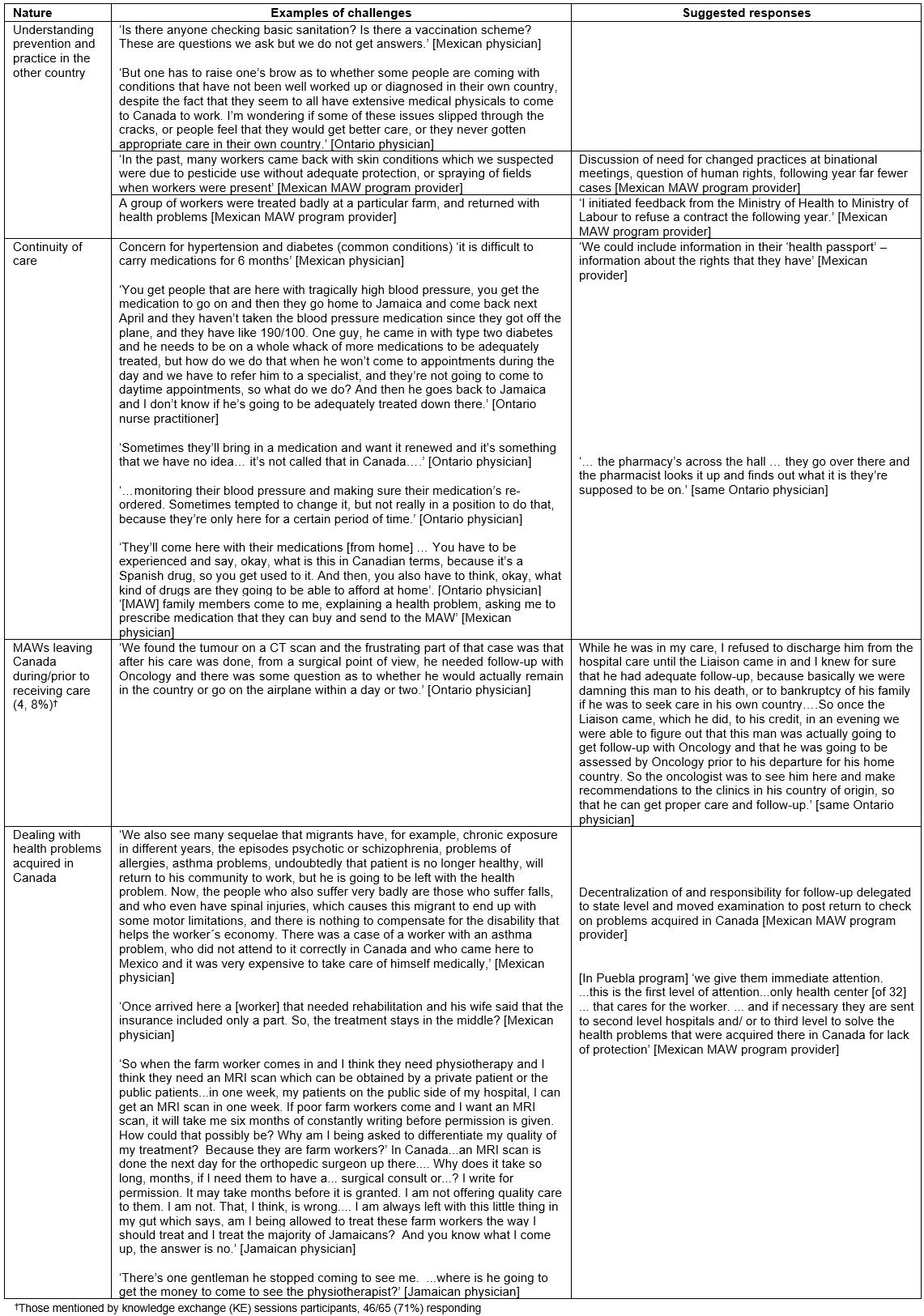
This research starts from the theoretical underpinnings of structural vulnerability38, which recognizes the social determinants of health, and the social structures that create systematic barriers to equitable health care for migrant workers. The researchers developed a qualitative design to tap the perspectives of healthcare practitioners responding to migrant workers in rural Southern Ontario. The critical realist, qualitative research design drew upon multiple methods to gather data, carried out by the authors (individually and in collaboration) over a 10-year period (Fig1). Below the authors comment on various aspects of this design in reference to key components of the ‘consolidated criteria for reporting qualitative research’ (COREQ) criteria for qualitative studies39.
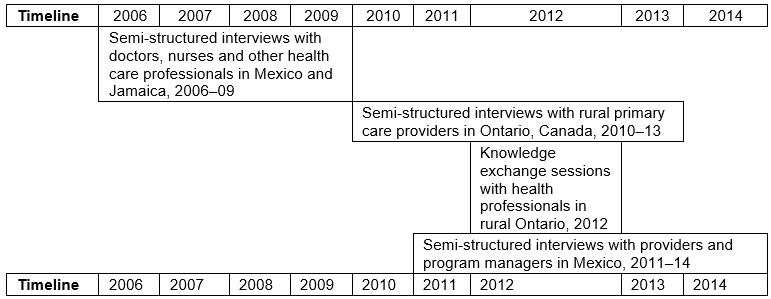 Figure 1: Timeline for data collection.
Figure 1: Timeline for data collection.
Research team
Lead project researchers included two interdisciplinary PhD social scientists (female), each with more than 15 years of qualitative and community-engaged scholarship with migrant workers in Canada. Other research team members were an occupational physician (male) and an occupational health nurse (female), each with extensive clinical experience with migrant workers, masters’ research training and respect among Ontario clinicians. Three authors are fluent in Spanish, having worked extensively in Latin America. Interviews were predominantly carried out by the research team members, with some Mexican interviews carried out by a male doctoral research assistant from Mexico. The research assistant received training in research ethics and interviewing and was provided an interview protocol and informed consent information for participants.
Interviews
Qualitative interviewing was the primary data collection method, allowing for an emphasis on health providers’ knowledge and perspectives. In keeping with semi-structured interview approaches, guides of open-ended questions with potential probes were developed for each set of interviews. Key questions-domains were similar, focusing on the challenges and particularities of providing care for the vulnerable population of migrant workers, including access to health services and workers’ compensation processes. Questions were added according to experience-expertise of the interviewee, given their different roles and national contexts. Interview guides were not formally piloted, but were iteratively adapted to ensure comprehension and responsiveness to interviewee concerns and insights. Interviewers had flexibility in order of questioning and extent of follow-up probing, but were careful not to frame the latter in a leading fashion.
Potential interviewees were discussed among research team members and purposively selected based on role and experience, with supplementary suggestions emerging from interviewees. Interviewers approached potential interviewees by phone or email and arranged the interview in a mutually convenient location, usually the clinician’s office. Some proposed interviews were unable to be concretized due to logistical challenges, but no potential interviewees refused outright. In total, 43 interviews were carried out with healthcare practitioners across the three countries, with no repeat interviews. During 2006–2009, co-investigator JM conducted semi-structured interviews in person with doctors, nurses and other healthcare professionals (n=24) who administer health examinations as well as provide care to migrant workers before they leave from and/or return to Mexico and Jamaica, as well as those who provide care to workers while in Ontario4. As part of investigating transnational aspects of care for MAW in a second project, additional interviews were carried out in 2010–2012 with primary care practitioners in Mexico and Jamaica (n=12) and with health professionals in Simcoe, Norfolk county, Ontario (a top receiving area for MAWs) (n=7)40. The interviews in Canada and Mexico were carried out in person, while the Jamaican interviews were conducted over the phone. The Canadian interviews were conducted by a Canadian physician, the Mexican interviews by a Mexican doctoral student research assistant, and the Jamaican interviews by one research team member (JM). All were conducted in private settings, usually the providers’ office, with no other individuals present. Interviewees in Mexico and Jamaica were referred to researchers from consular and Ministry officials and from migrant workers undergoing treatment. Although interviewees covered a range of genders and years in practice; only health professional role and province/country have been used in identifying interviewees to maintain anonymity. Interview duration was between 30 and 90 minutes, depending upon health professional availability and engagement. In all interviews, detailed notes were taken, and most interviews were transcribed verbatim, while some were partially transcribed for pertinent quotes only. Mexican interviews were conducted and audio-recorded in Spanish by bilingual researchers, and later translated into English for analysis.
Initial data analysis of the interviews occurred as interviews were conducted by the lead social scientist researchers with NVivo v7 (QSR International; https://www.qsrinternational.com/nvivo/home). Listening to audio-recordings, reviewing notes and reading transcriptions enabled a focus on relevant content areas (such as access to services and emerging themes, and language challenges). This iterative process informed judgements of saturation in each wave of interviewing: when no new content areas or themes emerged, additional interviews were not sought out. Subsequent coding incorporated the theoretical perspective on structural vulnerability.
Knowledge exchange sessions
In addition to these interviews, 20 knowledge exchange sessions were held with health professionals in Southern Ontario communities at hospitals, medical schools and medical clinics serving MAWs as part of a third project. These professionals were recruited through a sampling strategy that identified rural areas with high proportions of migrant workers in Southern Ontario, as well as with medical trainees (eg medical students) at surrounding medical schools. Sessions were held in the Ontario regions of Brant, Chatham-Kent, Essex, Haldimand-Norfolk, Hamilton, Middlesex, Niagara, Simcoe, Toronto, and Waterloo. Researchers contacted healthcare practitioners in these regions directly in order to seek participants, and referrals to other potential participants were solicited following a snowball approach. Participants were actively recruited by email and phone calls, and personal contacts were made with primary care and rural hospital providers, who advertised the sessions with staff and colleagues. Sessions were set at convenient hours and locations, and refreshments were served.
At the beginning of the sessions, informal knowledge testing questions, prior to the introduction of relevant material, were designed to obtain a baseline qualitative assessment of participants’ knowledge of, sentiments about, and experiences with healthcare and workers’ compensation access for migrant workers. Presenters took notes, and fielded questions and concerns expressed, recorded feedback on the presentation format and content, and developed an understanding of participants. At the close of each session, self-administered anonymous questionnaires gauged respondents’ perceptions of barriers to healthcare services and ways of overcoming them (n=65). The questionnaire assessed what participants had learned from the presentation, and obtained their perspective on what ways care or practices could be modified in response to migrant worker health issues and challenges accessing health care and compensation. Additionally, open-ended qualitative sections of the questionnaire gathered further qualitative information on possible improvements, concerns and questions.
All responses were entered into Excel worksheets by a research assistant and then checked with hard copy questionnaires by an author for accuracy and reliability. The 65 survey respondents worked in community health centres (24%), followed by acute care hospitals (21%), public health units (18%), and family health teams (8%) (other and unspecified 29%). Of these, the largest proportion were nurses and nurse practitioners (n=24, 38.1%), physicians (n=7) and administrators/managers (n=9), with a wide range of other health providers (n=12) (n missing=13). Most respondents reported seeing at least some migrant workers, with 42% of respondents seeing more than 20 migrant workers over their careers.
Analysis
Across primary sources, a framework analysis approach41,42 was used, informed by the literature, clinical experience and earlier research by the authors. The framework method of analysis is most suitable for analysis of multiple and disparate sources of interview data, and provides a well-structured overview of summarised data, which has guided interpretation of the study’s findings.
Based upon these orientations and the literature cited, data from each primary source was integrated into a database and then coded into three high-level nodes related to structural factors, which emphasized the contexts of the temporary migration program and the Ontario healthcare system; intercultural factors, which emphasized the factors related to language and cultural differences for migrant workers; and transnational factors, which reflected the experiences and challenges related to providing care to a group of patients who move transnationally from year to year. Using the framework approach, interview excerpts were coded into these three categories and then interpreted and discussed with specific reference to quotes and phrases employed by respondents. Findings were then consolidated into four tables (Supplementary tables S1–S4). Data were triangulated across data sources in order to strengthen the validity of findings. Co-consultation across authors, joint narrative writing, and iterative revisions produced the synthesis.
Ethics approval
Approvals for this research were through research ethics boards at the University of Toronto (Social Sciences, Humanities and Education (#18873) and Wilfrid Laurier University (#2865 and #2388).
Results
Good workers, poor patients? How structures of international labour migration programs and healthcare services influence provision of care
Most rural health professionals deeply admired MAWs:
I think these people work extremely hard; it’s back-breaking work, it’s repetitive work. They’re up early hours, they’re to bed late. They never leave the farm, except for Friday evenings and Sundays, but even still, some of them are working seven days a week for many, many months. (Ontario physician)
… they’re very easy to deal with, probably because they’re motivated. They’re motivated to get better. They want to work – most of them – and they come in here and you know, they’re genuinely concerned about some issue and you kind of feel that you’re their only person that they can talk to, so you kind of feel you’re doing something useful … (Ontario physician)
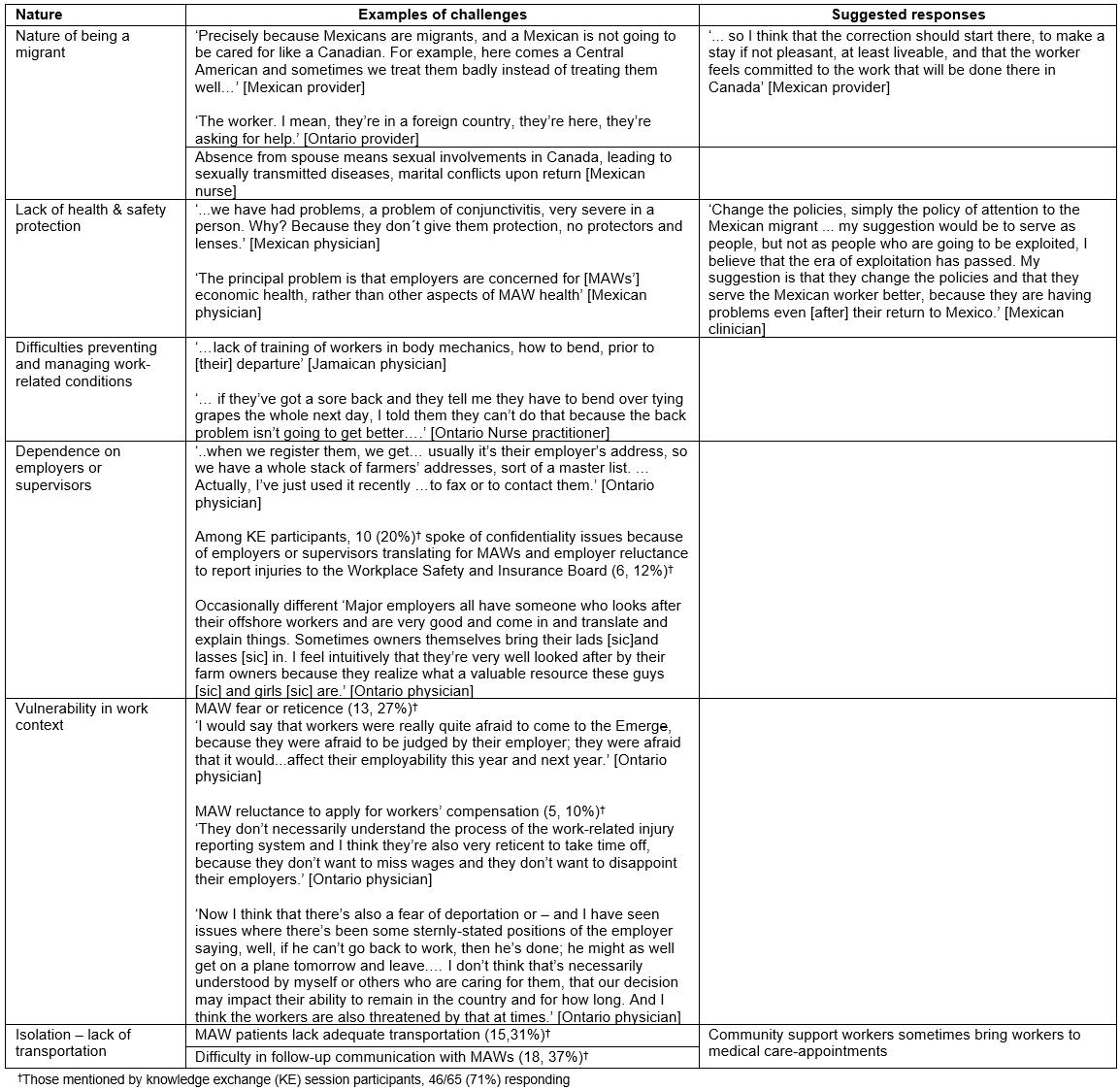
These health professionals faced a number of challenges providing care to MAWs (Table 1, with more detail in Supplementary tables S1,S2). Responses to these challenges (Table 2) were limited in the face of the structures of the migration program and health services. As one Mexican health professional noted for migrants, ‘… a Mexican is not going to be cared for like a Canadian’.
About half of knowledge exchange session participants understood that migrant workers were eligible for provincial health insurance, but only a third understood that migrant workers were eligible for workers’ compensation, with the remainder responding ‘no’ or ‘unsure.’ Health professionals noted the numerous barriers that MAWs face accessing care, with one Ontario physician commenting, ‘they wouldn’t see a doctor unless they’re very sick’. In rural Ontario, healthcare facilities are often long distances from farm residences and workers normally lack independent transportation (Supplementary table S1), only going into town on Friday evenings or weekends. In some cases, volunteer community support workers, bilingual co-workers or supervisors facilitate healthcare access for MAWs. However, most often transportation is provided by employers, whose involvement in medical consultations raised concerns about privacy and confidentiality (Table 1), including the use of medical information by consular officials (whose roles include mediating concerns between SAWP workers and their employers and arranging repatriation of workers). For example, when speaking about a health form requested by a consular official, one doctor explained, ‘I don’t really even know what that form is for. All I know is, I have to fill it in.’ MAWs’ concerns about jeopardizing current or future work in Canada, and fears of their employer or consular officials learning of their health problems, and ultimately leading to deportation if unable to work (Tables 1, Supplementary table S1), were noted by several Ontario rural physicians.
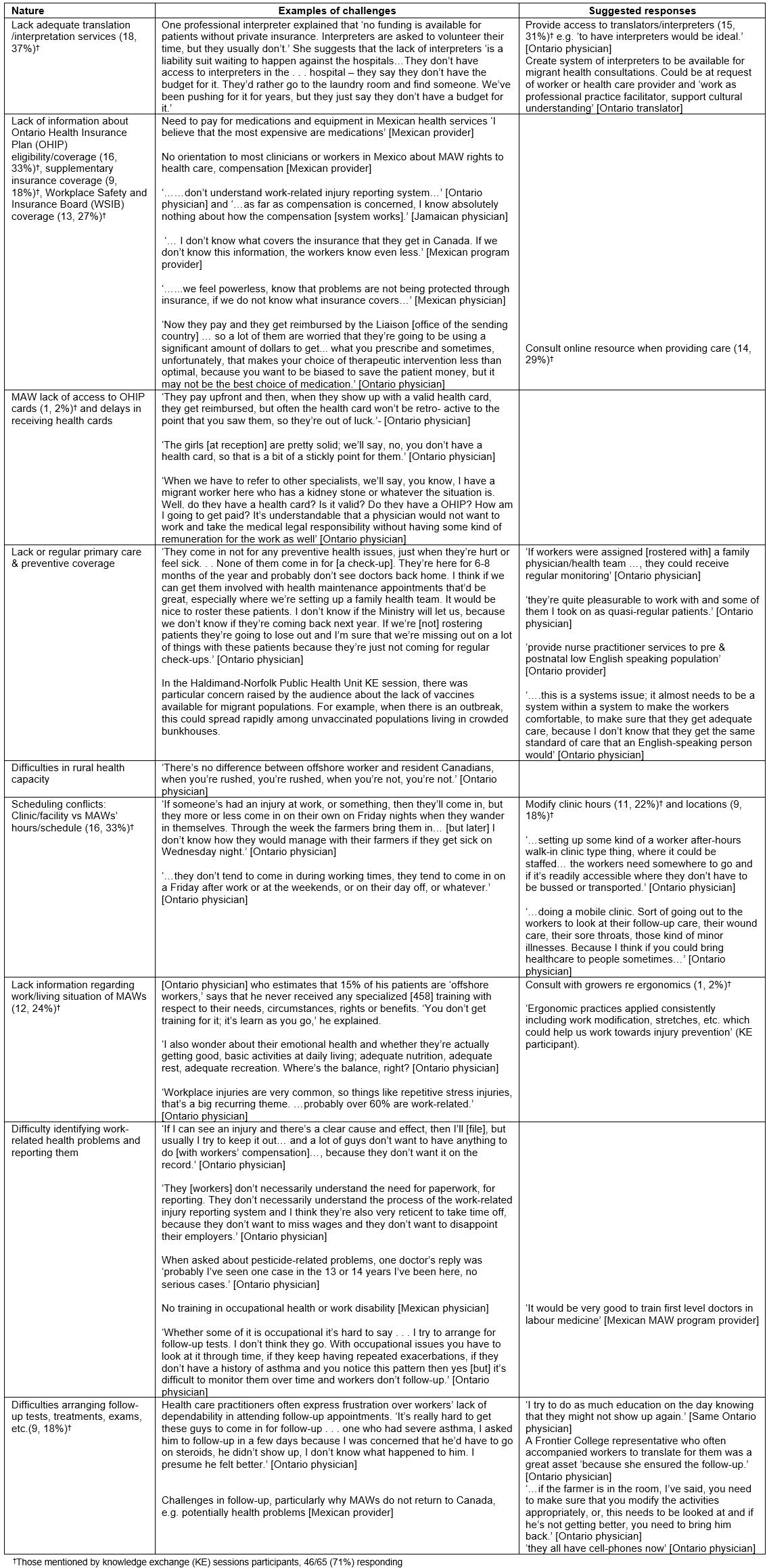
MAWs’ lack of insurance and/or health insurance cards at the beginning of the season impedes access to healthcare services, particularly specialists, and may limit investigations and treatment options (Tables 1, Supplementary table S2). Although a few rural physicians took on MAWs ‘as quasi-regular patients’, others argued for formal, continuous rostering of MAWs so that they could be regularly monitored each season in a primary care setting. The mismatch between when MAWs could get into town to see a health professional and most providers’ hours was a recurrent challenge, often resulting in workers seeking care at over-burdened rural emergency departments (Table 1, Supplementary table S2). Suggestions included modifying clinic hours (11, 22% of knowledge exchange participants); for example, one Simcoe clinic and pharmacy stayed open later on Friday nights when workers are typically bussed into towns in order to buy groceries, send money home, etc. Others suggested modifying locations (9, 18%), including mobile clinics to farms (Supplementary table S2).
Diagnosis of work-relatedness of diseases, such as asthma, which often required additional testing and follow-up, was difficult with MAWs (Supplementary table S2). Among Ontario physicians who were aware of workers’ entitlements to workers’ compensation, most indicated that they would offer to complete the required forms for a clear workplace injury. In more ambiguous cases, they would be less likely to do so, often because of the preference of workers, out of fear or pressure from employers, not to file a claim. Responses (Supplementary table S2) included education on the first visit, community volunteers who ‘ensured the follow-up’, and involving employers in work modification ‘and if he’s not getting better ... bring him back’ (Ontario physician).
Table 1: Overview of challenges perceived by health professionals serving migrant agricultural workers† 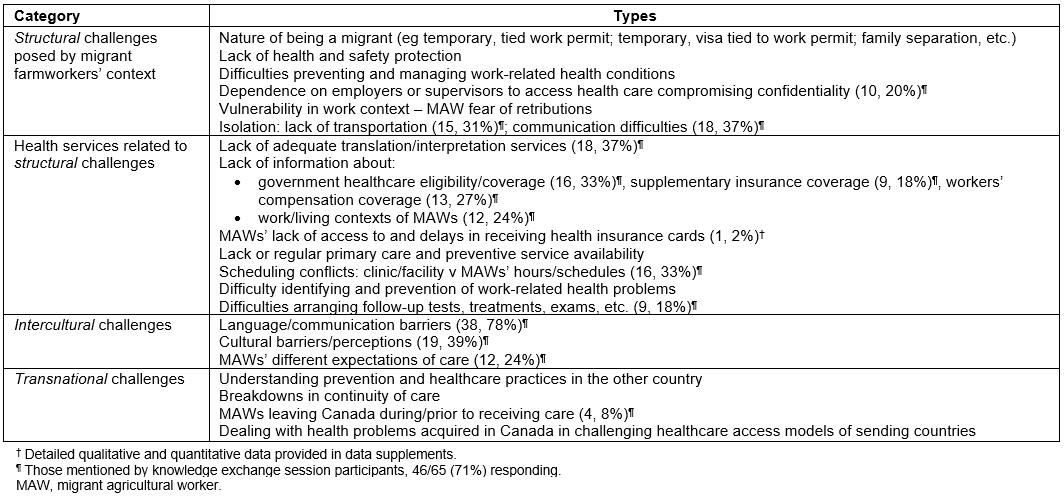
Worlds apart: intercultural challenges, knowledge gaps and responses
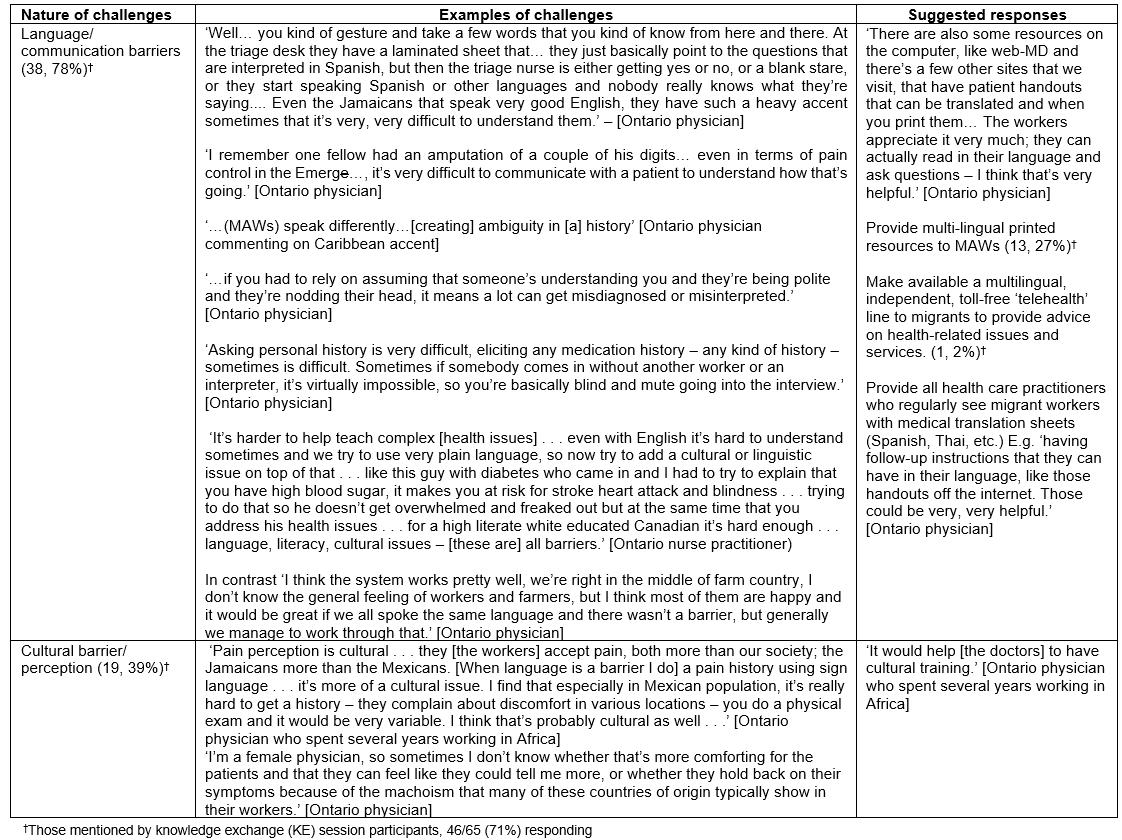
Communication barriers and knowledge gaps were the most commonly expressed challenge in knowledge exchange sessions with Ontario rural health professionals, particularly for English-only providers (the vast majority) serving Spanish-speaking MAWs (Table 1, Supplementary table S3). Challenges in mutual comprehension included language and accents for several Ontario physicians, and comprehension or literacy, including for a Jamaican physician: ‘Farmworkers are mostly illiterate, do not understand, even me sometimes. … Education level is a big barrier’. None of the rural Ontario health professionals had a regular translation service, so providing access to translators/interpreters (Supplementary table S3) was a priority for knowledge exchange participants (15, 31%). Multilingual resources, both printed and telehealth versions, for MAWs and health professionals were also mentioned as desirable (Supplementary table S3).
Some health professionals identified ‘cultural issues’ as challenges (Supplementary table S3). Different interpretations of illness presentations between MAWs and health providers were noted (eg around pain and bodily discomfort with mental distress). MAWs’ different expectations of care and treatment often reflected common practices in their countries of origin, such as injections in Mexico4.
Providers’ limited knowledge of MAWs’ work/living contexts and contractual situation posed difficulties in identifying and managing work-related health problems (Supplementary tables S1,S2). Mexican health professionals noted the need for training of primary care providers in occupational health (Supplementary table S2). Given the burden of musculoskeletal problems, Mexican, Jamaican, and Ontario providers encouraged training in ‘Ergonomic practices applied consistently including work modification, stretches, etc. which could help us work towards injury prevention’ (knowledge exchange participant). Health officials in Mexico noted that they instituted education sessions, which include some limited information about workers’ health-related rights and entitlements, primarily focusing on issues such as sexual health, nutrition and substance abuse. Many providers, particularly in sending countries, were unaware of Canadian workers’ compensation systems.
Care across borders: transnational challenges and responses
Both sending-country and Canadian rural providers had difficulty understanding preventive practices in the other country, for example sanitation and personal protective equipment when spraying pesticides in Canada among Mexican providers, and screening for conditions in Mexico among Canadian providers (Table 1, Supplementary table S4). A Jamaican physician bemoaned the lack of provision of training in body mechanics. Some Mexican providers critiqued the exploitation of MAWs, arguing that the ‘era of exploitation has passed’ and policies (particularly around providing greater protections and care to migrant workers) should be changed. They reported raising concerns with their Ministry of Labour and at binational meetings to correct deficiencies (Supplementary table S4).
Chronic conditions such as hypertension and diabetes presented challenges to continuity of care due to differences in medication names and availability, leading families in Mexico to request medication for a MAW in Canada from Mexican providers (Supplementary table S4). Further, MAWs would not always have sufficient funds to continue treatment started in the other country. When MAWs had to leave Canada prior to receiving full diagnostic workups and/or treatment, Ontario providers faced tough decisions about whether and when to approve a patient as fit to travel back to their country, and with what consequences (Supplementary table S4). One Ontario physician refused to discharge a patient with a newly diagnosed cancer until the worker, the specialist and the consulate official had laid out a plan of care and follow-up in the sending country. On the receiving end, Mexican providers complained ‘… that the migrants come with a problem from Canada that they are trying to solve here’. Both occupational conditions and sexually transmitted infections were mentioned. While clinicians identified the significant contribution of occupational factors to presenting health conditions and the need for preventive activities, no pathways for these were identified at the clinical level. A Jamaican physician was frustrated by the delays in approval by Canadian workers’ compensation authorities for investigations (eg MRIs) and treatments (eg physiotherapy). Mexican providers described shifting MAW screening to post-migration, decentralizing the services, and improving coordination of care with state health services to better manage MAW health problems. However, they noted that travel, equipment, medications, and treatments are often not fully covered by state health services, supplementary insurance, or workers’ compensation, leaving workers’ families to pick up the costs if they could (Supplementary table S4).
Discussion
Health professionals, working in sending countries and Canada, demonstrated substantial understanding of the complex challenges involved in providing care to MAWs in rural settings. As per Fennelly’s work35, the importance of ‘listening’ to rural providers’ experience as reflective insiders, in order to articulate better the challenges that they face and the opportunities for improvement, is clear. Much prior work has emphasized the views of health professionals in high-income countries (eg European providers grappling with competencies for addressing ethnic and cultural diversity)43. Previously, only Holmes20 interviewed providers in rural areas of both a sending country (Mexico) and a receiving country (USA). The present findings echo those of Holmes on the challenges that rural health providers grapple with in order to even partially address the social determinants of MAWs’ health within rural health services facing their own structural constraints. Recognizing the potential for feelings of powerlessness, as voiced by a Mexican physician in this study, is particularly important given the sometimes overwhelming nature of structural constraints, with providers feeling ‘caught in the same web’44.
However, in contrast with Holmes’ work on rural health service provision to irregular migrants, interviewees in the present study described potential for joint sending–receiving country governance mechanisms to address some of the challenges (Table 2)15. Suggestions for joint social protection have included ‘agreements between the Canadian insurers (Ontario) and the home country social security scheme’45, but few models of social protection agreements pertain to health46, particularly for migrants labelled low skilled47. Such a transnational perspective is increasingly germane as those with chronic conditions cross borders48 and health burdens accrued in one country fall upon another. Babe, I Hate to Go is a film about one such Jamaican worker diagnosed with cancer in Canada49. Ullman et al also documented different health burdens among rural Mexicans returning from the USA50. Such added health burdens pose challenges for MAWs and their providers, particularly in rural areas with limited access to care and medicines51, despite other improvements in health systems52. As Stan noted, the practice and governance task is to negotiate adequate health care for MAWs in an emerging ‘healthcare assemblage and citizenship regime in which patients’ movements across borders are closely interlinked with .… increasingly unequal access to public healthcare services’53.
Table 2: Towards continuity of culturally safe, transnational care for migrant agricultural workers 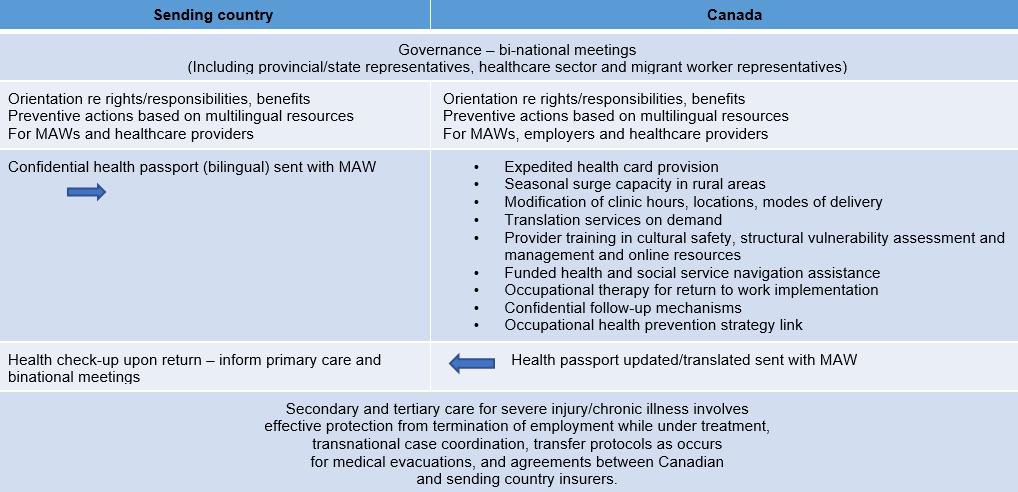
Limitations
Although this is the first study in Canada sharing rural health professionals’ perspectives, it had limited coverage geographically (only focused on the two largest MAW sending countries and the Canadian province where the largest numbers of workers are concentrated: Ontario) and professionally (focused on primary care versus a full range of specialties). Jamaican provider experience was inadequately covered with the few providers interviewed and primarily one sharing key insights. Although the data are 5–13 years old, little has changed in laws and programs that might affect MAWs’ structural vulnerability54. Innovative occupational and primary care services have been developed in some community sites (storefronts, churches, shopping malls) on Friday evenings and weekends55,56, but overall health care access and appropriateness has not substantially changed. Hence, the findings are still relevant, although substantial scope exists for further research, particularly transnationally.
Conclusion
A range of opportunities could enhance care for MAWs in rural Canada and in countries of origin. At the system level, health service delivery innovations could improve ‘fit’ between people and providers57. In the USA, funded migrant farmworker clinics exist in major rural agricultural areas and student-run community medical outreach approaches have been used58. Nurse-staffed cluster clinics for common conditions such as diabetes have been shown to improve MAW satisfaction with care59. Communication, access and follow-up challenges could be better addressed through budgeting for remote interpretation services60 and building on the work of care navigators61. Such responses could be amplified, building upon international examples of innovations to promote equity in primary health care62. At the rural provider level, training and resources for culturally safe approaches to health care63 could be expanded, in partnership with health professionals from the top MAW sending countries (eg Mexico and Jamaica, in the case of Canada). Other strategies include adaptations of existing guidelines for particular health problems, such as Kirmayer et al’s work on mental health64, implementation of tailored structural vulnerability assessment tools38, social prescribing initiatives65, and sharing of online resources on conditions and benefits for MAWs specifically66. The rewards in treating MAWs, expressed by interviewees in Holmes’ work and in this study, are important resources for innovation, although funding and support to rural health services overall will have to increase to ensure implementation.
Acknowledgements
The authors acknowledge participants, research assistants (Aaraon Diaz, Andres Furet, Eduardo Huesca, Pauline O’Connor, Lisa Stadelmayer), physician colleagues (Mike Pysklywec, Ted Haines) and community partner (Industrial Accident Victims Group of Ontario).
References
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/5313/#supplementary