Introduction
Between 1980 and 2014, 57 033 deaths due to parenchymal pneumoconiosis (dust-related lung diseases) were recorded in the death records of the US National Center for Health Statistics1. Of these, the largest category of deaths (38%) comprised those due to coal workers’ pneumoconiosis (‘black lung’)1. Regional variation in pneumoconiosis mortality rates is seen in the USA; the counties with highest mortality rates are concentrated in rural central Appalachia and Rocky Mountain states, which have a history of mining1. In 2019, almost 54 000 employees worked in the US coal mines2. With 28% of the world’s recoverable coal reserves in the USA, mining employment is likely to remain significant for many years3. Recent evidence points toward an ongoing increase in both prevalence and severity of coal workers’ pneumoconiosis since the late 1990s3-9. The 2017 data from the US National Institute of Occupational Safety and Health surveillance program showed a greater than 10% overall prevalence of radiographic pneumoconiosis for underground coal miners with over 25 years tenure. A 21% prevalence of radiographic pneumoconiosis was described in central Appalachian long-tenured miners8. The rate of complicated pneumoconiosis, a particularly deadly form of pneumoconiosis, in long-tenured underground coal miners was 1.1% in 2014, compared to 0.3% at its nadir in the late 1990s9,10. The rate of complicated pneumoconiosis in central Appalachia reached 4.5% for the 5-year period ending 20178. Most of the affected coal miners worked their entire careers after the 1969 dust limits had gone into effect, calling into question the effectiveness of modern dust controls in the USA9.
This re-emergence of pneumoconiosis has created a challenge for rural mining communities. While the number of miners requiring specialized care has increased, the multidisciplinary expertise available has contemporaneously decreased in rural USA11. This challenge demands innovative solutions to support quality multidisciplinary teams to improve the health and wellbeing of miners, who constitute an underserved, isolated, medically vulnerable and often underinsured rural population11. Given the dearth of skilled expertise in mining-related diseases, the education and mentoring of professionals in rural areas involved in the care of miners are necessary first steps.
The Miners’ Wellness TeleECHO (Extension for Community Health Outcomes) ‘clinic’ was jointly set up in 2016 by the University of New Mexico and a community-based miners’ hospital in New Mexico, USA, to provide structured longitudinal multidisciplinary telementoring to various groups of professionals caring for miners in pneumoconiosis mortality hotspots in the USA1. Professional groups telementored include rural clinicians, respiratory therapists, home health professionals, benefits counselors, lawyers/attorneys and others, creating a virtual community of practice. The latter is defined as ‘groups of people who share a concern or a passion for something they do and learn how to do it better as they interact regularly’12. This approach facilitates knowledge translation: helping knowledge-users become aware of multi-disciplinary knowledge and facilitating their use of it in their day-to-day work and decision-making in the ‘real world’13. Knowledge translation is believed to encompass a more holistic view than traditional continuing medical education (CME) and continuing professional development models, which may make it easier to close the gap between evidence and practice14. Studies in other disease states indicate a favorable impact of ECHO telementoring strategies on providers’ self-efficacy and competence15-17.
The community of practice approach for rural professionals caring for miners has, however, not been utilized and evaluated previously, constituting a critical gap in knowledge. There is a need to correct this gap in knowledge because, without doing so, evidence-based rural interventions for providing complex interdisciplinary care for miners would likely remain beyond reach. The objectives of this cross-sectional study were to help establish the knowledge gap, and to provide preliminary evaluation of the virtual community of practice approach in telementoring rural professionals caring for miners. If effective, it will provide an exciting opportunity for greater investment in interprofessional telementoring to foster collaborative healthcare practices in mining communities, with implications for similar rural and remote communities dealing with complex health issues everywhere.
Methods
Study design
This is a cross-sectional study of participants involved in the Miners’ Wellness TeleECHO Clinic, a novel community–university partnership, between a small rural hospital (Miners’ Colfax Medical Center, Raton, New Mexico) and its academic partner (University of New Mexico School of Medicine, Albuquerque, New Mexico) – the latter constituting the ‘hub’ site of experts. Stakeholder groups of participants include rural and academic clinicians, respiratory therapists, home health professionals, benefits counselors, lawyers/attorneys and others, including policymakers, administrators and mine safety officers, constituting the ‘spoke’ sites located all across the USA. The hub and the spoke partners engage in telementoring, and together form a virtual community of practice.
Program description
Each TeleECHO clinic, held at the same time twice every month, lasts for 75 minutes, and has a uniform format, which includes a 10-minute introduction and announcements section; a 15-minute didactic by an invited expert, followed by a 20-minute question–answer session; and a 30-minute interactive case discussion facilitated by the clinic director. This format has a greater focus on active learning through discussion than on didactic training. CME credits are provided without charge to the participants, upon completing the CME survey. The program utilizes a structured curriculum established by a multidisciplinary curriculum committee. The curriculum is continually adapted to reflect the needs of the learning community, based upon the review of the CME feedback reports. Participants attend the ECHO sessions voluntarily, regardless of whether they are presenting a case, so that they can view the didactic talk, partake in the case discussions, contribute insight from their own practice, and learn from the expert panel and their peers. Participants also benefit from access to experts at the hub or spoke sites between sessions, by email or telephone, for urgent consultation questions. ECHO sessions are recorded and archived in an online, freely accessible web-based library.
Program development
Since July 2016, the bimonthly program has used the ECHO model to provide structured long-term telementoring, an approach that differs from traditional telemedicine, where providers assume typically short-term care of individual patients. Unlike traditional didactic lectures or webinars, the ECHO model provides a real-time, interactive discussion of cases with expert panels; thus, the discussions are highly contextualized, which fulfils key learning theory principles. The ECHO model:
- uses technology such as multipoint video-conferencing and the internet to leverage scarce mentoring resources
- uses a disease-management model that is proven to improve outcomes in other disease states by reducing variation in processes of care and sharing best practices16-19
- uses the principle of case-based learning. Participants study with guidance from mentors, based on discussion, questions and investigation of patient cases under their care. Over time, with iterative practice and feedback, participants gain additional knowledge and skills and assume more independence
- creates a virtual community of practice. The emphasis of the group is on reciprocity in the sharing of information and skills, and promoting trust and respect, acknowledging that all participants bring some unique expertise in the multidisciplinary care of miners. By interacting on a regular basis, the community of practice members increase their own expertise and that of other participants. As a result, the program aims to increase the ability of individual rural participants to refer miners appropriately to other experts, accept miner referrals from other experts, and serve as local experts for untrained community professionals, thereby improving the care of miners
- uses an internet-based database (iECHO software) to monitor outcomes.
Outcomes
This study used geographical mapping of all participant locations and web-based CME surveys completed by participants using iECHO software. Additional outcomes include self-reported knowledge, self-efficacy and collective efficacy with respect to pneumoconiosis, using a customized instrument created for this purpose by a multidisciplinary curriculum committee. Because the program has several stakeholder groups, knowledge and self-efficacy measures for pneumoconiosis were identified for each of the disciplines (intradisciplinary measures) and common measures across the various disciplines (cross-disciplinary measures), based upon the review of the literature and feedback from individual stakeholder groups. The instrument also measured professional isolation and satisfaction in professional practice, using five-point Likert scales from ‘strongly disagree’ to ‘strongly agree’20.
Knowledge related to pneumoconiosis was evaluated using 10 standardized intradisciplinary and cross-disciplinary questions, based on those encountered in cases presented previously at the TeleECHO clinic. Each question had four response options, one of which was correct.
Self-efficacy, or a provider’s perceived ability to recognize and manage essential components of care of complex miners’ diseases and to serve as a local expert for these diseases for other community professionals, was assessed, adapted from previously validated instruments21. Participants reported on 14 self-efficacy measures, rating each measure on a scale of 1–7, where ‘1’ indicates none or no skill and ‘7’ indicates expert or ability to teach others. Standardized Cronbach’s alpha coefficient values for the instrument showed high levels of internal consistency (values ≥0.85 for all items).
Collective efficacy concerns group members’ belief in a collectivity’s ability to solve a problem through unified effort, which can positively influence the quality of team performance22. Collective efficacy is typically measured with items that capture overall social cohesion among group members and the perceived capacity for members to successfully act on the group’s behalf to achieve common goals. A collective efficacy measure was created using 12 scale items, adapted from prior research among medical staff, professional working groups and residential communities23,24. Items captured respondents’ level of agreement on a five-point Likert scale, from ‘strongly disagree’ to ‘strongly agree’20. The collective efficacy measure had a standardized Cronbach’s alpha of 0.88.
Knowledge transfer was conceptualized as receiving new and important knowledge regarding the care of miners during and outside of TeleECHO sessions from other participants. Beyond quantifying the number of knowledge sources, the extent to which members of different stakeholder groups received knowledge from members of their own versus different stakeholder or professional groups was examined. This analysis helped assess the extent to which participants acquire novel information from diverse sources. Patterns of group members’ knowledge transfer were analyzed using methods and insights from social network analysis25. Respondents indicated whether they received knowledge from specific knowledge sources, defined as colleagues who provided the respondent with new and important information or knowledge regarding the care of miners. Respondents identified knowledge sources from a roster that included Miners’ Wellness TeleECHO participants, broken down by stakeholder groups. The number of knowledge sources reported by respondents, as well as the proportion of sources that were outside of each respondents’ stakeholder group, were analyzed. Also examined were the differences in the number of knowledge sources and proportion of knowledge sources outside of stakeholder groups among ‘fresh’ and existing participants, and among clinical and non-clinical professional groups.
Data collection
The program monitored the number of sessions, learners, unique learners, geographical sites of learners and patient cases presented (using the iECHO software) during the 1-year study duration from 12 September 2018 to 18 September 2019. A convenience sample included 70 participants, who volunteered to complete an additional detailed survey, among all program attendees invited. Core program faculty did not participate in the survey. Data was collected using the Research Electronic Data Capture (REDCap), a secure web application for building and managing online surveys and databases.
Analytic strategy
Data collected were analyzed using Statistical Analysis Software v9.4 (SAS; http://www.sas.com). Frequency measures were analyzed. Fisher’s exact test was used to analyze categorical variables, and the non-parametric Wilcoxon ranked sum test for continuous variables, related to knowledge and efficacy. Comparison groups included clinical professional groups versus non-clinical professional groups, and fresh versus existing participants. Clinical professional groups include clinicians, respiratory therapists and home health professionals (mostly nurses). Non-clinical professional groups include lawyers/attorneys, benefits counselors and others. Fresh participants are defined as those who first attended the community of practice in the summer of 2018 (defined as from 9 May 2018 onwards), and existing participants are defined as those who had first attended between 1 July 2016 and 8 May 2018). Social network analysis techniques were used to study knowledge sharing within and between participants from stakeholder or professional groups, using student’s t-tests. A two-tailed p-value less than 0.05 was considered statistically significant.
Ethics approval
Approval was obtained from the institutional review board, Human Research Protections Office, at the University of New Mexico Health Sciences Center (HRPO 18-386).
Results
Over the 1-year period from 12 September 2018 to 18 September 2019, 21 clinics were held over 26.5 hours, involving 154 unique attendees, with a total attendance of 514, averaging 24.9 attendees per clinic session. Fourteen attendees presented 21 unique patient cases, and 21 invited experts presented 21 didactics at these clinics during the timeframe. Geographical mapping indicates that attendees were predominantly located in pneumoconiosis mortality hotspots in the Appalachian and Rocky Mountain regions (Fig1). Of the 129 CME surveys completed during this timeframe (survey response rate 24%), most participants rated the TeleECHO sessions as ‘very good’ to ‘excellent’ for survey items (Supplementary Table S1).
A convenience sample of 70 subjects (constituting 45% of the unique attendees) participated in a detailed survey. Most participants were white non-Hispanics, women, and aged 50 years or less (Table 1). Of all participants, 66% belonged to the clinical professional groups, including the clinician (29%), home health professional (20%) and respiratory therapist (17%) stakeholder groups; and 34% belonged to the non-clinical professional groups, including the lawyer/attorney (10%), benefits counselor (11%) and other (13%) stakeholder groups. Most participants reported caring for miners from mostly rural communities for no more than 10 years. Despite a high level of job satisfaction, a significant minority of participants reported professional isolation.
Most participants correctly responded to nine of the ten knowledge questions relevant to the care of miners (Table 2). Participants demonstrated the lowest knowledge score on ‘legal’ pneumoconiosis, among the questioned knowledge areas. Participants in clinical professional groups were significantly more likely to correctly answer the question on guidelines for providing supplemental oxygen than those in non-clinical professional groups (p<0.01, Fisher’s exact test). Compared to fresh participants, existing participants were more likely to correctly answer questions about the type of workers eligible for miners’ compensation programs in the USA and the small opacity profusion threshold using the international classification of radiographs of pneumoconiosis, also called B-reads (all p<0.05, Fisher’s exact test).
Although most participants reported high self-efficacy with respect to ‘soft’ skills (such as empathy and sociocultural competency), and ability to refer appropriately to other experts, participants reported relatively lower self-efficacy with respect to diagnosing miners’ conditions, interpreting B-read reports and determining eligibility for compensation under specific miners’ compensation programs (Table 3). As opposed to participants in non-clinical professional groups, those in clinical professional groups reported lower self-efficacy with respect to their ability to help miners navigate the compensation process and to serve as regional experts (all p<0.05, Fisher’s exact test). Participants in clinical professional groups reported greater self-efficacy with respect to managing and diagnosing health conditions (all p<0.05, Fisher’s exact test). As compared to fresh participants, existing participants demonstrated significantly greater self-efficacy with respect to empathy and the ability to refer appropriately to other experts, collaborate with and educate other team members, and determine eligibility for compensation (all p<0.05, Fisher’s exact test).
Participants rated the community of practice highly with respect to its willingness to help overall (93%), for improving patient care (91%), respect (91%), finding and sharing resources (89%), fostering members’ ability to care for miners (87%), being closely knit (87%) and trust (86%). The learning community was rated lower with respect to supporting each other in times of stress (66%), intervening if another participant was arriving at a wrong conclusion (73%), or figuring out what choices to make when the clinic faced decisions (77%; Table 4). There were no significant differences with respect to any of the individual collective efficacy items among participants in the clinical versus non-clinical professional groups, and fresh versus existing participants.
Results examining patterns of knowledge transfer within the community of practice are presented in Table 5. Across all participants, respondents reported having a mean number of 4.33 knowledge sources, with existing participants reporting a significantly higher mean number of knowledge sources than fresh participants. Among all participants, respondents reported on average that nearly half (0.47) of their knowledge sources were from outside of their professional group. Participants in the non-clinical professional groups reported a significantly higher mean proportion of knowledge sources from outside of their professional group than did participants in the clinical professional groups. Among the entire sample, the mean proportion of knowledge sources outside of an individual’s stakeholder group was 0.51. Existing participants reported a significantly higher mean proportion of knowledge ties from outside of their stakeholder group than fresh participants.
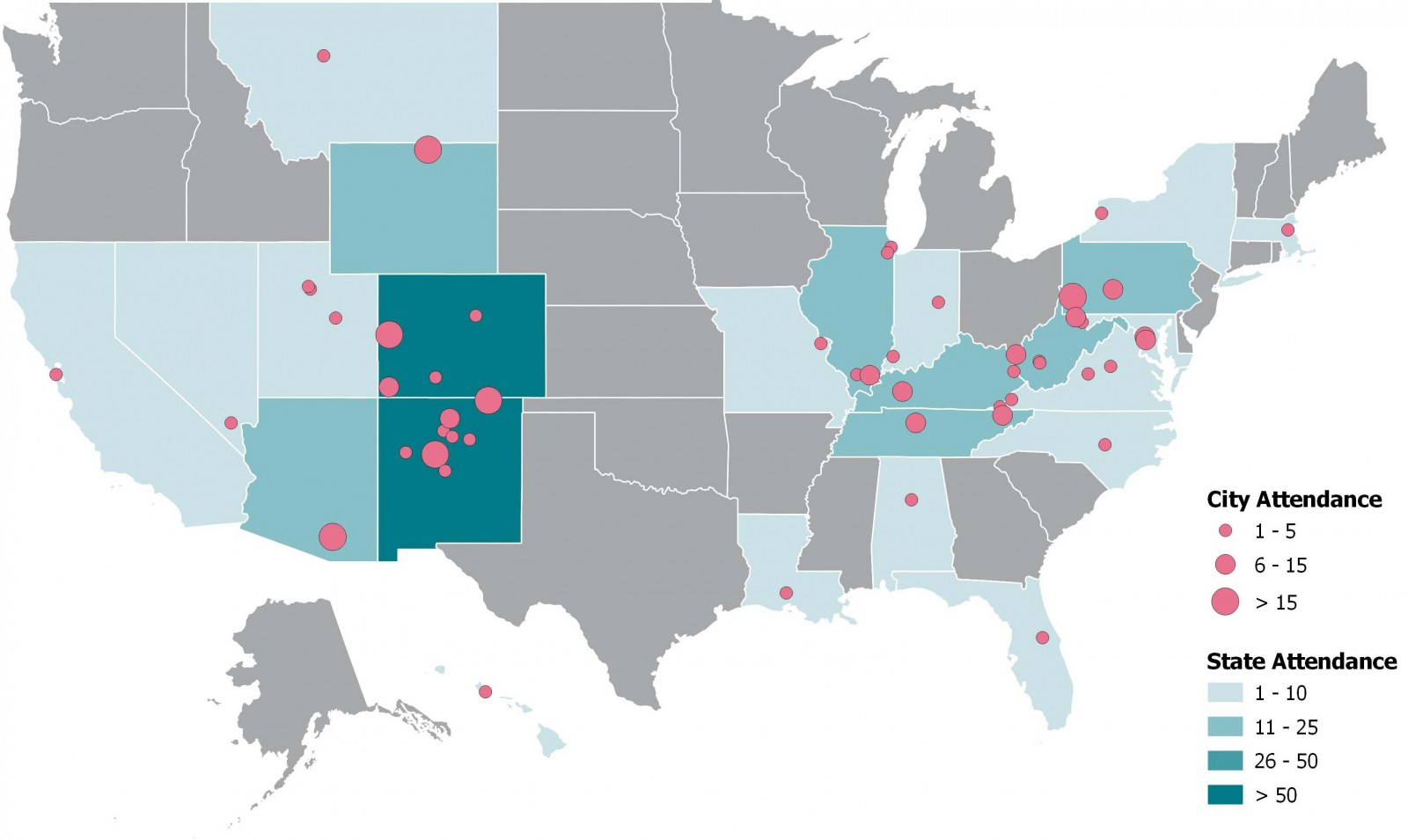 Figure 1: Geographical mapping indicates that participants in the ‘community of practice’ are located in pneumoconiosis mortality hotspots in the USA, September 2018 – September 2019.
Figure 1: Geographical mapping indicates that participants in the ‘community of practice’ are located in pneumoconiosis mortality hotspots in the USA, September 2018 – September 2019.
Table 1: Characteristics of surveyed participants (n=70)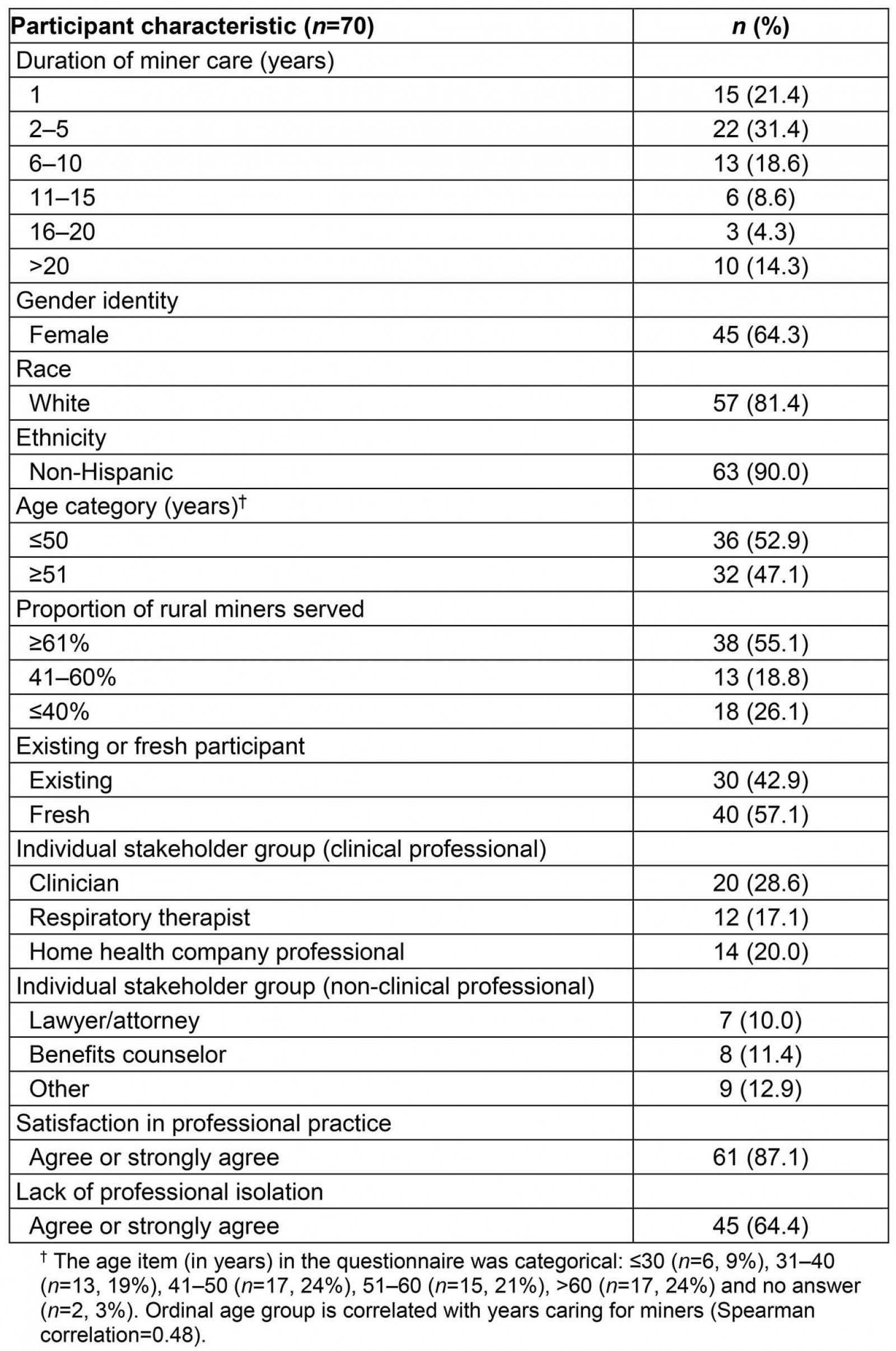
Table 2: Assessment of self-reported knowledge, from a convenience sample of 70 participants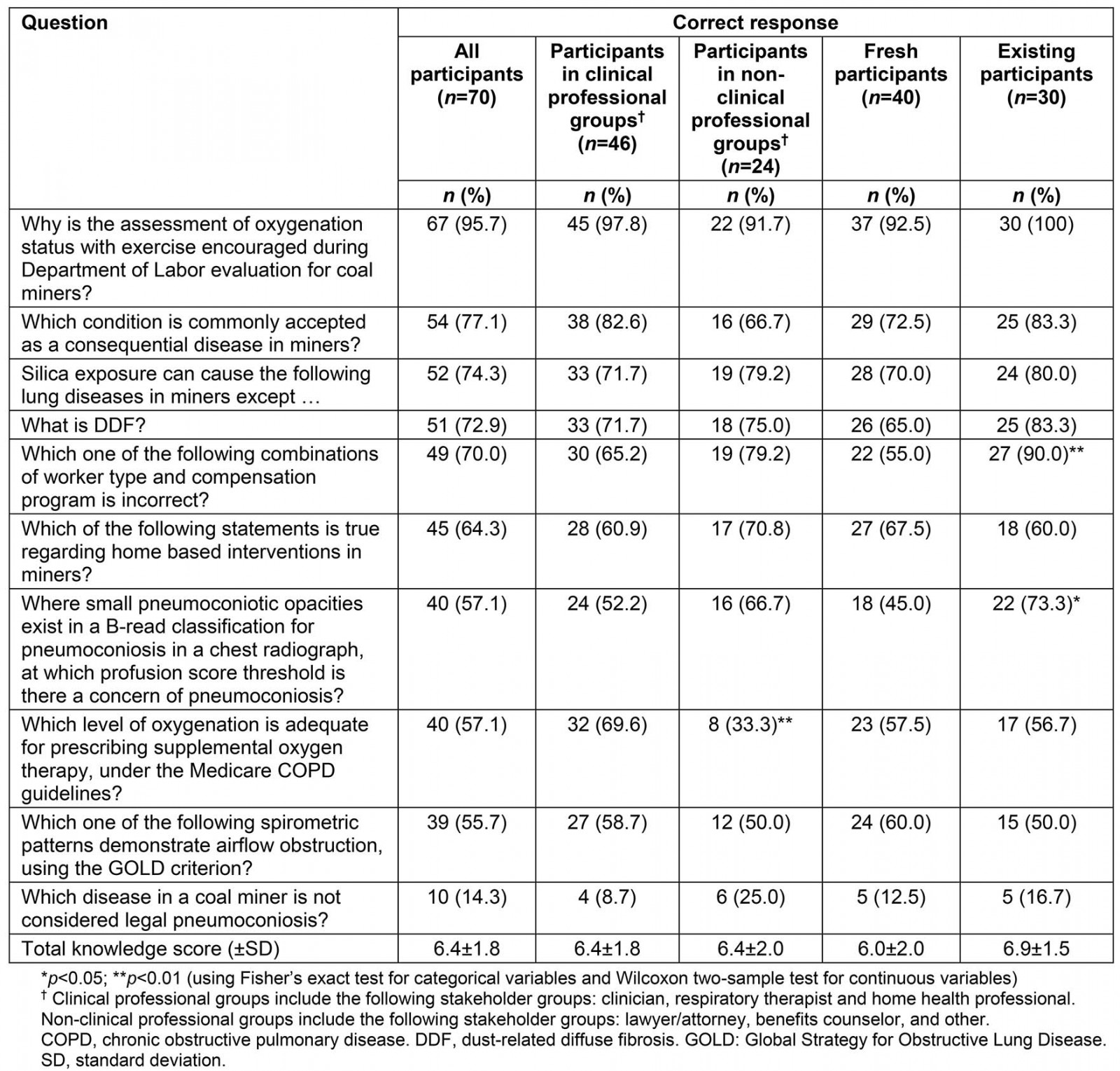
Table 3: Participants rating themselves as ‘competent’, ‘very competent’ or ‘expert’ on self-efficacy items (corresponding to the top three ratings on a scale of 1–7), from a convenience sample of 70 participants
Table 4: Participants agreeing or strongly agreeing with individual collective efficacy items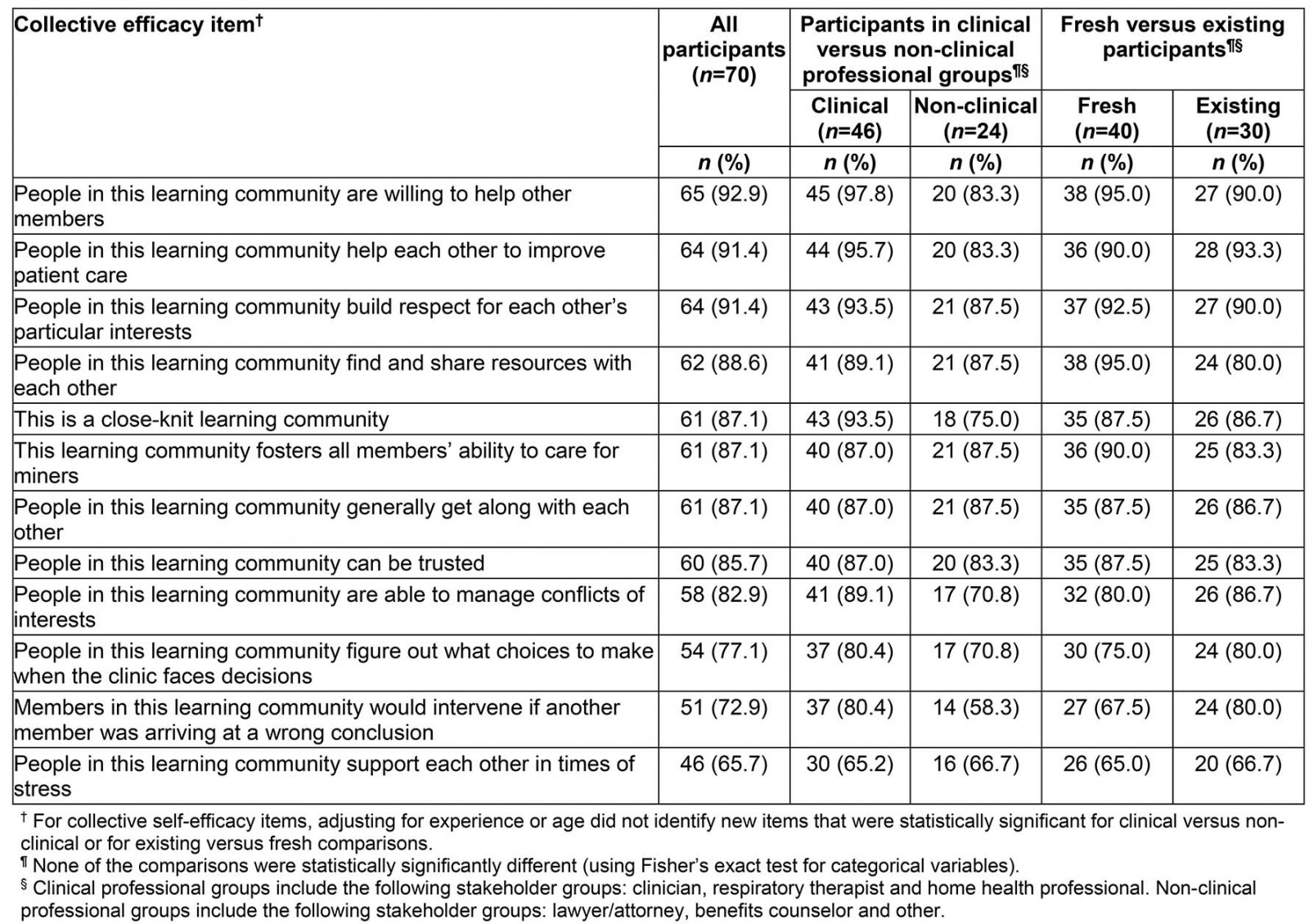
Table 5: ‘Community of practice’ network analysis of knowledge transfer for either individual stakeholder groups or collections of stakeholder groups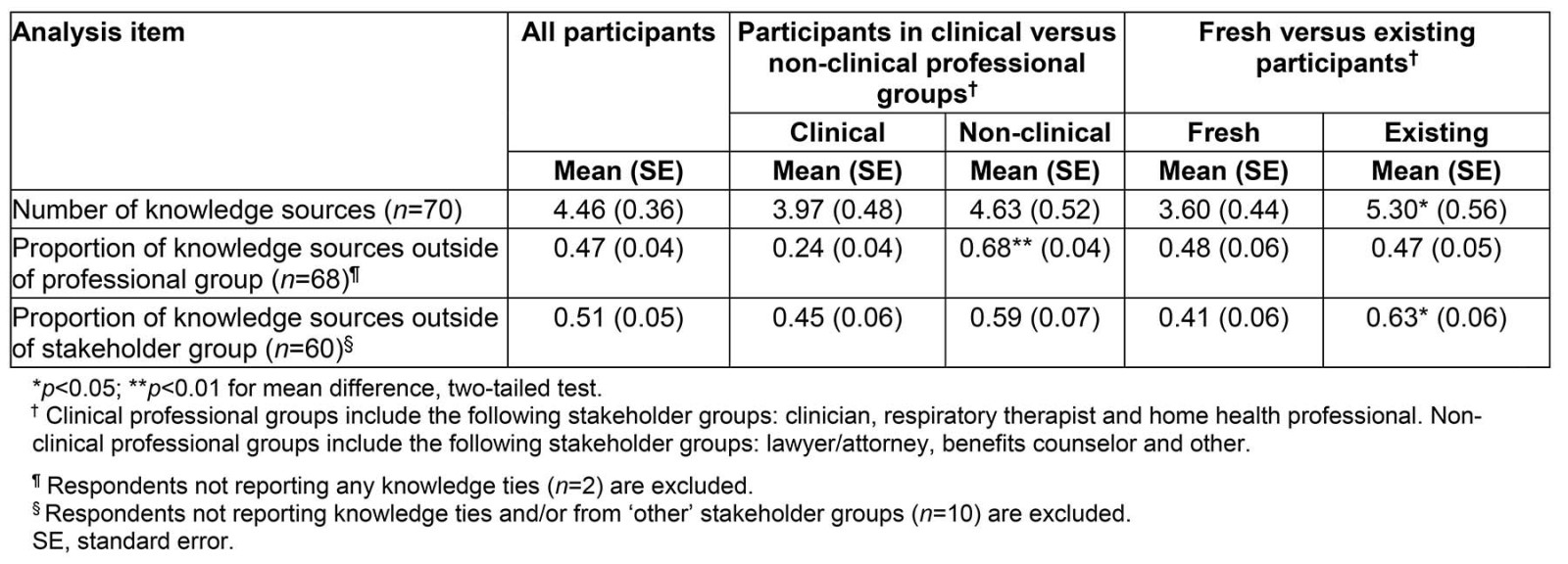
Discussion
The present study’s findings demonstrate a successful creation of a virtual multidisciplinary community of practice in pneumoconiosis mortality hotspot rural regions of the USA, with several stakeholder groups represented, including 29% clinicians. This community is rated highly with respect to trust, respect, willingness to help and being closely knit, even by fresh participants. Most participants utilize knowledge ties from outside of their stakeholder group, emphasizing the multidisciplinary nature of miners’ care. The preliminary evaluation of Kirkpatrick levels 1 and limited level 2 outcomes demonstrates that this approach may help improve participants’ ability to diagnose and manage miners with pneumoconiosis26.
Participants in this virtual community of practice demonstrated the lowest knowledge score on ‘legal’ pneumoconiosis, among the questioned knowledge areas. ‘Legal pneumoconiosis’, as defined by the US Black Lung Benefits Act, includes any chronic lung disease or impairment and its sequelae arising out of coal mine employment, which is not covered by the clinical pneumoconiosis definition. ‘Legal pneumoconiosis’ may include asthma, chronic bronchitis, emphysema, small airways disease, atypical fibrotic lung diseases and lung cancer. Because ‘legal pneumoconiosis’ is a collection of disparate medical conditions seen in coal miners, many professionals taking care of miners may find this term confusing, indicating that educational interventions need to focus on legal definitions of diseases. Educational interventions also need to focus on disease management and test result interpretation, areas in which the participants reported low self-efficacy.
The ECHO model recognizes the importance of multidisciplinary approaches to patient care. Thus, sharing information and skills within and across stakeholder groups is an underlying objective of this community of practice. The study indicates multidisciplinary knowledge transfer between different stakeholders, with existing participants reporting greater numbers of knowledge sources, and larger proportions of knowledge sources from outside of their stakeholder groups, than fresh participants. This finding suggests that access to and diversity of knowledge sources increases with time and participation in the community. As compared to clinical professional groups, participants in non-clinical professional groups were significantly more likely to receive knowledge from outside of their professional group. The role of these non-clinical stakeholders in knowledge transfer in this community of practice should not be underestimated. Based upon the preliminary need assessment surveys done prior to launching the TeleECHO program, surveyed stakeholders informed the authors that a key challenge was the complexity of the miners’ compensation systems. This needs assessment gap cannot be met without the active participation of non-clinical knowledge sources.
This study is an innovative intervention that targets rural stakeholders in order to address the barriers to the care of miners. Other strengths are its use of a virtual multidisciplinary community of practice; evaluation of group-based outcomes in addition to individual-based outcomes; use of internet-based technology to leverage scarce resources; use of the TeleECHO model, which is well studied in other diseases16-19; and recognition of the importance of knowledge source diversity. The study is topical and significant because it addresses a critical gap related to the emerging pneumoconiosis epidemic; this field of research is understudied, and is a priority need in the rural USA. The study’s high potential impact is related to the spoke site presence in pneumoconiosis mortality hotspots in the USA (Fig1).
The present study has several limitations. Program participants had variable competencies, with varying levels of sophistication, commitment, expertise, experience and historic levels of collaboration within the existing program. There are also intergenerational, interinstitutional and rural–urban disparities in ability to leverage technology by participating professionals. This variability may challenge the study’s ability to have standardized ways of testing outcomes. In this cross-sectional study baseline evaluation, longitudinal change in knowledge, skills and competencies of professionals and in patient outcomes, corresponding to higher level Kirkpatrick outcomes, were not evaluated27. Despite the relatively small numbers of participants studied, individual professionals and teams of professionals trained in the ECHO model can reach a large number of miners, with potential for creating exponential change.
Conclusion
The present study’s findings demonstrate a successful creation of a virtual multidisciplinary community of practice in pneumoconiosis mortality hotspot rural regions of the USA. Sensitizing participants to the knowledge, skills and competencies of participants from disciplines other than their own is an important goal of this community of practice. This virtual community of practice approach toward knowledge transfer for mentoring rural stakeholders may help ensure the delivery of high-quality interdisciplinary care to miners in pneumoconiosis mortality hotspots in the USA.
Acknowledgement
The Alpha Foundation funded this study. The organization has made no other contribution to the research.
References
You might also be interested in:
2021 - The renaissance of online medical education
2021 - Rural health research capacity building: an anchored solution
2008 - Clinical placement and rurality of career commencement: a pilot study

