Introduction
Background
The presence of a stoma after bowel surgery is associated with morbidity, gastrointestinal symptoms and impaired quality of life (QoL)1-3. Problems related to stoma are common and have both physiological and psychological aspects4,5. Reversal of a temporary stoma seems to improve or restore several aspects of a patient’s QoL6. A large proportion of patients undergoing rectal cancer surgery receive either a permanent or a temporary stoma. It is well documented that about 20% (9.5–27.5%) of temporary stomas are never reversed7-9. Large tumour size and anastomotic leakage seem to be the most common risk factors for this non-reversal7-9. If not reversed, a temporary stoma, and the problems associated with it, becomes unintentionally permanent.
Besides stoma-related morbidity, reversal of a temporary stoma is accompanied by complications such as small bowel obstruction and stoma site hernia10-12.
Some stomal complications, such as parastomal hernia, stenosis, retraction and prolapse, may require surgery. Problems primarily not requiring surgery, such as leakage from the stoma and skin problems, are also frequent13,14. The most common channel for medical advice on stoma-related problems is through a specialised stoma nurse15.
Since cancer recurrence has improved considerably16,17, QoL has become increasingly more important as an endpoint of quality after surgery. As a tool for assessing and comparing problems and QoL, validated questionnaires specific for colorectal cancer have been developed and used in many countries18,19. These questionnaires are named after the organisation responsible for their creation: the European Organisation for Research and Treatment for Cancer (EORTC). Such instruments are essential for the understanding of a patient’s life situation from their perspective.
Sweden has a nationwide rectal cancer registry: the Swedish Rectal Cancer Registry (SRCR)17. The latest validation of this registry showed a completeness of 99%, and data from this registry are considered to be population-based20.
The county of Västerbotten in Sweden is a large and sparsely populated area. Competence regarding stoma-related problems and problems related to the possible complications arising from a reversed stoma is restricted to hospital-based stoma nurses and surgeons. At the time of this study, colorectal surgery and specially trained stoma nurses were only present at two general hospitals located on the coast. A third district hospital located in a town in the sparsely populated western part of the county did not have these resources. In the remote western part of the county there are six municipalities lacking their own hospital, instead relying on their general practitioner (GP).
Almost 200 000 of the total Västerbotten population of 269 000 live in two coastal towns, leaving 69 000 inhabitants in 13 smaller municipalities21. Distance to the nearest hospital can be as much as 300 km for a patient living in the most remote western areas.
Educating patients about their stoma seems to improve QoL22. This is usually carried out by a stoma nurse at the hospital, but there are none in the rural areas. There is reason to believe that a longer distance to hospital and the absence of a specialised stoma nurse negatively affect the QoL of rectal cancer patients receiving a stoma at index surgery. In Sweden, healthcare legislation requires care on equal terms for the entire population23. Studies evaluating QoL of patients in different geographic areas are therefore of importance to achieve this goal. The effect of distance to nearest hospital on QoL in rectal cancer patients has not been studied previously.
Objective
The aim of this study was to investigate the impact of distance to nearest hospital on QoL in rectal cancer patients receiving a stoma at index surgery in Västerbotten county, Sweden. The primary outcome was global QoL, measured by the score in the general EORTC questionnaire QLQ C-30. Secondary outcomes were scores for remaining symptoms or functional scales in the QLQ C-30 and the colorectal cancer-specific QLQ C-29. The authors analysed differences in scores of patients in rural and urban areas, and those with or without access to a stoma nurse. The hypothesis was that living further away from the nearest hospital or not having access to a specialised stoma nurse impairs global QoL after surgery for rectal cancer with a stoma.
Methods
Study design
This was a cross-sectional study. The article is reported following the STROBE statement24. Data on patients diagnosed with rectal cancer in Västerbotten county in 2007–2014 were retrieved from the SRCR, including patient characteristics, surgical details and tumour classification (TNM). All patients receiving a stoma at index surgery were included.
The study population therefore comprised patients with either a permanent stoma or a non-reversed temporary stoma, but also patients who had had their temporary stoma reversed. The choice to include both present and reversed stomas was made because problems also occur when a stoma has been reversed. Reversal of a temporary stoma may be accompanied by serious complications such as stoma site hernia and/or bowel obstruction. Such complications may well affect the QoL of patients for a long time after stoma reversal and these complications are, just as stoma-related complications, often managed by colorectal surgeons located far away from the patients living in rural areas.
All eligible patients were asked if they would be willing to participate in the study by mail. In cases of no response, a reminder was sent two further times. In cases where date of index surgery was missing, the date of diagnosis was used.
Variables
Global QoL and secondary endpoints were assessed using the validated EORTC questionnaires QLQ-C30 (version 3.0) and CR2925,26. QLQ C-30 assesses general QoL and contains 30 questions corresponding to one global QoL measure, five functional scales and nine symptom scales. QLQ CR-29 is disease-specific for colorectal cancer and contains 29 questions related to symptoms occurring after surgery for colorectal cancer, six of which are questions addressing defecation/stoma output, and one specifically regarding stoma care problems. The 29 questions correspond to five functional scales and 18 symptom scales. Four of the questions in QLQ CR-29 comprising sexual problems are gender-specific, two questions are addressed to female responders only while two questions are addressed to male responders only.
Answers from these questionnaires were converted to a score ranging from 0 to 100. The scores are based on responses graded 1–4 on symptom and functional scale questions, and 1–7 on the global QoL questions. A high score in functional or global QoL scale represents a higher QoL or degree of functioning. A high symptom score is negative. Scoring was done in accordance with the EORTC scoring manual27. All scores derived from the questionnaires were transferred to a database containing matched cases from the SRCR and from Statistics Sweden, providing patient characteristics and socioeconomic variables.
The socioeconomic variables comprised income and marital status at the time of diagnosis. Income was converted from the Swedish currency (SEK) into Euros (EUR) based on the exchange rate on the bank day closest to New Year’s Eve at the year of diagnosis28.
Addresses of the patients were collected from the medical records at the time the questionnaires were dispatched. Distances from home to nearest hospital were calculated using Google Maps™.
Statistical methods
Given the geographical nature of Västerbotten county, a choice was made to divide the investigation using two separate models: the effect of distance to nearest hospital by dividing the responding population in rural and non-rural, and access to a specialized stoma care nurse.
Model 1: After closely examining the map of Västerbotten, the authors assigned all responding patients living 76 km or more from the nearest hospital to the rural group. These patients live in municipalities lacking their own hospital and instead rely on their local GP/district nurse for assistance. The rest comprised the non-rural group, with easier access to specialised care.
Model 2: This model was used to assess the effect of access to a specialised stoma care nurse. The non-rural group in the second model comprised the population of the two coastal towns with access to both a stoma nurse and a hospital routinely performing colorectal surgery. The rural group in this model comprised patients from 13 sparsely populated municipalities covering an area roughly the size of Switzerland, where access to a stoma nurse is lacking. One of these municipalities has a district hospital with surgical competence and a nurse who works part-time with stoma patients. However, at the time of the study this hospital did not routinely perform colorectal surgery or have a specialised stoma nurse.
When differences were found between the groups in these two models, a subgroup analysis was performed ,separating patients who still had a stoma and those who had had their stoma reversed.
The conversion of answers from the EORTC questionnaires to the appropriate scale was done using SPSS v18.0 (IBM; https://www.ibm.com/analytics/spss-statistics-software). All remaining statistical calculations were performed using STATA v13.1 (STATACorp; https://www.stata.com). When comparing means and responses between the groups from the EORTC questionnaires, independent student’s t-test was used. When comparing the groups regarding a categorical outcome, a χ2 or Fisher’s exact test was performed depending on cell sizes (≤5 Fisher’s exact test, otherwise χ2).
Ethics approval
Ethics approval for this study was obtained from the Regional Ethics Committee in Umeå, Sweden (Dnr 2016/155-31). Written informed consent was obtained from all individual participants included in this study.
Results
Participants
A total of 462 cases of rectal cancer were retrieved from the SRCR. Of these, 217 patients were deceased, 57 never had a stoma, one had moved from Västerbotten and one was double-registered. Of the 186 eligible patients, 129 responded to the questionnaires, giving a response rate of 69% (Fig1). Median time between index operation and the first dispatch of the questionnaires was 5.1 years (range 659–3732 days).
The number of incomplete scales in the 129 QLQ C-30 forms varied between 0 and 2 scales per patient. Responses to QLQ CR-29 were similarly complete. One exception was the questions dealing with female sexual interest/symptoms, where answers were more frequently missing. Complete scales in female sexual interest and dyspareunia were received for 92% and 66% of respondents, respectively. This lack of response was not seen among male respondents, where scales were 97% complete for male sexual interest and 92% complete for impotence.
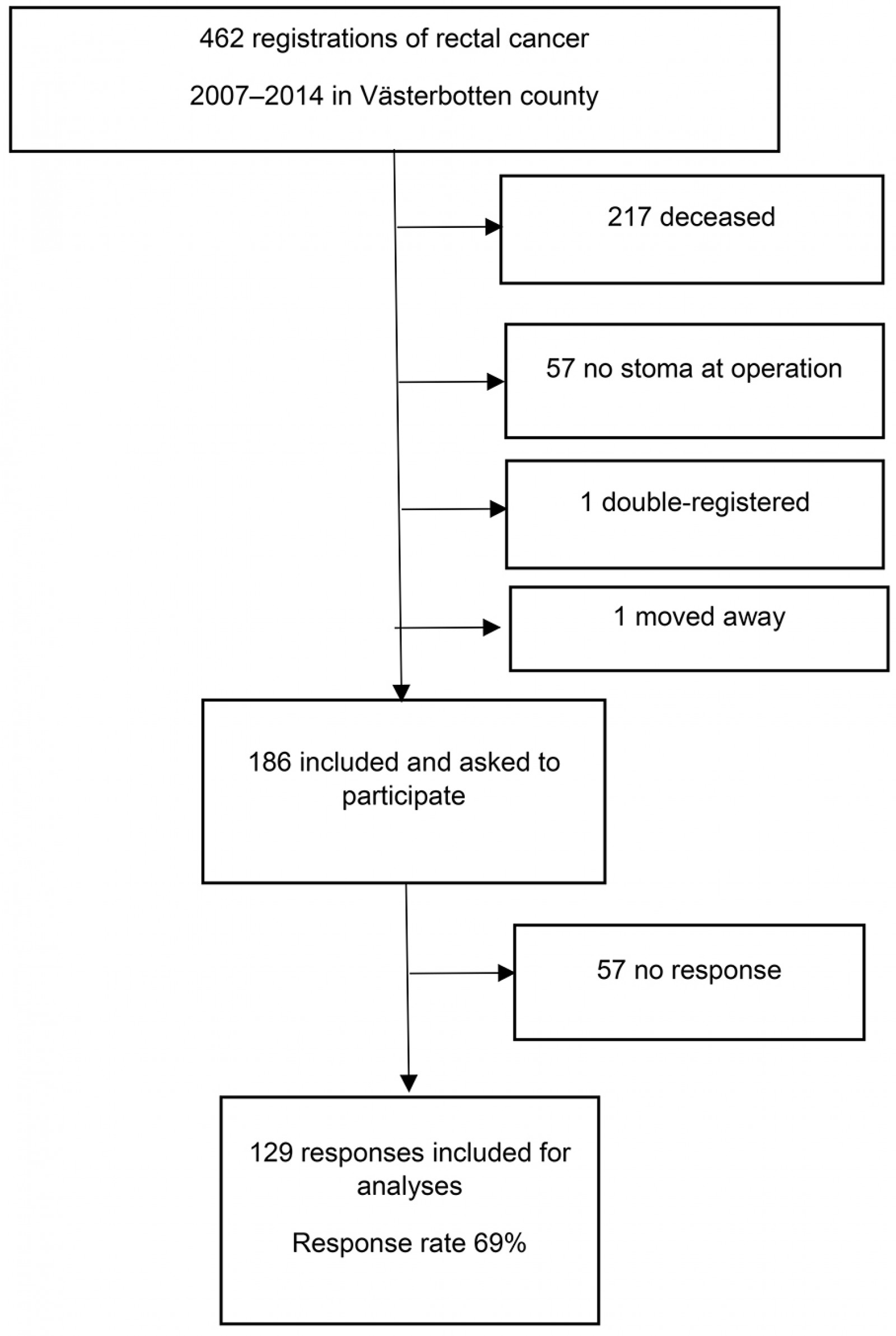 Figure 1: Flow chart of patients included in study.
Figure 1: Flow chart of patients included in study.
Descriptive data
The mean age of all responders was 66.3 years, and 59% were male. Of the 129 patients included, 65 received a permanent stoma and 64 a temporary stoma. Of the temporary stomas, 53 were reversed, giving a reversal rate of 83%.
In the first model, (travel distance to hospital <76 km v ≥76 km), there were no significant differences between the groups in patient or tumour characteristics (Table 1). However, a difference was seen in temporary stoma reversal rates, where patients living further away had a lower reversal rate than those living nearer to a hospital (Table 1).
In the second model (access to stoma nurse v no such access) a higher percentage of patients living in the two towns with access to a stoma nurse were married. No other baseline differences were seen between the groups (Table 2).
Table 1: Patient characteristics of the groups in the first model. Groups based on living further away or nearer than 76 km from nearest hospital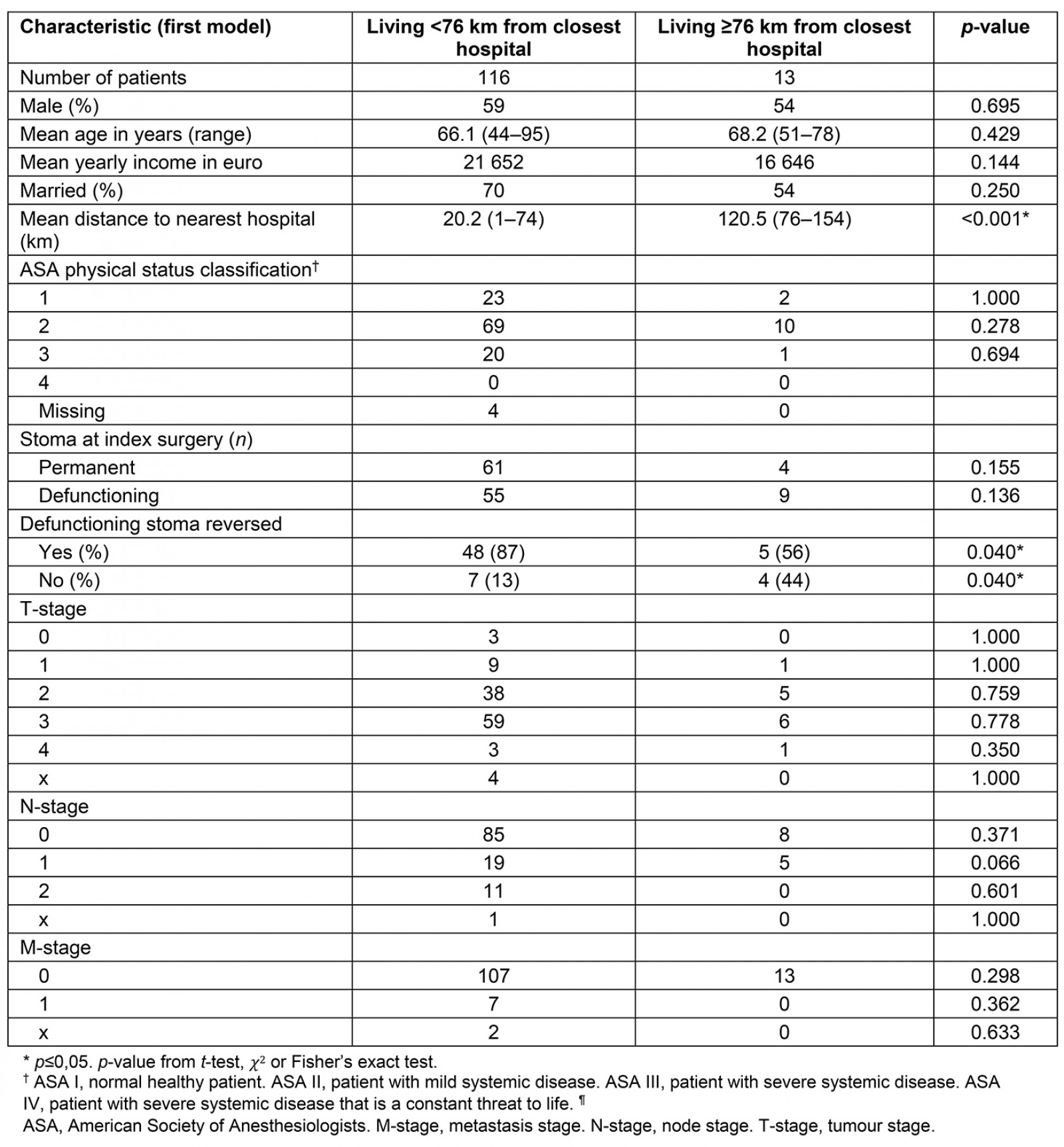
Table 2: Patient characteristics of the groups in second model. Groups based on living in a town with access to stoma care nurse or in a municipality with no such access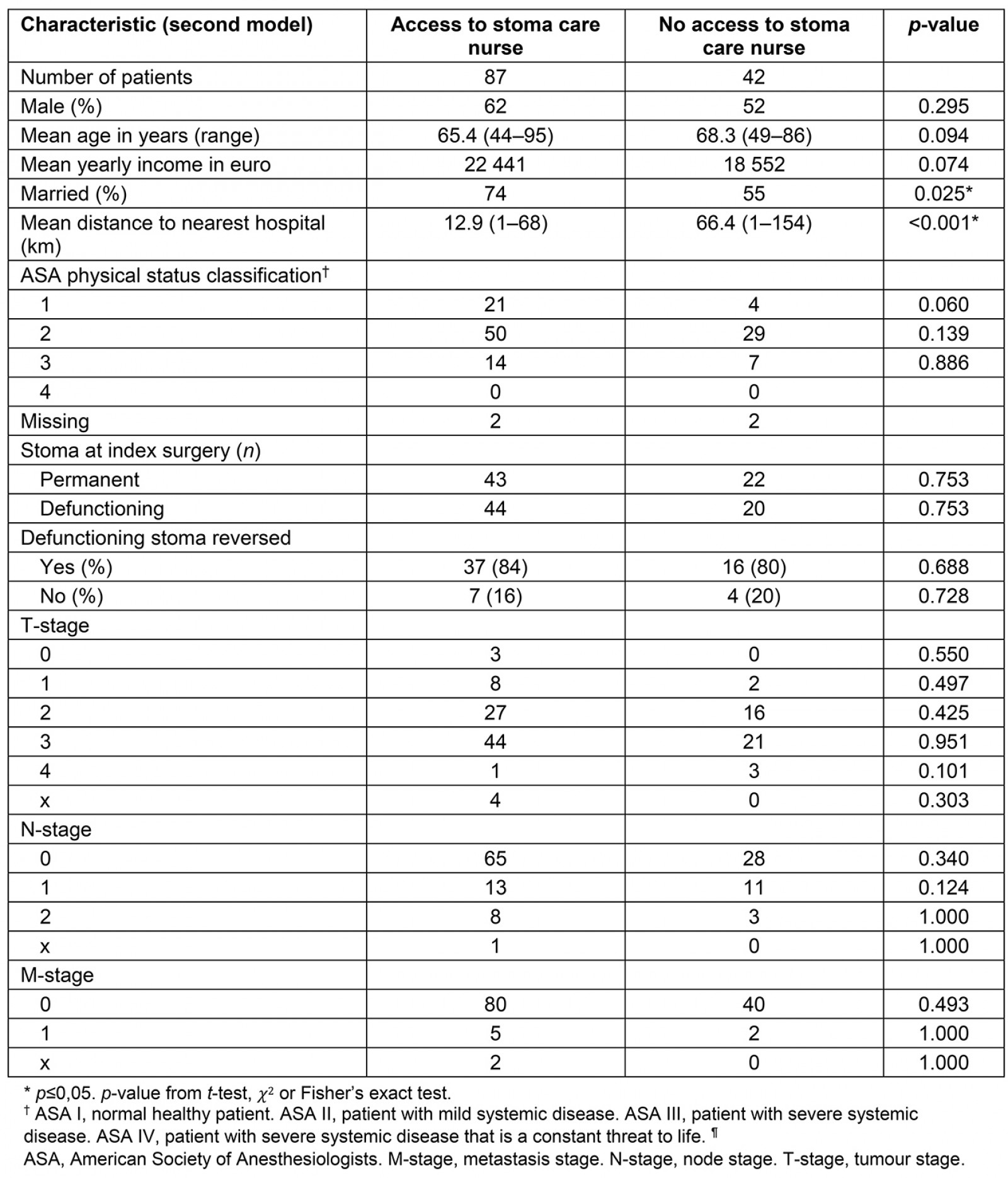
Main results
When assessing QoL in the first model (travel distance to hospital <76 km v ≥76 km), significant differences were seen between the groups. In the general QLQ C-30 form, the patients living further away reported significantly more pain, but no difference in global QoL (Fig2). The difference in pain score was 15.2 (p=0.032). In the colorectal-specific QLQ CR-29, the patients living further away reported significantly more sore skin and greater hair loss (Fig3). The greatest difference in score, 22.9, was seen for sore skin (p=0.004).
In the second model (access to stoma nurse v no such access), the responses to the general QLQ C-30 form were similar, and no significant differences were seen. When comparing scores from the colorectal-specific CR-29 in the second model, patients living in rural municipalities with no access to a stoma care nurse reported significantly more symptoms regarding dry mouth (p=0.038). Otherwise, no other significant difference was seen (Fig4).
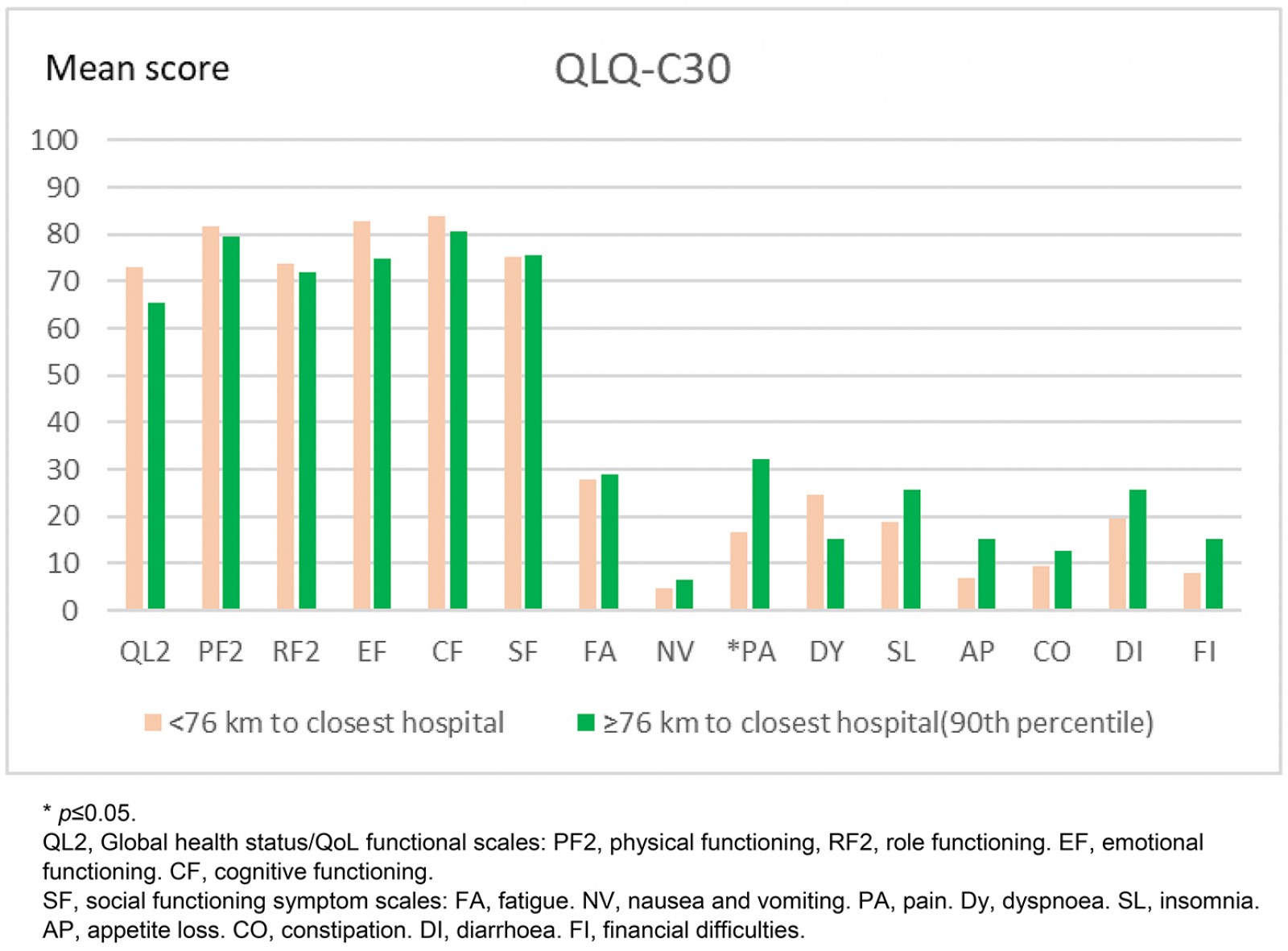 Figure 2: Differences in quality-of-life scores using the general QLQ C-30: living closer than 76 km from closest hospital compared to living 76 km or further away.
Figure 2: Differences in quality-of-life scores using the general QLQ C-30: living closer than 76 km from closest hospital compared to living 76 km or further away.
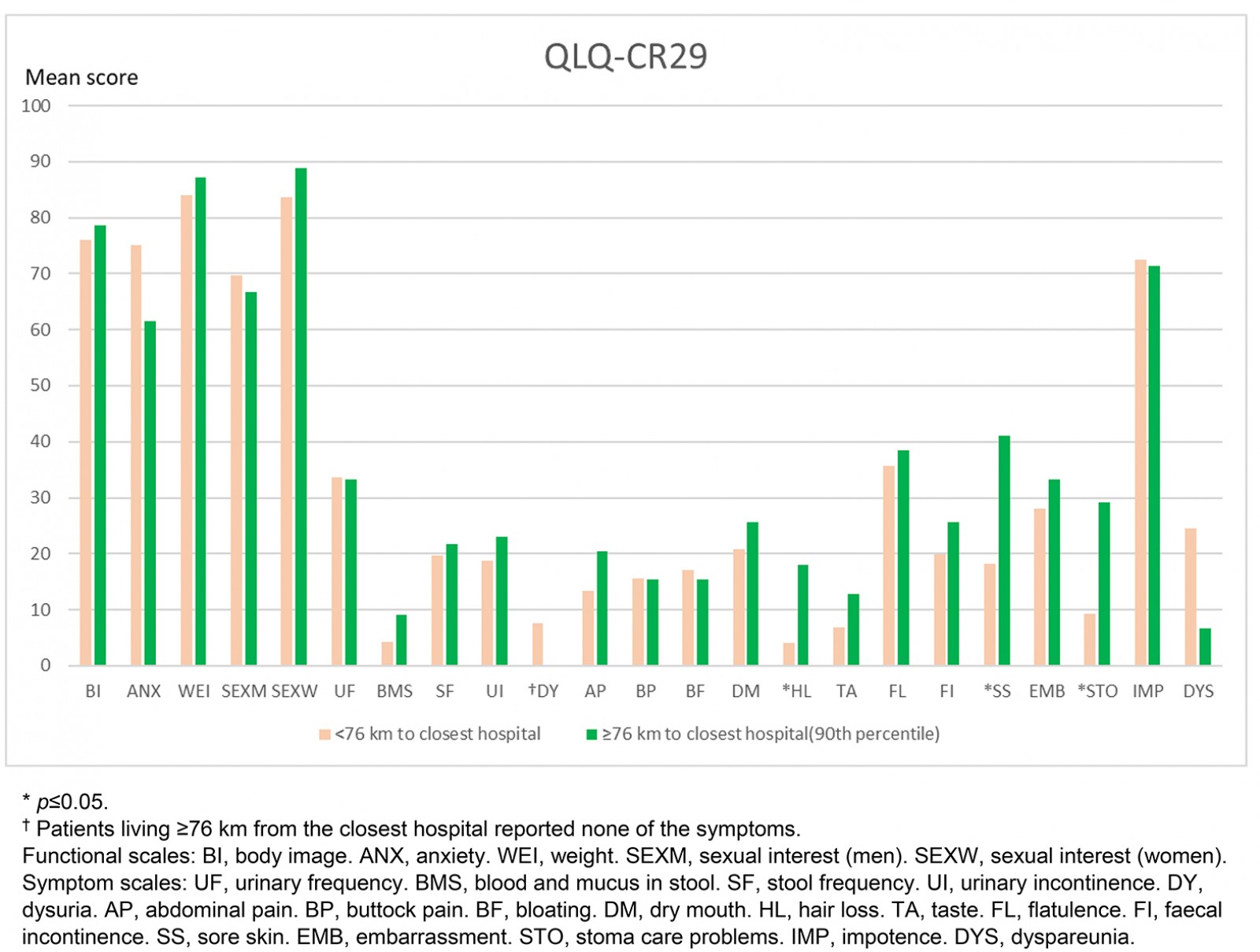 Figure 3: Difference in quality-of-life scores using the colorectal cancer-specific QLQ CR-29: living closer than 76 km from closest hospital compared to living 76 km or further away.
Figure 3: Difference in quality-of-life scores using the colorectal cancer-specific QLQ CR-29: living closer than 76 km from closest hospital compared to living 76 km or further away.
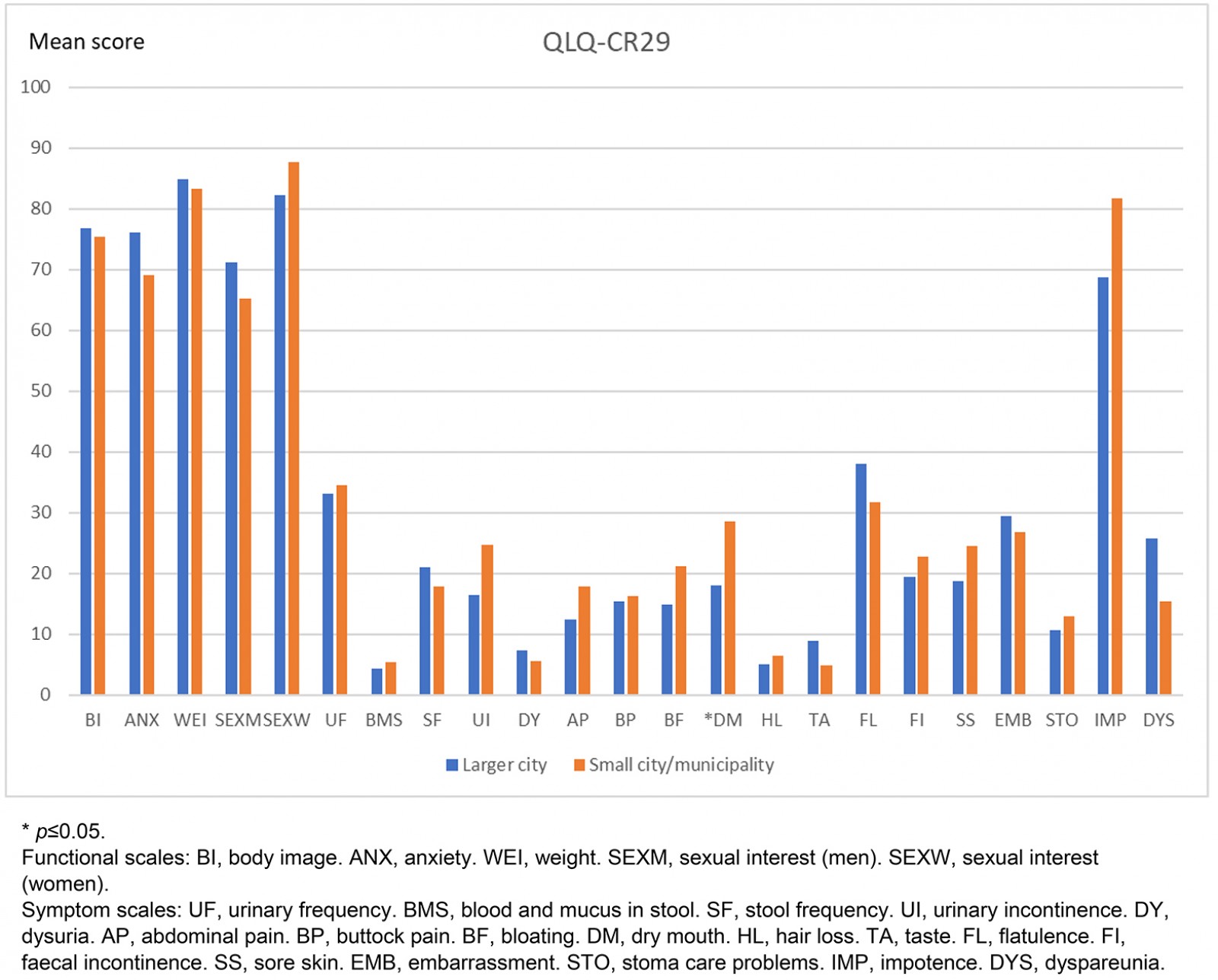 Figure 4: Difference in colorectal-specific quality of life score: living in larger city with access to stoma care nurse compared to small city/municipality with no such access.
Figure 4: Difference in colorectal-specific quality of life score: living in larger city with access to stoma care nurse compared to small city/municipality with no such access.
Other analyses
When performing subgroup analysis using the first model (travel distance to hospital <76 km v ≥76 km) separating patients who still had a stoma from those who had had their stoma reversed, further differences were seen for the patients who still had a stoma. In the general instrument, QLQ C-30, more pain was seen among patients living further away, as was seen for the entire group (p=0.005). The patients with a stoma who lived further away also reported a significantly poorer global QoL and higher stoma output (p=0.038 and p=0.047, respectively). The difference in pain score was 25.9 and 18.6 in global QoL score. In the colorectal-specific QLQ CR-29, a difference in sore skin was seen (p≤0.001) as for the entire group. Other than this, stoma patients living further away also reported significantly more stoma bag leakage, more bag changes and, overall, more stoma care problems (p=0.032, p=0.019 and p=0.004, respectively). The difference in score for stoma care problems was 19.9. When considering patients in the same model (<76 km v ≥76 km) who had their stoma reversed, no differences could be seen in the scores of non-stoma-specific questions.
Discussion
Key results
The major finding in this population-based study was that rectal cancer patients who received a stoma at index surgery and had a longer journey by road (≥76 km) to their nearest hospital reported significantly more pain and more sore skin than patients living less than 76 km from hospital. The authors did not find evidence for the hypothesis that a long journey to the nearest hospital has a negative impact on the global QoL of rectal cancer patients who receive a stoma at index surgery. However, subgroup analysis showed that living further away (≥76 km) did have a negative impact on the global QoL for patients who still had a stoma. These patients also reported more stoma care problems compared to those living closer. If the stoma was reversed, the negative effect on global QoL and scales not comprising stoma-specific questions disappeared and no significant difference could be seen between the groups.
However, the present results show that there were significantly more negative differences regarding pain and sore skin for those rectal cancer patients living further away who received a stoma at index surgery.
Interpretation
Patients living further than 76 km away from the nearest hospital are only to be found in the rural, sparsely inhabited western part of Västerbotten. The median time between index operation and the first dispatch of the questionnaires was 5.1 years. This means that most questionnaires were answered after the final follow-up visit at the surgeon’s office for rectal cancer according to the national guidelines (36 months). To help these patients, GPs are encouraged to routinely offer an additional follow-up visit to patients who live in a rural area and receive a stoma at index surgery, focusing on the individual patient´s problems.
Interestingly, the results showing significant differences between the groups came from the first model (travel distance to hospital <76 km v ≥76 km) and not the second (access to stoma nurse v no such access). This apparently incongruent result indicates that distance to nearest hospital, not lack of access to a stoma care nurse, is a barrier for the included patients to either seek or to obtain adequate help with symptoms in the follow-up period after rectal cancer surgery if a stoma was placed at index surgery. Danielsen et al concludes in two studies that structured patient education seems to have a positive effect on QoL22,29. Patient education in Västerbotten is mainly provided by a stoma nurse, but no such positive effect could be seen in global QoL in this study.
The greatest differences in score between the groups in the first model (travel distance to hospital <76 km v ≥76 km) were sore skin (22.9) and pain (15.2). A difference in score greater than 5 is considered clinically significant, and differences over 20 are considered ‘very much’ according to an article assessing the interpretation of these types of form30.
Together, these findings clearly indicate a geographical inequality leading to significantly more pain for rectal cancer patients living in a rural area who receive a stoma at index surgery. Rural patients with a stoma also reported more stoma care problems and an inferior global QoL. It is difficult to define a specific reason for this geographical difference. Baseline data in all groups were similar, which suggests that patient or tumour characteristics were not the reason. This leaves logistic inequality as being a probable cause.
The difference in reversal rate between the groups in the first model, where patients who had a longer journey by road (≥76 km) to their nearest hospital had a lower reversal rate obviously led to a higher proportion of non-reversed loop ileostomy in this group. The faecal content for an ileostomy is looser than that for a colostomy and is therefore more difficult to handle. This could be a reason why the stoma patients living further away reported higher stoma output and more bag changes. Furthermore, a large prospective study also showed that ileostomy is an independent risk factor for the development of major stoma-related complications such as parastomal hernia, prolapse and stenosis31.
Results from the subgroup analysis in the first model (travel distance to hospital <76 km v ≥76 km), showed that differences were mainly the result of patients still having their stoma. When considering this group alone, further significant differences were found. This suggests that as long as a stoma is present after rectal cancer surgery, rural patients report markedly more symptoms than those living closer to the nearest hospital. Besides experiencing disturbing symptoms, rural patients’ global QoL is affected negatively if their stoma is present, but not so when it is reversed.
Limitations
The design of this study does not provide a clear answer as to why the symptom scales in the questionnaires used gave markedly higher scores for pain and sore skin in patients living far away from the nearest hospital. Future explorative studies evaluating the living circumstances of patients in rural areas may provide an answer.
To the authors’ knowledge, no similar studies evaluating QoL based on distance to hospital have been made. However, a recently published article from members of the authors’ research group, also analyzing patients from Västerbotten county, found no effect of distance to hospital regarding the risk for emergency colon cancer surgery32. These results suggest that a longer distance to hospital has no impact on the quality of management of patients with colorectal cancer up to and including surgery. Instead, any difference in quality based on distance seems to arise in the follow-up period, a fact that decision-makers should be aware of in order to allocate resources in an appropriate way.
A strength of this study is the high response rate and the completeness of the responses. Herrle et al, who compared QoL in relation to stoma closure, reported a completeness of more than 95% for all scales not assessing sexual issues. In their study, however, only around 60% of men and 30% of women answered questions on sexual interest6. In the study, completeness of scales not involving sex was greater than 98%. Ninety-seven per cent of the scales on male sexual interest and 92% on impotence were complete, compared to 92% of women answering on sexual interest and 66% on dyspareunia. The relatively higher rate of completed questionnaires in this study is a strength and adds validity to the scores regarding sexual problems. The results were not affected by ongoing postoperative adjuvant chemotherapy, because the last patients included received their diagnosis in 2014 and the questionnaires were sent out during the spring of 2017. Chemotherapy otherwise constitutes a common confounder in studies evaluating QoL in conjunction with index surgery.
A weakness of this study is the size of the population. The small sample sizes reduce the power to detect group differences in QoL scores, which is an inherent weakness of performing such studies in small rural populations. However, finding a region in Sweden where the effect of distance to nearest hospital can be studied is difficult because the southern part of Sweden is more densely populated, and distance is usually shorter than the cut-off used in this study.
The generalisability of these results, however, should be good in other countries with a low population density and many patients living in remote areas, such as Australia, parts of Indonesia and northern parts of Scotland, Norway and Finland33,34.
There is indeed an overlap between the division in an urban/rural group and patients with/without access to a specialised stoma nurse in that some patients classified as urban do not have access to a specialised stoma nurse while none of the rural patients have access to that facility. One could argue that it would have been appropriate to use another statistical method to better illustrate the impact of distance (eg logistic regression). The choice to use the t-test in this study is motivated by the fact that the validation of the EORTC questionnaires has been done using student’s t-test. Furthermore, in the light of the distribution of patients between the groups described above, the additive value of such an analysis would be limited.
Even though patients who receive a stoma at index surgery and who live far away from the nearest hospital report more pain and skin problems, no differences were seen between the groups regarding global QoL. This suggests that, for patients living in rural areas, these perceived insufficiencies do not impair a patient’s experience of QoL in their daily life, or that other parameters outside the scope of this study compensate for these.
Conclusion
Rectal cancer patients who receive a stoma at index surgery and live in a rural area far away from the nearest hospital report a similar global QoL but suffer significantly more pain and more sore skin than those living nearer. These differences seem to be explained by patients still having a stoma as opposed to those who have had it reversed. Patients still having a stoma also report more problems with stoma care and poorer global QoL. Not having access to a specialised stoma care nurse did not explain the differences seen, leaving logistic inequality as a likely cause for the problems suffered by patients living far away from the nearest hospital.
Acknowledgements
Financial support was received by regional agreement between Umeå University and Västerbotten County Council (VLL-675981), grants from Lion's Cancer Research Foundation, Umeå University and Visare Norr. Peter Cox is acknowledged for help with the manuscript.
References
You might also be interested in:
2014 - Knowledge and perceptions of Chagas disease in a rural Honduran community