Introduction
In Brazil the primary healthcare model is organized through the Family Health Strategy (FHS), based on complete health care, with multiprofessional teams associated with the population of a given territory, focussing on the longitudinal reach of activities. It is considered the preferred gateway to the health system and is responsible for coordinating the healthcare networks1,2.
Family health team characteristics vary with location and have been the subject of several evaluations with different approaches. Such evaluations are important for evidencing different realities and can contribute to the preparation of planning that is more focussed on the needs of users, reformulation of the work processes of teams, reorientation of care arrangements, prioritization of actions by managers and better training for the new demands resulting from the social realities presented3.
In the different contexts and populations served by the FHS care arrangement, riverside populations are considered traditional in the Amazon region. These populations are characterized by groups located on the banks of small and large rivers, in homes planned for survival in times of floods and droughts4. The deficient infrastructure present in these communities and the geographic characteristics – alongside extreme climatic conditions, which often isolate them during floods and droughts, depending on the time of year – contribute to hinder the implementation and maintenance of health services for the population.
Among the numerous rivers of the Amazon region live riverine populations who, despite the wealth of the area, constitute vulnerable groups excluded from public goods, facing difficulties to access services such as health care and education, and basically living off fishing, subsistence farming, gathering of forest products and the federal government aid, called Bolsa Família4.
In the context already described, factors such as geographic accessibility, defined as the distance between the population and healthcare resources, and organizational accessibility, characterized as the way healthcare services are organized, constitute, in some cases, major challenges to be considered in the planning and implementation of the care provided5 and mainly in the organization of work processes.
Aiming to expand access and build models that could reach more inaccessible regions, the Ministry of Health instituted, through Ordinance 2191 (3 August 2010), two modes for municipalities to choose: the fluvial FHS (FFHS) and the riverside FHS, whose planning prioritized service for the riverside population of the Legal Amazon and Pantanal Sul-Mato-Grossense regions. Later, Ordinance 2488 (21 October 2011) provided new criteria for the planning of teams and Ordinance 2436 (21 September 2017) established the review of the guidelines for the Organization of Basic Care6,7.
Fluvial family health teams carry out their activities in fluvial basic health units, in boats or ships, and in riverside communities of the catchment area, while riverside family health teams work in fixed units in communities, with the possibility of moving the teams between rivers in smaller vessels7.
The mode chosen in this study to analyze the work process with riverside communities was the FFHS. Considering this goal and the few studies on fluvial family health, after reading studies on the work process and on the evaluation of primary health care in various contexts, the following research question was devised: how does the work process occur in the fluvial family healthcare arrangement in a municipality of the Amazon region?
Therefore, the study aim was to understand and analyze the work process of fluvial family health teams in the context of riverside populations.
Methods
Type of study
This was cross-sectional, qualitative research, with three FFHS teams as the empirical research field. The health work process approach8,9 as theoretical framework and the action research approach10,11 as methodological framework were used for this study (Fig1). The instrument used to guide the methodology was the Consolidated Criteria for Reporting Qualitative Research12.
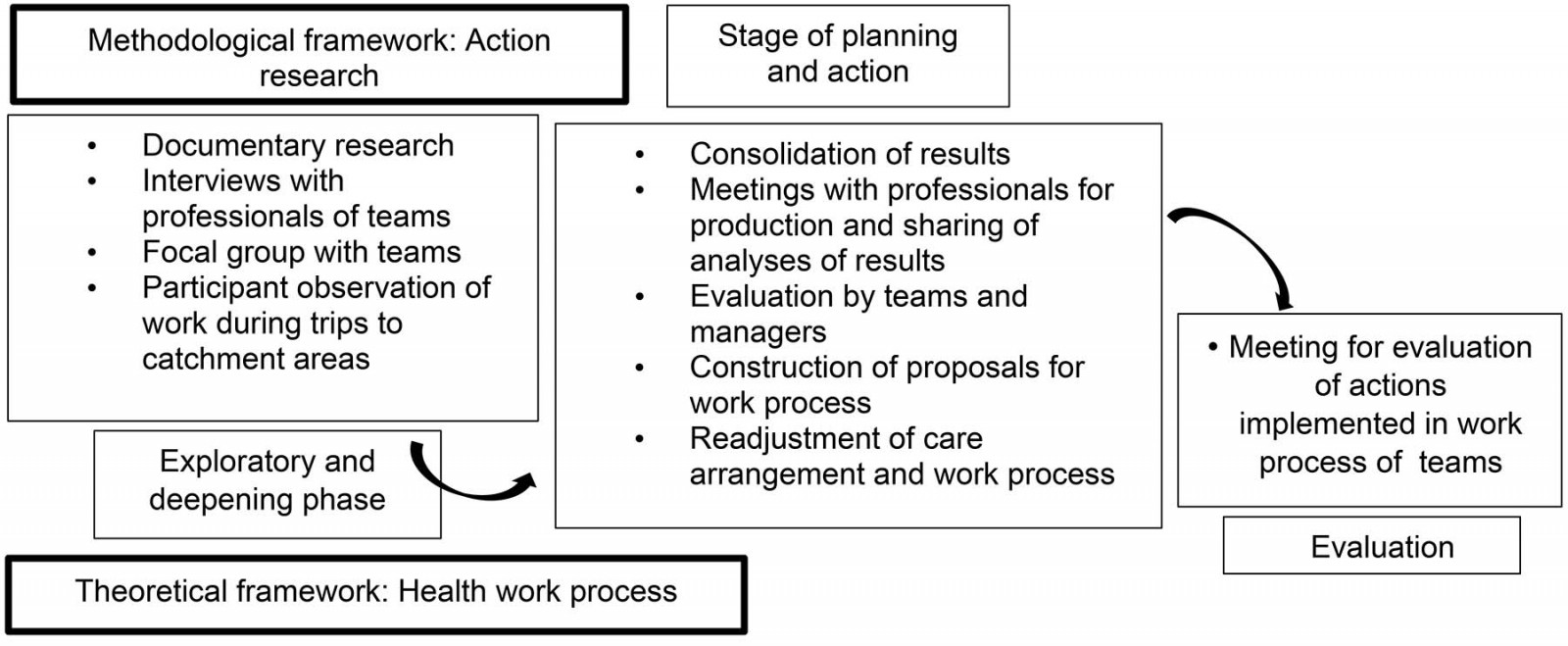 Figure 1: Flowchart of the study ‘Work process in fluvial family health strategies’, Santarém, Pará, Brazil, 2018.
Figure 1: Flowchart of the study ‘Work process in fluvial family health strategies’, Santarém, Pará, Brazil, 2018.
Study setting
The study setting was the municipality of Santarém, in the west of the state of Pará, northern Brazil, with an estimated population of 302 667, of whom 29% live in rural areas13.
In the river regions of the municipality lives a population of 50 950, using boats as a means of transportation. Some of these communities are located far from the urban center, about 20 hours by motorboat, being the poorest population of the rural area, with extractive communities and others self-recognized as indigenous14. Districts of the Tapajós and Arapiuns rivers host the fluvial family health teams under study, called Abaré I (one team) and Abaré II (two teams), serving only part of the population of the areas with the family healthcare arrangement. In the Tapajós region live a total of 1866 families, with 367 families served by the Abaré I team (16 workers). In the Arapiuns region live 945 families, and Abaré II team 1 (13 workers) serves 480 families, while team 2 (15 workers) serves 465 families.
Collection, participants and organization of data
The researchers conducted a pretest with the data collection instrument of semi-structured interview, with the team working in the fluvial mobile unit in the floodplain region, to ensure compliance with the proposed objectives of the research.
The data were collected from September 2017 to May 2018. The interviews were recorded with an audio device and later transcribed to ensure the reliability of the information. The average interview duration was 47 minutes.
Workers with more than 1 year of experience with the fluvial teams and available during the collection period were included. Of the total of 44 workers from the three teams, 27 participated in the interviews and focus groups. Of these, 10 were from Abaré I, 8 from Abaré II team 1 and 9 from Abaré II team 2. Of the 17 non-participants, four were on vacation, four on health leave, three on unpaid leave, three had less than 1 year of work experience with the team and three withdrew due to difficulty attending meetings at the scheduled times.
The methodological framework used was action research, which is a type of social investigation consisting of relating research and action in a process in which the actors and researchers engage, participating in a cooperative way in the elucidation of the reality of which they are part, not only determining collective problems, but also seeking and experiencing solutions in real situations10.
In this perspective, this study adopted the following logic in constructing action research steps.
1. Exploratory phase: A meeting was held to present the project to managers and workers of the teams for knowledge of and adherence to the research. After the necessary approvals, the documents (team deployment projects, reports of health actions carried out) were analyzed and interviews with workers commenced following a semi-structured roadmap. The researchers conducted a focal group with each team (average of nine participants) with triggering questions, totaling three groups. Interviews and groups were audio-recorded and transcribed. On average, interview and focus group durations were 47 minutes and 70 minutes, respectively.
2. Deepening phase: Documentary analysis (team composition, trip schedules, inputs and expenses, sociodemographic profile of the communities) was conducted. Follow-up trips to the teams were done for participant observation, and the work carried out in a total of three trips was registered in the field diary. Researchers observed the work process, facilitating and complicating factors, teamwork and other information following an observation roadmap.
3. Planning and action phase: Meetings were held with the managers and teams to disclose the results found and to share analysis and construction of proposals for the reorganization of the work process.
4. Evaluation phase: A meeting was held with some key participants to evaluate the implementation and reorganization of the work in riverside areas after 6 months of the action phase.
Data analysis
The interviews and focus groups were transcribed and the data analyzed through content analysis to determine the empirical categories in the following stages: pre-analysis, exploration of the material, treatment of the results obtained and interpretation15.
Ethics approval
This study was approved by the Unicamp Research Ethics Committee under opinion no. 2,079,984 (24 May 2017).
The participants were informed of the objectives, methodology and all ethical aspects of the research, having freely consented to contributing. To guarantee confidentiality, codes were used for participants of the focus groups (FG1, FG2, FG3), for the teams (FHS1, FHS2, FHS3) and for participants (P1, P2, P3, etc.).
Results
The study included 27 workers of the fluvial health teams. Of these, 15 were female and 12 were male. The largest age group (24 participants) was 30–49 years. Regarding educational level, 21 participants had complete secondary education, two had incomplete secondary education, and four had higher education.
For work experience in primary health care, 16 participants had up to 4 years, and nine had more than 10 years in primary health care. In fluvial family health work, 15 participants had up to 4 years and 12 had 4–10 years of experience. For work contract, 19 participants were employed by the government, all being community health agents, and the others (eight) had a temporary service contract.
Based on the theoretical framework of the health work process, the following thematic categories were built: work object of the fluvial family health teams; agents executing the working process (who are the workers of the teams?); work technologies (the instruments of the fluvial health work process); and challenges for achieving the purpose of the work process.
Work object of the teams
The teams perceived their main purpose to be the care provided to users, family and community to meet health needs. Their work object was the user with his or her unique needs, but contextualized within the family and community.
These regions are very needy, needing much care. The community members and their families need our work because they have no other place for the service. They have no conditions [are unable] to go to urban areas to receive care. (FHS1,P1)
We care for people individually, but also cases that involve the whole family. There are also situations in which we need to mobilize the community to solve collective problems, so our work focus to solve the problems varies a lot. (FHS2,P2)
We also work with health promotion, not only with cases of diseases. We implement initiatives together with the CHAs [community health agents] with activities involving groups for preventive activities, such as at school, in the group of mothers of the church, in groups of community work. (FHS3,P5)
Work agents: who are the workers?
The activities are carried out by subjects who do the operational work individually, who are the community health agents in the community during the periods in which the fluvial basic health unit is not in the assigned area, and by the other members of the team (physician, nurse, nursing technician, dentist, dental technician) when they are present in the area. It is understood that the work of the community health agents is not dissociated from the process as a whole, because their production and their actions help solve various problems encountered and reported to the team. The accounts emphasize the involvement of nursing in the organization and implementation of the works in the community.
As we live in the community, we are here in some periods when the boat [of the fluvial basic health unit] is not in the area, doing the work little by little in the community. We are the eyes of the team in the community. In fact, we are very engaged in our work in the community. (FHS1,FG1)
We agents and the nurses with our technician do everything possible to ensure that the work goes well. Not that the other teams do not do that, but we perceive more initiative and engagement of some people. (FHS2,P3)
They report that the work is done as a team and that there is mutual support of workers among themselves and with the community. The researchers perceive an effort to build teamwork, but the nursing professional and the community health agents are particularly highlighted.
Teamwork happens, in fact, we meet and discuss. Each one presents an idea, we discuss and work happens. Everything is shared. The nurse knows the area, knows our difficulty. Only we and the nurses who know our work are familiar with our reality. (FHS3,P2)
In participant observation, the planning of the activities and of the regions to be visited by the teams was recorded.
The trips are organized by nurses responsible for the team, by the Strategies coordinator, an adviser of the rivers region, and by the basic care director. For that the nurse has a previous meeting with the team to check and discuss the needs that should be prioritized so the work can be carried out properly. The schedules and routes of visits are defined together with the team in accordance with the priorities and the time since previous visits. (participant observation)
The workers report everyday situations in which there are health risks, such as accidents and occupational diseases.
Our job involves many risks. When the river is dry, we have to find a way to pass. There are branches in the middle of the stream, we have to cut them, sometimes we get hurt, the canoe sinks, and many other situations. (FHS2,P6)
Many colleagues have chronic problems because of work. They have back problems, skin problems because of exposure to sun, gastritis for not eating at proper times, because it's a long way to go back so we mostly stay in the communities. (FHS1,P5)
Work technologies: instruments of the fluvial health process
Participants mentioned situations that characterize the material and immaterial instruments of the work process, referring to the logistics used in the programmatic actions that compose the work and knowledge needed to operate them. They emphasized the lack of training on the various subjects needed for their work in the communities.
For example, prenatal care: we receive the pregnant women, register them, and immediately refer them to the boat laboratory for tests. The lab technician collects the material and does what can be done right away. The serologists immediately collect and freeze it and take it to town and on the next trip already bring the result of serology. The others are already done right away. The vaccine, blood typing, in short, they take the opportunity to do them as soon as possible. (FHS3,P6)
We need more knowledge to carry out our work. It’s been a long time since we’ve had any training! CHAs [community health agents] often do not know the information to inform families. (FHS1,P7)
They also reported carrying out innovative, playful practices, considered successful by the team and community to provide improvement and satisfaction in the work carried out, as well as the importance of intersectoral initiatives to perform the work so as to meet needs.
We’ve already had puppet theater, a beauty day for the elderly in partnership with the school, doing hair, shaving, hair straightener. (FHS3,P1)
Here’s the deal, we have workshops, gym and hiking. The group is not only about giving them medicine. On Children’s Day, each partner helped with toys. We work in partnerships with other services for the activities in the community. (FHS2,P1)
Participants reported on working conditions for teams so they can do their work in communities.
They need more support from our political leaders and managers, and our remuneration needs to improve more. We lack transport, monthly fuel, support material (scales, thermometer, sunscreen, etc.). (FHS1,P2)
They should provide conditions so the work can be carried out. There are problems of access to families, they need a rabeta [small outboard motor], canoe, as well as learning the proper handling, the right way to maneuver [steer the boat] in storms. Risky job! We’ve already had two rabetas that sank when I was on board. (FHS2,P4)
They emphasized the appreciation and sharing of traditional knowledge associated with the knowledge of health workers to mitigate the difficulties encountered at work. Participants reported that communities still have belief in traditional health providers such as faith-healers and midwives and that they seek to approach them for shared work.
People often seek help from individuals in the community who work with alternative therapies such as puxador, faith-healers and midwives and we encourage them to continue to use natural means before intervention with medicines, always with caution. (FG1)
We seek to never oppose their traditional knowledge and practices, their beliefs, we seek to learn and share knowledge. They are also our allies in our work in the community. (FHS1,P3)
Challenges for achieving the purpose of the work process
Workers report weaknesses and potential of the work in FFHS that help or hinder achieving the purpose of the work process. Some larger communities have a health center structure with a nurse and a nursing technician, who live in the communities and also provide service to nearby communities.
One of the difficulties of our team is the physician. Currently, we’re only registered because of the Cuban physician (Mais Médicos program), otherwise the team would be disaccredited and not working. (FHS3,P1)
Something that makes it easier is that there is a health center in my community, so I can refer patients, answer questions immediately, ask for help. The vaccine comes to update the children’s situation. This is very good! (FHS1,P9)
Researchers observed the attempt to order the flow in the healthcare network for achieving the purpose in the FFHS work process.
The evaluation and conduct on the approach to be used with users of riverside communities is set by the team, after observing and confirming the conditions in which they live, so there is certainty that the work will be conducted based on the socioeconomic and family support conditions that users will have. (participant observation)
The difficulty of transport to the urban area of the municipality (from community to urban zone) is a limiting factor for continuing care when the person needs to be referred to a specialized professional, so we discuss with the family how they can proceed. (FG2)
In meetings with the teams to devise proposals to be implemented in order to improve the work process there were the following suggestions: greater proximity of management; support with essential materials such as scales, thermometer, clothing suitable for work, rabetas (small outboard motors) and canoes; priority for workers who need care; improving the flow of user referrals; conducting frequent training for teams; expanding the schedule of visits of fluvial basic health units to communities; support for the basic health units of the area; permanence of professionals in the teams; and valuing workers.
Discussion
The proposal of the Ministry of Health for the basic care of riverside regions, established in the FFHS care arrangement, would be the possibility of guaranteeing services based on their health needs, being as close as possible to the population of these regions. Health care should be considered according to the context in which the subjects live, with all their inherent conditions, so complete care can be planned6,7.
The arrangements were created using present health teams, the riverside family health teams or mobile teams, in the form of FFHS that reach the population in their territory and in their geographic, social, cultural, economic and political contexts, and should provide the interventions required to meet the health needs of the population subjected to geographic isolation and lack of various public services7.
Investments in health in the region and the creation of models of teams adapted to the reality of the communities enabled the restructuring of basic care, expanding the outreach of services, the structuring of physical facilities and the permanence of professionals in these locations, providing better access and thus improving indicators of population health.
All workers in this study have experience in primary health care and fluvial health. Nineteen are community health agents employed by the government and the others are temporary workers. Precarious work leads to higher turnover, generating overload for those who remain, weakening the work processes and undermining the bond with the population and the quality of care16, contributing to the low assessment of the worker–user affiliation.
A study conducted in the five regions of Brazil shows that there is dissatisfaction of professionals working in FHS with a strong connection to the management of health work in primary health care, mainly associated with working conditions such as training and role in the production process, employment relations, salary, quantity and quality of work instruments, and the knowledge to execute them17.
The elements of the work process relate to what is considered as the work object. This may be, for example, the biological body, the family or a man/woman in his/her condition of existence. Depending on what is considered as the work object, certain actions and different practices are conducted18.
It was observed that FFHS workers considered the work object to be the users with their individual health needs and also as part of the family context for the production of care, as well as families within their communities when associated with collective health issues. In a study conducted in the state of Paraíba, Brazil, when analyzing the perception of FHS workers about their work object, the workers pointed to users, family and community with specific health needs beyond the individual and biological dimension, considering the social determination, and the family and community relationship19. These findings are similar to those found as the work object in fluvial family health teams.
Workers are engaged in the activities of work process agents, highlighting the community health agents in the community and the nurses in the management of health teams and units, in addition to the focus on teamwork recognized by the participants. This teamwork mode in FFHS differs from that reported in a study conducted in southern Brazil which, when analyzing the perception of health workers regarding FHS, found that they worked in individual spaces, conducting independent activities and with little possibility of interaction; thus, teamwork was characterized by the juxtaposition of professions, without the establishment of relations among workers from each area20.
When work conditions are inadequate, health workers cannot work in order to help users at the time of care, because the quality of life of these workers relates to the quality of the means to conduct their activities and to working conditions. This confirms the need for a support network for those working in FHS21. This need is directly related to better performance at work. Community health agents are exposed to numerous unsuitable conditions at work that can lead to accidents or diseases, showing the impact of the work process on the health of workers22.
In the work process, it is possible to identify work technologies, which are instruments that can be material or immaterial23. Examples of these instruments are the material elements and knowledge necessary for the production of care. In FHS, other kinds of knowledge and new instruments are needed, because the families should be considered in their specific conditions that require knowledge such as that of popular culture, produced by means of dialog, listening, bonding, humane care and empowerment24.
This study found that having health units in larger and strategic communities with nursing teams can reduce the difficulties of access to care: these workers can support the fluvial teams. The difficulty for medical professionals to stay in teams located in remote areas of the country persists, and it interferes with the implementation and permanence of the teams, especially in riverside regions.
Valuing traditional health providers in communities is considered to have potential. A study conducted in Nigeria shows the scarcity of health workers in rural areas and that there is preference for informal health providers in communities because they do not always have health workers available. Low availability leads to low demand for services, discouraging primary health care workers and leading to absenteeism or the decision to leave the community25.
Regarding the challenges to achieving the purpose of the health work process, a study analyzed how the Hong Kong and Chinese governments enhanced universal health coverage through community nursing services. They introduced services in communities, for example for less complicated cases, increasing accessibility to the service, improving quality of life and expanding the service to those who have difficulty in accessing health centers26.
The workflow of the service provided to users is a challenge to be overcome, considering the difficulties of geographic access as well as social and economic issues of the communities. There is no sure way to follow for this population, because there is no assessment directed to this issue. A study in Greece aimed to determine how the existing patient care integration and flows occur and organize the operational connection of primary health care, recommending alternatives and workflows to improve integration27. The care service flows were mapped and analyzed, and the recommendations for a primary care integration model were organized. Lack of integration can result in fragmentation of care and precarious health outcomes, as well as problems related to funding, planning, efficacy and function of the health system27.
In the USA and France, studies show that there is wide interest in redesigning primary care practice models to guarantee access to quality health care by valuing workers, especially nurses, as agents of transformation, in addition to the population as care receivers28,29.
In the Amazon region, teams need to be flexible according to the needs and difficulties of community members, because there is no possibility of standardization of services, with rigid protocols, and with greater flexibility it is possible to achieve the purpose of the work, which is to meet the health needs identified.
In the action research evaluation stage, meetings were conducted with team and management members to determine what was implemented in the work process. It was found that, after the implementation of the new National Primary Care Policy (2017), there were some changes in the structure of the teams, with two teams being disaccredited, changing from FFHS to primary care teams in the main communities, as a way to minimize financial resources in the municipality. The change in the Mais Médicos program caused a negative impact due to the difficulty of having medical professionals stay in remote communities.
At the same time, the Permanent Education Center was established to organize training activities among workers. With regard to material instruments, the delivery of uniforms and other equipment to the health teams and units was already scheduled.
To organize the workflow of care for riverside populations, a basic health unit was structured in the urban area, strategically located to meet the demands of the riverside communities. Medical consultations, nursing consultations and laboratory exams, as well as areas for service in some medical specialties, were available for this population, if necessary, through referrals by the basic health units in the communities.
Contribution to the areas of health and public policies
This study presents the challenges and potential that fluvial family health workers face in the work process in adverse contexts such as those of riverine regions. It offers contributions for municipal managers to solve local problems to improve dynamics and workflow and the care provided to riverine users. It emphasizes the strategic work of nurses as coordinating agents and, possibly, as structuring agents in the work process of teams.
Conclusion
This study highlights the recognition of the work object centered on individuals based on their unique needs, associated with a family unit for production of care and with the community when referring to collective issues.
The lack of teams in the riverside areas of the Brazilian Amazon generates care gaps aggravated by the lack of fixed health units in some localities, as well as the large distance from the communities to the nearest unit.
There is a need to strengthen intersectoral and mutual support activities with the communities to improve the work and greater popular participation in decisions about the organization. Few studies show and analyze the workflow of the care service provided to riverside communities and provide the ordering of referrals and counter-referrals. There is a need for professional training, permanent education initiatives, workers’ health and improvement of working conditions (physical structure, materials and inputs).
Finally, the impact of changes in the National Primary Care Policy in 2017 is shown, with the neglect of local and regional differences and difficulties leading to the disaccreditation of two fluvial health teams considered costly by the municipal government and the decision to maintain the basic care teams in the communities in which that service (nurse and nursing technician) already existed. This may result in lower expenses for the municipal government, but also in less access for riverine populations.
Acknowledgements
The authors thank the workers of the study health teams and are grateful to the Coordination for the Improvement of Higher Education Personnel for a doctoral grant.
References
You might also be interested in:
2021 - Change in the geographic distribution of human resources for health in Turkey, 2002–2016
2019 - Rural women’s first-person perspectives on the role of mental health in substance use
2011 - Receipt of preventive counseling among reproductive-aged women in rural and urban communities


