Introduction
Patients suspected of having had an acute stroke require rapid assessment with brain imaging to guide further management. Reperfusion therapy with intravenous thrombolysis and mechanical thrombectomy are optimal treatments for the most common type of stroke, acute brain ischaemia, but both must be delivered within hours of symptom onset. However, only 10% of patients actually receive thrombolysis1 due to various pre-hospital and intra-hospital delays2. Thrombectomy can currently only be provided in specialised centres with dedicated neurointerventional facilities, and correct identification of patients that would benefit from direct transfer would optimise clinical outcomes cost-effectively.
Patients who live in remote and rural areas are at particularly high risk of not receiving reperfusion therapy due to long transport times and lack of opportunities for direct access to diagnostic imaging facilities. As previously demonstrated, clinical assessment of patients in rural areas can be supported by secondary care specialists while en route to the hospital with live transmission of audio and video data. This could potentially facilitate management upon arrival at a healthcare facility and improve outcomes3-5.
The management of patients suspected of having had an acute stroke would improve if there was a basic imaging tool in place that could be used by rural general practitioners (GPs), paramedics or community nurses to help make treatment decisions. Transcranial ultrasound can be used for assessment of blood flow in the major intracranial vessels in order to detect steno-occlusive lesions6,7 and to detect intracranial haemorrhage in the central structures, such as the basal ganglia8, which can also cause midline shift of brain structures9. Neurovascular examination with portable transcranial colour-coded duplex sonography (TCCS) is a rapid, relatively inexpensive and non-invasive assessment that can be carried out with technology available in many primary care settings. However, it is important to ensure that transcranial ultrasound operators are adequately trained if their assessment results are to be used to guide further management. Thus, a short training package has been previously proposed by Klinzing et al (2015) for training inexperienced ultrasound operators to perform TCCS 10.
The authors of the present study hypothesised that novice transcranial ultrasound users could perform a complete transcranial ultrasound assessment through the temporal bone window and acquire a set of images and video clips suitable for expert interpretation after a 3-hour training package. The aim was to investigate whether the inexperienced operators could capture the midline, cerebral peduncles, major brain arteries forming the circle of Willis and calculate blood flow velocity in the middle cerebral artery (MCA). In addition, feedback from participants was collected to assess their perspective on the overall experience after training.
Methods
This pilot training project was executed in a university setting in Inverness, Scotland. Actual field testing was not part of this work.
Participants
Adult (aged 18 years and over) male and female healthy volunteers who were qualified clinicians or students of nursing or medicine with no practical experience in transcranial ultrasound were recruited in May–July 2019.
Training package
Transcranial ultrasound scanning of healthy volunteers was performed through the temporal bone window using a SonoSite M-Turbo® Point-of-Care ultrasound machine and a 1–5 MHz low-frequency phased array transducer. Volunteers were asked to remain in a sitting position throughout the scan. Participants received three 1-hour training sessions combining theoretical aspects and hands-on practice on healthy volunteers. All three training sessions were provided by a single trainer, a qualified neurologist with more than 2 years of experience in transcranial ultrasound. Transcranial greyscale and colour-coded duplex sonography was performed to:
- visualise the midline structures and the opposite skull bone in the transverse plane using greyscale in order to identify the temporal bone window sufficiently for interpretation of findings
- make three consecutive measurements of the midline as a distance from the third ventricle to the ipsilateral skull and calculate the midline shift as reported previously11. Midline shift in suspected stroke patients might suggest a space-occupying haemorrhagic or ischaemic lesion. It has been reported to be a reliable indicator of intracranial haemorrhage with a significant correlation between haemorrhagic focus volume and midline shift8,9
- visualise the cerebral peduncles to localise the circle of Willis anteriorly
- visualise the major intracranial arteries comprising the circle of Willis bilaterally using TCCS. MCA was identified as orthograde blood flow at an insonation depth of 40–65 mm and 30–40 mm for proximal (M1) and distal (M2) segment, respectively. The anterior cerebral artery (ACA) was detected as retrograde flow at a 60–75 mm insonation depth. The posterior cerebral artery (PCA) was visualised as orthograde (P1 segment) or retrograde (P2 segment) at 55–75 mm depth12
- calculate the mean blood flow velocity in the MCA as described previously13.
Training session 1 was aimed at learning steps 1–3, training session 2 at steps 4 and 5, and session 3 at steps 1–5. Participants were given an opportunity to perform scanning on two to three healthy volunteers during all three sessions, including self-scanning.
Quality assessment of acquired images and video clips
Within 1 week of the third training session, participants were asked to perform an unsupervised complete transcranial ultrasound scan (steps 1–5) on a healthy volunteer, being assessed on the basis of the acquired set of images and video clips. The time required to complete scanning was recorded, but the maximum allowed time was 1 hour. The quality of video-recording in the transverse plane was assessed by the trainer using the visual analogue scale (VAS) from 0 to 5, where 0 indicated that the acquired video clip did not allow interpretation and 5 represented a high quality video clip. This part was essential for confirming that the novice operators had achieved the required skill level. A participant’s ability to capture the intracranial structures of interest was assessed as correctly labelled, incorrectly labelled or not identified.
Qualitative feedback from participants
As a final step, all participants were asked to anonymously comment on their experience by completing a feedback form and answering multiple-choice and closed questions about the easiest or most challenging part of the training, how confident they felt and how they would rate their overall experience (Appendix 1).
Finally, participants were asked to provide any comments or suggestions, for example if they would like to suggest any changes to the training package.
Data analysis
A narrative synthesis was applied, structured around the assessment results and qualitative feedback from the participants.
Ethics approval
This study was granted ethics approval from the University of Aberdeen’s College of Life Sciences and Medicine Ethics Review Board (ID 1669) and was also approved by the National Health Service Highland Research Management (ID 1521).
Results
Eleven volunteers with no prior experience in transcranial ultrasonography were recruited. Time to complete a full transcranial ultrasound assessment ranged from 29 minutes to 47 minutes (median 38 minutes, interquartile range 36.0–43.5 minutes).
Quality assessment of acquired images and video clips
The capture rates for the intracranial structures of interest are presented in Table 1.
Midline was correctly identified and measured in 64% of cases (by 7 participants out of 11), with 36% (4/11) being incorrectly labelled. The majority of participants (91%, 10/11) correctly identified brainstem with only 9% (1/11) incorrect labelling. In 3/11 cases (27%) it was technically difficult for novice ultrasound users to identify the MCA and ACA. The correct labelling rates were 73% (8/11) and 64% (7/11) for the MCA and ACA, respectively. In 1 of 11 cases (9%), the ACA was incorrectly identified based on the blood flow direction. The incorrect labelling rate was the highest for the PCA, at 18% (2/11).
The quality of greyscale ultrasound scans in the transverse plane varied from 0 to 5 on VAS with a mean value ± standard deviation of 3.8±1.6. No participants had insufficient temporal acoustic window.
Table 1: Transcranial ultrasound capture rates for intracranial structures of interest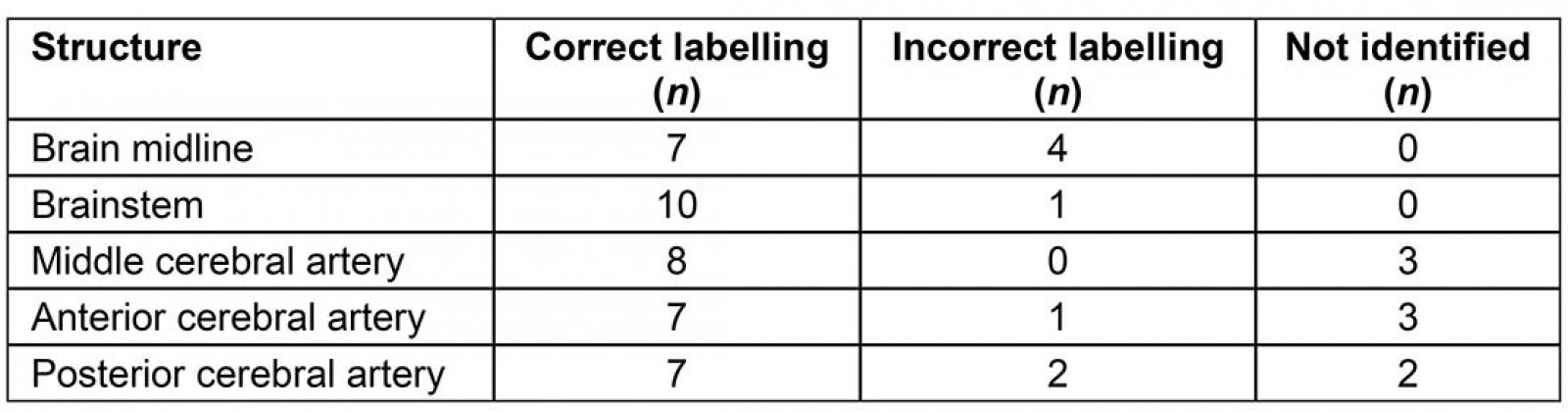
Qualitative feedback from participants
A total of 82% (9/11) participants rated their experience during the training sessions highly (5 out of 5). One participant commented, ‘Excellent. Good content and well explained’. From the volunteers’ perspectives, the right amount of time was allocated in order to acquire the new skills; however, the general feedback suggested more practice and follow-up sessions would be needed to maintain the newly acquired skills: ‘More practice needed to feel confident about reliably performing a … TCUS [transcranial ultrasound scan]’; ‘More practice would be better (more subjects [healthy volunteers to scan]?)’.
As demonstrated in Figure 1, about 45% of participants (5/11) found greyscale transcranial ultrasound the easiest part of the training, and 36% volunteers (4/11) thought that imaging of the major intracranial vessels using TCCS was the least challenging.
Figure 2 illustrates that 73% of participants (8/11) rated the transcranial ultrasound assessment scanning as the most difficult part. The remaining 27% of volunteers (3/11) said that greyscale transcranial ultrasonography was more complicated.
One of the highlighted challenges for novice users was technical difficulties associated with operation of the ultrasound machine at the same time as maintaining the probe’s position (‘difficult to use both hands’).
Using VAS, 55% of volunteers (6/11) rated their confidence level when performing a complete transcranial ultrasound assessment as 3 out of 5, whereas 45% of inexperienced operators (5/11) rated it as 4 out of 5. Participants’ opinions regarding the quality of the acquired images and video clips on a scale from 0 to 5 varied from 2 to 4, with 45% of participants (5/11) rating the quality as 3 (satisfactory, just enough for someone to interpret it) and another 45% rating it as 4. One participant (9%) rated the quality of their images and video clips as 2.
All volunteers thought that this training package could be used for GPs, paramedics and other clinical staff working in remote and rural areas, with one pointing out, ‘Maybe could use it on our placement or work place to keep updated with it. Better suited for community nurses, GP etc. as they can do it all the time’.
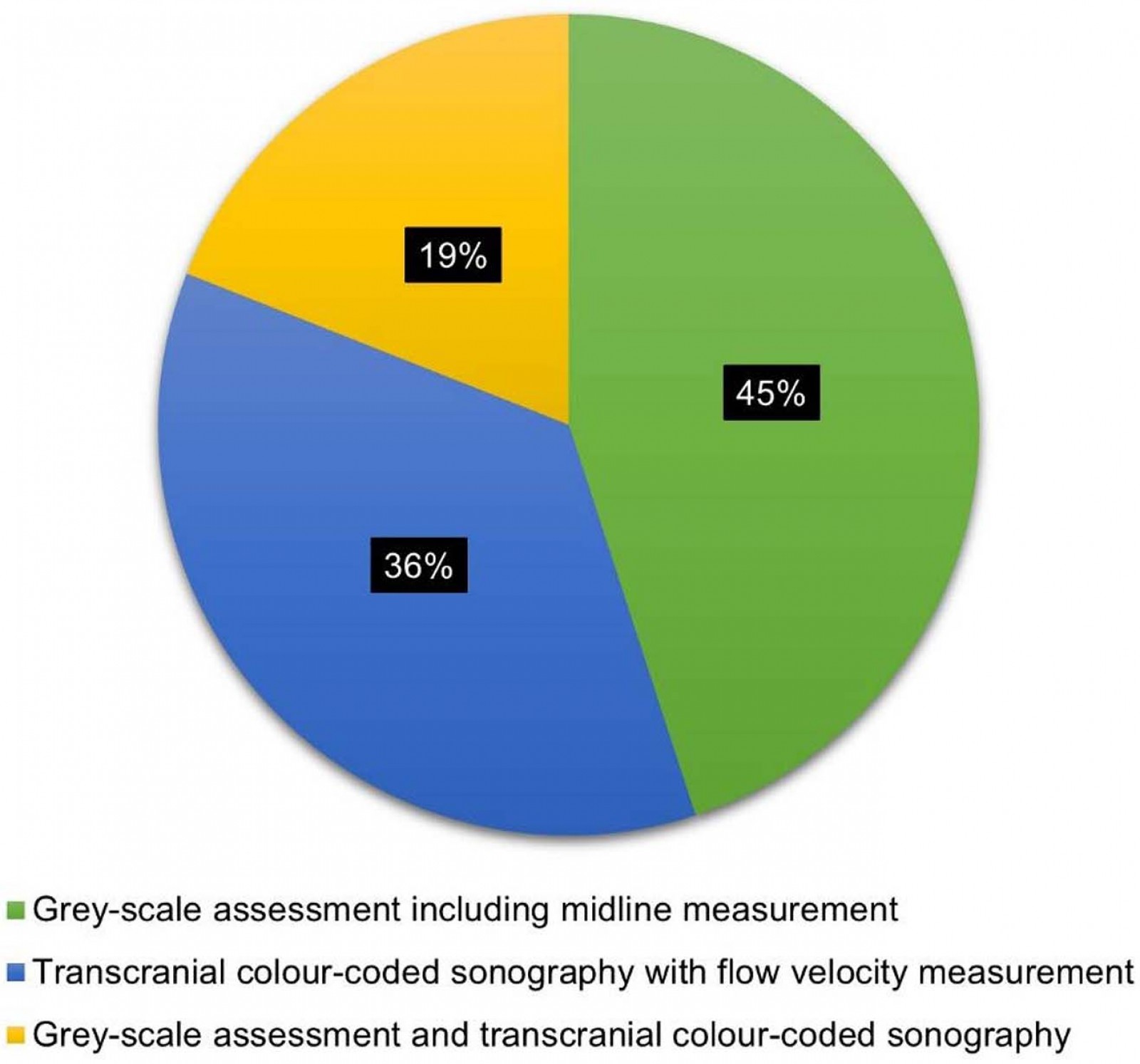 Figure 1: Proportional representation of qualitative feedback from participants on the easiest part of training.
Figure 1: Proportional representation of qualitative feedback from participants on the easiest part of training.
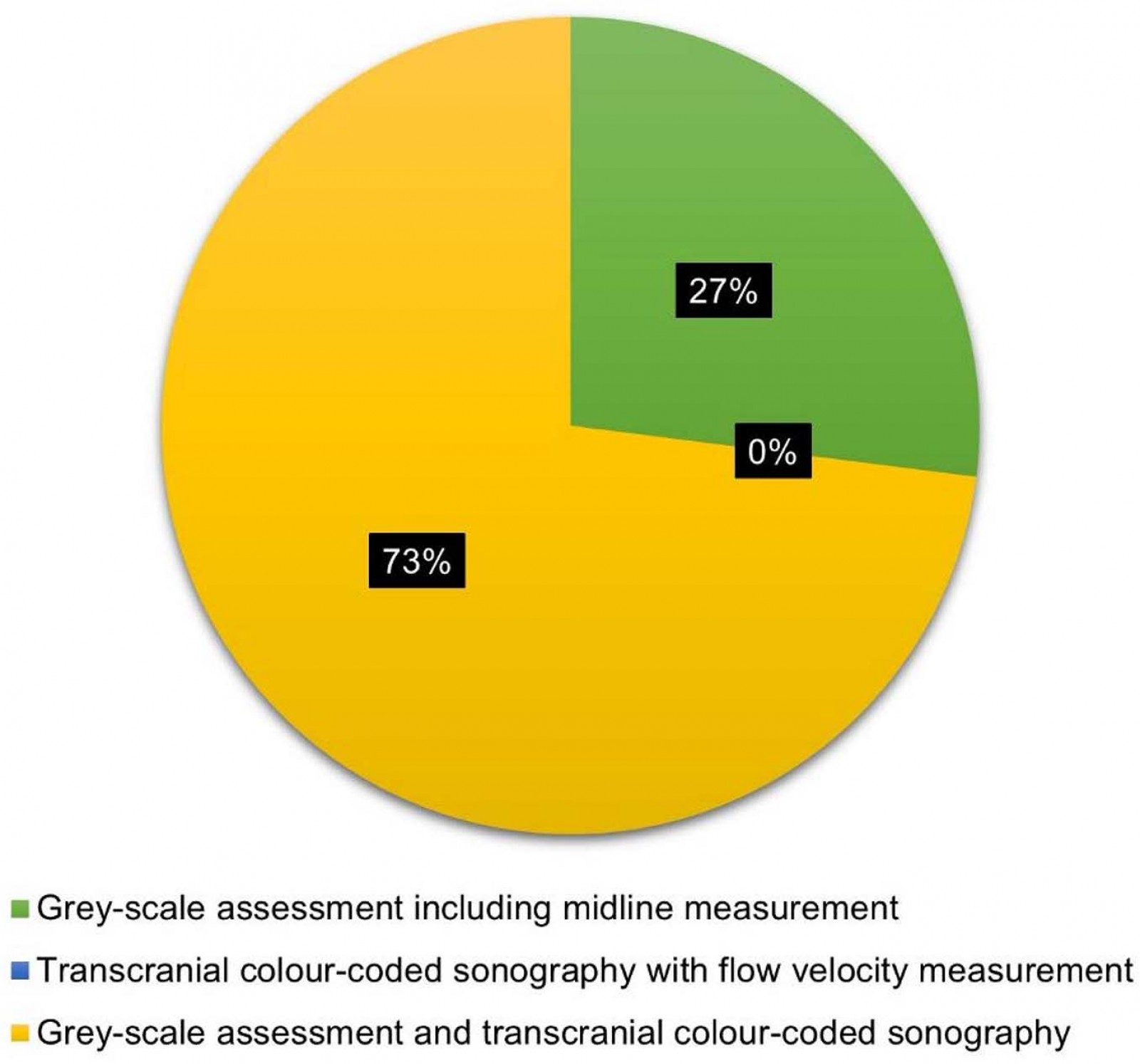 Figure 2: Proportional representation of qualitative feedback from participants on the most challenging part of training.
Figure 2: Proportional representation of qualitative feedback from participants on the most challenging part of training.
Discussion
As previously demonstrated by this research group, basic transcranial ultrasound examination of patients in rural areas can be performed by inexperienced operators guided and supported by secondary care specialists using live transmission of audio and video data3-5. In the present study a brief training package for novice users with a potential application for medical staff working in remote and rural areas has been proposed. The overall quality of images and video clips acquired by novice operators was demonstrated to be satisfactory to allow expert interpretation. The trainer and the participants gave their images similar quality rating using VAS reaching an agreement. Both midline shift and the brainstem were correctly labelled in the majority of cases. Participants demonstrated good performance in detecting major intracranial vessels. Among the three major intracranial arteries of interest, ACA and MCA were technically more difficult to capture, with the highest rate of non-identification (3/11, 27%). The PCA was incorrectly labelled in a bigger proportion of cases than the ACA and MCA (2/11, 18%).
In a previously published study by Klinzing et al (2015), six inexperienced TCCS operators measured the mean flow velocity in the MCA in 10 healthy volunteers after participating in an introduction session. The introduction covered the basic anatomy of the brain and intracranial vessels as it is visualised using TCCS, technical characteristics required to operate the ultrasound machine and finding the adequate temporal acoustic window. The inexperienced TCCS users then observed one transcranial sonography examination performed by an experienced operator and were given a chance to perform one or two supervised assessments. Thereafter, three operators had active supervision while performing all 10 scans, and the other three participants were supervised only during their first five transcranial examinations. Measurements were compared with those obtained by two TCCS users who completed formal training and had at least 2 years of experience. The results of the present pilot study are in agreement with the findings published by Klinzing et al (2015), which showed that examination of the major brain vessels using transcranial ultrasound can be easily achieved with supervision during initial examinations10.
Neulen et al (2013) showed that even experienced transcranial Doppler ultrasound users (6 months to 20 years of experience) tend to misinterpret up to 37% of the major intracranial arteries. The accuracy of the study might be particularly limited in case of anatomical or pathological variation of the vessels or repositioning by a space-occupying lesion (large haemorrhage, tumour, etc.)14. This limitation might result in misinterpretation of the scans and lead to false management decisions. The auto-pilot software tool (image guidance) for inexperienced transcranial Doppler ultrasound users among medical students resulted in improved accuracy of interpretation of Doppler findings by 27% within a 10-minute limited study14. In addition, image guidance assisted in interpretation of transcranial Doppler data in more complex cases, such as anatomical variation of the MCA and insonation through a burr hole after a craniotomy14. Future work is required to overcome user dependency, which is currently one of the main barriers to the wide implementation of transcranial ultrasonography as a diagnostic tool.
Another technical limitation of transcranial ultrasonography is inadequate acoustic window, which occurs in 8–29% of the general population15, or inability to visualise brain structures of interest. Inadequate acoustic window is most frequently detected in women aged over 50 years and in people who are Asian16. Temporal acoustic window was adequate in all healthy volunteers who participated in the present study, which is not surprising and is probably due to their young age.
Participants gave positive feedback on the training materials and time allocated for learning. Transcranial greyscale ultrasonography was rated by 45% of participants (5/11) as technically the easiest part among all training sessions. The complete transcranial assessment containing all the individual parts, such as greyscale ultrasonography and TCCS, was considered the most challenging. This may be because inexperienced operators did not receive any supervision during the final assessment session and probably felt least confident at that time.
In the present study the average time required for a complete examination, including assessment of the intracranial vessels, was approximately 40 minutes. Previously it has been shown that the time to acquire images of midline measurements of sufficient quality increased by approximately 52% in hands of operators who were initially unfamiliar with transcranial ultrasound5. Mikulik et al’s (2006) bedside study demonstrated that telemedicine-guided transcranial Doppler ultrasound examination performed by a novice ultrasound user led to a substantial increase, of 27 minutes, in assessment time17.
Endovascular treatment is a minimally invasive and effective reperfusion therapy for patients with acute ischaemic stroke due to large vessel occlusion1. Mortality rate in this group of stroke patients can be as high as 80%18, and shorter time to endovascular reperfusion is associated with better clinical outcome19,20. Therefore, the focus of current care has been shifted to consider accurate selection of patients who would benefit from mechanical thrombectomy as it can only be offered in specialised centres with neurointerventional facilities.
In remote and rural areas, non-specialist pre-hospital practitioners, such as GPs and paramedics, currently have to decide whether to transfer a patient with suspected stroke to a local hospital that can only offer intravenous thrombolysis or to arrange longer and costly travel to a regional centre offering mechanical clot retrieval. Travel time between the local and regional hospital should be considered: if the travel time is long (90–120 minutes), the ‘drip and ship’ model (thrombolysis followed by a transfer for mechanical thrombectomy) would be favoured over the ‘mothership’ strategy (direct transfer to the endovascular centre)21.
A number of clinical assessment tools have been proposed to serve this purpose22 but their diagnostic accuracy is currently insufficient: at least 20% of patients with large vessel occlusion would be incorrectly transferred to a local hospital with no neurointerventional facilities available23. Added transcranial ultrasound information on presence or absence of intracranial haemorrhage and blood flow within the major arteries could potentially improve diagnostic performance to allow more accurate triage. According to the literature, sensitivity of transcranial ultrasound in detecting stenosis and occlusion of the major brain vessels ranges from 68% to 100%24. It is a relatively inexpensive and widely available diagnostic tool in comparison to other imaging tests, such as brain CT 25, that might have potential application in countries where there are remote and rural areas with long transport times.
It is likely that potential transcranial ultrasound users in remote and rural areas – such as rural GPs, paramedics and community healthcare professionals – will have infrequent exposure to suspected stroke patients in comparison to medical staff working in urban areas. It would therefore be important to ensure that the acquired knowledge and skills are maintained because even experienced users can get less accurate measurements when using transcranial Doppler ultrasound relatively infrequently26. One of the limitations of this pilot work was absence of any follow-up assessment to determine the retention rate of acquired skills, for example, short-term (after 1 week and/or 1 month) and long term (3–6 months after the initial training). This should be incorporated in the study protocol in the future. Further regular follow-up training, with possible supervision, would be required to help novice users build up confidence, improve technical skills and ensure that acquired skills are retained.
Further assessment with a larger sample size is required to support the application of the proposed training model. Future work is needed to validate this training package for stroke patients. It would be important to investigate whether the proposed training can be provided to medical staff working in remote and rural areas to help them make treatment decisions for patients suspected of having had an acute stroke. In pre-hospital settings, initial and follow-up training as well as support during assessment of acute stroke, aided by real-time transmission of images, could be provided remotely by hospital-based experts as reported previously3-5,27.
Conclusion
This pilot study demonstrated that a brief training package can be used to train inexperienced transcranial ultrasound operators to acquire diagnostic images and video clips that would allow expert interpretation. Positive feedback from the volunteers was provided on the package content and time given to learn this new technique. The developed program could potentially be used for training of remote and rural medical staff and could improve acute care, specifically for suspected stroke patients, by facilitating treatment decisions and triaging patients to the hospital that can offer the most appropriate treatment, such as mechanical thrombectomy. Future research on a larger sample, potentially involving stroke patients, is needed.
References
appendix I:
Appendix I: Participant feedback form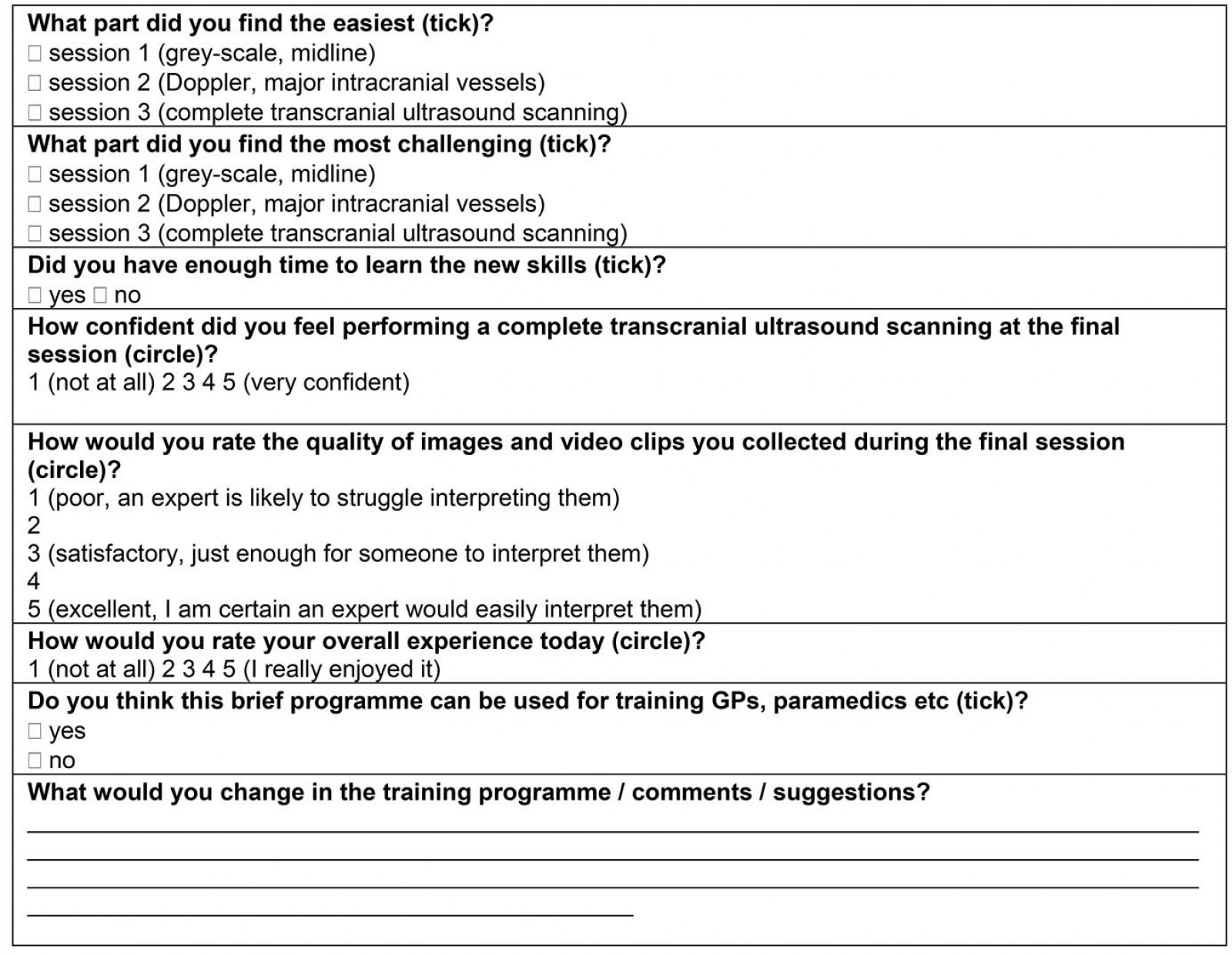
You might also be interested in:
2005 - A database to record, track and report health student rural placements
