Introduction
One of the most common causes of poor dental health is dental caries, or tooth decay, which are caused by the bacterial breakdown of tooth enamel1. Dental caries are preventable, and although the prevalence has decreased over time in the USA, it remains the most common chronic disease among US children2.
Factors contributing to poor oral health among children shadow disparities in sociodemographics. Research conducted by Flores and Tomany-Korman revealed that African American, Native American, and Latino American children have poorer oral health as compared to their white, Asian/Pacific Islander and multiracial counterparts3. This study also reported that Latino Americans had the highest rates of dental caries3. The observed racial/ethnic differences can be influenced by differences in dietary practices and other factors, such as lower socioeconomic status and low birth weight4.
The impact of social determinants such as socioeconomic status on oral health was recently recognized by the American Academy of Pediatric Dentistry5. The 1999–2004 National Health and Nutrition Examination Survey data show that 54% of children aged 2–11 years whose family income was less than 100% of the federal poverty level had dental caries, and 32% of those children had untreated dental caries6. The survey also showed that those who are black, Hispanic, or have low socioeconomic status have greater rates of dental decay and a higher frequency of untreated teeth compared to other children aged 2–11 years6. Although 38.7% of children who are at or below 200% of the federal poverty level had received preventive dental care in the past year, children living in poverty were more than twice as likely to have untreated decay (24.7%) than were children in families whose income exceeded 400% of the federal poverty level (9.1%)7,8.
Additionally, environmental and interpersonal factors that may influence disparities in dental caries among children include educational attainment of parents, access to dental care, diet, genetic predisposition, bacteria, salivary production issues, fluoridated water, and geographic location9-12. Differences in the development of dental caries among children may correspond to disparities in rural–urban oral healthcare access and outcomes12-15. Barriers to oral health care include access, which remains a top rural health priority, and utilization of care, economic factors, and limited dental workforce in rural areas16. These barriers impact not only the receipt of dental treatment but also of preventive oral health care: children aged 1–17 years in rural areas are less likely to undergo preventive dental visits than children in urban areas17.
Purpose of the study
A 2019 report by the United Health Foundation on the health rankings in the USA places Louisiana as 49th in the country in regard to health indicators18. As of 2014, out of 64 parishes, 54% were classified as rural and over 46% of these are designated dental health professional shortage areas (HPSAs)19. In 2018, there was an estimated rural population of 749 722 out of 4 659 978 individuals in Louisiana20. Furthermore, 25% of the rural population are Medicaid enrollees, while 16% were uninsured15. The prevalence of dental caries among Louisiana’s children is higher compared to the national estimate (53%) and the Healthy People 2020 goal of 49%. 7,21. Furthermore, the percentage of untreated caries is higher among Louisiana children compared to the national levels21.
To the authors’ knowledge, there is a gap in the literature that describes rural–urban differences in oral health outcomes among children, especially in Louisiana. Thus, the purpose of this study is to assess the distribution of dental caries and examine the association between the mean decayed, missing or filled permanent teeth (DMFT) scores and other variables among elementary school-aged children in south-eastern Louisiana. The main outcome of interest was any rural–urban differences in dental caries and DMFT outcomes.
Methods
Study design and population
This cross-sectional study used dental screening and sealant data from The Health Enrichment Network (THEN), a community health outreach non-profit organization funded by the Health Resources and Services Administration, of 46 public and parochial elementary schools from south-eastern Louisiana parishes, which included 963 children. The screening and sealant data comprised a convenience sample collected by THEN’s school-based dental sealant program from 2007 to 2014. The authors were not provided with information regarding the number of eligible children for sealants nor the number of children who received sealants but did not consent to participate in the screening. The program adhered to the Centers for Disease Control and Prevention’s Sealant Efficiency Assessment for Locals and States (SEALS) program, which is designed to capture, store, and analyze data from school-based sealant programs. The Louisiana Department of Health and the local school boards to provide the services contracted THEN’s school-based dental sealant program. Parents provided consent for their children to participate in the school-based dental sealant program. Data were de-identified and entered into a REDCap database.
Measures
The primary outcome of interest was the presence of DMFT diagnosed by volunteer dentists using a basic screening clinical examination. The data were collected through retrospective screening forms, so the authors did not have information about the number of dentists that assessed children’s teeth. In this study, DMFT was defined as any caries experience in permanent molars. Therefore, the DMFT scores could range from 0 to 8. DMFT scores were dichotomized, comparing no caries experience (DMFT=0) to any caries experience (DMFT≥1).
Schools were classified as either rural or urban using the US Census classification of each school address. Additional information including age, sex, race/ethnicity, and dental insurance status was obtained during the dental screening process. When urgent need was identified by the volunteer dentist, the child was referred for urgent care. Urgent need included child having pulpal exposure, abscess, a tooth requiring extraction, as well as extreme rates of decay among other urgent indicators, and this was determined by the dentist’s expertise and reporting after assessment.
Statistical analysis
Descriptive statistics (eg mean and prevalence) depicting children’s demographics and oral health outcomes were estimated. The χ2 test was used to assess rural–urban differences among children with any DMFT. Univariate and multivariable logistic regression were used to estimate the prevalence odds ratio (POR) between DMFT and rural–urban differences, with adjustment for covariates considered confounders. The association between DMFT and each study variable (age, race/ethnicity, and grade level) was examined with a separate model. Three multivariate logistic regression models were assessed to analyze the relationship between DMFT and geographical location. Age and race were adjusted for in model 1; in model 2, gender was added; and model 3 had two additional variables: insurance and grade level. Based on model fit statistics and likelihood ratio test, model 2 was found to be the best fit to explain the relationship between DMFT and the geographical location of school. All statistical analyses were performed using the Statistical Package for the Social Sciences v9.4 (SAS Institute; http://www.sas.com).
Ethics approval
The study protocol was reviewed and determined to be an exempt research activity by the Louisiana State University Health Sciences Center – New Orleans Institutional Review Board.
Results
Dental screening forms for 963 children, of whom 58% attended schools in rural communities and 42% attended urban schools, were analyzed. Over 30% of the total study population had some dental caries. Table 1 shows the demographic characteristics of the study population categorized by geographical location of schools. While children 6–8 years of age were evenly distributed between rural (49%) and urban (51%) schools, among children aged 9–12 years, 62.5% were in rural compared to 37.5% in urban schools. The population of rural school children was 58.4% non-Hispanic white and 38.7% non-Hispanic black, compared to urban schools with 22.4% of the population non-Hispanic white and 75.5% non-Hispanic black children (p<0.0001).
Among rural schools, 35% of children had a DMFT score ≥1 compared to 19% of urban children. The mean DMFT was greater (0.82) for rural children compared to urban children (0.58) (p<0.0001). A total of 38% of rural children were referred for urgent treatment, while 24.6% of the urban children presented with urgent treatment needs (p<0.0001). Sixty-three percent of the rural children reported having Medicaid or the State’s Children Health Insurance Plan compared to 27% of the urban children; however, a larger proportion of urban screening forms reported insurance as unspecified. About 28% of the screening forms did not report information on insurance.
Table 2 presents the crude PORs for the association between DMFT and other variables. The crude analysis showed that children who attended rural schools were twice as likely to have any DMFT compared to children who attended urban schools (POR=2.17, 95%CI: 1.61–2.93). Similarly, non-Hispanic black children (POR=0.55, 95%CI: 0.41–0.74) had reduced risk of any DMFT compared to non-Hispanic white children. Additionally, rural children were 1.88 (95%CI: 1.41–2.50) times more likely to need urgent treatment, 1.95 (95%CI: 1.46–2.59) times more likely to have an untreated cavity, and 1.17 (95%CI: 0.90–1.52) times more likely to have dental caries than their urban counterparts.
Table 3 presents POR for the status of DMFT controlling for age, race/ethnicity, and grade level. Children who attended rural schools were 2.07 (95%CI: 1.47–2.91) times more likely to have a DMFT score of at least 1 compared to children who attended urban schools. Adjusting for the similar set of covariates, non-Hispanic black children had reduced risk of DMFT compared to non-Hispanic white children (POR=0.70, 95%CI: 0.51–0.97). The mean age for non-Hispanic black children was 7.90 years and for non-Hispanic white children 8.31 years.
Table 1: Characteristics of screened children for rural and urban schools in south-eastern Louisiana (n=963)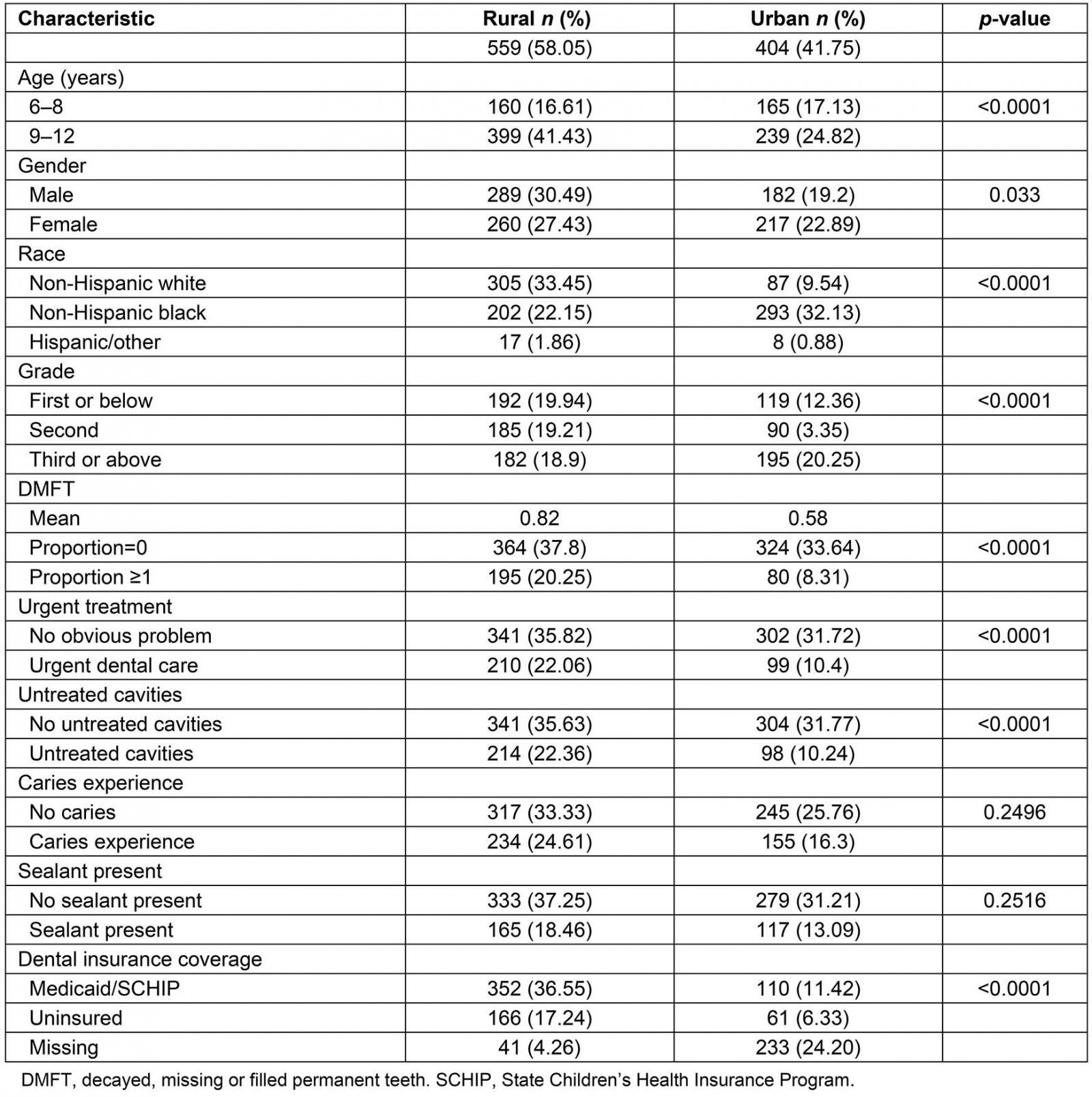
Table 2: Unadjusted prevalence odds ratios and 95% confidence intervals for dental outcomes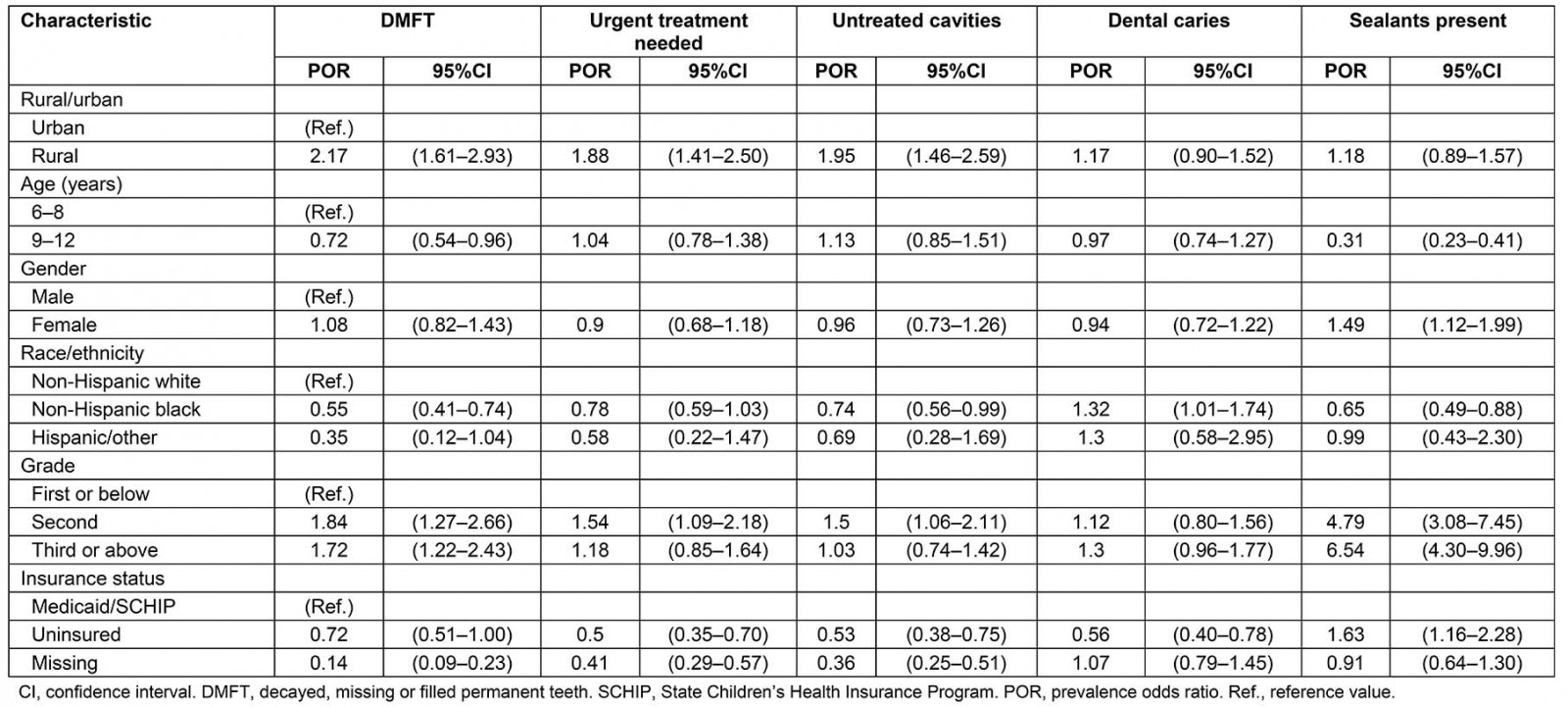
Table 3: Adjusted prevalence odds ratios and 95% confidence intervals for damaged, missing or filled permanent teeth from three models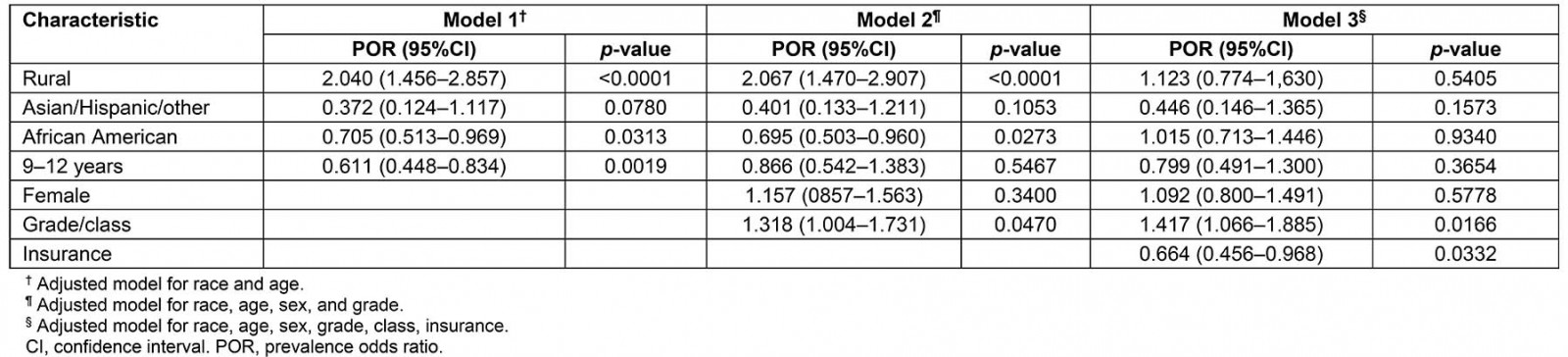
Discussion
This study highlights the rural–urban disparities in dental caries distribution among elementary school-aged children across 46 schools in Louisiana. The study found that about 40% of the children, regardless of whether they attended school in a rural or urban area, had a caries experience. Slightly over 30% were observed with untreated cavities, which is higher than the national prevalence of untreated dental caries of 18.6%22. The findings are inconsistent with observations from the 2009 Louisiana Bright Smiles for Bright Futures basic screening survey of third-grade children, which found 65.7% of children had any caries experience and 41.9% reported with untreated cavities23. This may be explained by the smaller size of the study population included in the present study’s analysis compared to the larger size of the study population of the Louisiana Bright Smiles for Bright Futures study. Regardless, the burden of childhood dental caries is higher in Louisiana compared to national estimates.
Higher DMFT scores are found to negatively impact children’s quality of life and school performance24. The mean DMFT scores for rural and urban children in this study were 0.82 and 0.58, respectively. It is difficult to draw comparisons between this study’s results and the results of other studies because previous studies assessing the prevalence of dental caries using the DMFT score often used the WHO criteria to calculate the score and they assessed all teeth, not only molars24-31. However, in research conducted by Wang et al, where all teeth were assessed using the DMFT score, molars were found to be the most affected30. This may suggest that the present study’s mean DMFT scores are of significance, considering only permanent molars were assessed, and require further research to determine whether or not, and how, assessing all teeth will impact the DMFT score for rural and urban children30.
The authors observed rural children had an increased risk of any DMFT as opposed to urban children, and this remained after controlling for age and race/ethnicity. Global studies corroborate these findings in that children and adolescents in rural areas tend to have poorer DMFT scores compared with their urban counterparts25-28. This study also showed that over 30% of the children in both rural and urban schools needed urgent dental care, which is lower than estimates previously reported for urgent dental care need among children in Louisiana. However, as with the present study the need for urgent dental care was higher for children in rural schools than urban schools23. Furthermore, rural children in Louisiana were found to be at increased risk of having untreated cavities than their urban counterparts. This may be because rural areas are often characterized by childhood poverty, unemployment, low education, and fewer healthcare providers, which are social determinants of oral health14. The availability of dentists may also impact oral health. Some parishes in Louisiana have one dentist per over 7700 individuals32.
The present study’s findings compel the need to explore the social determinants that have been documented in the literature that affect dental care utilization, such as poverty levels, dental HPSAs, oral health literacy, and insurance, specific to rural Louisiana33,34. This study indicated that the majority of children in rural areas reported being insured by Medicaid or the State Children's Health Insurance Program (SCHIP), which is not surprising considering the national observation that children in rural areas are more likely to have public insurance than those in urban areas14,17,35. Despite the Early and Periodic Screening, Diagnostic and Treatment Medicaid benefit and efforts to improve children’s oral health through Medicaid, those who are Medicaid or SCHIP recipients may face the challenge of accessing oral health care, as only one third of dentists in the nation accept public insurance, and 43% of dentists in Louisiana participated in Medicaid for child dental services in 201433,36,37. Furthermore, dentists accepting Medicaid may not correlate with access to dental care among Medicaid children; factors such as geographic distribution, need, and convenience play a role in accessing dental care38.
This study found that non-Hispanic African American children had a reduced prevalence of any DMFT compared to their non-Hispanic white counterparts. However, previous studies assessing racial/ethnic disparities found that Hispanic children, followed by non-Hispanic black children, had an increased risk of DMFT as compared to non-Hispanic white children39,40. The contrast in findings between the present study and others may point to a possible selection bias in this study and the need to assess other potential confounding factors that may explain if any true difference exists. Furthermore, the increased risk of DMFT among older children as compared to younger children is similar to national trends6.
Research is limited regarding the analysis of factors that contributed to differences in oral health in children across the country. A comprehensive, national database is not readily available to identify current contributors to poor oral health, and this makes it difficult to compare differences among states and other demographic and genetic factors3.
Limitations
Although this cross-sectional study provides insight into children’s oral health in south-eastern Louisiana, there are several limitations. First, the study population was a convenience sample of children with parental consent, which may have introduced selection bias, as evidenced by the reduced prevalence of DMFT among non-Hispanic black children, which was inconsistent with previous literature on oral health disparities. Furthermore, this limits the generalizability of the study. Second, the different dentists (who were not calibrated), screening the students and the screening forms used to record the presence of caries, sealants, and DMFT scores were subject to various changes throughout the years; thus, data collection was inconsistent because two different forms were used. Third, there may have been a measurement error, which may have led to an inaccurate estimation of the association between DMFT and geographic location. Furthermore, there may be a potential underreporting of the caries experience in this study considering that DMFT was defined as presence of caries in permanent molars and did not include the evaluation of primary teeth.
Implications for research, practice, and policy
Oral health remains one of the top health priorities in rural areas, especially for mid-western and southern states16. The present study’s findings indicate that a sample of children from the eight Delta states in the USA exhibited high rates of dental cavities and untreated cavities, which are preventable, as well as the need for urgent treatment, and that the caries burden is higher among children in rural areas than those in urban areas. This points to the need to better understand why such distribution exists and the critical steps needed to be taken to improve oral health outcomes for children in Louisiana.
Although the prevalence of untreated caries is decreasing overall among children, especially in minority children, racial/ethnic disparities still exist41. Therefore, mechanisms that explain these disparities need to be identified40. Programs and policies addressing the social determinants of oral health, such as community water fluoridation and access to providers who accept Medicaid and services, need to be refined and implemented14,42. Initiatives to improve oral health in rural Louisiana are underway, such as the Dental Rural Scholars Track program to advance the workforce, the Louisiana Seals Smiles program to increase dental sealant outreach, and the fluoride varnish campaign. Other possible programs and policies to implement include medical–dental integration, community dental health workers, teledentistry, and increasing dental hygienist practice jurisdiction.
Despite its limitations, this study contributes to the literature on rural–urban differences in oral health status and adds to the limited body of research on Louisiana children’s oral health. To the authors’ knowledge, this is one of the first studies that aims to assess the distribution and association of dental caries among rural and urban children in south-eastern Louisiana. Further research is needed on the extent of rural–urban geographic variations in oral health for Louisiana’s most vulnerable populations. This is needed in order to comprehensively define the extent of the problem to inform the development and implementation of proper programs and policies.
Acknowledgements
We would like to acknowledge Marissa Duckett and TΗΕΝ.


