Introduction
Bypass behavior occurs when people choose non-local rather than local health care1-3 and is common throughout the world in countries ranging from, for example, Australia to Tanzania and China to Brazil. Even across healthcare systems, patients often bypass local health care because it is perceived as inferior or inconvenient4-8. For urban residents, with a broader selection of health care, bypass behavior has a limited effect on the community. Still, for rural residents, bypass can have significant consequences on their individual and community wellbeing1. Because fewer clients and healthcare providers exist in rural areas, the loss of rural clients due to bypass behavior undermines the economic viability of rural clinics, contributing to their closure, and ultimately creating healthcare deserts1-3,9,10. Research also suggests that when rural residents utilize local care, some of the positive outcomes include reduced travel time, increased healthcare accessibility for vulnerable rural populations, and continuity of care throughout a patient’s life11. Because bypass can have such a significant effect on rural health care, a more detailed understanding of the drivers of bypass behavior is needed to help ensure rural healthcare access.
A growing body of research examining rural bypass behavior comes from the USA. In the USA, rural residents, on average, live twice as far from a hospital when compared to urban residents12. The country is geographically large, and in many midwestern and western states the rural population density is quite low, with limited resources. Many communities have limited healthcare providers. Bypassing local healthcare providers can, therefore, potentially threaten the economic viability of the few healthcare options in rural communities.
Most of the bypass research uses hospital records to examine rural healthcare selection. However, hospital records do not provide insights into individual care preferences, economic constraints, and other socioeconomic factors that influence decisions about health care1,3. Therefore, the current literature is limited in the scope and effectiveness of healthcare policy, resource allocation, and stakeholder decisions10-15. Other research suggests that bypass behavior is used to obtain better health care2,3,16 and assumes that residents are willing to travel further to obtain higher quality health care. Bypass is also associated with a perceived limited selection of local doctors or individuals who already use an out-of-town specialist9,15. However, a better understanding of why people bypass their primary care provider can help policymakers and practitioners provide better health care to rural residents and ensure adequate healthcare resources for rural and remote places.
Existing literature describes variation in bypass behavior by country6,17-19, state3, insurance type3, and on a rural–urban spectrum1. It also predicts the likelihood of bypass according to individual characteristics2,16, community characteristics10,20, frequency of care9, distance to hospitals, and hospital characteristics9,17. This study expands on these by measuring community ties, individual characteristics as well as a new index to measure and rank the social vulnerability of each town included in the sample.
Community context
More than geographic boundaries define a community. It is ‘filled up by people, practices, objects, and representations’ (p. 465)21. Other research concurs and conceptualizes community as ‘a particular way of organizing society in which the interactions essential to daily life remain embedded within primary ties in local solidarities’, rather than just a geographic space22,22. Thus, local amenities such as shopping, restaurants, and health care, as well as social ties and connections, are an integral part of the community experience, and essential elements of studies attempting to understand healthcare selection. Geographic mapping alone cannot capture how residents’ choices are shaped by the place they live.
Satisfaction with amenities and strength of community ties impact residents’ healthcare selection behaviors; previous healthcare research finds community patterns10,20. Previous research found that negative perceptions of local health care10,15 and dissatisfaction with community amenities such as shopping and restaurants10,23 can push rural residents to seek health care outside their community. Additionally, residents who already travel outside their communities for shopping or who work out of town are more likely to consolidate their travel time by bundling errands or commuting with health care, saving both time and money by scheduling healthcare appointments during the same out-of-town travel10,23. Alternatively, other community factors can encourage or pull residents to stay in town for health care. Strong community ties, increased number of friends, and friends who have interests in common decrease the incidence of healthcare bypass10,23. Thus, healthcare decisions are not exclusively an individual’s privilege or constraint, but these decisions are influenced by their community of residence.
This study replicates parts of the study by Sanders et al by including the same community push and pull factors for healthcare selection10, as well as testing two new community pull factors: dissatisfaction with local roads and length of residence. People who are dissatisfied with local roads are less inclined to drive further distances for their health care, and people who have lived in the community longer are more accustomed to local amenities that would pull them to use local health care. Community amenities and ties matter for health care. Thus, this study explains how several community variables influence residents’ healthcare selection while controlling for individual privilege, as well as place-based vulnerability.
Individual privilege and ability
Decisions to stay or bypass are made within socioeconomic privilege constraints. After all, regardless of how far away services are, less privileged people may not have the ability to bypass. Research shows that various socioeconomic factors influence the likelihood of bypassing, including age11,20, income11,19, education6,11,16, living in remote locations6,16, and being a recent migrant20. This study considered these various individual demographic factors, along with the intersection of community privilege and community vulnerability. By breaking down healthcare selection by not only individual demographics, but also how various privileges and disadvantages are exacerbated by community vulnerability, this study provides valuable findings for people who make macro-level healthcare decisions such as public healthcare workers, county health departments, and healthcare administrators.
This study answers the question of not only who is bypassing, but why they are choosing to bypass – information that is useful for clinic administrators, doctors, practitioners, and other rural healthcare workers. While previous research has examined who can bypass, the literature has largely overlooked the reasons for doing so. Because analysis of open-ended, short-answer responses is needed to understand why people bypass, this study contributes to the existing literature by providing an assessment of respondents’ short-answer responses explaining why they bypass. Understanding these reasons can help rural practitioners better meet local healthcare needs.
Place-based constraints
Previous healthcare research examined how distance from services affects healthcare access16; however, the research presented in this article measured the influence of place by incorporating not only a distance measure but including a place-based vulnerability measure that captured the influence of place on individual healthcare selection. The present study introduced an established measure – used in disaster literature for measuring characteristics of place – called the Social Vulnerability of Place Index, or SoVI, into healthcare literature. The SoVI comprises town-level socioeconomic variables from census data that contribute to a resident’s vulnerability (eg percentage of the population renting, per capita income, percentage of residents with insurance, median home value, and percentage of healthcare workers in the area)24-26.
Social vulnerability is partially the product of social inequalities – those social factors that influence or shape the susceptibility of various groups to harm and that also govern their ability to respond. However, it also includes place inequalities – those characteristics of communities and the built environment, such as level of urbanization, growth rates, and the economic vitality, that contribute to the social vulnerability of places (p. 243)25.
The SoVI has previously been used to understand resilience to natural disasters, migration27, and mental health28. Additionally, the SoVI has been used to map out individual medical needs and community healthcare access in Australia29, the social vulnerability of households to climate change in Ghana30, the social vulnerability of provinces in Indonesia for tuberculosis31, the social vulnerability of counties across the USA and prevalence of breast cancer among female veterans32, and a county-level analysis social vulnerability and the prevalence of Lyme disease across the US33. Thus, while the SoVI has been used in various countries29-31, as well as in studies examining various health problems28-33, this study contributes a novel approach to existing research by exploring the use of the SoVI as an indicator of healthcare selection. Individual healthcare selection decisions are made within various constraints: individual privilege and ability constraints, as well as community and place constraints. Understanding how place-based vulnerability affects healthcare selection will help public health workers better prioritize community sensitivity.
Summary and expectations
Bypass decisions are made within privilege and place constraints. Previous research has established that various community push/pull factors and individual abilities affect whether a person was likely to bypass. The present study introduced a measure of place-based vulnerability to the healthcare literature to illustrate how place privileges and constraints affect individual healthcare selection decisions.
This study contributes to the existing literature on healthcare selection and bypass behavior by (1) illustrating which privileges and abilities enable rural people to bypass their healthcare and which limitations discourage people to bypass, (2) showing which community ties influence individual healthcare selection, (3) measuring place-based social vulnerability level for each town via the SoVI, and (4) using open-ended short-answer responses to understand the reasons people give for bypassing healthcare available in their communities.
Methods
This study employed survey data collected from residents of 25 rural towns in the western US state of Utah during the summer of 2017. All of the towns had populations between 2500 and 5000. Sample frames were obtained from postal data, and respondents were selected using systematic random sampling. Respondents received three rounds of mail surveys using the Dillman approach34; towns with lower response rates received hand-delivered surveys. The adjusted response rate (which accounts for surveys mailed back as undeliverable or marked ‘return to sender’) was 51.44%, making the total sample size 1309. After accounting for missing data using listwise deletion, the total sample size was 1061.
Survey data addressed community sentiment, satisfaction with local amenities, self-reported health, healthcare-seeking behaviors, and demographic information. Additionally, open-ended responses from this survey asked respondents why they made their healthcare selection decisions.
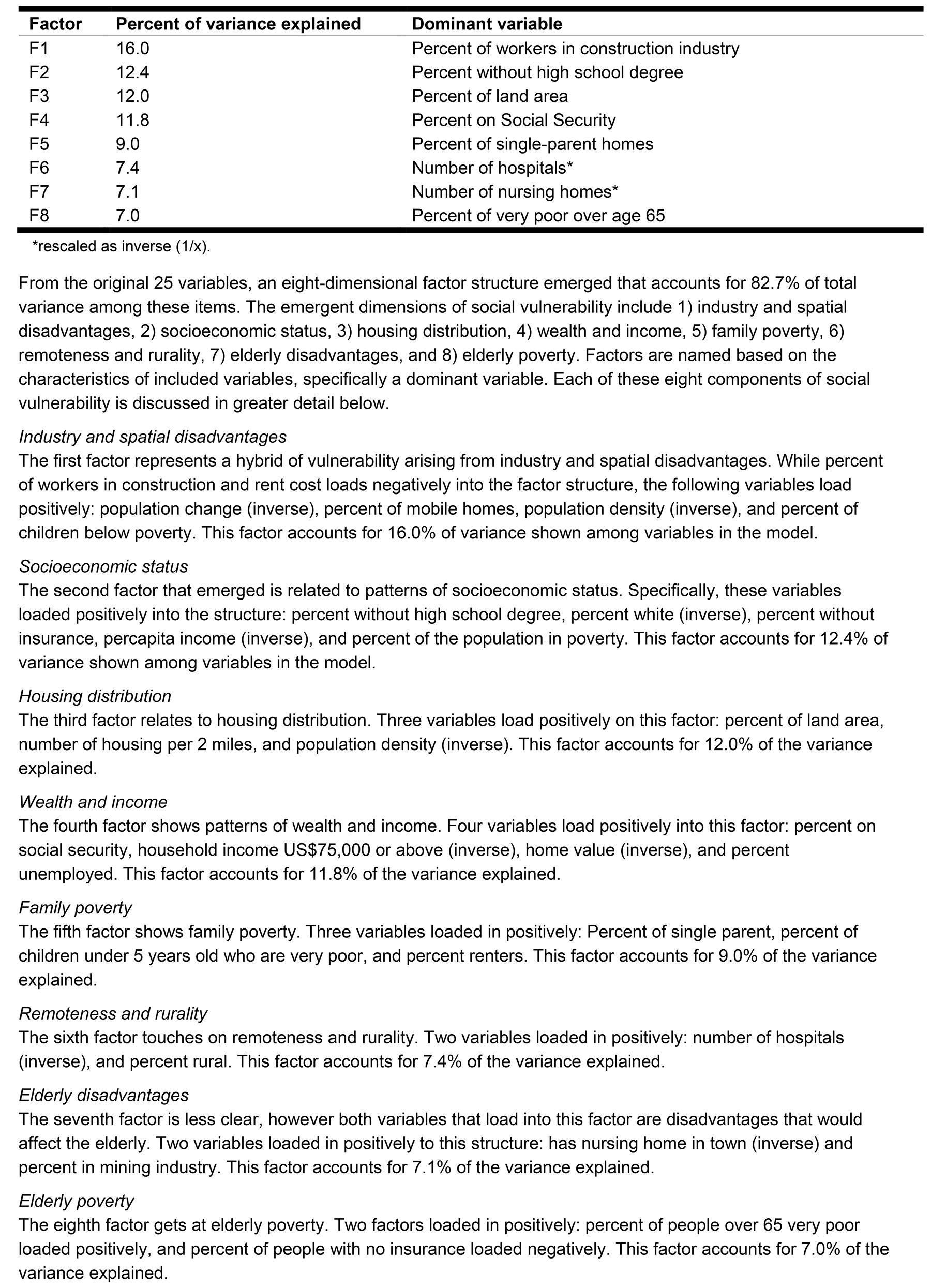
Supplementary data from the American Community Survey and the US Census were used to create a SoVI. Variables in the SoVI included, for example, per capita income, percentage of renters, mean rent cost, percentage spent on food stamps, and percentage rural. These variables were drawn for each town. The SoVI was created using factor analysis and, after the index was created, each town was assigned a SoVI score. Towns were then sorted into high, mean, or low vulnerability according to their SoVI score. If towns scored greater than one standard deviation above the mean, they were considered highly socially vulnerable, while those with scores less than one standard deviation below the mean were considered low socially vulnerable. Towns with scores within one standard deviation above and below the mean were considered socially vulnerable. For descriptive statistics about the variables drawn from census data that measure social inequalities, as well as place inequalities, included to create the SoVI, see Appendix I. For SoVI factor loadings, see Appendix II.
Measurements
Background: Previous measurements of bypass rely on postal codes and distance cut-offs to determine if people sought health care outside their community35. Such studies are limited because a person’s concept of community usually extends beyond their postal code. Other studies looked at whether people traveled outside their county15, or traveled long distances to hospitals3, to determine if respondents bypass care close to their residence. Others mapped the exact location of residents and their healthcare providers10. However, in ancillary analysis, phone conversations with the county health departments and Google Maps revealed the nearest clinic and hospital locations for each town in the sample. Next, researchers called local healthcare providers and clinics and asked where the nearest places patients in their community could go for specific services. Many rural providers reported that their patients had to go to the nearest metropolitan area, rather than a closer hospital or clinic, showing (with follow-up questions) that, in many cases, providers were unaware of the nearest health care to their communities. Such residents sent to metropolitan areas did not intentionally bypass closer local care – they were unaware of its existence. Thus, a self-reported healthcare selection variable was used in this study to account for the said measurement error.
Dependent variable
Primary care provider bypass: The primary care provider bypass variable was created using survey questions that first asked residents to self-report if they were seeking primary health care within or outside their community. Thus, this measurement took into account the resident’s perception of the boundaries of their community rather than a geographic range. If they reported seeking outside care, space was provided for them to explain the reasons for their decision. Responses such as ‘no healthcare available in my town’ were coded as 0 (for not bypassing). To make the bypass measure more conservative and precise, vague responses such as ‘availability’ or ‘that’s where the doctor is’ were also coded as 0 (for not bypassing) because it was unclear whether the respondent had the option to seek local care. Responses that indicated that the respondent had access to local care but decided to choose other care were coded as 1, meaning that the respondent deliberately bypassed local health care.
Independent variables
Community push factors: Dissatisfaction with local shopping and dissatisfaction with local health care are community push variables – residents who were dissatisfied with their community amenities were theoretically less likely to shop locally. Both of these variables were measured on a 1–7 scale, 1 being ‘very satisfied’ and 7 being ‘very dissatisfied’. Missing data were accounted for by mean substitution.
Community pull factors: Dissatisfaction with local roads is a community pull factor. If the roads in and surrounding a community are of poor quality, people would be less likely to leave their communities, especially during inclement weather. Dissatisfaction with local roads was measured using a 1–7 scale, 1 being ‘very satisfied’ and 7 being ‘very dissatisfied’. Percentage of friends in the community was measured ordinally. The categories were 0–25%, 26–50%, 51–75%, and 76–100% and indicated that the more friends people had in their communities, the more connected they felt to them. Finally, the length of residence, which measured the proportion of life for which respondents resided in the community, was considered a pull factor because those who have lived in the community for some time should feel more satisfied with its services and amenities.
Individual privilege: Because bypass behavior theoretically stems from ability and privilege to bypass, this study included various demographic characteristics to get a better idea of which kinds of privilege enabled individuals to bypass. Age was coded ordinally as 18–34, 35–49, 50–64, and ≥65 years, as found in other healthcare literature10. Dummy variables were included for sex (‘male’=1), marital status (‘married’=1) ) and race (‘white’=1). Race was included as a dummy variable because separate racial minority categories separate left too few cases for regression. Number of children is a continuous variable and was included because the more children a person has, the more difficult it would be to bypass because it is time-consuming and resource-draining to travel longer distances. Education is categorical and was coded as ‘no college’, ‘some college’, and ‘college or more’, as found in other healthcare literature10. Employment status was also included as a dummy variable ('working'=1). Income was treated as a continuous variable, with responses ranging from ‘$1–10,000’ to ‘$150,000+’ USD. This study also included a self-reported health variable from the Rural Utah Community Survey (RUCS) by asking, ‘On a scale of 1 to 7 how would you rate your health?’ Answer options were on a scale with 1 being ‘very poor’ and 7 being ‘excellent’. Missing data were accounted for with mean substitution. Distance to the metropolitan area was calculated for each town using Google Maps to calculate the distance between each town and the closest metropolitan area. See Table 1 for descriptive statistics about residents’ community ties and demographics.
Table 1: Descriptive statistics (n=1061) 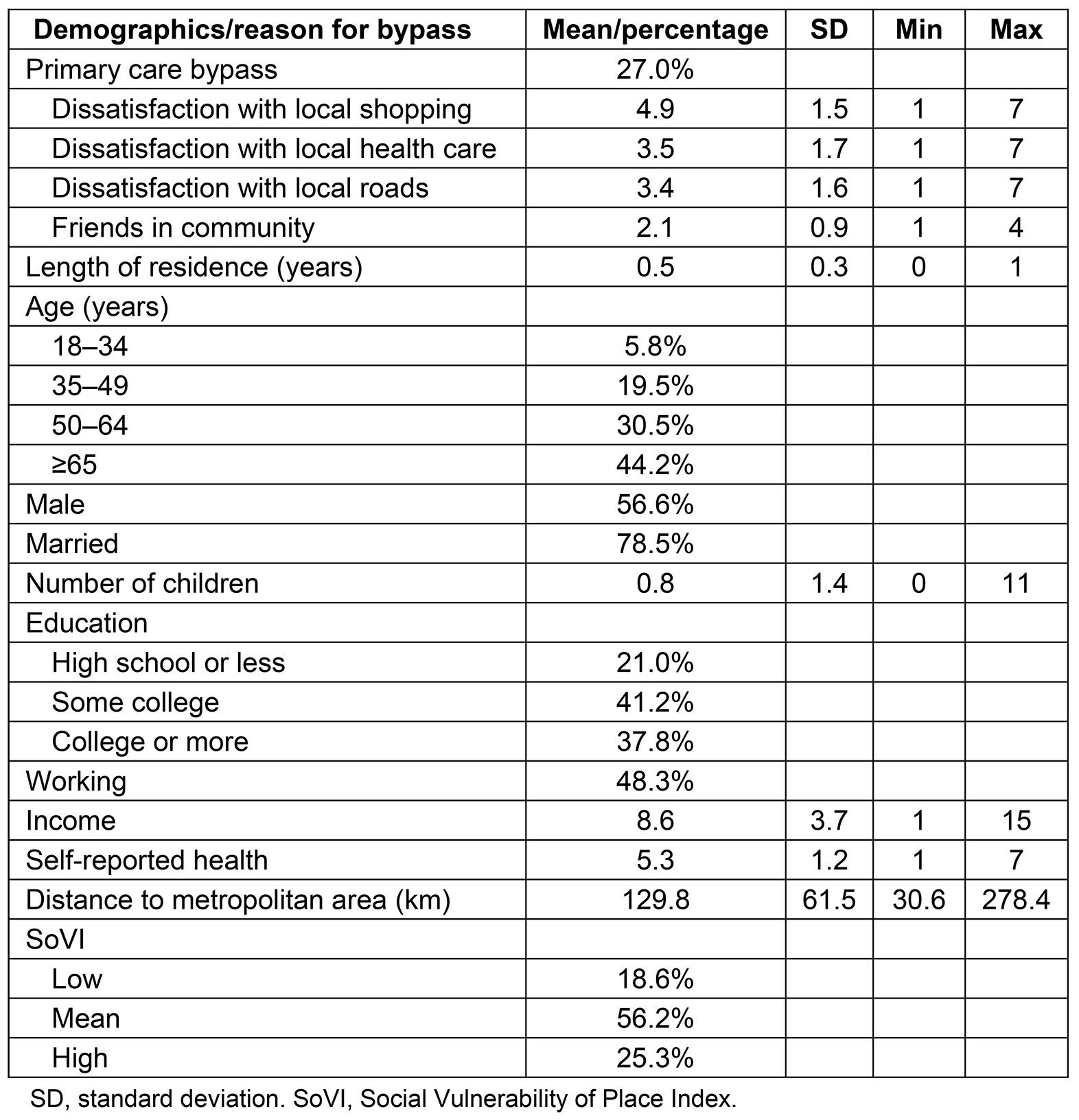
Social vulnerability of community (SoVI): The SoVI was calculated using factor analysis, and 42 variables that measured different socioeconomic characteristics of each town, such as percentage of renters in town, per capita income, and percentage of children under 5 below poverty. (See Appendix I for a comprehensive description of all variables used in this SoVI.) After calculating the index, each town was assigned a SoVI score. Towns that were one standard deviation above the mean were considered highly vulnerable, and those one standard deviation below the mean were low vulnerable. All towns selected for this study had small populations, were rural and remote, and were thus socially vulnerable. The SoVI shows, however, that there was variation in the degree of place-based vulnerability, even among relatively homogeneous residents.
Short-answer responses
Reasons for bypass: Responses were cleaned and sorted. Only responses from respondents who reported that they had access to primary health care in their community, but still chose travel outside their community, were included in this study. Taking a grounded theory approach, the researchers created categories for responses based on the content of responses. The categories drawn from the data include healthcare quality, selection, consistency, cost/insurance, one-stop shop, and confidentiality. Respondents who gave several reasons for bypass were included in each applicable category.
Analytic strategy
Logistic regression models predict the likelihood of bypass. Respondents with missing data for community measures, income, and self-reported health were accounted for using mean substitution. Respondents with missing data from age, sex, marital status, number of children, education, and employment were removed from these analyses using listwise deletion. Table 2 shows a pooled model of all 25 towns, and Table 3 shows the same model with towns separated according to SoVI.
Table 2: Logistic regression of bypass (n=1061)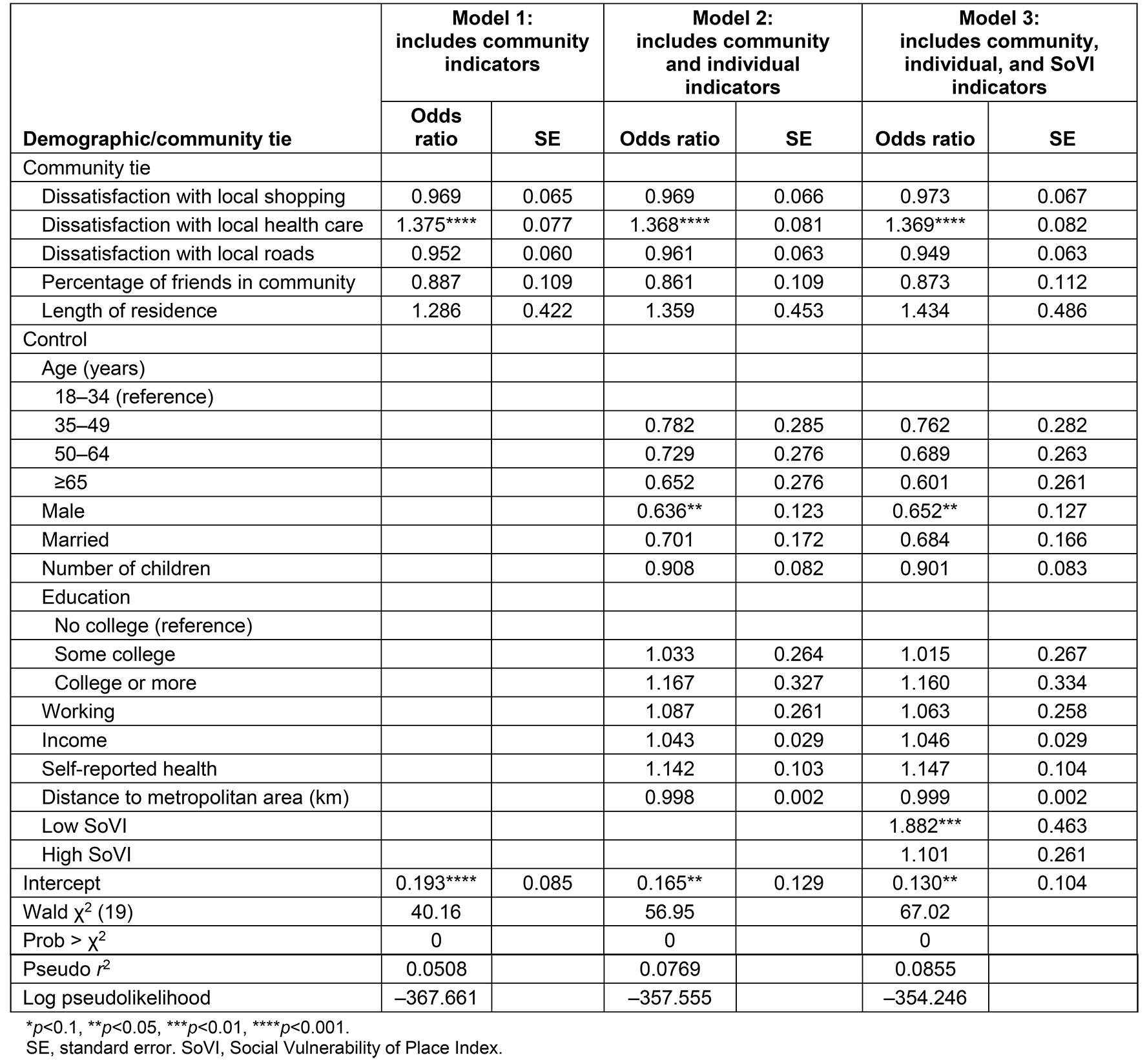
Table 3: Logistic regression of bypass by SoVI (n=1061)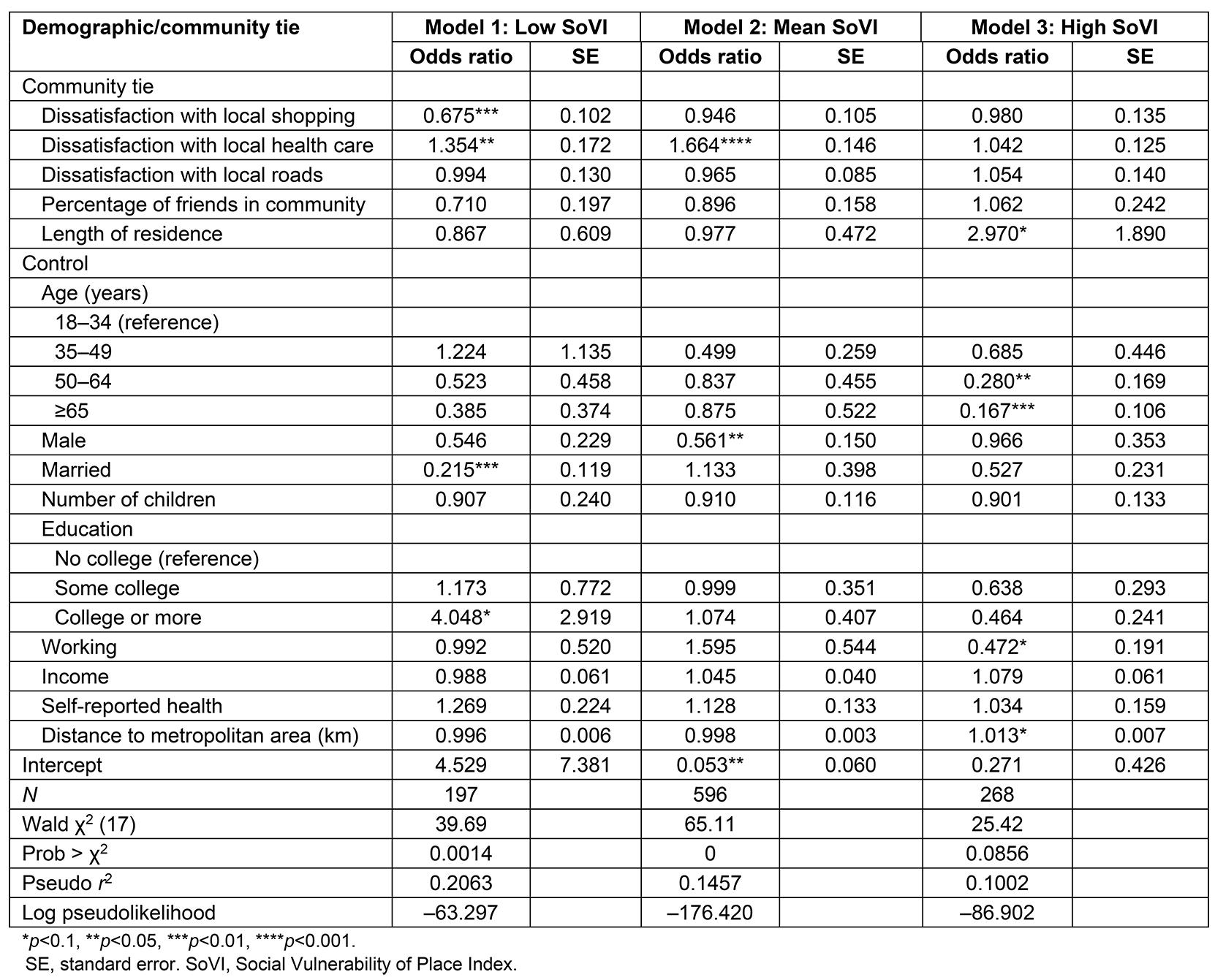
Ethics approval
The Brigham Young University IRB approved the RUCS (approval number E16349).
Results
Logistic regression estimates predicting odds of bypass are reported in Table 2. Model 1 (Table 2) shows a logistic regression predicting the odds of bypass for various independent variables measuring aspects of community and community sentiment. This study found that those who are dissatisfied with local health care are more likely to bypass local providers (OR=1.38). However, dissatisfaction with shopping, with roads, the percentage of friends in the community, and length of residence in the community have an insignificant effect on bypass behavior. Thus, dissatisfaction with local amenities, lack of community attachment, and lack of community ties are not significant push factors for the residents.
Because bypass behavior does not seem to be a community phenomenon, this study also brings in individual demographic characteristics in model 2 (Table 2). Controlling for age, sex, marriage, children, education, employment, income, self-reported health, and distance to nearest metropolitan area, the findings in model 1 are consistent: dissatisfaction with local health care increases the odds of bypassing local health care (OR=1.37), but no other community characteristics drive local healthcare-seeking behaviors. Additionally, of all the individual demographic variables, men are less likely to bypass local care than women (OR=0.64), but no other variable significantly explains bypass behavior. Model 3 (Table 2) includes a measure of the social vulnerability of place. Divided by one standard deviation from the mean, this model compares low socially vulnerable towns (low SoVI) and high socially vulnerable towns (high SoVI) to mean socially vulnerable towns (mean SoVI). These results show that, compared to the mean, residents in low SoVI towns are significantly more likely to bypass (OR=1.88).
To further investigate the relationship between bypass behavior and SoVI, bypass behaviors of residents in low, mean, and highly socially vulnerable towns were compared (Table 3). The likelihood of bypass can be explained with a combination of the level of town social vulnerability and individual privilege. Model 1 (Table 3) shows the community and individual characteristics that influence bypass behavior in low socially vulnerable rural towns. These residents live in less vulnerable places compared to the rest of the residents in the sample, which means that the characteristics of their community are advantageous. Interestingly, this study showed that those who were dissatisfied with shopping were significantly less likely to bypass (OR=0.68), while those who were dissatisfied with local health care were significantly more likely to bypass (OR=1.35) (Model 1).
Additionally, married individuals were significantly less likely to bypass than single individuals (OR=0.22), and those with a college degree were four times more likely to bypass local health care compared to those who did not go to college (OR=4.05). Thus, people living in the most privileged places, with privileged positions (single, more education) are more likely to bypass local care and opt for better care elsewhere. Model 2 (Table 3) shows that people living in areas of average social vulnerability, dissatisfaction with local health care have significantly higher odds of bypass (OR=1.66), and men in these towns are significantly less likely to bypass than women (OR=0.56). Model 3 (Table 3) shows that people living in highly vulnerable areas and those who have lived longer in the town are three times more likely to bypass (OR=2.97). Additionally, older residents have significantly lower odds of bypass compared to young residents (age 50–64 years, OR=0.28; age ≥65 years, OR=0.17), and people who are employed have significantly lower odds of bypass compared to unemployed people (OR=0.47). (Most of the ‘unemployed’ respondents are homemakers and retired people, both of which are privileged positions.) However, no other individual characteristic or privileged position significantly predicts the likelihood of bypass for people in highly vulnerable towns. Even so, unlike low SoVI residents, residents in high SoVI towns are more likely to bypass the further they live from metropolitan areas (OR=1.01).
This research contributes to the bypass literature by answering the following questions: ‘Who is more likely to bypass?’ and ‘Why are rural people bypassing?’ This research analyzed short-answer responses to understand people’s reasons for bypassing local health care. Table 4 shows the distribution of open-ended short-answer responses, with reasons for healthcare bypass, in six main categories: better quality health care, greater selection, consistency with provider, lower cost or insurance network, one-stop shop, and confidentiality. Residents who said they bypassed local health care for better quality health care elsewhere offered comments such as ‘No physicians here, only PAs [physician assistants],’ ‘Because it’s scary going to local hospital + physicians. Too many mistakes made + lack of knowledge + common sense. I have to tell them what to do,’ and ‘I don’t want to die.’ Perceived low-quality local care, as well as negative experiences with care, pushed people to bypass their care. Rural clinics can focus on increasing the quality of their services to pull people to use local clinics. Respondents who cited a greater selection of providers as their reason for bypass said, ‘Very limited options for healthcare in my community’ and ‘choice (female GYN) quality & privacy.’ Increasing the number of providers as well as increasing the types of specialist providers could pull people to use local services rather than bypass. Those who wanted consistency with their primary care provider were willing to bypass local care: ‘Hometown with doctors I know’ and ‘Family doctor for 30 years.’ Rural providers that can build trusting relationships with new residents might be able to encourage them to use local care rather than continue their care in their previous community. Those who mentioned costs as reasons for bypass commented, ‘Better Healthcare and much cheaper!’ and ‘Affordability with regards to insurance providers.’ Healthcare administrators who broaden the number of insurance networks accepted at their clinics could appeal to residents who have obscure insurances. Additionally, any financial assistance or payment plans should be made known to prospective patients. Interestingly, respondents mentioned concerns about confidentiality with their local care, saying that ‘People know your health issues (they) come out of the doctor’s office’ and ‘I don’t want locals knowing my business.’ Clinics need to ensure that all staff keeps patient information confidential. Regular HIPPA (ie legal requirements for patient confidentiality) training could help remind staff of the importance of confidentiality, and posted signs around the clinic could help patents feel more trusting towards providers, as well as remind staff to keep patient details private. Others said that they had already bypassed for other reasons, including ‘Because other family members have doctors there’ and ‘Better care and visit family.’ These responses indicate that they bundle personal and family health care or other social needs, which could be more difficult for existing rural providers to address. New rural clinics, however, should choose their location carefully, selecting real estate close to town centers or other important amenities.
Table 4: Reasons for bypass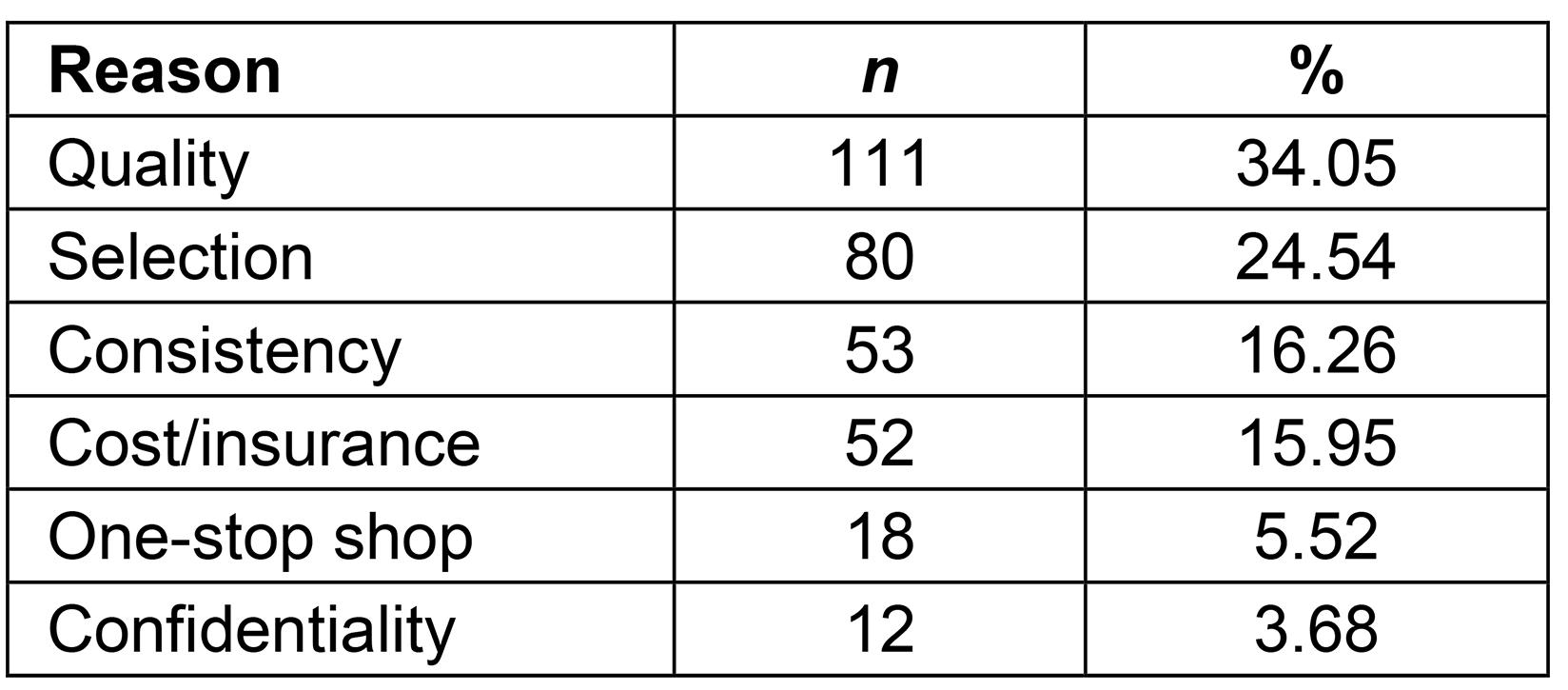
Discussion
Healthcare selection varies depending on various household and individual socioeconomic characteristics, community sentiments, and socioeconomic status of place. This research expands on existing bypass literature by including the SoVI to understand the likelihood of individual bypass behavior according to the social vulnerability of the town. This is arguably the greatest contribution this study makes to healthcare bypass literature; by incorporating the SoVI, this study provides a clearer picture of individual indicators and community indicators to rural healthcare selection behavior than models that look at rural healthcare selection without a place-based breakdown (compare Table 2 to Table 3).
Table 2 shows that, despite the findings of previous research10, community ties are not significant push and pull factors for healthcare selection amongst rural residents. Significant, however, is their perception of local health care. Thus, local clinics should ask for and incorporate feedback from their patients, helping residents feel more confident in their local health care. Doing so could help small clinics retain patients and ensure that their clinic doesn’t close, contributing to a rural healthcare desert.
It is worth noting that, while men were more likely to bypass than women (Table 2), the rest of the individual privilege indicators included were not significant. This non-finding is important for other healthcare researchers. Especially in cases studying rural health care, where populations tend to be more homogeneous (in race, income, etc.), the effects of individual privilege variables on health care might be washed out. The most interesting findings of this study are illustrated by first identifying the vulnerability level of each town and then, while controlling for place-based vulnerability, showing how individual privileges are significant, and certain privileges matter more depending on place vulnerability level (Table 3). Thus, the explorations in this study of using the SoVI in measuring primary healthcare selection generally should be applied to other rural healthcare research studies.
Limitations
Because this survey was not asking about health care exclusively, but also included sections on community, education and employment, there were fewer questions about health care compared to datasets used in previous healthcare literature. The RUCS lacks information about the respondents’ health insurance, frequency of use, and personal illness or injury.
Additionally, this survey was limited to rural Utah, and the 25 rural towns included were predominantly non-Hispanic White. Therefore, this study’s findings are not generalizable to more racially diverse rural populations. Additional research is needed to more fully understand how and if bypass behavior varies across different racial and ethnic communities. The goal of this study, however, was to test the SoVI in more broad healthcare research. This study shows that the SoVI facilitates understanding healthcare selection; other healthcare researchers should consider using the SoVI when studying bypass in other settings. Thus, even with these limitations, this study’s findings do provide new insights into healthcare selection for geographically remote populations and are consistent with the general findings of several international studies4-8,10.
Conclusion
The SoVI helps to outline healthcare vulnerabilities – not just disaster vulnerability as in previous research24-26,29-33,33. This study shows that social vulnerability is a significant indicator of healthcare selection. Similarly to previous research24-26,29-33 this study used publicly available census data to create the SoVI, making the index relatively accessible and straightforward. Thus, healthcare policymakers, county health departments, and other stakeholders can create SoVIs for towns in their regions to identify areas that need higher investment in healthcare infrastructure. While supplementary healthcare data is needed to understand local needs better, the SoVI alone can help officials target healthcare resources when policymakers or county health departments lack the resources to gather the data. This study’s novel contribution suggests that the SoVI should be utilized in other settings where healthcare policy, resources, and funding decisions are being made.
People living in low SoVI towns are significantly better off compared to medium and high SoVI places. However, the present study found that residents were more likely to bypass compared to the residents living in mean SoVI towns (Table 2, model 3). Considering which people in low SoVI towns are more likely to bypass health care, this study found that the privileged are most likely to do so (Table 3, model 1). Increased bypass amongst privileged people, however, can create healthcare wastelands and negatively impact less privileged people living in low SoVI towns. Thus, policymakers should ensure that healthcare services in low SoVI areas meet the needs of less privileged residents.
For residents in high SoVI towns, those who are long-term residents are three times more likely to bypass local care. Long-term residents, when compared to new residents, feel the quality of health care is poor, or have concerns with confidentiality (Table 4). Additionally, this study shows that, although no amount of individual privilege helps people to bypass in highly vulnerable areas (Table 3, model 3), living further away from metropolitan areas makes those in such areas more likely to bypass. This finding has implications for policymakers: highly socially vulnerable areas that are also remote should be targeted to improve healthcare quality, selection, cost-effectiveness, and confidentiality for those living there.
Furthermore, the SoVI works for researchers looking at healthcare selection processes. This is perhaps this study’s most important contribution: social vulnerability of place matters for health care. Privileged people – those who live in low vulnerable areas and have individual privileges such as higher education – often seek health care elsewhere, although education does not help those in medium and highly vulnerable places to seek outside care. The information provided by the SoVI helps providers and policymakers to use a more targeted approach to public health. Rather than targeting only those with low educational attainment for all rural areas, stakeholders can broaden their reach to highly vulnerable areas while focusing on those with lower educational attainment in low vulnerable areas. Additionally, this study shows that aging populations in highly vulnerable rural areas need additional help to access better health care. Healthcare selection is best understood as a multifaceted process that includes not only community ties and individual ability but also the area’s social vulnerability. Future healthcare research should utilize the SoVI in other settings to confirm the index’s applicability to healthcare questions and articulate more precise findings.
This study’s final contribution is the coded responses to the short, open-ended questions that provide information about why people bypass. These explanations can help rural providers address concerns that people have with local care. Based on this study’s findings, rural providers can focus on increasing the quality of their services, expanding their insurance networks, and/or ensuring confidentiality. Resolving concerns with local care will result in fewer residents bypassing and the prevention of rural healthcare deserts.
References
appendix I:
Appendix I: Descriptive statistics of variables composing the Social Vulnerability of Place Index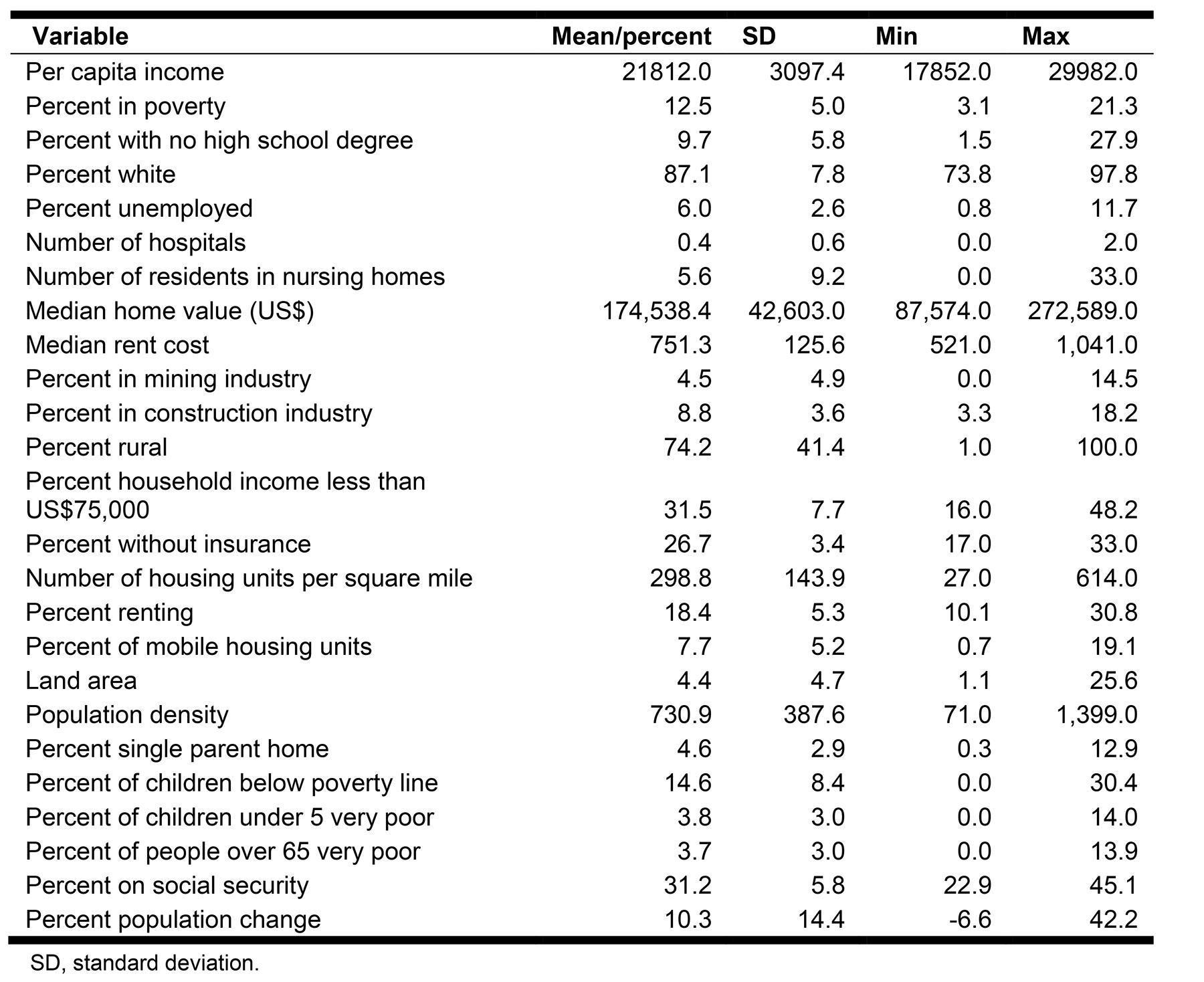
You might also be interested in:
2020 - Why we need better rural and remote health, now more than ever
2008 - Obstetric services in small rural communities: what are the risks to care providers?