Introduction
Canada’s vast geography is a considerable healthcare challenge because limited services are dispersed across a substantial land mass. As a result, under-resourced rural communities1,2 are unable to lean on large neighboring centers for support1-4. Locally relevant research is indispensable in these contexts; rural physicians intimately understand community barriers and needs, and their ability to create robust and evidence-informed solutions through academic pursuits is well recognized1. Yet, facilitating this research is no easy task; rural health research has been described as lacking order3 and requires a programmatic intervention to surmount considerable challenges.
Research capacity building is ‘a funded, dynamic intervention operationalised through a range of foci and levels to augment the ability to carry out research or achieve objectives in the field of research over the long-term, with aspects of social change as an ultimate outcome’5. RRCB programs are exceedingly rare, perhaps due to the same myriad issues that have long suppressed the voice of rural scholarship. At a time when science is increasingly interdisciplinary and the expectations of journals are more rigorous than ever, academic resources in rural areas are scarce. Designing and delivering an RRCB that effectively fosters research capacity despite these overwhelming odds is a logistical chimera that few scholars worldwide have achieved. How can a program support high-caliber academia in locations where there are no scholarly institutions, extreme distances between team members, poor communication technology, no mentors, and countless other barriers?
In Canada, our team has taken decisive action by developing a RRCB ecosystem comprising the 6for6 and Rural360 programs that is made possible by a unique anchored delivery model. In this article we describe how this model allows us to overcome the significant challenges of rural scholarship and achieve the features of an effective research capacity building program while catering to a rural audience.
6for6 and Rural360: background
6for6 is a research skills training program where rural physicians learn the fundamentals of research. The program is named after its unique format where six physicians attend six sessions comprising two graduate-level university courses covering topics such as scholarly writing, study design, team building, research conduct and qualitative and quantitative research. Participants (30 to date) also pursue a single capstone research proposal throughout the courses, meeting one-on-one with an expert academic mentor assigned to coach them through the process of research formulation, execution, and eventual publication. More details on 6for6, including mentorship and curriculum design and development through a rigorous needs assessment and curriculum development approach, are available in prior articles2,6. Articles demonstrating the high research productivity rates (eg grants, articles) and increased research competency (ie knowledge, attitudes, skills) of 6for6 participants7, and delineating the program logic and plan for a rigorous evaluation8, have been submitted for publication.
In 2017, we supplemented 6for6 with an in-house funding initiative called Rural360 that provides grants for research by physicians in northern Newfoundland and coastal Labrador. This program is designed to provide continued support for participants from this particularly isolated region to complete their projects. A previous article by Asghari and colleagues9 outlines the Rural360 program in further depth and provides preliminary evidence of its success in helping participants bring their projects to fruition.
Defining an anchored delivery model
An anchored delivery model is a centralized approach to RRCB, where a program harnesses the resources at an academic institution (the ‘anchor’) to foster research capacity in jurisdictions where those resources (eg funding, expertise, mentorship) are not available. The model is grounded in a conceptual framework that includes complexity science, systems thinking and anchored instruction, which facilitate scientific progress and knowledge translation. Multiple programs can be linked under an anchored delivery model to create an ecosystem for RRCB that yields scholarship and builds toward health system change.
6for6 and Rural360: an anchored RRCB ‘ecosystem’
The 6for6 and Rural360 programs complement each other and form an RRCB pathway catalyzed by a surrounding support network and sustained advocacy. The pathway builds toward research capacity by recruiting rural physicians, providing them with education in research fundamentals (6for6) to expand their capabilities, and funding their research projects (Rural360). This facilitates research that contributes to evidence-informed change within the health system, which then inspires other physicians to make research part of their portfolios as they observe its value for both rural practice and patients. Together, the programs work as a research incubator that nourishes rural physicians with support so they can develop a community of research and move toward being rural research leaders.
Conceptual framework
Complexity science, systems thinking, and anchored instruction models are core concepts that power our anchored RRCB ecosystem, spurring scientific progress and knowledge translation10.
Complexity science is a conceptual framework for change. It describes the complex relationships between systems and groups, how they behave, and how they adapt to change11. Implementing such change is largely influenced by context12, a dynamic and changing element in itself that can adapt with interventions. The rural context offers great opportunity for healthcare research because of its unique groups and subsequent need for unique interventions. Complexity science can assist in understanding how rural communities behave, and what researchers can do to appropriately adapt healthcare system interventions with regard for all the groups within the context.
Systems thinking is a holistic approach that articulates the components of a system, their interrelationships, and how smaller systems work within larger systems and over time. RRCB programming uses purposive systems (those with an end goal over a period of time13) to iterate the importance of building a research plan and attaining it throughout the course of the program.
Anchored instruction is a major paradigm in learning where a small group of people work together to comprehend and resolve lifelike problems. In this approach, the learning materials are presented in the context of a real-life event relevant to the learners, which helps to anchor or situate the materials. It enables learners to identify and define problems while exploring the content from several viewpoints. Anchored instruction provides opportunities for instructors and learners to work cooperatively in shared experiences14,15. This is an essential component of teaching in an RRCB.
Application of conceptual framework in practice
To envision how the complexity of rural health could be supported by generating and integrating knowledge, we identified different components of a rural healthcare research program and how it could work over time and within the larger system. Our RRCB ecosystem allows learners to participate in active learning, enables them to identify room for change within their current systems, and allows the program to grow with the learners over time (ie continuance of research projects through support and Rural360 opportunities).
Rural health complexities were the primary anchor or focus of this program. We established learning objectives to train participants, making them competent in investigating contextually important health problems. The use of rural health issues as the anchor encouraged rural physicians to see the anchor from their own perspectives, creating a narrative for their learning. These narratives were real-world issues brought to the table by every participant. This enabled an element of personal experience that facilitated learning links by exploring the problems identified through their clinical practice. Addressing the barriers of geographic isolation and lack of resources to conduct rural health research in situ, we supported participants with access to librarians, research assistants, mentors, subject matter experts, and graduate students from the main Memorial University campus. Another crucial component of the anchored delivery model was installing a dedicated staff member at the institution to act as a point of contact between the institution and the participants, connecting participants with resources and troubleshooting barriers to access. We also encouraged engagement of communities and citizens as partners during the program. We have articulated these components using logic models in our previous work.
Changes in participants’ understanding were developed through the introduction of new ideas by the instructors, from the learning resources, and from their peers. The instructors mainly worked as facilitators, supporting learners by developing instructional frameworks16 and helping them define their own learning goals. Learning plans were made to be suitable for busy rural practice with limited access to resources in remote areas. The learners were responsible for monitoring their own progress using the instructional framework and being involved in peer feedback. Learning in a group of six individuals, they were able to provide multiple opinions and suggest several solutions to each problem presented.
The entire anchored delivery process occurs within an environment of sustained advocacy for rural research with stakeholders and decision-makers, and support. Table 1 describes each of the guiding principles through which this is achieved and explains how each is actioned by our RRCB.
Table 1: Guiding principles of an anchored delivery model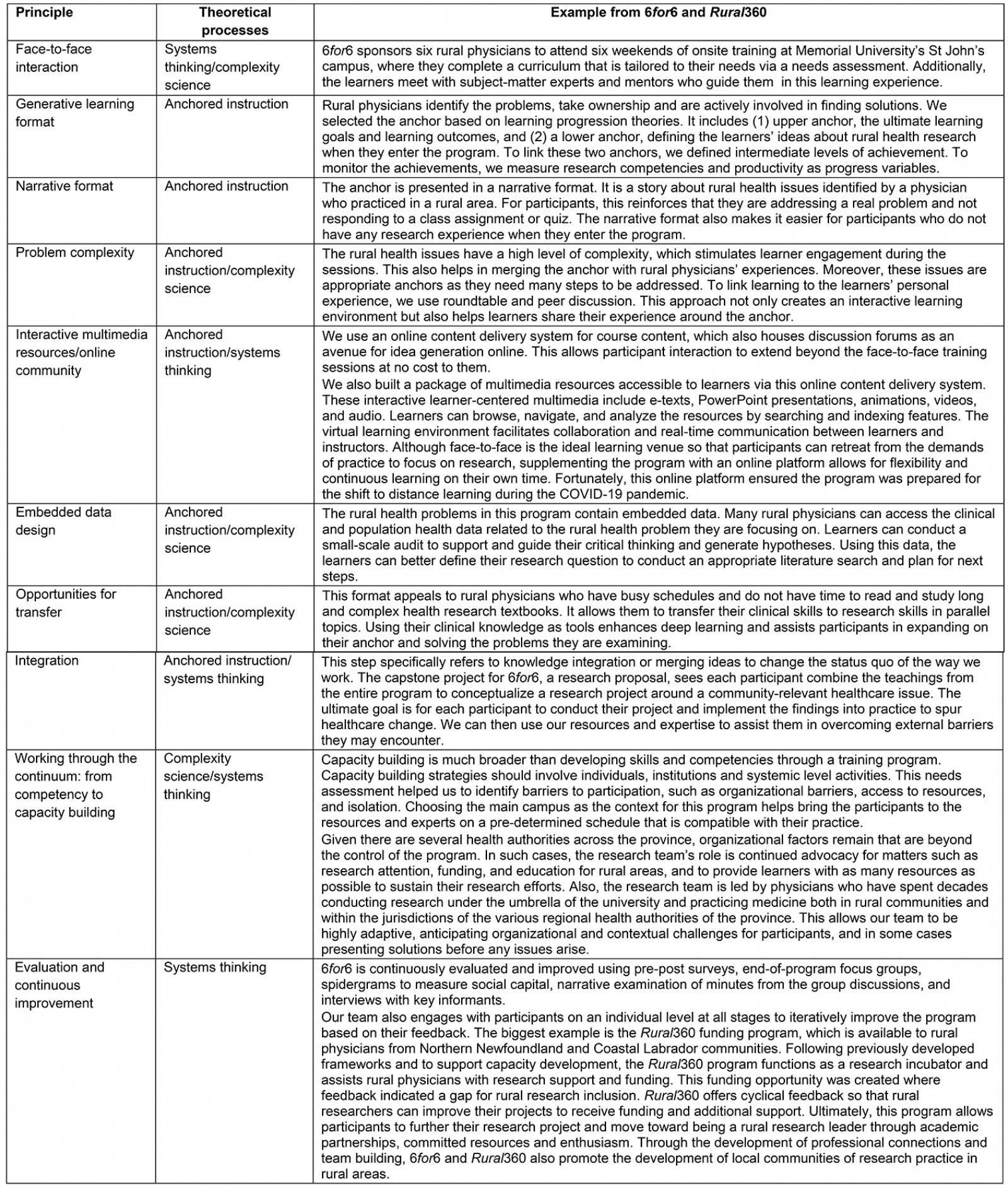
Outcomes of the anchored delivery model
The anchored delivery model enables key components of research capacity building typically precluded by the nature of rural areas. For example, geographical and professional isolation in rural areas7 restricts mentoring, networks, and collaborations; access to infrastructure; training; and research facilitators. Research funding, another crucial component, is also limited in rural areas1,17. By hardwiring the RRCB program to a resource pool where these elements are available, the anchored delivery model removes these barriers and facilitates research leadership and the prioritization of research objectives by research-inclined rural physicians. This results in important contributions to research priorities. Below are some specific outcomes of our anchored delivery model:
- Community of research practice: Communities of practice represent a critical mass of people or organizations working on a particular matter18,19. One of the goals of 6for6 is to generate a community of rural research practice across Memorial University’s jurisdiction. This community of practice can then leverage the resources, professional connections and training opportunities from Memorial University where they are more readily available. The end result is rural physicians who can conceptualize research with a broader scope, rigor and impact than normally possible due to local limitations. They develop a network of collaborators who can assist with their research project and continue to enhance communities of rural research practice after completing the training program. They ultimately develop the skills and confidence to contribute to and influence priority healthcare decisions.
- Self-organized group learning20: 6for6 participants schedule the training weekends as a group according to their availability and the bulk of learning is completed in-person to address geographical and professional isolation issues characteristic of rural life.
- Collaborative decision making and participatory action research21: The intimacy of the doctor–patient relationship in rural settings22 puts physicians’ fingers on the pulse of community and patient issues. 6for6 participants’ research projects are inspired by these relationships and, in a sense, are crowdsourced by triangulating numerous, rich conversations with patients to determine the issue that needs investigating23. Many participants involve citizens as project team members in varying capacities and disseminate their findings back to the public.
- Social accountability9: A central idea behind 6for6 is that participants apply the skills they learn to conceptualize and eventually conduct a research project that addresses a local healthcare issue. Overall, the impetus for these projects is physicians’ own empathy for their communities. This passion drives their learning and motivation and is enhanced through dialogue with other participants as they gain perspectives from other regions and knowledge of situations therein.
Discussion
The anchored delivery model can be used as a delivery approach for RRCB programming to help rural physicians harness academic skills and resources, and it has been an effective method of delivery for our ecosystem across several years. The many components of our model work together to create a personalized and effective learning environment and increase the opportunities for impactful results in rural communities that need it most. Overcoming research challenges associated with rural disparities is the underlying motivation of this particular delivery approach. We feel our work thus far may be useful for addressing the barriers and recommendations recently made by Lionis and colleagues24 for enhancing health research capacity.
The anchored delivery model is just one option. There have been a modest few other attempts around the world to provide rural health researchers with a framework of support25-27, including Schmidt and Kirby’s ‘modular’ Rural Research Capacity Building Program in Australia28, and Matsubara and colleagues’ academic consultation and referral service in Japan29. Schmidt and Kirby’s modular approach28 offers advantages (eg greater context by delivering the RRCB program in situ) and disadvantages (eg reduced access to resources due to delivery in low resource area) relative to the anchored design. However, by focusing on similar fundamentals as 6for6 and Rural360 (eg resource allocation, partnerships, leadership) their Rural Research Capacity Building Program, also described by Webster and colleagues in 201125, succeeded in empowering rural physicians to conduct research relevant to their community and practice, and emphasizes the importance of in situ research to the rural research capacity building process.
By contrast, Matsubara and colleagues’29 consultation approach includes elements of the anchored model but operates differently than described here; rural physicians correspond remotely with an expert who provides feedback on their work. This program also shares core concepts of resource allocation, partnerships and leadership with our programming, although the nature of email correspondence may be limiting compared to what is available in 6for6 and Rural360.
With many needs to be addressed in rural health research, we wish to encourage dialog about this exciting new area so that it may grow from a strengthened foundation of scientific discussion. Ultimately, there are pros and cons to any design, and models should be selected based on what best meets local needs.
Conclusion
Rural Canadians have long dealt with major health challenges and disparities30. As the historically under-appreciated matter of RRCB garners interest24,31, we hope attention will be paid to the factors that enable or prevent rural physicians from researching the required solutions. However, this growing emphasis on rural scholarship will occur in a system that has at times questioned its merit32. The anchored delivery model is a solution to empower rural physicians to break this mold to become researchers, scholarly practitioners, and purveyors of change.
References
You might also be interested in:
2016 - The answers are out there! Developing an inclusive approach to collaboration
2008 - Rural nurse job satisfaction
2005 - Recruiting undergraduates to rural practice: what the students can tell us


