Introduction
One of the challenges of delivering safe, reliable, quality health care is ensuring the workforce have access to the right training at the right time wherever they are1,2. Like other high reliability fields, healthcare education has recognised the important role of simulation based education in embedding a culture of readiness for practice3. This article shares the development of a national managed educational network (MEN) for clinical skills and how its principles were used to analyse the performance of a mobile simulation delivery unit over a 5-year period.
In Scotland, the requirement to raise the quality of healthcare services through local delivery, particularly in remote and rural locations, has recently been highlighted4,5. The National Health Service (NHS) Education for Scotland (NES), a non-territorial health board with responsibility for the training and education of the health service workforce, commissioned a national review of clinical skills using simulation based training. This led to the implementation of the Scottish Clinical Skills Strategy Partnerships for Care6, which advocated a national approach to using simulation to assure standards of educational practice7. This strategy identified four key priority outcomes for the NHS workforce (Box 1).
Whilst there is substantial literature on the use of simulation in healthcare education and practice8-11 there is relatively little on the use of a mobile simulation unit12,13.
 Box 1: Key priority outcomes for the National Health Service workforce with a particular emphasis on remote and rural practitioners14
Box 1: Key priority outcomes for the National Health Service workforce with a particular emphasis on remote and rural practitioners14
Methods
An action research approach15 was used to identify how the mobile simulation unit has changed the delivery of simulation based education as part of a national MEN for clinical skills education.
Development of a managed educational network in clinical skills
Simulation is known to be a powerful educational tool, but to be ‘most effective’ it needs curricular institutionalisation and endorsement by the host organisation6. The implementation of the Scottish Clinical Skills Strategy identified the opportunity to develop a national educational network to deliver quality assured, simulation based education irrespective of geographical or professional boundaries14.
The seven core principles agreed for managed clinical networks (MCNs)16 were adapted to an educational context of:
- functioning with explicit management arrangements
- embedding systems of accountability
- agreeing expected outcomes
- utilising an evidence base
- having a multiprofessional and multidisciplinary staff engagement focus
- engaging in a system of dissemination
- generating better value for money
- committing to research and development.
This provided a national approach to meeting the four key priority outcomes (Box 1) for the NHS workforce.
Development and implementation of a mobile simulation unit
The mobile simulation unit (MSU) was part of the proposed solution to the ‘inequity of provision of clinical skills education using simulation’, to support the training needs of the NHS workforce, particularly in remote and rural Scotland7.
Utilising the principles of the Clinical Skills Managed Educational Network (CSMEN), the MSU (Fig1) was developed with the same facilities and equipment found in fixed specialist simulation centres.
 Figure 1: The mobile clinical skills unit.
Figure 1: The mobile clinical skills unit.
Collection and analysis of data
Between 2014 and 2018, data were collected by the CSMEN team on the performance of the mobile simulation unit. Venues visited, job titles of participants and courses attended (a mix of local and national) were recorded by the venue hosts and collated by CSMEN staff.
Results
Findings for the previous 5 years (2014–2018) were analysed using the framework of the principles of the MEN. The results show the type of simulation and clinical skills education, the number of participants from different professional backgrounds involved and where this occurs, and includes evaluations from educators and participants.
Functioning with explicit management arrangements
The MSU local facilitators are known as hosts and provide crucial support for the MSU visit. Prior to the visit, hosts attend a 2-day faculty development course held centrally or occasionally at local venues and created specifically for educators who will use the unit, ensuring hosts are equipped with the knowledge and training to best use the equipment on board.
A total of 125 people from a range of health boards and other organisations have been trained on the faculty development course (Table 1).
The impact of this course has led to the development of a national faculty database for the MSU to facilitate the concept of flying faculty (providing faculty where required).
Another aspect of the explicit management is the operational group, which has responsibility for all operational activities relating to the unit including logistics, vehicle maintenance, driver availability, servicing and purchasing of equipment, data collection and liaison with educational providers.
Table 1: Number of people who attended faculty development course, according to National Health Service organisation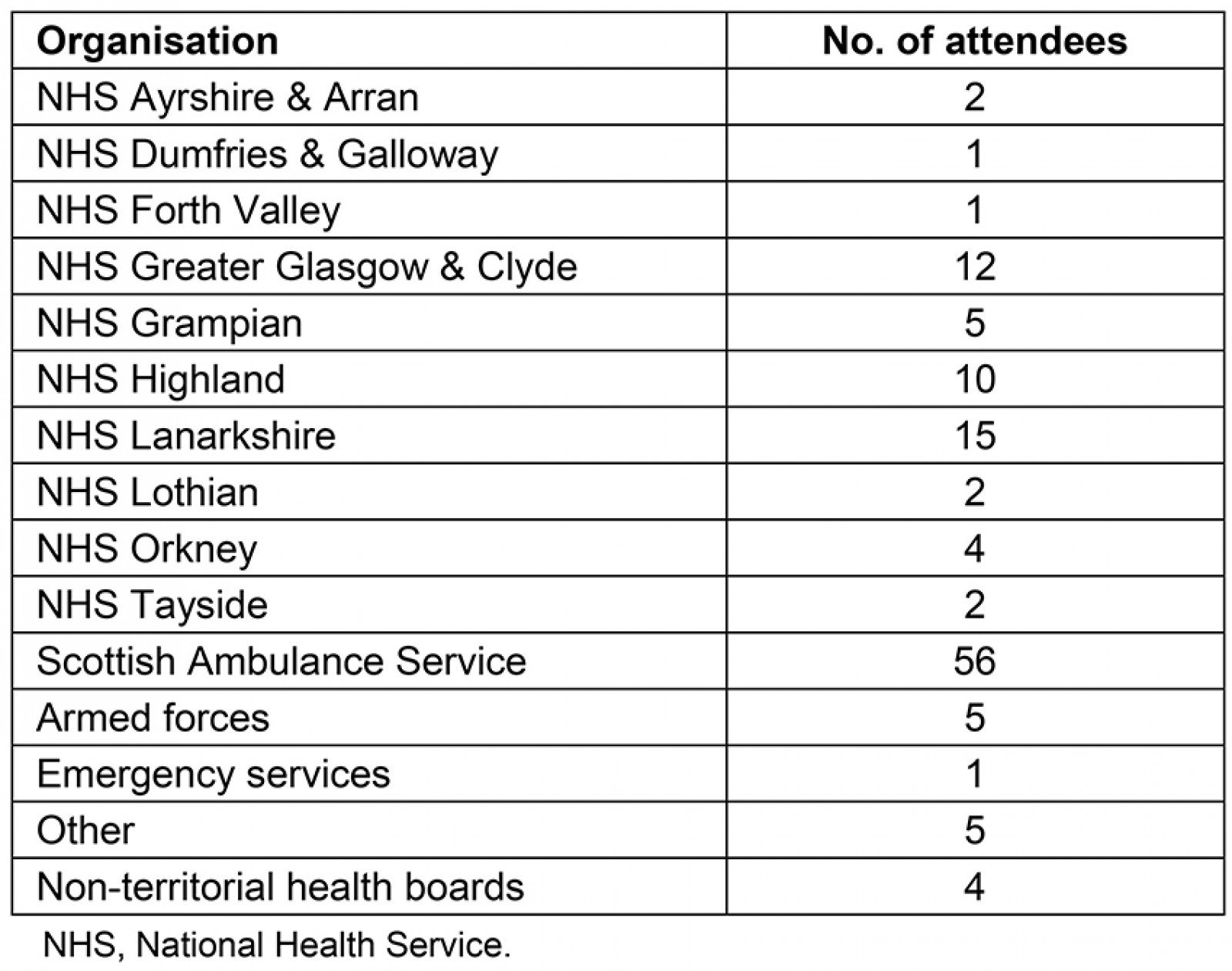
Utilising an evidence base
Three areas demonstrate the principle of utilising an evidence base in relation to the mobile simulation unit:
- Local adapted guidelines from Scottish Intercollegiate Guidelines Network: Those attending the MSU program have access to adapted clinical guidelines on common conditions such as asthma, acute coronary syndromes and sepsis developed by the Emergency Medicine Retrieval Services.
- Online resources: Online evidence based resources for clinical skills17 have been developed by the CSMEN group using expert input from the NHS and universities, providing learning opportunities prior to and after the face-to-face programs of the MSU.
- Quality assurance system: A framework for simulation based education (SBE) was developed to reflect the simulation based educational process. Each part of the process has been led by the CSMEN core team and agreed through consultation and consensus with the wider CSMEN community (Fig2).
A three-tiered approach was developed to identify key improvement outcomes for faculty: (1) educator awareness of SBE, (2) introduction for SBE educators and (3) advanced SBE for educators.
This outcome framework matches frameworks of the Academy of Medical Educators, Association for Simulated Practice in Healthcare and General Medical Council so that national standards can be locally implemented.
A national scenario template for designing a SBE session has been developed to ensure standards of design are considered in the development of new scenarios for the MSU. The quality assurance of debriefing on the MSU is part of the national faculty development program, ensuring the quality of simulation based education delivered locally.
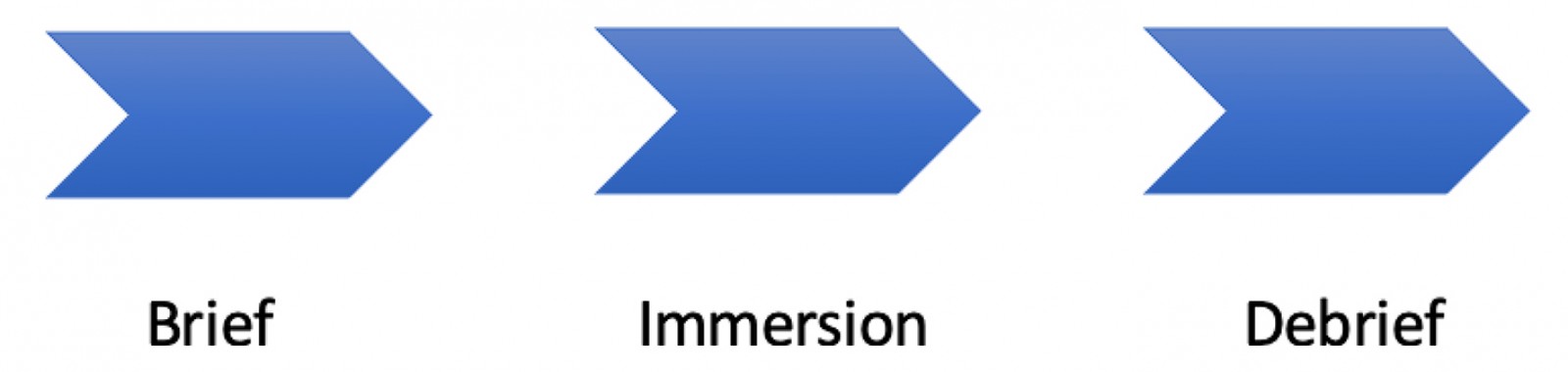 Figure 2: The simulation based education process
Figure 2: The simulation based education process
A multiprofessional and multidisciplinary staff engagement focus
The mobile unit was primarily intended to provide opportunities for multiprofessional healthcare staff training using simulation across geographical and professional boundaries in remote and rural Scotland. The spectrum of healthcare and emergency services professions trained as well as members of the public is shown in Table 2.
Table 2: Number of people trained on mobile simulation unit, according to job family, for National Health Service and emergency staff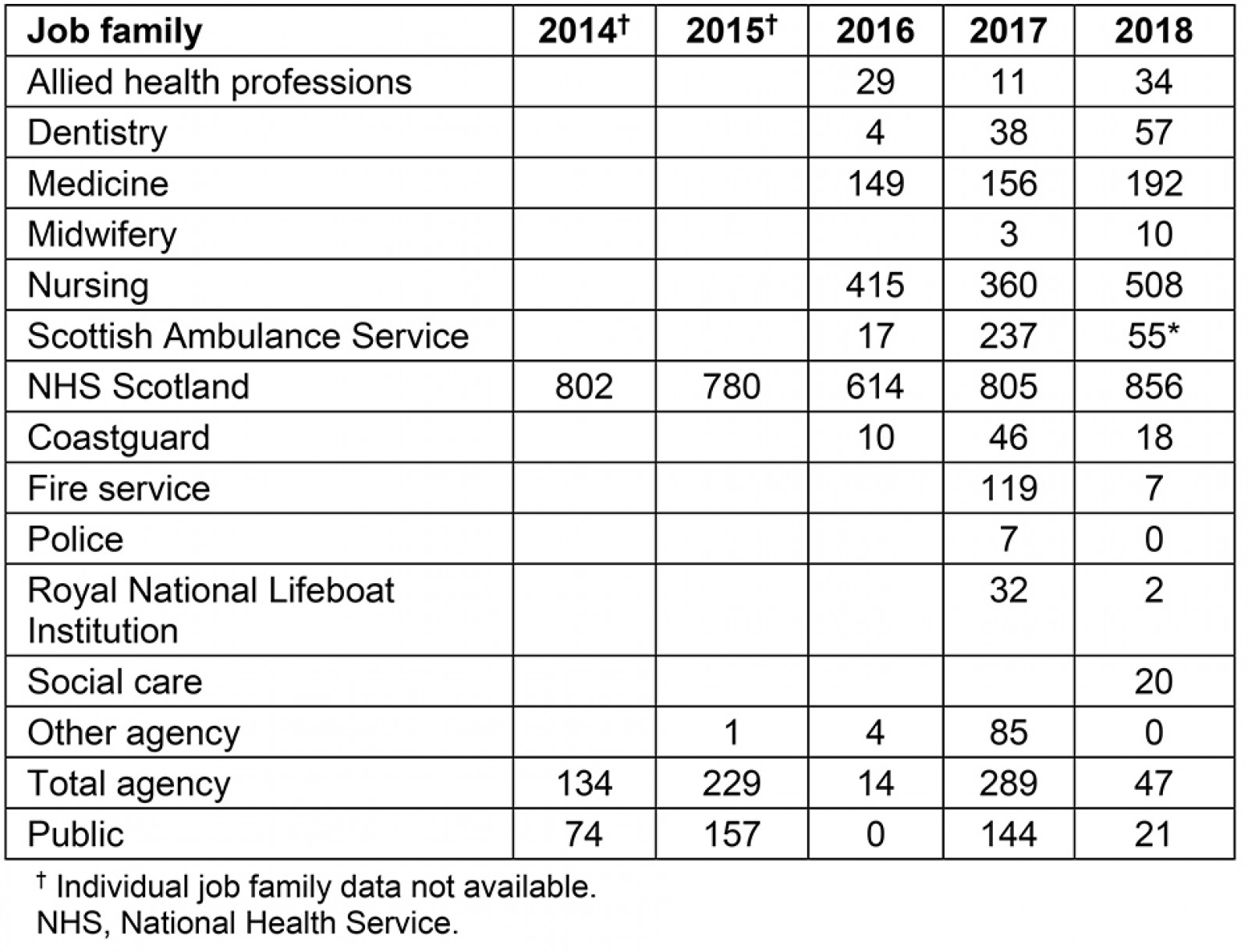
Agreeing expected outcomes
There has been a prevalence of acute and emergency care sessions delivered using simulated scenarios as well as the related procedural skills as a focus (Fig3). The most popular training sessions are shown in Table 3.
Table 3: Twelve most popular sessions run on mobile simulation unit, 2014–2018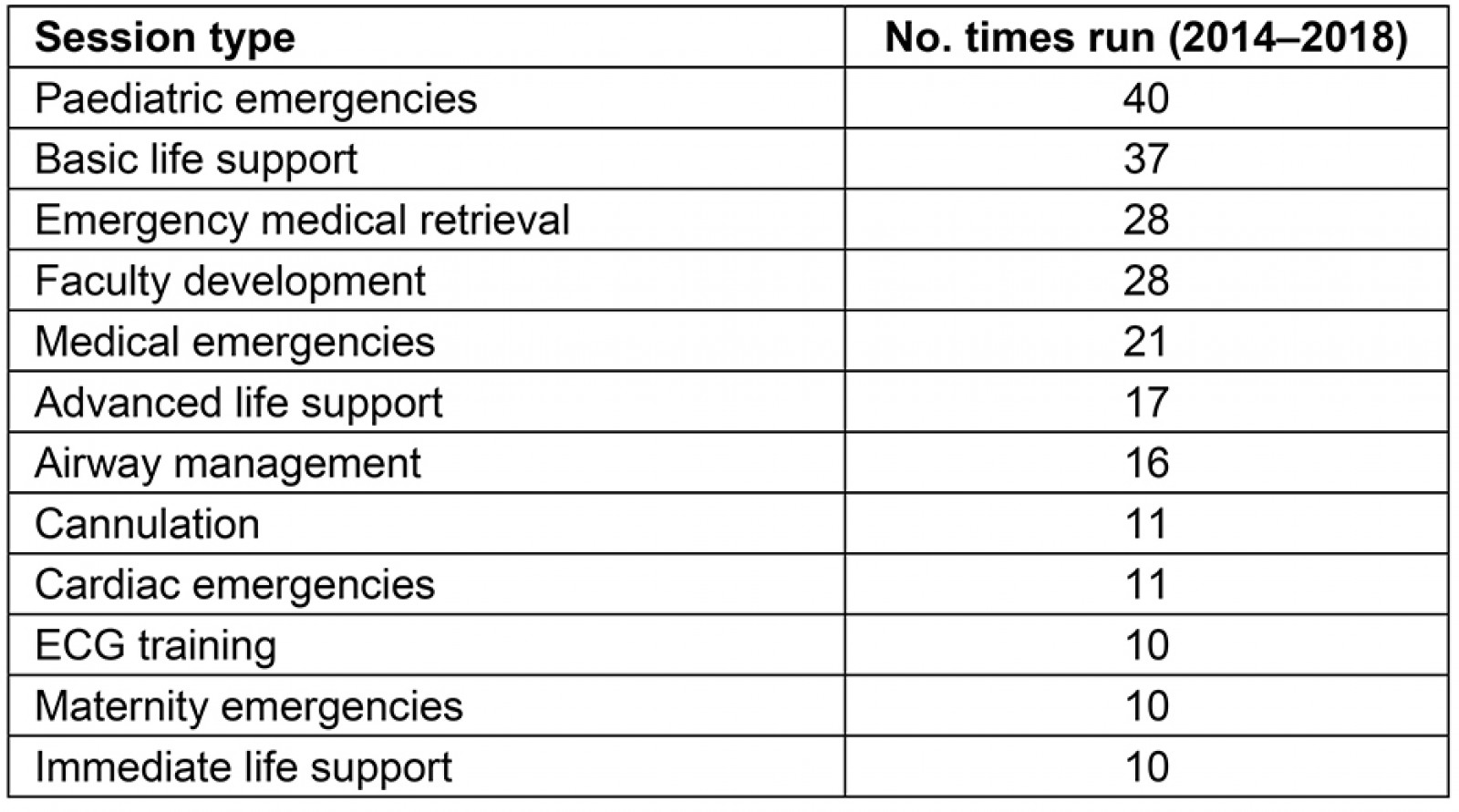
 Figure 3: Courses run on the mobile simulation unit.
Figure 3: Courses run on the mobile simulation unit.
Between 2014 and 2018, the MSU provided access to training for 10 of the 14 territorial health boards. It was also utilised by the Scottish Ambulance Service and the armed forces.
Four health boards (NHS Highland, NHS Forth Valley, NHS Lanarkshire and NHS Shetland) have requested the MSU every year. NHS Ayrshire & Arran and NHS Greater Glasgow & Clyde have requested visits for only 2 years or less (Table 4). Four health boards (NHS Lothian, NHS Tayside, NHF Fife and NHS Borders) did not request the unit for a training session during 2014–2018. These boards all have access to fixed simulation facilities.
Table 4: Frequency of visits to the various health boards, 2014–2018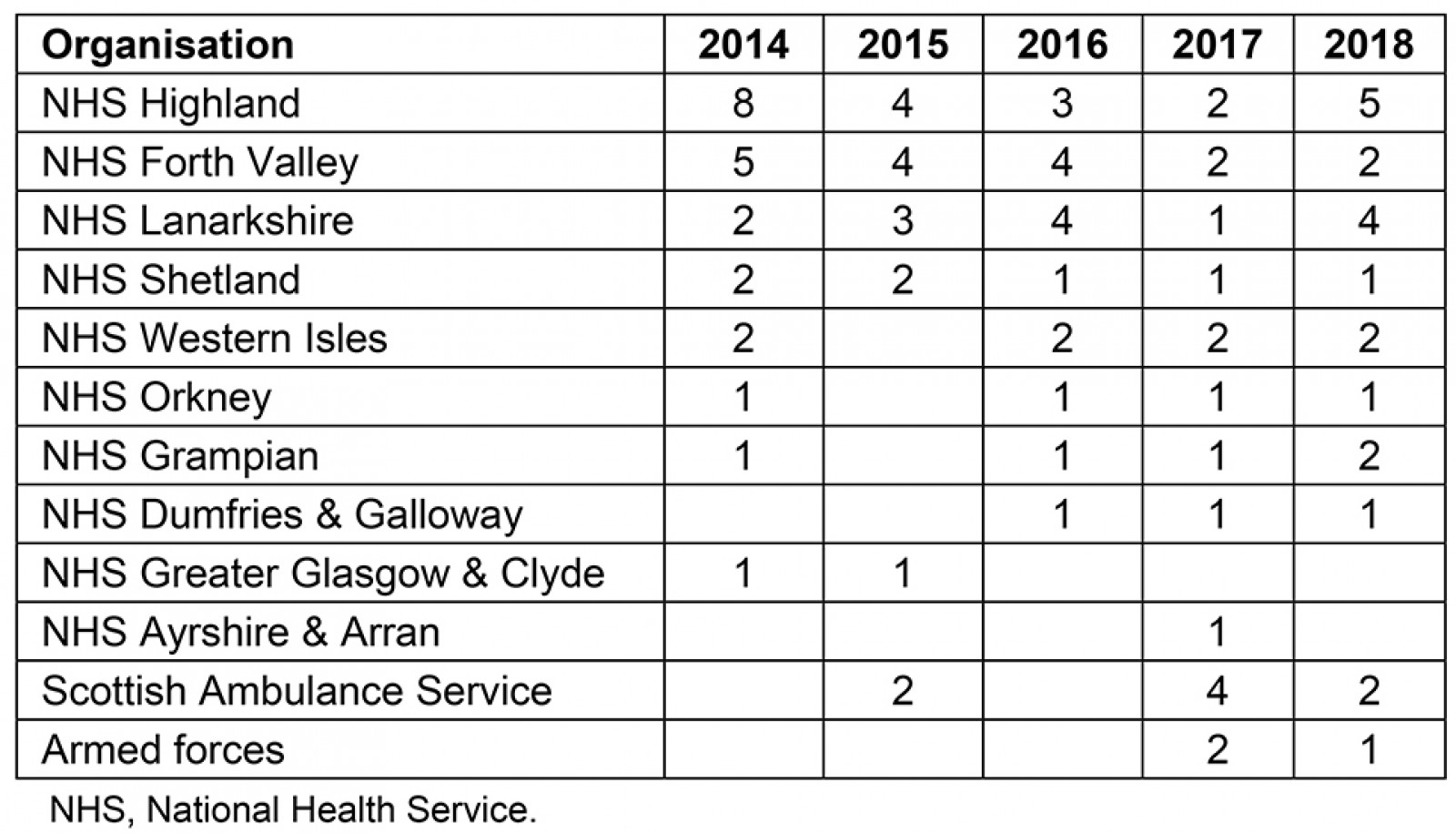
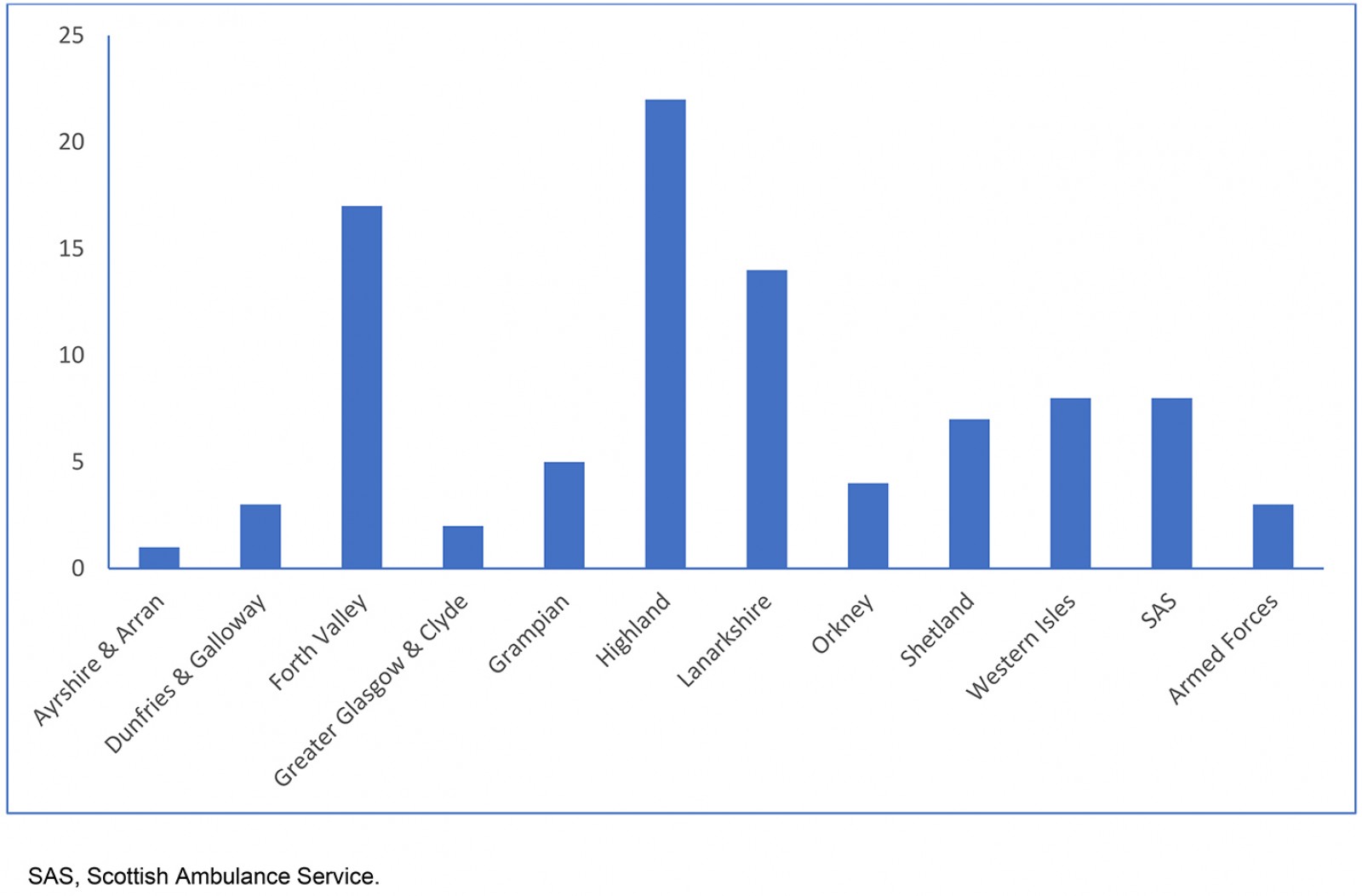 Figure 4: Number of visits to the various health boards 2014–2018.
Figure 4: Number of visits to the various health boards 2014–2018.
Generating better value for money
The average cost per course, per participant for training on the MSU has been calculated to be £37.50. Comparing this to estimated costs to local health boards to either send staff to a central simulation centre or provide basic skills training at an external location works out to be £265 per course per participant (based on 595 individual NHS Scotland employees with a total cost of £157,468, which includes course fees and travel costs but not costs for backfill). In addition, there is the equivalent of an estimated 770,000 km saved by the unit travelling to locations rather than staff travelling to central/local locations.
Generating research and development
During 2014–2018 the MEN disseminated the analysis of the data in relation to the mobile simulation unit at both national and international meetings, including 17 regional, national and international workshops, four poster and eight oral presentations.
There have also been seven peer reviewed publications and two grants of over £50,000.
Conclusion
An MSU as described in this article is not unique, but few examples of mobile simulation facilities exist in the UK, and none have the longevity of the CSMEN MSU.
These results demonstrate the effective use of simulation based education ensuring equity of access, irrespective of geographic location or professional background. This has been achieved without compromising national standards through local delivery by embedding systems of accountability with an explicit management system while generating value for money. The structure of a MEN embeds the infrastructure support required in relation to logistics and integrating the MSU as one of the delivery units aligned to the overall national strategy.
References
You might also be interested in:
2015 - Rural health activism over two decades: the Wonca Working Party on Rural Practice 1992-2012
