Introduction
Heart failure (HF) is a chronic medical condition characterized by the inability of the heart to provide sufficient blood flow to meet the body’s requirements1. Individuals with HF experience progressive debilitating symptoms that result in functional impairment and require the assistance of informal caregivers (eg family, friends) to meet daily needs and assist with disease management2. These activities occur while caregivers also manage household-, child-, and employment-related activities and attempt to care for themselves3. Providing care for patients with HF significantly affects many aspects of informal caregivers’ lives, including their physical, psychological, and social wellbeing. Often, informal caregivers experience feelings of emotional distress and uncertainty in managing periods of HF instability and worsening of symptoms.
In the USA, approximately 39.8 million informal caregivers provide care for individuals with a chronic condition, such as HF4, and, of these, 15% live in rural areas5. Caregivers are the hidden structure of the social and healthcare system, particularly in rural areas where healthcare services and resources are limited6. Yet, providing care for patients with HF is stressful, with essential care often required 24 hours a day7. Further, rural caregivers report lower incomes8 and are more likely to confront unique challenges such as food deserts (living in areas where it is difficult to buy affordable and healthy food)9, limited health and social services, increased travel for services, and more limited transportation options than their urban and suburban counterparts10. More than half of rural caregivers also work outside the home. Rural caregivers are more self-reliant, often caring for individuals with HF alone5.
Unsurprisingly, rural caregivers are prone to negative outcomes, including decreased quality of life and physical health, sleeplessness, and mood changes11. In HF caregivers, depressive symptoms, negative life changes, poor self-care, and higher caregiver burden are common7,12. Yet, previous research findings suggest social support, problem solving, and family function may influence these outcomes2,13,14. Low levels of social support and poor family functioning is associated with depressive symptoms, higher caregiver burden, and more negative life changes15-17, while poor problem solving is associated with more depressive symptoms and worse self-care13,18. Improving social support, problem solving, and family functioning may be important targets for intervention. However, the influence of these factors on outcomes in rural HF caregivers is unknown.
Rural caregivers face many stressors when providing care for patients with HF. Thus, this study was guided by the theory of stress, appraisal, and coping19, which postulates that coping resources (eg social support, problem solving, family function) influence the manner in which one copes with stressful situations. Caregivers’ coping abilities are influenced by problems encountered in the caregiving role, their usual coping strategies, and available resources to manage caregiving challenges. Coping responses are strategies used by rural caregivers to manage common problems as they attempt to either eliminate, change, or lessen caregiving demands19.
Factors such as social support, problem solving, and family functioning may influence stress and caregiver outcomes19. For example, caregivers who have better social support, effective problem-solving skills, and optimal family functioning will appraise caregiving situations objectively and cope more effectively in managing caregiving stressors in the home. In using these skills to manage caregiving problems, rural caregivers may be more likely to have fewer depressive symptoms, more positive perceptions of caregiving-related life changes, better self-care, and less caregiver burden. The purpose of this study is twofold: (1) to examine whether social support, problem solving, and family function predicted depressive symptoms, caregiving-related life changes, self-care, and caregiver burden in rural HF caregivers; and (2) to compare differences in these variables between rural and urban caregivers.
Methods
Study design and sample
This study was a secondary analysis of data from an online, descriptive, cross-sectional survey (n=530) where a subset of 114 of these caregivers who lived in rural areas, as determined by the Rural Health Information Hub (RHIH) tool20, were used for the current analysis. In determining rurality, the RHIH tool uses various rural definitions, including those used as eligibility criteria for federal programs, seven common rural definitions (eg Rural Urban Commuting Areas by census tract, Rural Urban Continuum Codes), and shortage areas (eg Health Professional Shortage Areas). Compared to the current analysis, which compared both rural and urban caregivers, the parent study was a mediational analysis combining both rural and urban data scores to examine whether social support and problem solving mediated relationships among caregiver demands and burden, self-care, depression, and life changes in HF caregivers. Hence, the parent study analysis neither compared rural and urban scores nor examined whether social support, problem solving, and family function predicted selected study outcomes in rural HF caregivers. A full description of recruitment and study procedures used in the parent study has been published13.
Purposive sampling was used to recruit caregivers, with recruitment efforts coordinated between two study sites in south-eastern USA. Caregivers were recruited by multiple methods (eg flyers, newspaper advertisements, social media sites, study website, face-to-face and telephone) to enhance the diversity of the participants21. Caregivers were included in the study if they were: (1) 18 years old or older; (2) able to read, write, and understand English; (3) not cognitively impaired (less than 8 on the Six Item Cognitive Impairment Test – 6CIT)22; and (4) responsible for assisting patients with HF with completing daily care activities for 6 months or more.
Procedure
Participants were recruited locally from the south-eastern USA (using face-to-face and telephone contacts, posted flyers, newspaper advertisements, and social media sites), nationally (newspaper advertisements and social media) and internationally (using social media). Potential participants were directed to the study website to complete the online survey. These methods recruited participants who lived in 24 states within the USA, as well as from Canada, England, Ireland, Scotland, and Wales.
A copy of the written informed consent was provided for review at the beginning of the survey, followed by items to assess inclusion/exclusion criteria and cognitive screening. Completion of the online survey represented an individual’s consent to participate in the study. The online survey was deployed using Qualtrics, a web-based platform with several data safeguards23,24.
To enhance validity of data, researchers examined the completed surveys, removing those from analysis based on the following recommendations from empirical literature: (1) inconsistent responses were provided on sociodemographic items; (2) surveys were completed in up to 10 minutes (less than average completion time); (3) multiple surveys were submitted using the same IP addresses; (4) the incorrect month and year were provided (compared to date stamp); and (5) submitted surveys used similar or unrealistic email addresses25,26. CAPTCHA (Completely Automated Public Turing test to tell computers and Humans Apart) also was used to prevent fraudulent survey submissions26.
Data were collected between November 2016 and June 2017, with inclusion/exclusion screening and data cleaning measures occurring concurrently. A total of 768 online surveys were screened for eligibility; 244 surveys were removed during data cleaning (ie based on exclusion criteria and potentially fraudulent submissions), and 544 surveys were retained. Another 14 surveys were removed for possible cognitive impairment (scored 8 or more on the 6CIT)22, resulting in a final 530 online surveys retained for data analysis13. Of the total sample, a subset of 114 surveys from rural caregivers was used in the current analysis. In the USA, caregiver geographic location was determined from participant-provided zip codes and the RHIH tool, which is supported by the Health Resources and Administration of the US Department of Health and Human Services. This online tool evaluates whether a specific zip code is considered ‘rural’ based on eight criteria20. For other countries, postal codes (eg Canada’s postal codes specify rural versus urban status) and population/census (eg small population area statistics) data for those postal codes were used. The sample included caregivers who lived in 24 states within the USA, as well as Canada, England, Ireland, Scotland and Wales.
Measures
Caregivers answered a researcher-developed sociodemographic and clinical survey for caregivers and patients with HF that included caregiver and patient gender, marital status, age, education level, race, number of people living in the home, caregiver relationship to the patient, whether or not caregiver lived with the patient, time providing care, household and individual income, zip code, major diagnoses/comorbid conditions, and time since the patient received an HF diagnosis. Items concerning the severity of HF symptoms were answered by caregivers based upon the standardized New York Heart Association (NYHA) HF Classification27. An investigator who was an advanced practice nurse with cardiology expertise determined the class of HF based upon caregivers’ responses.
Independent variables
Social support: Social support was measured with the Interpersonal Support Evaluation List-12, a Likert-type scale that assesses belonging, tangible, and appraisal support. Response options range from definitely false (0) to definitely true (3), with total scores ranging from 0 to 36. Higher scores indicate higher levels of support28. Validity and reliability have been supported in previous studies using general populations28. In this study, Cronbach’s alpha was 0.86.
Problem solving: Problem solving was measured with the Social Problem-Solving Inventory Revised-Short, a 25-item five-point Likert-type scale that measures positive problem orientation, negative problem orientation, rational problem solving, impulsivity/carelessness style, and avoidance style. Response options range from 0 to 4 and total scores range from 0 to 20, with higher scores indicating better problem-solving skills29. Empirical evidence supports its content and construct validity for family caregivers, with adequate internal consistency30. Internal consistency reliability in the current study was 0.84.
Family function: Family function was measured with the five-item Family APGAR (adaptability, partnership, growth, affection, and resolve) that assesses satisfaction with adaptation, partnership, growth, affection, and time commitment. Response options range from 1 to 3 and total scores range from 5 to 15, with higher scores suggesting a higher level of family functioning31. Validity and reliability have been previously supported31,32. Cronbach’s alpha in this study was adequate (α=0.71).
Dependent variables
Depressive symptoms: The 20-item Center for Epidemiological Studies Depression Scale was used to measure depressive symptoms, with response options ranging from 0 to 3 and total scores ranging from 0 to 60. Higher scores indicate more depressive symptoms, with scores of 16 or more suggesting some degree of depression. Prior research supports its validity and reliability33. Internal consistency reliability in the current study was 0.94.
Caregiving-related life changes: Caregiving life changes was measured with the Bakas Caregiving Outcomes Scale, a 15-item, seven-point scale that assesses caregivers’ perceptions of how social functioning, subjective wellbeing, and physical health have changed from providing care. Response options range from –3 (1) to +3 (7) and total scores range from 15 to 105, with higher scores suggesting more positive life changes34. Research has supported construct validity and internal consistency in HF caregivers35,36. In this study, Cronbach’s alpha was 0.85.
Self-care: Caregiver self-care was measured with the Denyes Self-Care Practice Instrument37, an 18-item instrument that measures self-care activities that are universal self-care requisites (eg diet, rest, exercise). Response options for each item range from 0 to 100, with a total score calculated by averaging the item responses for all 18 behaviors, and higher scores representing better self-care38. It has support for construct validity and acceptable internal consistency with adult populations39.
Caregiver burden: Caregiver burden was measured using the 38-item Dutch Objective Burden Inventory, an instrument that examines both objective and subjective burden. Responses for each item range from 1 (‘no’, ‘never’; ‘not at all burdensome’) to 3 (‘yes’, ‘often’ or ‘always’; ‘very burdensome’), with total scores on each subscale ranging from 1 to 3. Higher scores indicate greater perceived objective and subjective burden. Although caregivers rate both the frequency (objective burden) and perceived burden (subjective burden) for each caregiving task, only the subjective component was used in this analysis because no significant relationship was found between objective burden and study outcomes40,41. The validity and reliability of the Dutch Objective Burden Inventory have been supported previously40. Cronbach’s alpha was 0.92 in this study.
Statistical analysis
Descriptive statistics for participant characteristics and study variables were computed. Because data were not normally distributed, a Mann–Whitney U-test (two-tailed, α=0.05) was used in an exploratory analysis to assess differences in study variables among the full sample (rural=114, urban=426) to determine the need for further analysis of the rural subset data. The remaining analysis was conducted in two primary steps. First, bivariate correlations among outcome variables were assessed using Spearman's rho. Second, a multivariate linear model was built to simultaneously model relationships between four dependent variables (depressive symptoms, life changes, self-care, and caregiver burden) and three independent variables (social support, problem solving, and family function), while controlling for eight sociodemographic/clinical variables (gender, education, relationship to patient (spouse vs other family/friend), time (years) providing care, age, time (years) since HF patient diagnosis, number of HF patient comorbidities, and HF patient NYHA classification). The model was reduced by sequentially eliminating variables with very small effect sizes (ηp2<0.05) until only terms with effect sizes larger than 0.05 remained. Of the four commonly used multivariate tests (ie Pillai’s trace, Hotelling’s T2, Wilk’s lambda, and Roy’s largest root), Pillai’s trace is the most powerful multivariate statistic. However, in cases where degrees of freedom exceed one, Roy’s largest root is the recommended multivariate test and has higher power than Pillai’s trace42. Therefore, Roy’s largest root was used to determine the relative importance of terms in the model. Roy’s largest root is a positive-valued statistic defined as λ1(1+λ1), where λ1 is the largest eigenvalue of the generated test matrix and larger values indicate that the effects in the model have large contributions to the model under question. Model assumptions were examined by reviewing standard residual plots.
Ethics approval
The study was approved by institutional review boards from two university-affiliated sites, the University of Alabama at Birmingham (161117003) and Florida State University (2016.20014).
Results
Demographics
The researcher-created sociodemographic instrument showed that caregivers were primarily Caucasian (84.2%), married (93.0%), and women (58.8%) who were the spouse of the patient (51.8%), with an average age of 41.45 (standard deviation (SD)=9.01) years (Table 1). Slightly less than half of patients with HF had no comorbidities (47.4%; Table 1) and were male (n=53, 46.5%), and half of patients had a high school diploma or less schooling (n=57, 50.0%). Patient mean age was 51.6±16.9 (range=32–94 years). The majority of patients were diagnosed with HF in the past 5 years (69.3%) with more than three-quarters of patients having a standardized NYHA HF classification of either I or II (78.1%) (Table 1).
Comparison of rural and urban caregivers
Although the parent study was a mediational analysis combining both rural and urban data, when comparing rural and urban data separately, rural caregivers experienced lower mean scores on social support (21.81±6.72 for urban; 19.01±7.55 for rural), problem-solving skills (11.78±2.85 for urban; 10.72±2.06 for rural), self-care (57.62±17.02 for urban; 56.79±18.28 for rural), and family functioning (11.58±2.23 for urban; 10.99±2.32 for rural) than those caregivers living in urban areas. These rural caregivers also had higher mean depressive symptoms (20.37±11.97 for urban; 24.94±13.58) for rural) and subjective caregiver burden (1.65±0.40 for urban; 1.77±0.39 for rural). However, rural participants had some greater perceived positive life change scores (60.48±12.6 for urban; 61.56±11.82 for rural) than urban caregivers as a result of their caregiver role.
In comparing differences in study variable scores among rural and urban caregivers using the Mann–Whitney U-test, it was seen that rural participants experienced significantly less social support (p=0.001), worse problem-solving skills (p=0.003) and family functioning (p=0.009), and greater depressive symptoms (p<0.01) and subjective burden (p=0.001) than urban participants. There were no significant differences in caregiver self-care (p=0.416) and perceived life changes (p=0.346) among rural and urban caregivers (Table 2).
Correlations
Bivariate correlations among the four dependent variables were calculated using Spearman's rho. Using Cohen’s43 recommended correlation classification of the magnitude of 0.10–0.29 for weak correlations, 0.30–0.49 for moderate correlations, and above 0.50 for strong correlations, strong correlations were observed between self-care and life changes (ρ=0.644, p<0.001) and between self-care and caregiver burden (ρ=0.536, p<0.001). Moderate correlations were observed between depressive symptoms and caregiver burden (ρ=0.424, p<0.001), life changes and caregiver burden (ρ=–0.406, p<0.001), and self-care and depressive symptoms (ρ=–0.374, p<0.001). Depressive symptoms and life changes were weakly negatively correlated (ρ=–0.269, p=0.004).
Final model
After removing educational level because of its small effect size (ηp2=0.034), the final model contained all of the other variables and no violations to the multivariate regression assumptions were found. The adjusted R2 values were 0.686, 0.389, 0.509 and 0.0491 for depressive symptoms, life changes, self-care, and caregiver burden, respectively. Social support contributed the largest effect (Roy’s largest root 0.690, p<0.001) to the multivariate model (Table 3). Social support had a large effect on depressive symptoms (ηp2=0.384), a moderate effect on self-care (ηp2=0.108), and a small effect on caregiving-related life changes (ηp2=0.055) (Table 4), with fewer depressive symptoms (ηp2=–1.139, standard error (SE)=0.142, p<0.001), more positive life changes (ηp2=0.422, SE=0.173, p=0.016), and better self-care (ηp2=0.846, SE=0.239, p=0.001) as social support increased (Table 4). Problem solving had a moderate effect on depressive symptoms (ηp2=0.078) and a large effect on caregiver burden (ηp2=0.23) (Table 3), with depressive symptoms improving (ηp2=–1.329, SE=0.45, p=0.004) and caregiver burden decreasing (ηp2=–0.09, SE=0.016, p<0.001) as problem solving improved (Table 5). Family function had a moderate effect on life changes (ηp2=0.104), self-care (ηp2=0.088), and caregiver burden (ηp2=0.116) (Table 3), with more positive life changes (ηp2=1.398, SE=0.404, p=0.001), improved self-care (ηp2=1.768, SE=0.56, p=0.002), and less caregiver burden (ηp2=–0.044, SE=0.012, p<0.001) as family function improved (Table 4).
Table 1: Caregiver characteristics (n=114)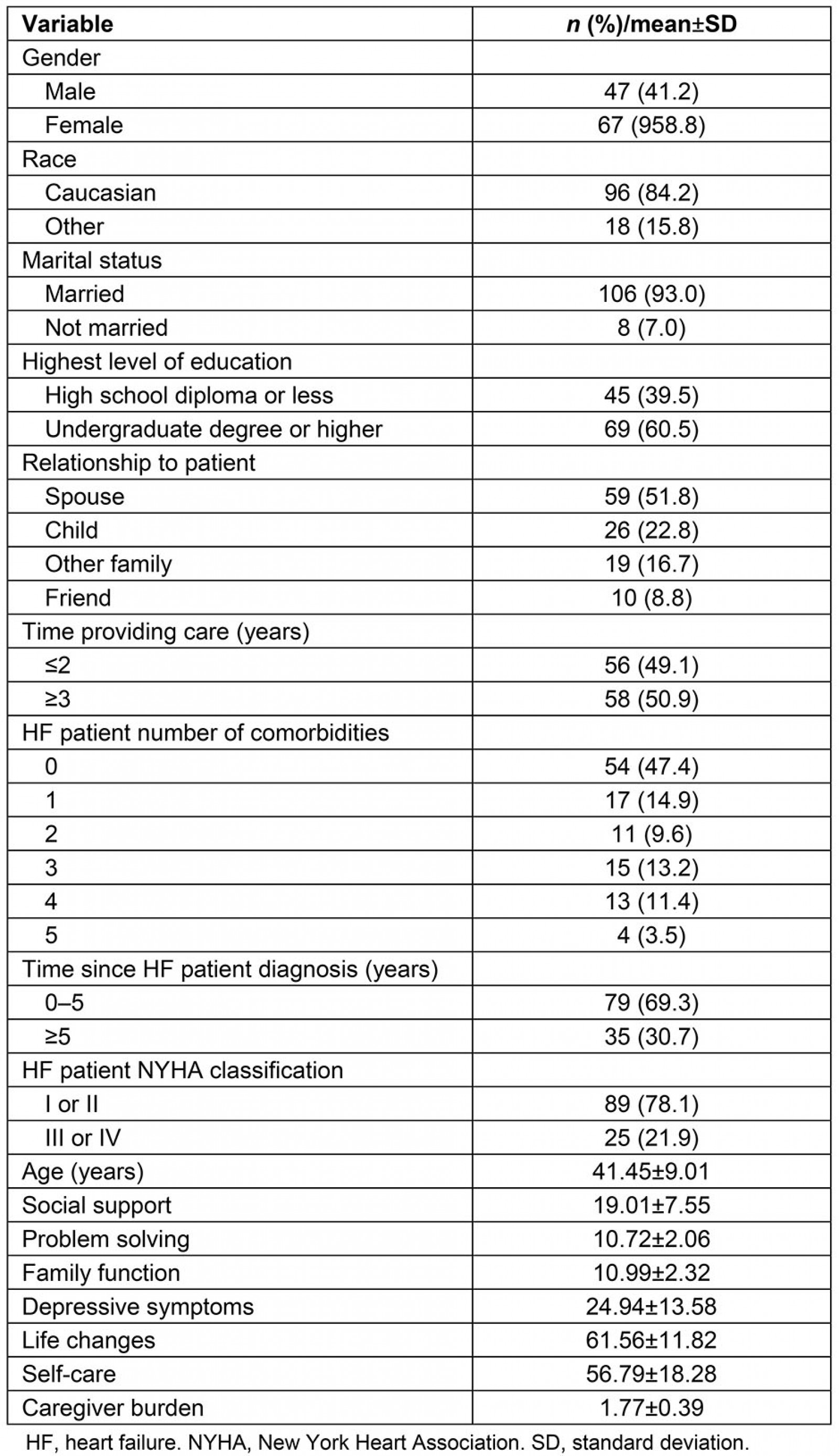
Table 2: Descriptive differences between urban and rural caregivers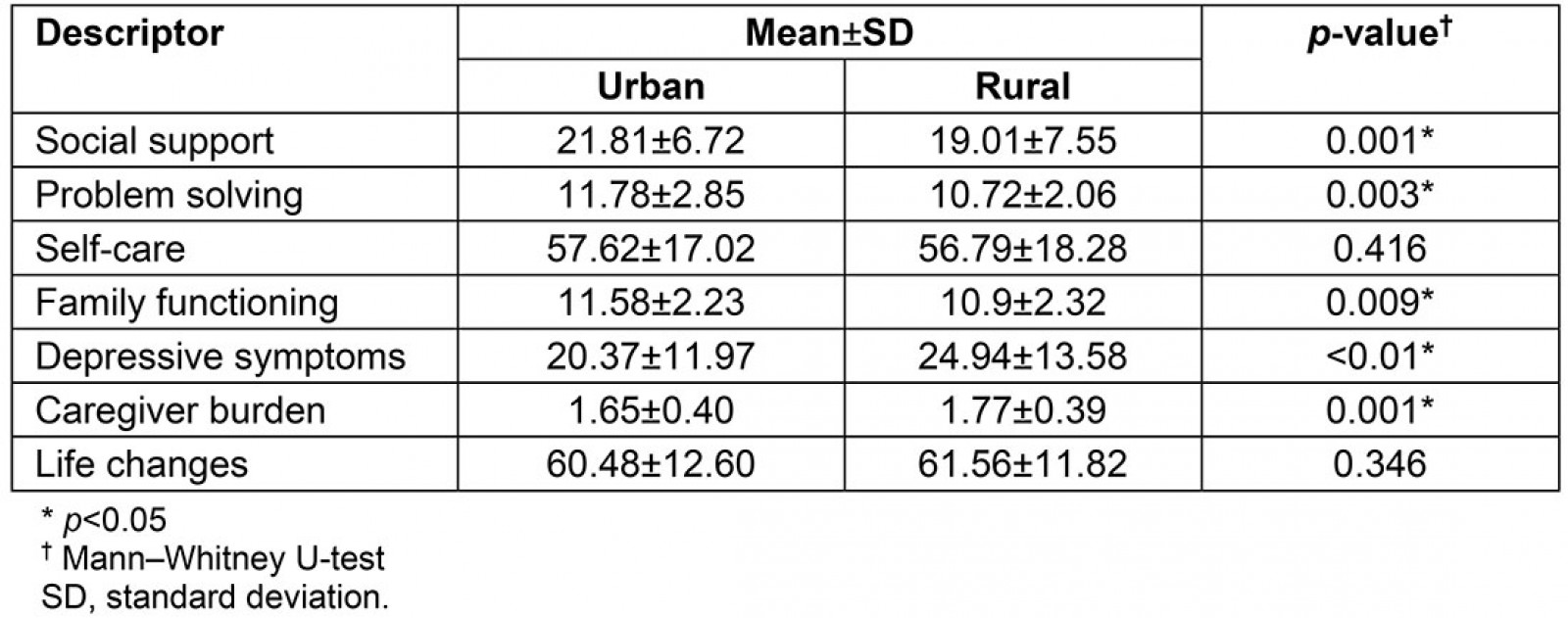
Table 3: Multivariate tests for the overall model†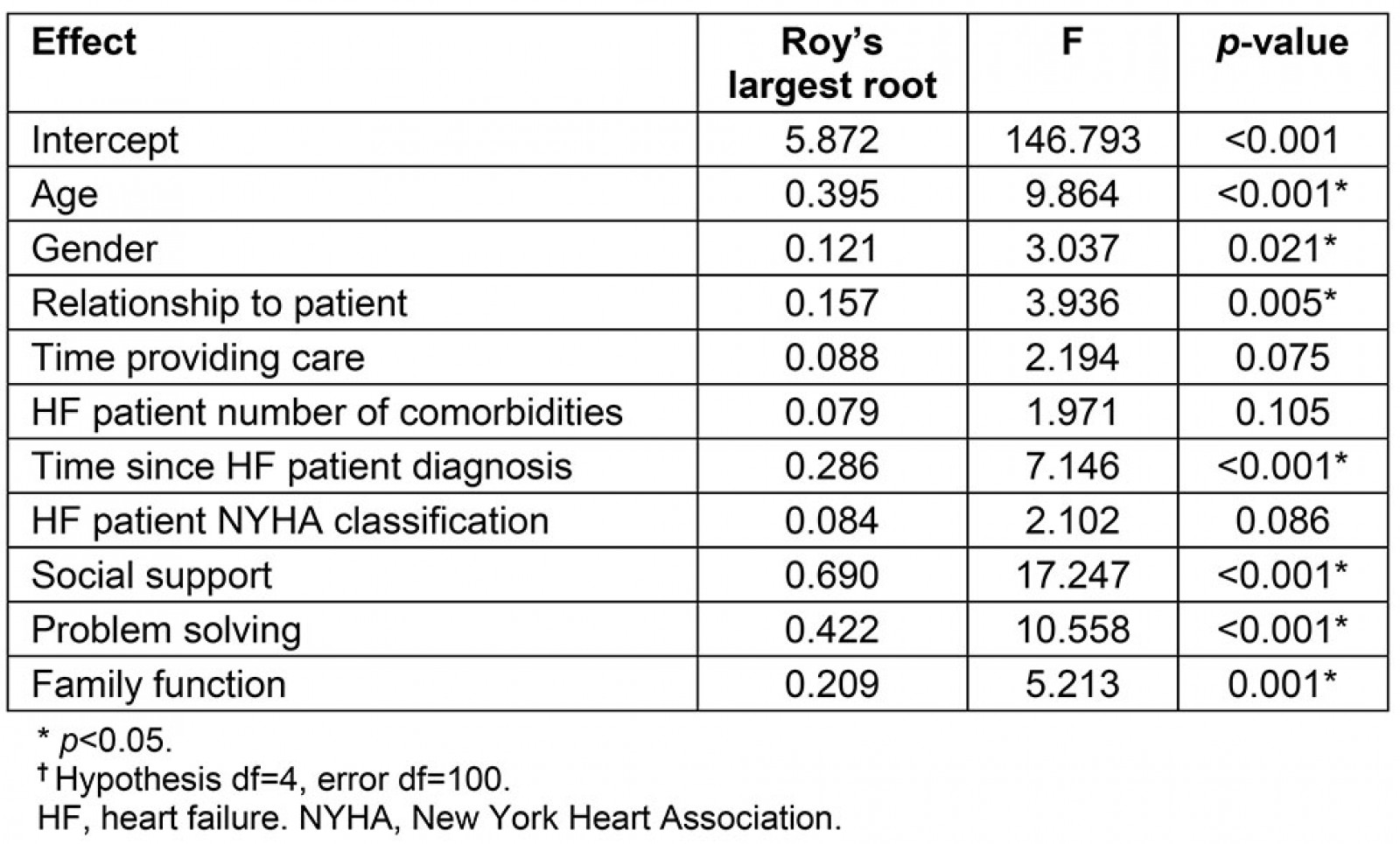
Table 4: Univariate tests of between-subject effects for the final model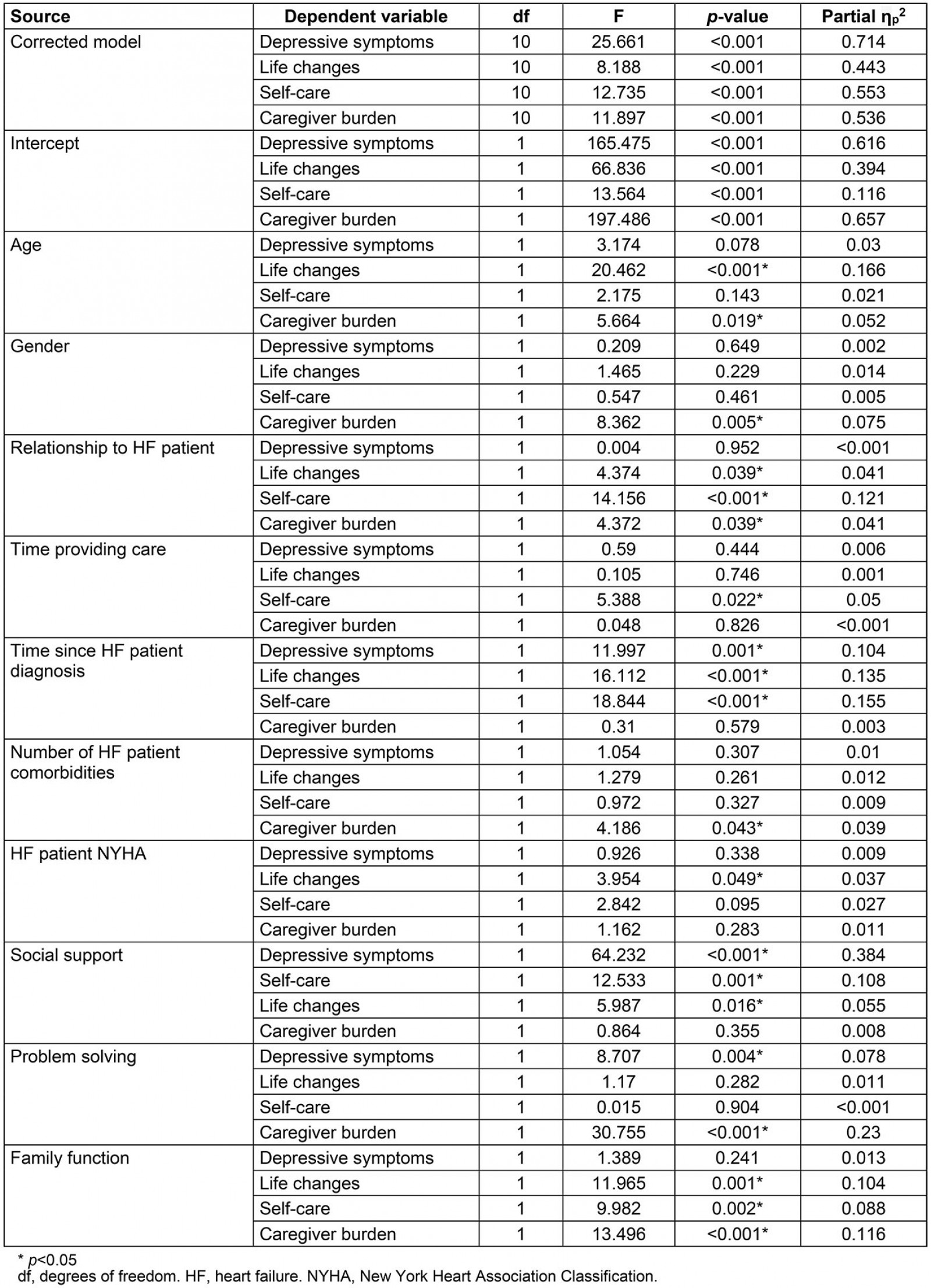
Table 5: Parameter estimates for final multivariate model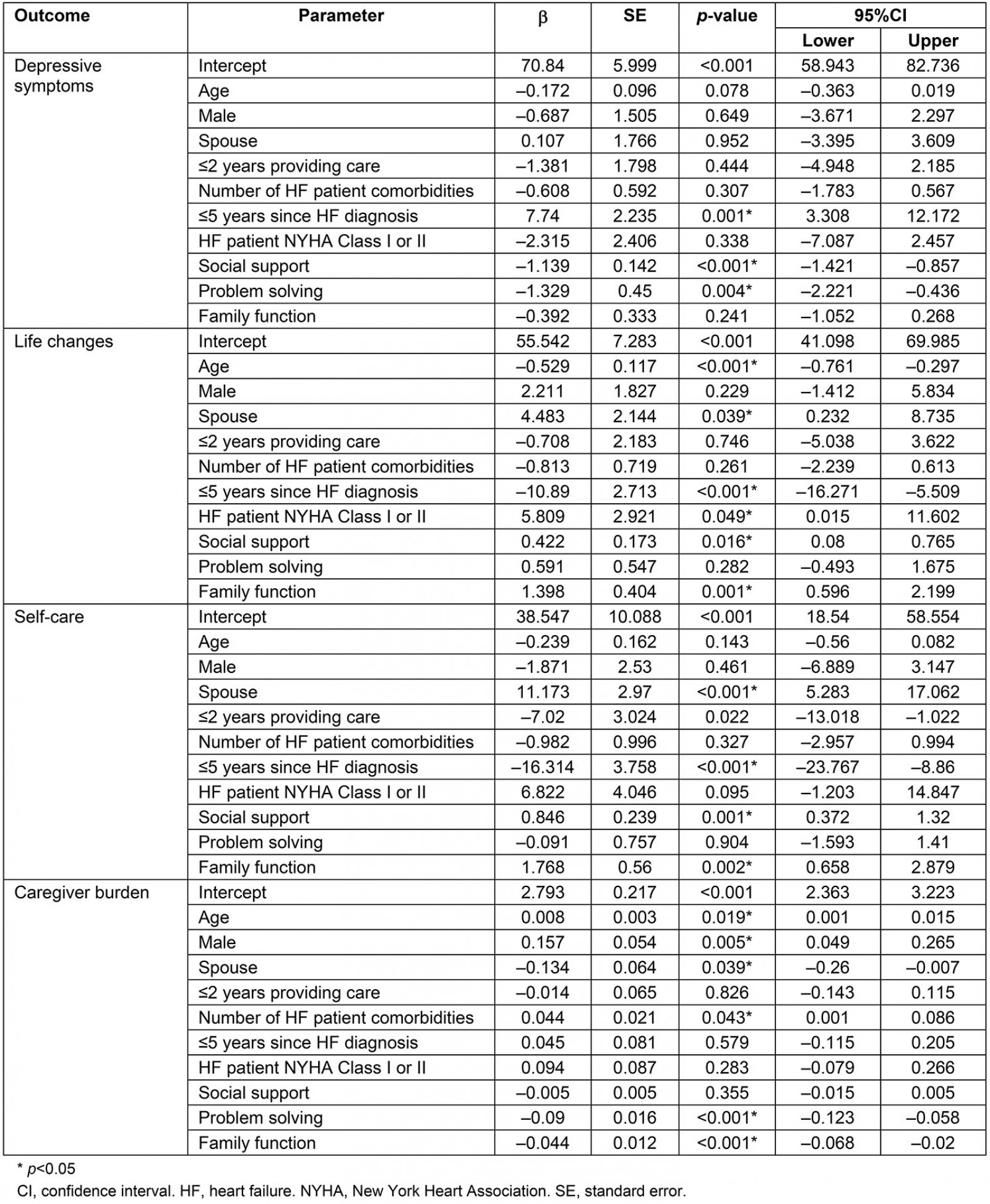
Discussion
Caring for patients with HF is stressful, with daily demands necessitating optimal coping resources and skills3,7,15,19. Rural HF caregivers must navigate additional challenges related to rurality (eg limited transportation, food deserts, lack of assistive care)9,44, which further threaten psychological and physical wellbeing and increase the need for adequate coping19. Findings of this study illustrate the dire need for studies targeting psychosocial factors in rural HF caregivers, as most caregivers in this study had low levels of social support, problem solving, and family functioning. Thus, it was not surprising that this rural sample also reported high levels of depression, more negative life changes due to caregiving, poor self-care, and increased caregiver burden.
Social support and depressive symptoms
These findings are consistent with the parent analysis and prior studies showing that higher levels of social support are related to fewer depressive symptoms in caregivers45. Caregivers have greater difficulty in completing caregiving activities due to caregiver burden, inadequate family support, and caregiver stress. Caregivers monitor HF symptoms, assist with HF self-care activities, and manage complex treatment plans. Caregivers also assume many responsibilities previously carried out by patients with HF, such as household chores. Assuming these activities frequently leads to social isolation and inadequate socialization7, which often is already present in both rural and urban communities and favors depressive symptoms in these caregivers.
In rural areas, caregivers of patients with HF often report they have inadequate support from friends, families, and healthcare providers3,14, with family abandonment41, as well as inadequate emotional, informational, and tangible support46. Inadequate professional support and guidance by healthcare professionals47 also occurs in rural areas due to heavy provider workloads and inadequate interactions between family and healthcare personnel48. Caregivers need skills to obtain social support, in addition to voluntary and formal services offered by health providers49. Caregiver support groups commonly are not used because of isolation, conflicting schedules, and a desire to remain anonymous50. Further, rural caregivers may not be able to access support groups because of a lack of transportation or income to travel to urban areas where these resources are more likely to be available.
Social support and self-care
In the current study, social support also had a significant effect on self-care. While it is widely assumed that social support influences caregiver self-care, there are limited studies in HF caregivers that support this belief7. Further, to the authors’ knowledge, this is the first study examining social support as a predictor of caregiver self-care in rural HF caregivers. Considering the daily challenges experienced by HF caregivers3,7, it is unsurprising that social support would influence rural caregivers’ self-care behaviors. Rural patients most often have one primary caregiver, and assistance from others only occurs when the primary caregiver’s health declines or they do not live with the patient51. In rural caregivers, factors such as greater distances, more limited transportation, and inadequate use and unavailability of social, volunteer, and in-home support services may negatively influence rural caregivers having time to perform healthy behaviors5.
These findings also are consistent with the parent study, which found social support had a significant effect on self-care, although the effect was small. Empirical data support the fact that urban caregivers have challenges and report inadequate time to prepare nutritious food and to perform heathy behaviors, such as exercise. Caregivers often report they have either failed to schedule or missed routine health provider visits because of caregiving demands. Those who have more caregiving hours also are more likely to engage in unhealthy behaviors, such as smoking and eating more saturated fat52.
In a qualitative study using components of cognitive behavioral therapy and spiritual counseling by health providers, caregivers reported greater participation in self-care activities53. Other interventions to enhance self-care include e-health-based caregiver support with experienced healthcare personnel who provide individualized information, advice, and support54,55. Further, caregivers often participate more in self-care activities when they receive feedback about their chronically ill family members56; thus, providing information on the patients’ status may be a promising strategy to enhance caregiver self-care.
Social support and life changes
Social support also influenced caregiving-related life changes (eg social functioning, subjective wellbeing, and physical health) in this study, although the effect was small. Empirical literature suggests social support is important to rural caregiver quality-of-life outcomes2. Caregivers report lack of professional support49 and low familial support15, which affects their perception of the caregiving experience57. In fact, higher levels of social support are associated with more positive caregiving experiences in HF caregivers57. Factors such as rural isolation and limited personal resources and rural health delivery systems may contribute to the inability of caregivers to socialize and to maintain or enhance their social functioning and psychosocial wellbeing. Interventions that increase social support and optimize available community resources (eg church groups, community health workers, senior centers, home health aides) within rural areas may help to enhance the caregiving experience in rural settings5. In contrast, the parent study found no significant relationship between social support and caregiving life changes. Because the effect was small in rural participants, further research is needed before proposing reasons for these differences in social support and caregiving-related life changes between rural and urban participants.
Problem solving and caregiver depressive symptoms
These findings also suggest that as problem solving improves, depressive symptoms lessen. Studies examining problem solving in HF caregivers are limited, and, of available studies, findings differ. For example, in the parent study13 that examined both urban and rural caregivers (n=416, urban; n=114, rural), problem solving did not influence depressive symptoms. Similarly, in a study of caregivers of older adults with dementia, no relationship between problem solving and depressive symptoms was found58. However, earlier work in HF caregivers18 showed a negative orientation to solving problems (a component of problem-solving) was significantly associated with higher depressive symptoms. Likewise, in stroke caregivers, a negative problem orientation had a significant effect on depression59. Rural HF caregivers, in particular, may have greater deficits in problem-solving skills due to low health literacy60, as well as lower educational levels and limited access to educative programs44, predisposing them to more depressive symptoms. However, problem-solving literature in HF caregivers is scarce, and, thus far, no prior studies have evaluated problem solving in rural HF caregivers. Therefore, more research is needed to examine its influence on rural HF caregiver outcomes and determine its usefulness for interventions in this population.
Problem solving and caregiver burden
This study’s findings are consistent with the parent analysis and prior studies using both urban61,62 and rural caregiver populations53,62, showing that caregiver burden declined as problem-solving skills improved. A perceived lack of time, limited availability of resources, and an unwillingness to ask for assistance from others are factors contributing to both urban and rural caregivers’ hesitancy in seeking assistance from others. However, studies suggest caregivers more effectively manage physical, psychosocial, family, and financial caregiving stressors when using problem-solving skills and resources53,61,62. For example, using a quasi-experimental design, stroke caregivers using modules with small-group-guided discussions and problem-solving skills training reported significant reductions in caregiving burden and improved life changes over 6 months63. Theoretical principles suggest that caregivers using these strategies to manage common problems will appraise caregiving situations objectively and cope more effectively in managing caregiving stressors in the home19, but more research is needed to evaluate this assumption.
Family functioning and life changes, self-care, and burden
The parent study using both urban and rural caregivers did not examine the role of family functioning on study outcomes. However, family is an important component of rural lifestyle64; thus, it is not surprising that family functioning affected caregiver outcomes in this analysis. Family functioning had significant effects on caregiving-related life changes, self-care, and caregiver burden. Few HF caregiver studies have examined the influence of family function, and to the authors’ knowledge this is the first study involving rural HF caregivers to do so. However, studies on other populations (such as people with schizophrenia) found a significant relationship between family functioning and quality of life in physical, psychological, social, and environmental domains65. Other studies support family cohesion, satisfaction, and quality of family communication as lessening caregiver burden, whereas disengagement increases caregiver burden66. These findings underline the importance of family relations in evaluating caregivers who care for patients with HF. Significant correlations with family functioning and these caregiver outcomes also highlight the importance of further studying and examining the effectiveness of interventions for treating life changes, self-care, and caregiver burden within the context of family relations.
Implications for practice
In rural communities, the use of community or lay health advisors to provide individualized suggestions and strategies may improve caregiver outcomes. Educators, community and religious leaders, and other stakeholders, such as nurses, family counselors and therapists, nurse practitioners, social workers, and mental health providers, could develop information regarding common caregiving issues and available support services and resources for caregivers. For example, social workers can provide resources for accessing social, financial, transportation, and volunteer and in-home support services in rural communities.
Trained community or peer health advisors who have experienced similar problems could follow caregivers over time and offer social support and useful information and suggestions to assist with problem identification and management through the use of personal networks and community engagement models67, using a range of formats (eg both telecommunications and face-to-face contacts)68. Health providers work together with these trained peer health advisors who live in rural communities to identify available resources and companionship, material aid, and emotional support services to meet the needs of rural family caregivers. Assessment of family functioning, with referrals to family counselors and mental health therapists for counseling and therapy also are important services. Caregivers also may need appointments with physicians, nurse practitioners, and other healthcare providers for declining self-care. These services emphasize the interrelation among social support, problem-solving, and family functioning as resources by assisting families in identifying sources of conflict and strategies for resolution, setting mutual caregiving goals, and using family member strengths to work on identified problems together.
Limitations and future research
Although this study provides new information about rural HF caregivers, there are some limitations that must be addressed. First, this study primarily included younger, Caucasian caregivers with higher educational levels, who may not be as representative of caregivers living in rural communities. Given that 84.2% of our sample were Caucasians compared to 77.8% in rural populations, future studies examining rural populations of color (eg Hispanics, African Americans) are essential. On average, caregivers mostly cared for patients with HF who had less severe HF and no comorbidities, potentially influencing study outcomes. Findings from a large literature review suggests that HF caregivers are more likely to report depressive symptoms and caregiver burden when providing care for patients with more severe HF and worse physical health2. Caregivers also responded to an online questionnaire and self-identified as being a HF caregiver. While recommended empirical strategies were used to verify the accuracy of caregiver status and the validity of collected data, it is plausible some participants may not have been HF caregivers. Binary classification of rurality must be recognized. While multiple criteria are used by the RHIH tool17 for classifying rurality, factors such as changes to census methodologies and population growth and the presence of rural areas within metropolitan counties may influence the accuracy of a rural/urban classification. These factors also were an issue for classifying participants living in areas other than the USA. More research is needed to evaluate the influence of social support, problem solving, and family function on rural HF caregiver outcomes to inform future intervention strategies that target quality-of-life outcomes for this population.
Conclusion
This study provides evidence that both social support and problem solving have significant effects on depressive symptoms in rural HF caregivers, while social support and family function influence self-care. Problem solving and family function also affect caregiver burden, while social support and family functioning influence caregiver life changes. There are few studies examining these variables in rural populations, so this represents an area needing further exploration. Rural caregivers are often separated by long distances, and have transportation issues, and limited access to healthcare providers and support services; therefore, innovative strategies are needed to explore the usefulness of these variables in improving caregiver outcomes.
References
You might also be interested in:
2021 - COVID-19 in a rural health system in New York – case series and an approach to management



