Introduction
Health inequities among different population groups are an important public health challenge, causing significant burden on the social and economic structure of countries1. Such inequities hint at the suboptimal use of resources and an insufficient reach of healthcare delivery to those most vulnerable2,3. The root cause of most health inequities is social factors, such as place of residence, education, employment and income, and health inequities can result in mismanagement of chronic disorders, with increased morbidity and mortality1,2.
The International Diabetes Federation considers type 2 diabetes to be one of the most prevalent non-communicable diseases worldwide4, itself causing significant morbidity and mortality and negative economical and societal impacts5,6. Type 2 diabetes affects an average of 8.5% of the European population aged 20-79 years, with figures showing a trend of increasing prevalence4. Multiple studies have studied the bidirectional relationship of type 2 diabetes and depression, reporting an increased prevalence of depression in patients with diabetes and an association with worsening diabetes control and increased diabetes-related complications7.
Type 2 diabetes is a highly prevalent chronic condition in the Maltese archipelago, a small European island state situated in the central Mediterranean8. The archipelago consists of the mainland of Malta and the smaller sister island of Gozo, with a total area of 316 km2 and a population of about half a million people. The population inhabits 68 settlements spread across the islands9, with these being further divided into four major areas: the South, Central, North and Gozo. A large proportion of these settlements, especially those in the South and Central areas of Malta, merges to form a large conurbation and creates the urban centre of the islands, while settlements in the North area and Gozo are more likely to be separated by countryside, giving these areas more suburban characteristics1,10.
The public primary healthcare system in Malta is free of charge at the point of care and is available at all times from nine governmental health centres in Malta and another centre in Gozo. Private GPs work in community retail pharmacies or in their own private clinics with no official patient registration system. A national, descriptive, cross-sectional study showed that patients in the private sector experienced better continuity of care than patients in the public sector; however it reported more difficulty in accessing out-of-hours care11. Diabetes clinics are carried out in the public primary healthcare centres in Malta by specialised GPs, as the vast majority of patients with diabetes are followed up in the primary healthcare setting. A referral system to hospital specialists is in place for patients whose diabetes is uncontrolled as per the Diabetes Shared Care Programme Protocol12.
Despite Malta enjoying a relatively good health profile13, the prevalence of type 2 diabetes in the Maltese islands is one of the highest in Europe, with 13.2% of the population between the ages of 20 and 79 years suffering from the condition2, and a further 10 000 people unaware that they have the disease8. Estimations indicate that type 2 diabetes costs the country about 3.64% of the total health expenditure8. Chronic depression affects about 5.3% of the population, with projections indicating that it costs the country about 4% of the gross domestic product14.
Due to the relative social homogeneity expected in a small, densely populated island state, urban–suburban health inequities may not be expected, but as Agius delineated in his descriptive exposition review on social and health inequities in 1990, social inequities have contributed to differences in the overall health status of the population across different regions of Malta. This was especially significant with the prevalence of infectious diseases that were found to be more common in the south-eastern region of Malta and Gozo at the time1.
This study aimed to identify patients with type 2 diabetes with depression. The objective was to study the urban and suburban differences that might be associated with the demographic, socioeconomic and clinical pictures of patients with diabetes that might contribute to health inequities.
Methods
A quantitative, retrospective, descriptive study was carried out on a convenient sample of patients attending the three main diabetes outpatient clinics in the northern, central and southern regions of Malta between June and September 2018. All consenting subjects older than 18 years with an established diagnosis of type 2 diabetes4 who attended the designated clinics for their appointment during the period of recruitment and did not require emergency care were invited to participate. Participants who were excluded included those not consenting to participate, having a diagnosis of diabetes other than type 24, having cognitive impairment, being unable to perform the study, attending other clinics at the health centre, or attending the diabetes clinic in Gozo. The data were collected via a self-administered questionnaire with no study-specific interventions carried out. Participants provided consent prior to participating in the study.
The Patient Health Questionnaire-9 (PHQ-9) was used as the validated tool to measure depression15, with patient sociodemographic and disease characteristics collected by a questionnaire developed by the author. The questionnaires were translated to Maltese and peer-reviewed to reduce translation errors. A pilot study involving 17 subjects was carried out in a separate health centre to test the relevance and comprehensibility of the questionnaires. Questions regarding the process that were addressed included, for example, ‘How long does it take to fill in the questionnaire? Are patients easily recruited?’ By testing comprehensibility of the questionnaires, several questions were answered, for example, ‘Are the instructions understood by all respondents?’ For the closed questions, are all reasonable alternatives included for the respondents? This led to recording the reported capillary blood glucose test rather than the last HbA1c result because patients were unable to recall the latter.
The tool used to quantify depressive symptoms, the PHQ-9 questionnaire, was chosen because it can be used both to assess the severity of depression in known cases and make a diagnosis of depression in at-risk populations15. This tool asks participants to score response categories with a scale of 0, 1, 2 and 3 (corresponding to ‘not at all’, ‘several days’, ‘more than half the days’ and ‘nearly every day’ respectively). The scores are then computed, with the final score categorised in one of the following depression categories: 0–4 (none), 5–9 (mild), 10–14 (moderate), 15–19 (moderately severe) and 20–27 (severe depression)15.
Personal data such as name, identification number and contact telephone number were not recorded. The localities of patient health centre attendance were noted. The urban cities and suburban towns were defined as considered in the European Urban Health Indicator System project, relying on the categorisation made by local experts16.
The variables studied in the context of the participant place of residence included age, gender, nationality, marital status, highest level of education, employment status, monthly income, smoking status, subjective weight assessment, family history of diabetes and depression, and information about the diabetes status of the study subjects. The last was assessed by recording the years spent with diabetes, the medication used and medication compliance, the subjective and objective diabetic control and the presence of co-morbidities and diabetic complications. Obesity was assessed subjectively, as patients were asked to categorise themselves as of ‘normal weight’, ‘slightly overweight’ or ‘obese’, whereas a capillary blood glucose test of 10 mmol/L was taken as the cut-off point for the objective diabetic control. These data were anonymised and stored accordingly.
Descriptive analysis and statistical testing were carried out using the Statistical Package for the Social Sciences v25.0 (SPSS; www.spss.com). Pearson’s χ2 and Fisher’s tests were used to assess the association between the region of residence and the variables mentioned, while logistic regression analysis was used for the variables that showed statistical significance when tested against the region of residence to adjust for confounding factors. These included monthly income, subjective weight assessment, nationality and PHQ-9 depression score variables. A p-value of <0.05 was used to signify statistical significance. No sub-group analysis was carried out.
Ethics approval
Ethical approval was obtained from the University Faculty Research Ethics Committee of the University of Malta (reference number 58/2017) and the Data Protection Officer of the Primary Health Care Department.
Results
There were 142 participants recruited from the suburban outpatient clinic, and 306 participants recruited from the urban outpatient clinics, with an overall response rate of 89.3%. There were no missing data recorded during data collection. The mean age of the participants was 69 years. Men made up the majority of participants (n=216, 54%) and they smoked more, were less compliant to medication and had worse glucose control. Women were generally older, more obese and more likely to be widowed, worked at home, had a lower income and had received basic education. Hypertension and dyslipidaemia were more common in women, while myocardial infarction and cerebrovascular accidents were more prevalent in males. The prevalence of depression among patients with diabetes was 29.7%, with women having a higher prevalence (37%) than men (23.6%). Statistically significant differences between the genders were found for marital status, education level, employment status, smoking status and the presence and severity of depression (Table 1).
Examination of the factors according to urban–suburban residence revealed a statistically significant association with severity of depression, nationality, monthly income, subjective weight assessment, and degree of control of diabetes. Residents in urban regions had a significantly higher prevalence of moderate, moderately severe and severe depression than their counterparts in suburban areas (Fig1). Urban residents reported an overall higher income, and there were proportionally more non-Maltese participants in the suburban region. Subjective overweight and obesity were more prevalent in the suburban region, with a higher rate of reported uncontrolled diabetes than their urban counterparts. Urban participants were less likely to know the result of their capillary blood glucose test than participants in the suburban region (Table 2). Age, gender, marital status, education level and employment, smoking status, presence of a family history of diabetes and depression, years with diabetes, medication use and compliance, perceived diabetes control and presence of co-morbidities and diabetic complications were not significantly associated with the place of residence.
Logistic regression was performed to assess the impact of a number of different patient-reported factors on the likelihood that these occur in those patients with diabetes living in suburban regions as opposed to those living in urban areas (Table 3). The model contained five independent variables (severity of depression, monthly income, blood capillary glucose readings, weight and nationality). The full model containing all predictors was statistically significant, c2 (5, n=400), p<0.001, indicating that the model was able to distinguish between urban and suburban areas. The model as a whole explained between 10% (Cox and Snell R2) and 20% (Nagelkerke R2) of the variance in urban and suburban areas, and correctly classified 73.8% of cases.
As shown in Table 3, all five independent variables made a unique, statistically significant contribution to the model. Elevated blood glucose and obesity tended to be more prevalent in suburban respondents than in urban participants. Conversely, participants with diabetes living in urban areas were more likely to be severely depressed, be Maltese and have a higher income.
Table 1: Overview of statistically significant participant characteristics according to gender15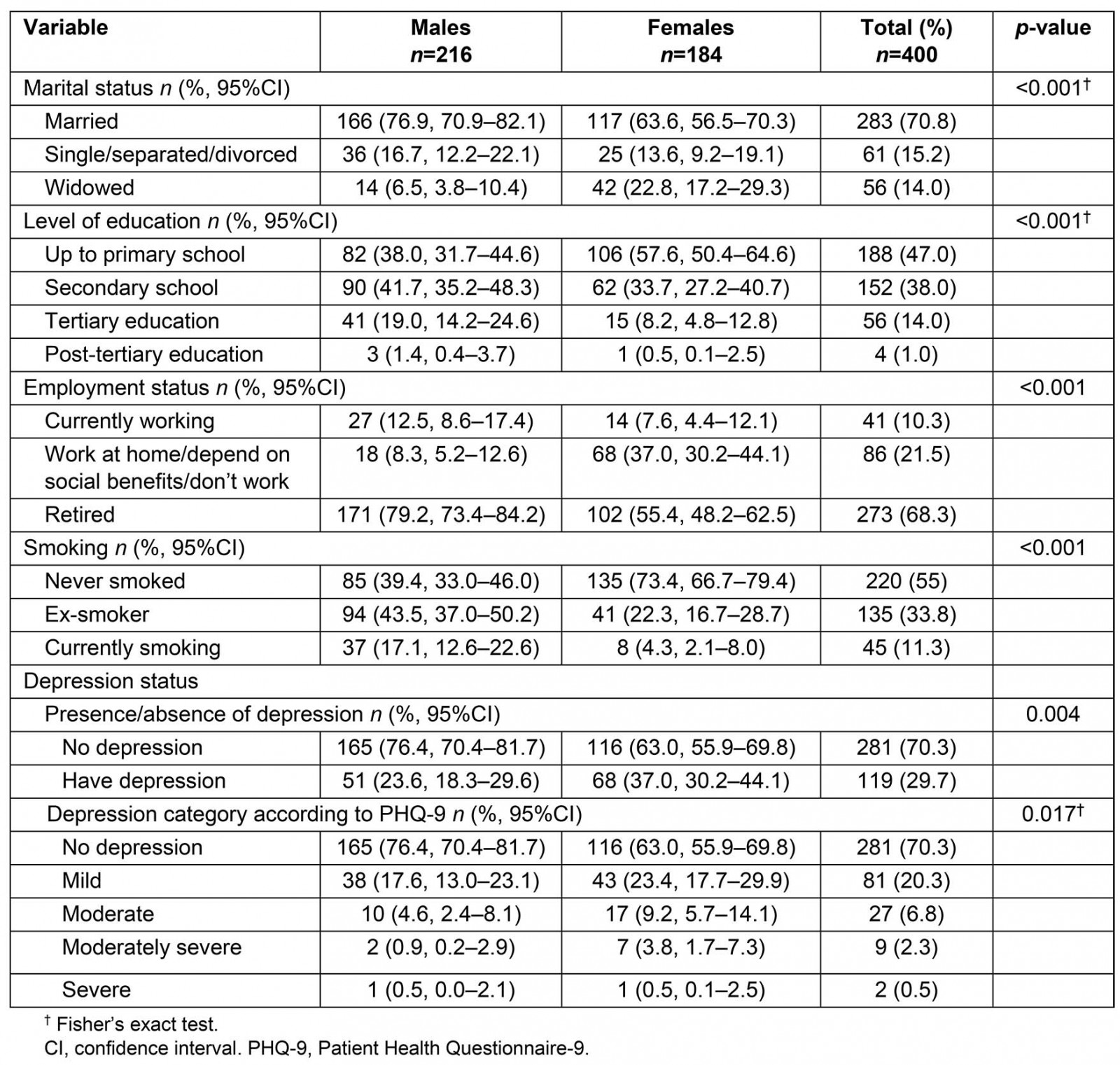
Table 2: Overview of the statistically significant participant characteristics according to place of residence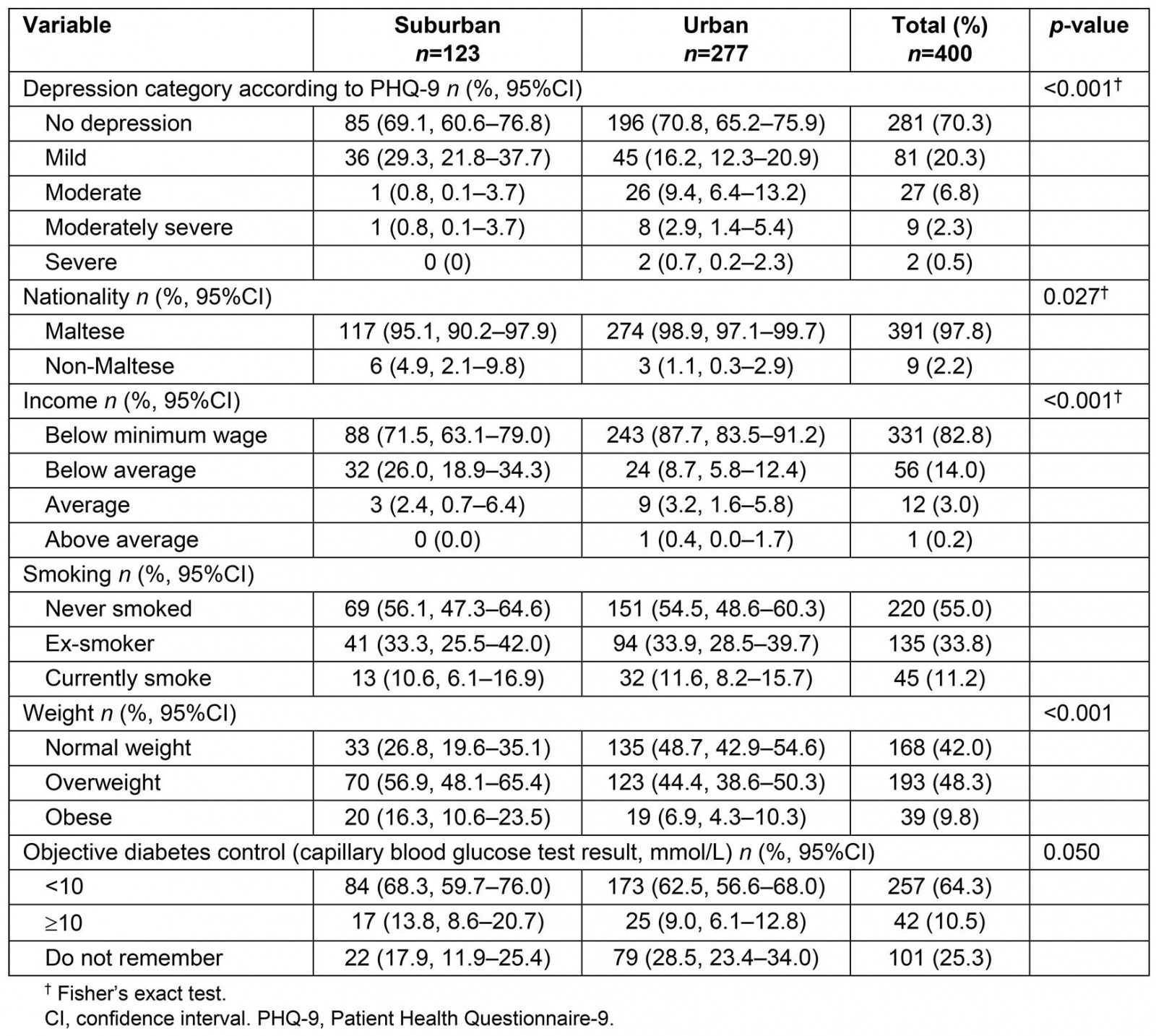
Table 3: Logistic regression analysis of statistically significant variables in urban and suburban regions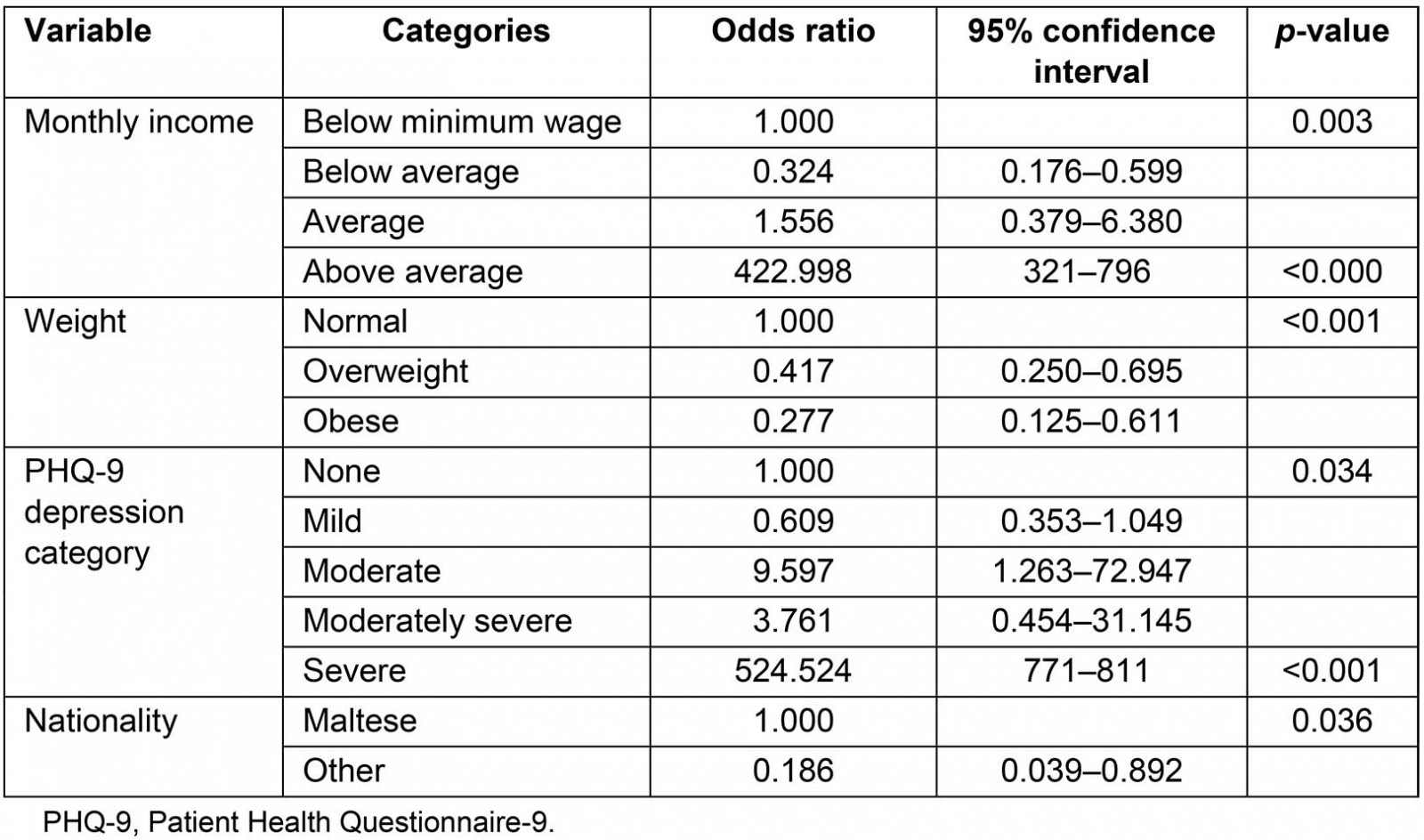
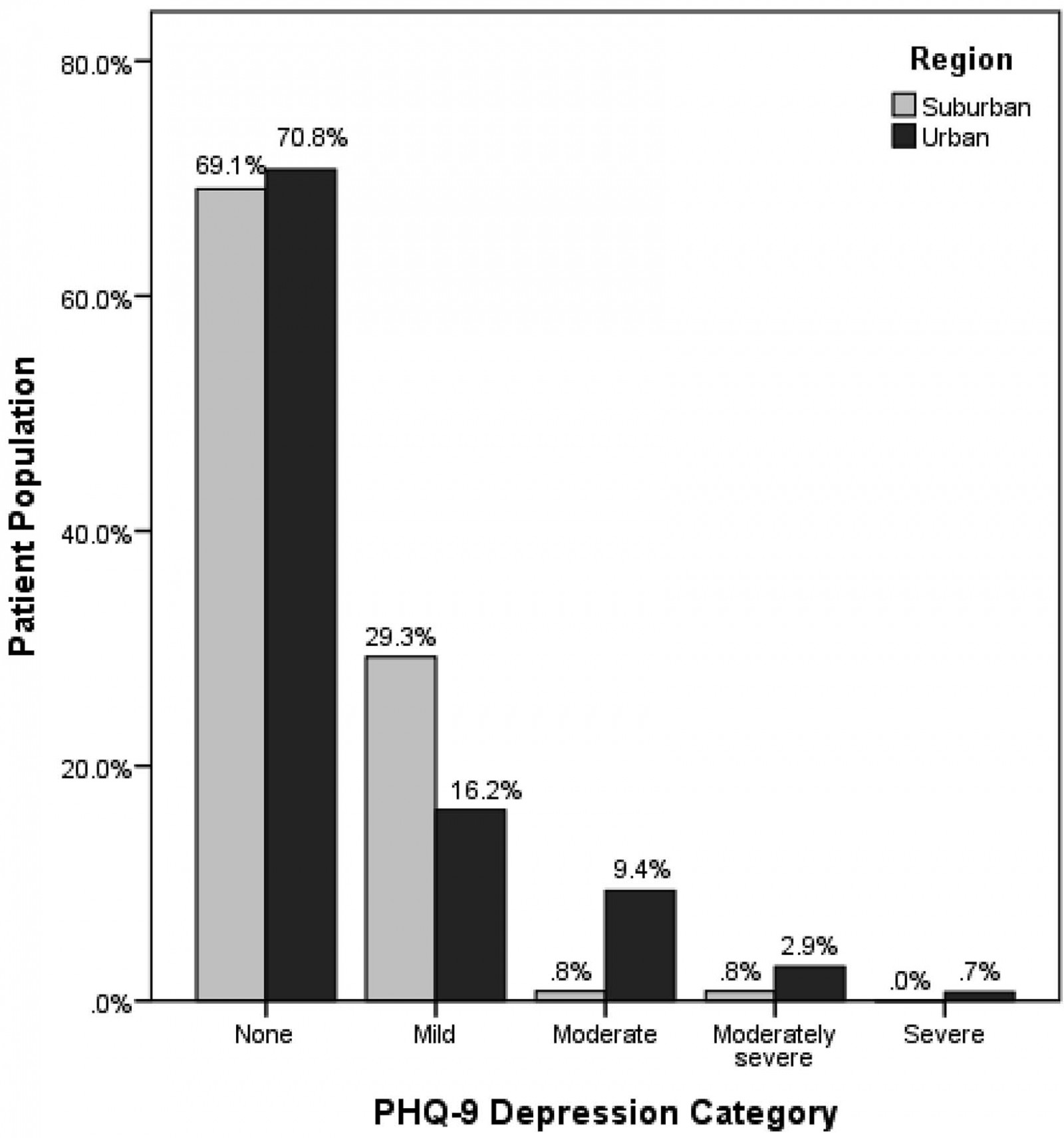 Figure 1: Severity of depression (according to PHQ-9 categories) in patients with type 2 diabetes according to urban and suburban regions.
Figure 1: Severity of depression (according to PHQ-9 categories) in patients with type 2 diabetes according to urban and suburban regions.
Discussion
The prevalence of depression in patients with type 2 diabetes in urban and suburban areas of the Maltese islands was not statistically different; however, the prevalence of moderate, moderately severe and severe depression was significantly higher in the urban region of the island. Interestingly, studies investigating the association of depression with urbanisation, which is a known risk factor for depression14, showed similar results17-19. Furthermore, these results follow the patterns of depression severity according to urbanisation for the country of Malta as demonstrated by Eurostat data, whereby severe depression was more prevalent in urban areas while mild depression was more common in suburban areas20.
This pattern of depression severity could be explained by socioeconomic differences between the different districts in Malta. Residents in the Southern Harbour district and, to a lesser extent, the Northern Harbour district, both of which form part of the urban conurbation of the islands, have lower average household disposable incomes and higher unemployment rates than residents in other districts9. This is in line with multiple other studies that have explored the association between depression and societal inequities, such as a low education level, unemployment and low income21-23.
Notably, this present study found a statistically significant difference in the incomes of participants from suburban and urban areas: those living in urban areas have a marginally higher income overall than those living in suburban areas. This finding could be explained by the fact that the Western district of the island, where most of the high earners live9, also forms part of the urban conurbation of the islands, thereby balancing out the lower income of participants from the Southern Harbour district.
The Maltese islands’ general demographic trends as reported by the National Statistics Office were further reflected in the proportion of non-Maltese residents with diabetes making use of the public primary health centres for follow-up of their diabetes, with the higher number of non-Maltese attending the suburban clinic reflecting the higher number of non-Maltese residents living in the suburban Northern region of the islands9.
Observations from studies investigating weight differences among rural and urban areas have shown a consistent trend, with rural participants demonstrating a higher rate of overweight and obesity than their urban counterparts24,25. Befort et al (2012) attributed this phenomenon to a higher consumption of unhealthy food and reduced availability of healthy food options in rural areas24. Additionally, Jokela et al (2009), who investigated migration patterns, pointed out the effect of social selection and social causation mechanisms that were likely to contribute to such a difference. In the latter study, obese individuals were more likely to live and migrate to rural areas while leaner individuals had a higher propensity towards urban regions. Moreover, regional differences in lifestyles and health behaviours between rural and urban areas were attributed to the differences in weight24,25. Similar to these studies, the current study showed a higher prevalence of overweight and obese individuals living in the suburban areas of the country.
Overweight and obesity are known risk factors for type 2 diabetes26 and might worsen its control27. In keeping with the findings of this study, participants living in suburban areas had worse overall control of their diabetes than their urban counterparts. However, residents in suburban areas tended to remember their capillary blood glucose test results more than those living in the urban region. These results were concordant with a Burmese cross-sectional study investigating rural–urban differences among patients with diabetes carried out in Myanmar, which showed a higher proportion of residents with uncontrolled diabetes living in a rural setting compared to the urban area28.
Due to time and resource constraints, primary care activities occurring in Gozo, in private hospitals and during home visits were excluded from this study. In Malta, any medical doctor can practise in the community but cannot be included in the Malta Medical Council Family Medicine specialist register unless qualified. Therefore, this study did not capture general practice activities carried out by practitioners not registered in the Malta Medical Council Family Medicine specialist register. These include hospital-based specialists and community-based specialists in both the public and the private sector.
Recall bias could have arisen when subjects selectively remembered details from the past. The participants were aware of the fieldworker’s professional background and may have tried to answer in the way they believed the fieldworker wanted them to answer, rather than according to their own beliefs (the ‘halo effect’). With questionnaires, there is the potential for participants to alter their behaviour in reaction to the researcher’s presence or to the realisation that they are being studied (the ‘Hawthorne effect’)29. Therefore, to counteract this response bias, the researcher showed a non-judgmental attitude and tried to be as objective as possible, particularly when participants needed help.
This study was not able to infer the temporal sequence of events or to demonstrate causality. The evidence was limited to key findings and associations. There might have been an overrepresentation of patients who are frequent users of primary care services. It is important to note that need might have been unperceived by patients (for example, in mental illnesses) and, therefore, might not have led to demand. This study did not assess whether these services were cost-effective and grounded in evidence-based medicine. Future research can address these limitations.
Conclusion
Despite the small size of the Maltese islands and the availability of free comprehensive public health care at the point of use, the presence of health inequities in this select group indicates the presence of social factors that prevent vulnerable groups from accessing the healthcare services that they need. This study provides valuable information to healthcare professionals, policy-makers and researchers to increase the awareness and sensitivity towards the effect of social inequities in the epidemiology of disease in urban and suburban areas.
References
You might also be interested in:
2010 - Understanding rural practice: implications for occupational therapy education in Canada
2009 - Youth alcohol and drug use in rural Ireland - parents' views
2008 - Are children from Crete abandoning a Mediterranean diet?
