Introduction
Retaining a health workforce willing to serve in rural areas is a global problem faced by both developed and developing countries1-5. Various strategies and recommendations to retain doctors have been developed and suggested by WHO1,2 and have been implemented. These include a year of compulsory service in rural areas for new medical and specialist graduates, offering high financial incentives to work in rural areas and giving priority in specialist training admission for doctors who have rural service experience. The evidence suggests that interventions based on incentives have worked well for recruitment, but not for retention6. These approaches are mainly behaviorist (based on external incentives). Typically, the effect of behaviorist drivers does not last for long after the incentive is taken away (or no longer seen as an incentive) – such as increased pay that starts to be seen as normal7 – unless it is internalised and becomes intrinsically meaningful and owned.
Social cognitive theory
Bandura’s social cognitive theory provides a useful lens on this phenomenon. According to this theory, there are reciprocal interactions between human behaviour, cognitive factors and social environment8. This means that humans are not simply reactive to environmental stimuli; they have cognitive abilities and behaviours (agency) that influence their actions9. Human cognitive abilities include anticipating consequences of one’s actions, thinking, planning and self-motivating. Agency refers to acts done intentionally9. These cognitive abilities and agency enable individuals to intentionally direct their actions toward the accomplishment of tasks and goals that give meaning and satisfaction to their lives9.
Self-efficacy is vital for personal agency9. It is an individual’s belief that he or she is able to successfully perform a novel or difficult task10. Highly self-efficacious people tend to see problems and adversities as challenges to overcome, not as threats. Hence, self-efficacy has a role in developing motivation and goals to achieve despite challenges, and to persevere during the process.
Resilience and its dimensions
The concept of self-efficacy is closely linked to resilience10. Resilience is the ability of a person to rebound, spring back and maintain wellbeing, which enables that person thrive during ongoing stress and adversity11-14. This can be illustrated as a rubber ball that bounces back to its original form15. The difference between the concept of resilience and self-efficacy lies on the presence of a stressor. One cannot be perceived to be resilient without any stressor, while self-efficacy may be present without any stressor10.
Retaining doctors in rural areas is not easy because they face more uncertainties and adversities than their urban colleagues15. Doctors who are not well prepared and equipped to work in rural areas may feel lost, lonely and distressed with a risk of becoming burnt out. Job dissatisfaction is the main factor that drives doctors to leave rural contexts16. The most common sources of work-related distress reported by doctors are poor work–life balance, fear of making mistakes17 and lack of control over workload18,19.
Personal resilience has been recognised as a key component of wellbeing20,21 and it is associated with better quality of life13. Improving wellbeing contributes to lowering stress and improving retention of rural doctors22. Therefore, resilience has been suggested to be a core competency in rural general practitioner (GP) registrar training23 and studies suggest that medical schools should focus their curriculum on providing opportunities for the development of students’ resilience13.
Resilience consists of several dimensions: determination, endurance, adaptability, recuperability, comfort zone and life calling24. Determination is a person’s willpower and decision to persevere and/or to succeed. Endurance is a person’s strength to withstand difficult situations without giving up. Adaptability is a person’s capacity to be flexible and resourceful and to cope with adverse environments and adjust oneself to changing conditions11,25. Determination, endurance and adaptability are associated with career satisfaction in nurses25.
Recuperability is a person’s ability to recover from various types of harm, setbacks or difficulties11,25. Doctors in rural areas are always dealing with uncertainties and various adversities and difficulties along their rural career, so it is logical to assume that this ability may also have a role in their staying in rural areas. Comfort zone is the ability of an individual to accept and feel enough/satisfied with their current condition. Doctors who are satisfied with their job or the compensation received tend to stay longer in rural26 areas.
Life calling is an individual’s sense of personal fulfillment and meaning from recognising or simply believing that what they do has a socially useful purpose27, which cannot be substituted by economic means24. A reported reason that doctors kept working in rural areas was because they had a desire (or calling) to serve underserved populations26,28.
Thus, it is plausible that promoting personal resilience has the potential to support the mere survival and even thriving of doctors at work despite adversities and challenges. Logically then, resilience may play an important role in the retention of doctors in rural areas23,29.
Exploring resilience and rural retention
Based on this argument, the relationship between personal resilience and retention of doctors in the rural context is likely to be important. However, to the best of the authors’ knowledge, this relationship has not been studied in the Indonesian context. Studying this relationship in different cultural contexts is important: what may be found in one context may be different in others. By studying these phenomena in various context, a deeper understanding can be achieved. This study seeks to examine the association between rural doctors’ personal resilience and duration of rural practice.
Methods
Context
This study was located in Nusa Tenggara Timur (NTT) Province, a rural province in Indonesia. NTT is an archipelago province with 1192 islands, of which only 44 are inhabited. The population of 5.28 million is a culturally diverse but predominantly Christian (90%)30. The NTT Province predominantly consists of medically underserved areas (18 of 22 districts)31. NTT has the second-lowest doctor-to-population ratio in Indonesia (14/100 000), which is much less than the recommended WHO ratio of 100/100 00032.
Participants
Participants in this study were doctors working in NTT Province, excluding those working in the capital, Kupang City. For the selection of the participants, a total sampling approach was used33. The inclusion criteria were as follows: GP or intern; working in the health sector (eg primary health centre/puskesmas, hospital, district health office, non-governmental organisation); working in NTT Province (except in Kupang City) during the study period; and available and willing to participate. In Indonesia medical education is typically an undergraduate entry program, with medical graduates conducting a year-long internship before being fully licensed. After this they can opt to apply for a hospital, clinic or community health service position, either in a city or rural areas. They can also choose to apply for a specialist or primary care training pathway. Thus in this study ‘GP’ refers to a medical doctor, before they undertake any further study, working in a rural area34.
Participants who could not participate due to illness (physical or mental) or detention were excluded. Participants who were actively involved in any political campaigns and with possible vested interests at the time of the study period were also excluded. They were identified through the contact person for the Indonesian Doctor Association branch in each district.
Instrument
The adapted Indonesian version of Taormina’s Adult Personal Resilience Questionnaire was used24. The internal consistency (Cronbach’s alpha) of the adapted questionnaire was 0.81–0.96 for each dimension24.
This adapted questionnaire consisted of six dimensions, with five items in each dimension. Examples of the items are ‘Once I set a goal, I am determined to achieve it’ (determination), ‘I can withstand a difficult situation’ (endurance), ‘I can change to fit into many kinds of circumstances’ (adaptability), ‘I am able to bounce back from any kind of adversity’ (recuperability), ‘This is the right place for me’ (comfort zone) and ‘Even in difficult situations, God has been there to guide me’ (life calling)24.
The questionnaire was scored using a five-point Likert scale ranging from 1 (’strongly disagree’) to 5 (‘strongly agree’). The range of total scores for each dimension (five items) was 5–25 with a mean range of 1–5. For all subscales, a higher mean score indicated a higher resilience level for that particular dimension11. Because there is no previous reference for a doctor’s performance on this scale, for the purpose of this study and its statistical convenience the ranges of the mean score (1–5) were distributed evenly into three classifications: low (<2.3), moderate (2.3–3.7), and high (>3.7).
The scores analysed and presented in this article are the subscales/dimension scores, not the composite score. Combining all dimensions into one composite score, although statistically logical, tended to obscure the results. The participants’ resilience profiles of which dimensions were strong or weak would be unknown. For example, having scores of one in three dimensions and five in the other three dimensions would result in an average score of 3.
Design
A cross-sectional comparative design35 was used to measure and compare the resilience profiles between groups of participants with different durations of rural practice. An online survey was selected as the data collection strategy because of its large-scale population access36.
Survey process
The data collection procedure involved several steps (Fig1). Data about potential participants (eg names and mobile phone numbers) were identified from the database of the Provincial Indonesian Doctor Association in NTT, district health offices, and by snowballing37. All of the registered GPs in NTT, except for those in Kupang City, were contacted by WhatsApp or SMS and asked to participate in the study. Links to further explanations about the study, informed consen, and the online version of the questionnaire were also sent by WhatsApp or SMS. The WhatsApp social media application was chosen as an alternative to email because many people in NTT Province use this social media application and open it frequently. Reminders were sent to non-responders 1 week and 2 weeks after the previous reminder36.
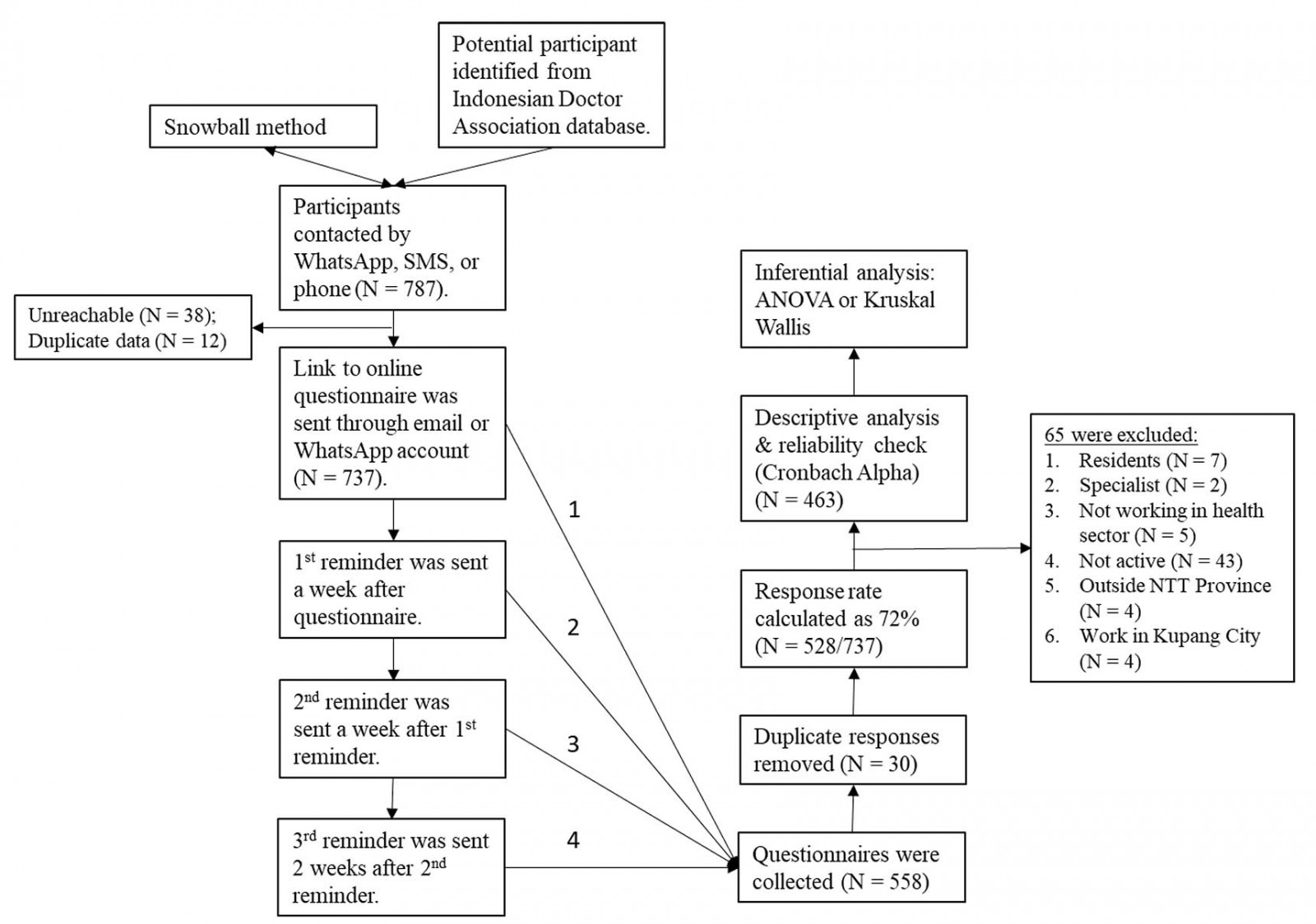 Figure 1: Flowchart of data collection and analysis procedures.
Figure 1: Flowchart of data collection and analysis procedures.
Data analysis
Data analysis procedures involved several steps (Fig1). First, descriptive analysis (means, percentage, range of scores and 95% confidence interval (CI)) were calculated. Second, internal consistency coefficients of each dimension were determined using Cronbach’s alpha36. Third, inferential analyses were conducted using one-way analysis of variance (ANOVA) on each dimension. The Statistical Package for the Social Sciences v20 (IBM; http://www.ibm.com/SPSS/Statistics) was used.
The independent variables were duration of rural practice (in the province and in the current/last district). The participants were divided into four groups: intern, young GPs (<5 years of experience), mid-career GPs (5–10 years of experience) and senior GPs (>10 years of experience). The dependent variables were resilience dimensions, and six dimensions of resilience were tested: determination, endurance, adaptability, recuperability, comfort zone and life calling)24. Because those six dimensions behave largely as independent constructs, ANOVAs were done separately for each dimension in relation to the duration of rural practice. Each dimension’s effect size was determined using the eta squared (%u019E2) measure38.
Ethics approval
This study was approved as part of a bigger study, which aims to design a clinical education model as an intervention to enhance resilience development, previously approved by the Ethical Committee, Faculty of Medicine, University of Gadjah Mada, Yogyakarta, Indonesia (KE/FK/0877/EC/2018) and University of Nusa Cendana, Kupang, NTT, Indonesia (64/UN15.16/KEPK/2018).
Results
Demographic
A total of 528 out of 737 (72%) registered GPs who were contacted responded to the questionnaire. Of these, 65 participants were excluded (Fig2), leaving 463 participants for the quantitative analysis (Table 1). Most of the participants were Christian, females and not in a relationship (Table 1). The schooling background of the participants showed a movement from the rural to the city as they grew up (Table 2).
Table 1: Demographics of study participants (n=463)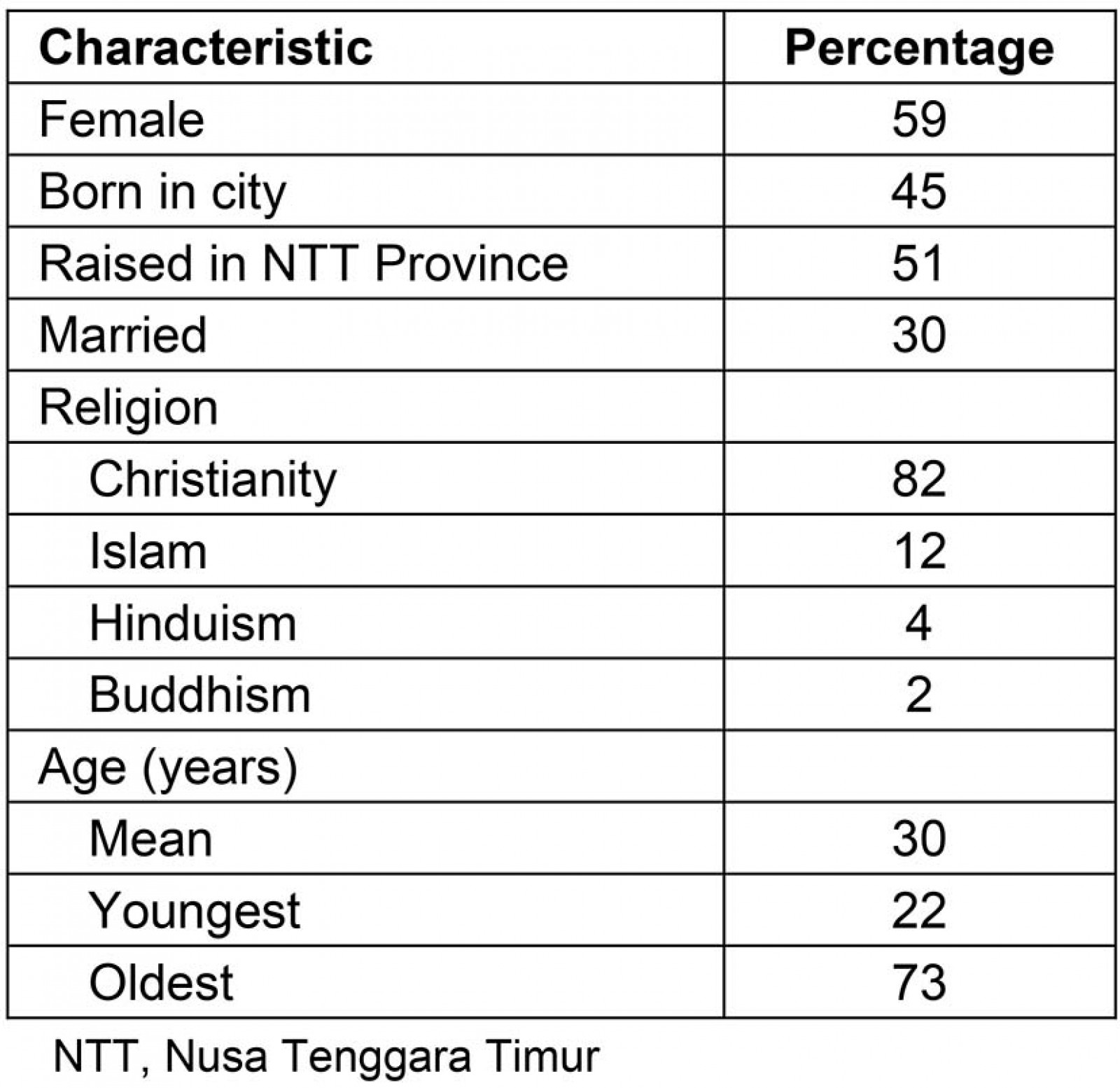
Table 2: Level of school education by participant childhood location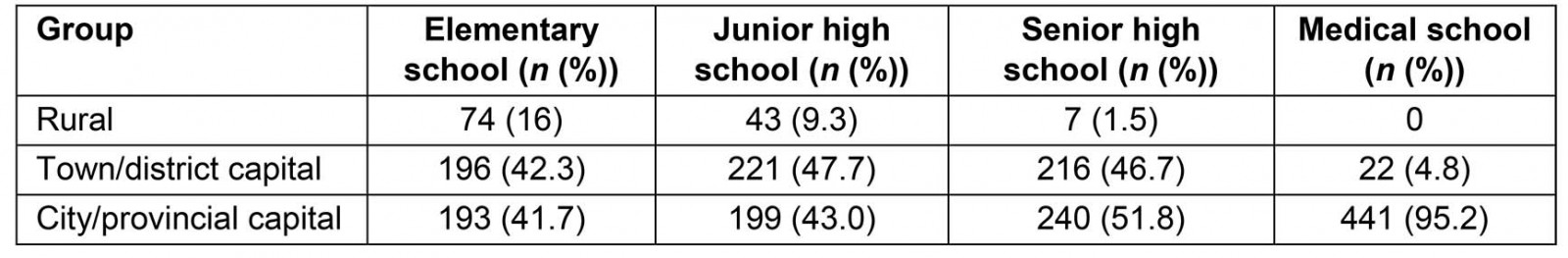
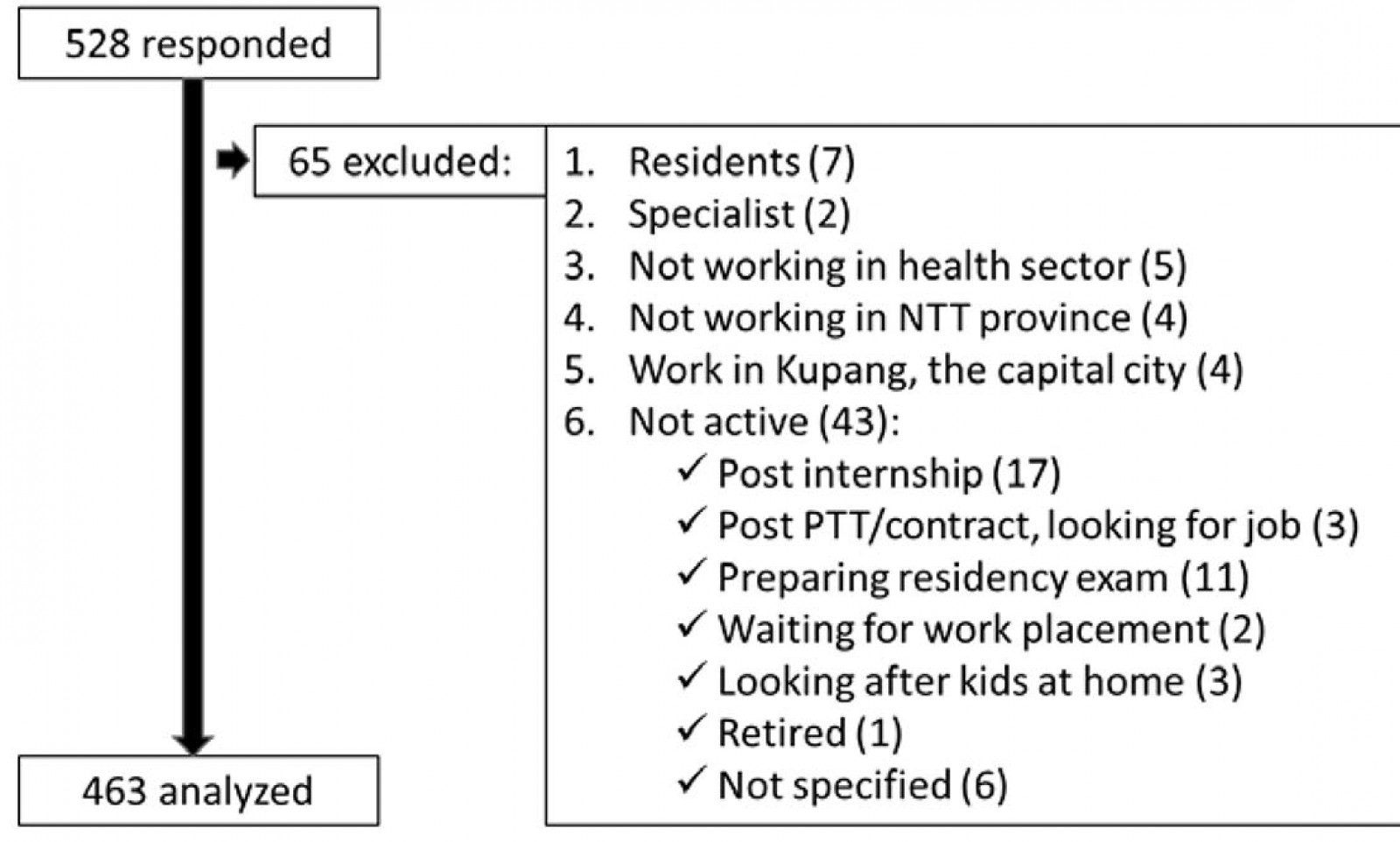 Figure 2: Study exclusion criteria and numbers.
Figure 2: Study exclusion criteria and numbers.
Resilience dimensions
Analysis of each of the dimensions of resilience showed that the internal consistency of the scales was high (Cronbach’s alpha score range 0.79–0.96). Determination and life calling had the lowest and the highest scores, of 0.79 and 0.96 respectively. Given the high internal consistency of each dimension – some even higher than the internal consistency of the total scores – it was decided not to represent the final score by a single composite score but by six different scores, with each score representing its particular dimension.
In general, the analysis of the scores of the total group of participants showed that the mean scores for all dimensions except comfort zone were high (>3.7 on five-point Likert scale). Comfort zone was moderate (between 2.3 and 3.7) with a mean score of 3.30 (95%CI 3.23–3.36). The highest mean score of 4.59 (95%CI 4.54–4.65) was for the life calling dimension (Fig3).
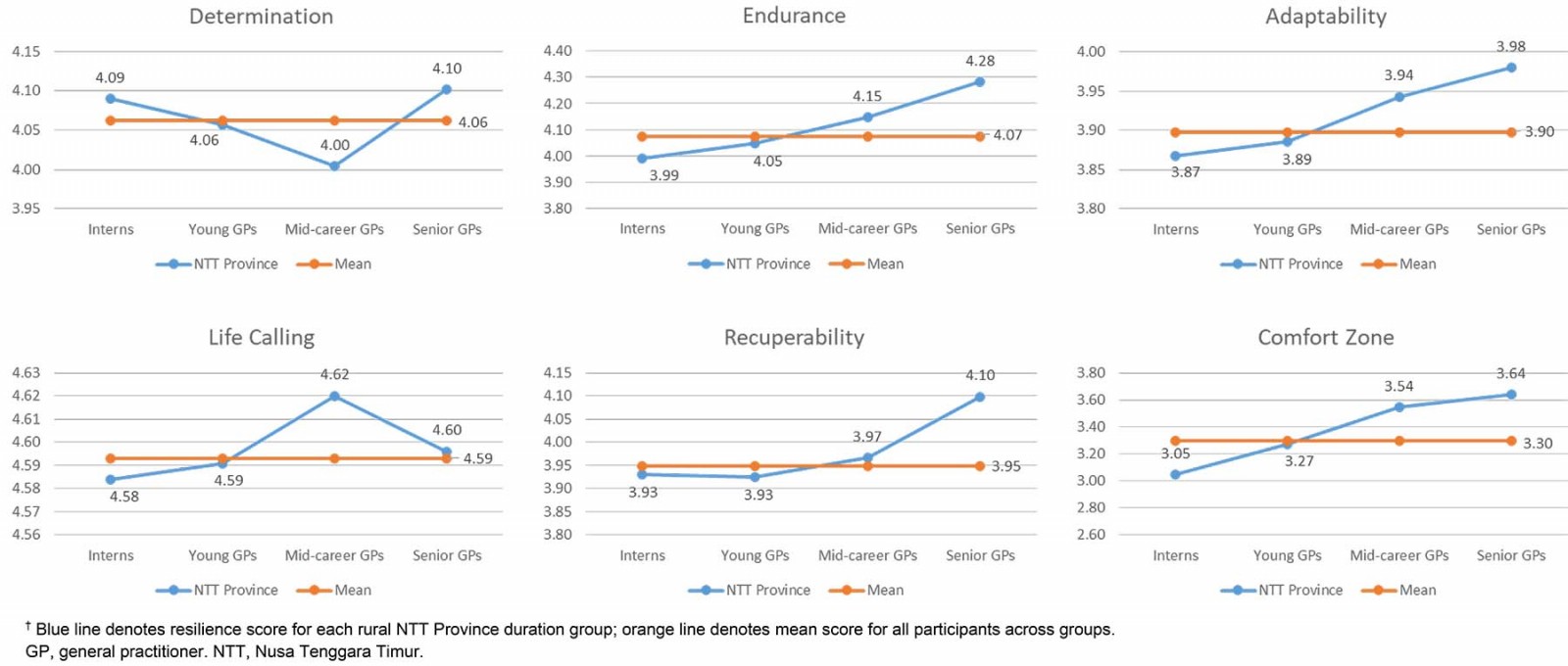 Figure 3: Dimensions of resilience by rural duration.†
Figure 3: Dimensions of resilience by rural duration.†
Resilience and retention
There are three important findings. First, groups with longer rural experience showed higher levels of resilience. However, these differences were significant in only two dimensions: endurance and comfort zone. Second, these significant differences were found only between groups with >10 years difference in rural practice and, specific for comfort zone, when there was a change in the status from intern to GP. Third, life calling held the highest score among the six dimensions. However, it showed no association with the rural duration since the differences between groups were very small.
The differences between groups in the endurance and comfort zone dimensions were statistically significant, with p-values of 0.011 and 0.0001, respectively (Table 3). Tukey’s posthoc analysis was conducted to examine which groups within these two dimensions were different. The significant p-values (p<0.05) are summarised in Table 4.
Table 5 shows that the practice duration for interns, young GPs and senior GPs were 0.5 years, 2 years and 16.5 years, respectively. Therefore, endurance and comfort zone were significantly higher in groups with at least 10 years of differences in rural practice (senior GPs compared to interns and young GP groups). However, only 21% (98 out of 463) of participants had >5 years of rural experience, and even a smaller number of participants (11%) remained after 10 years (Table 5). In contrast to endurance, the comfort zone score for interns was significantly different compared to all groups.
Life calling had the highest total participants’ mean score of 4.59 (95%CI 4.54–4.65) and the intern group had the lowest score, of 4.58 (95%CI 4.47–4.70). To further explore the unique trend in life calling, in which the senior GP score was lower than the mid-career GP group, the groups’ classification was restructured based on working duration in most recent district only (excluding practice duration in previous different districts). The graph of results is similar to the other dimensions in which the groups with longer rural experience showed higher scores. This is illustrated in Figure 4 as a change from the blue line to the orange line. However, both before and after the change, the differences between groups were not statistically significant: the difference between the lowest (4.584) and the highest (4.651) scores was only 0.071 (Fig4).
Closer examination of the different trends of the life calling dimension for different rural groups’ classification found that 14 participants in the senior GP group had moved across districts. This is illustrated in more detail by the red arrows in Figure 5. These two histograms show that the participants who moved across districts had lower scores of life calling when compared to those who stayed longer in the same district. The red arrows denote the locations of these 14 participants’ scores within the group, which exist on the left histogram (provincial duration) and not on the right histogram (‘current/most recent district only’ duration). Those scores are considered to be within the lower range of the group scores.
Table 3: Within- and between-group ANOVA results for resilience dimensions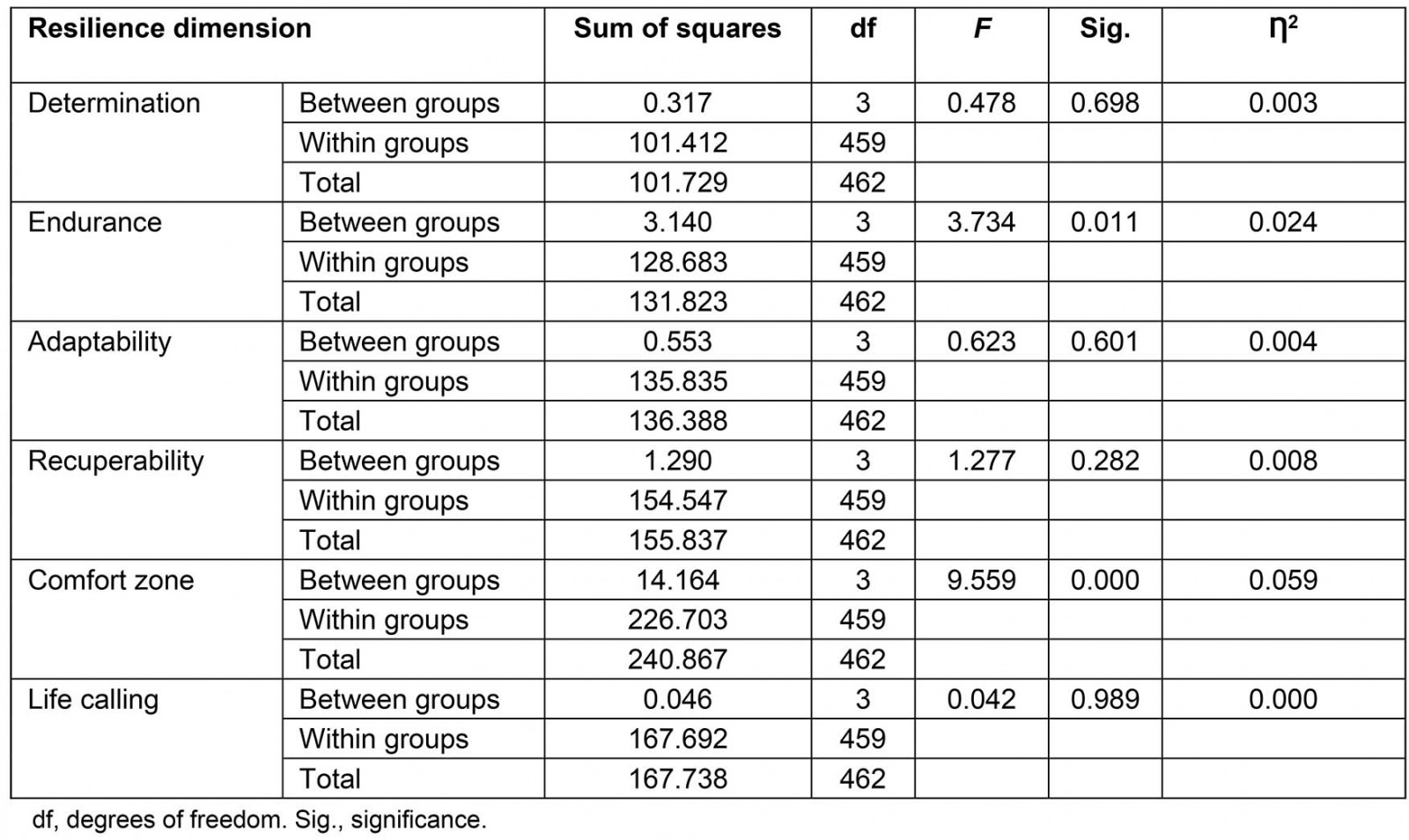
Table 4: Statistically significant groups on Tukey’s posthoc analysis (p<0.05)†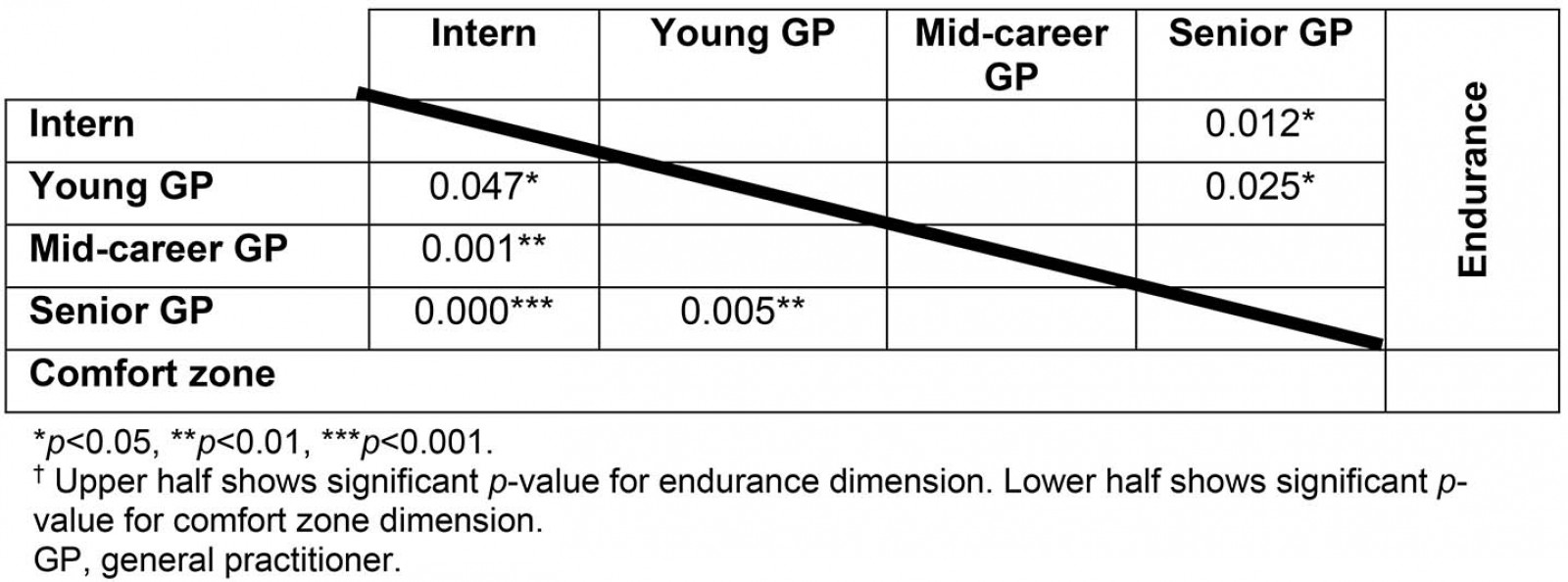
Table 5: Rural experience by group and participant childhood location (NTT Province or not)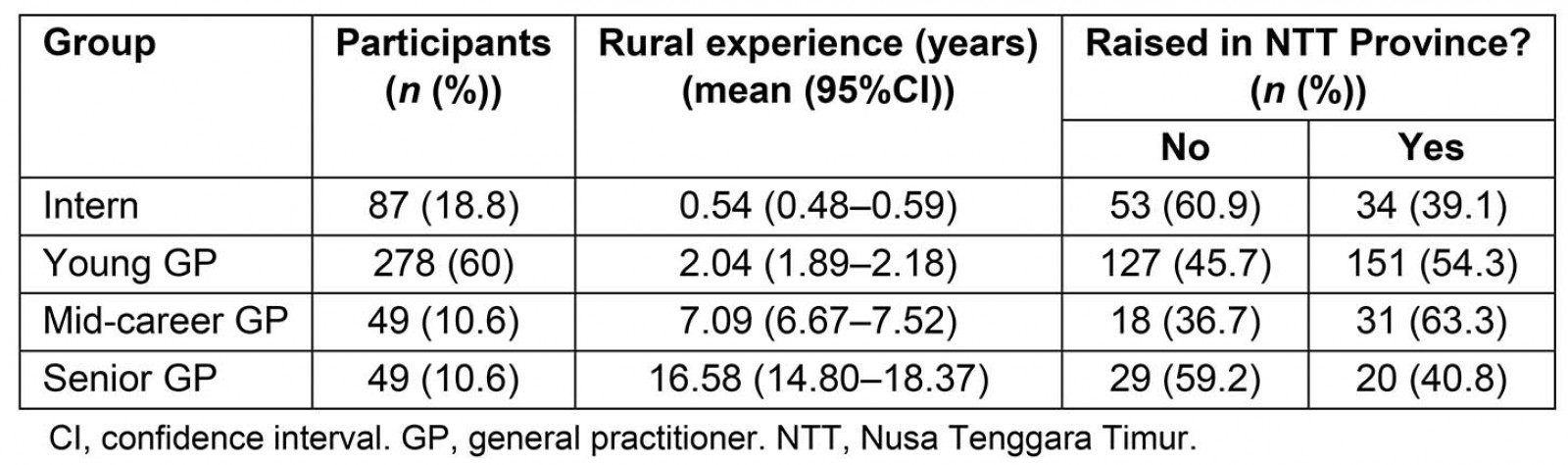
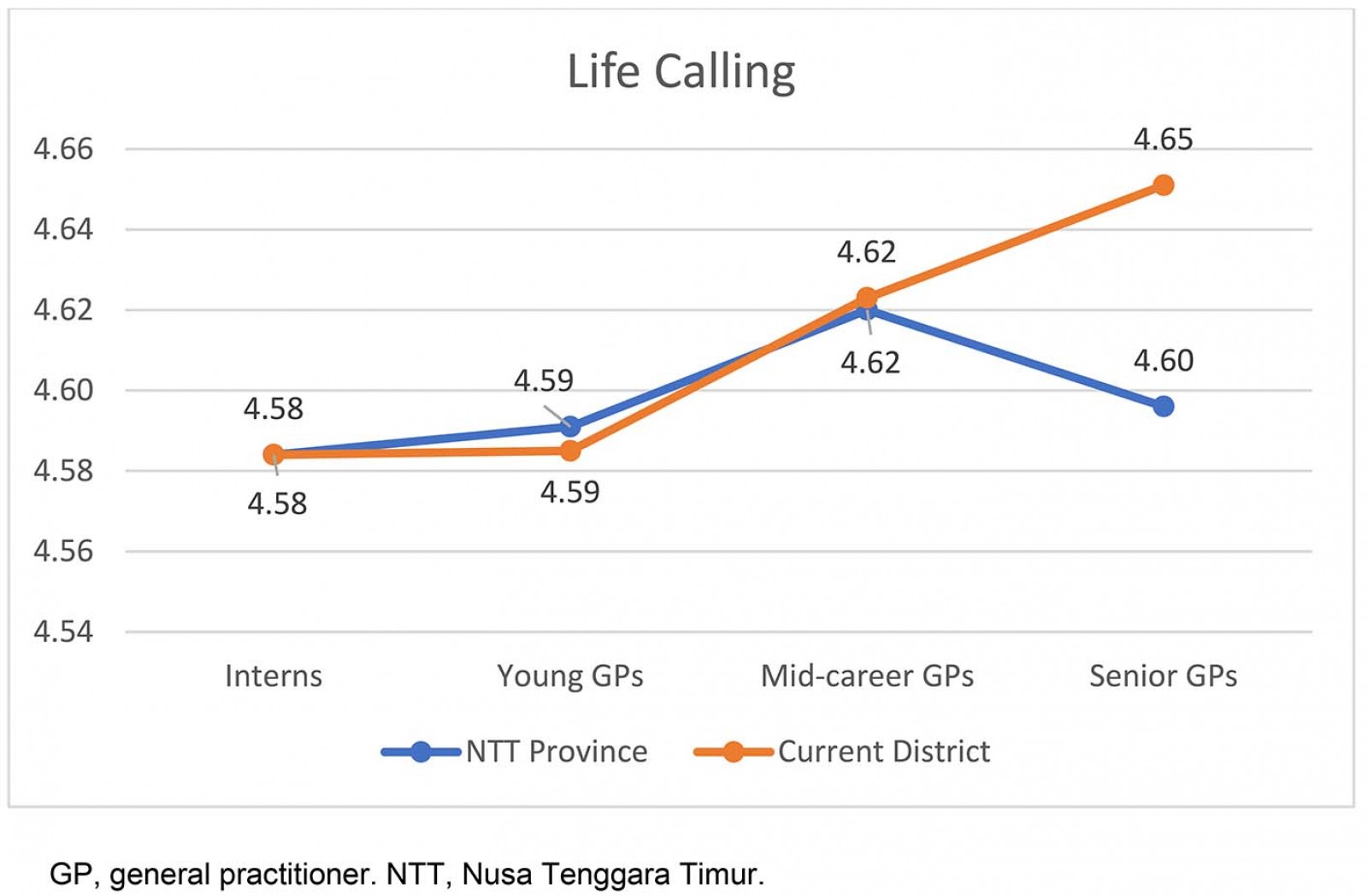 Figure 4: Life calling analysis by participant group and most recent practice location.
Figure 4: Life calling analysis by participant group and most recent practice location.
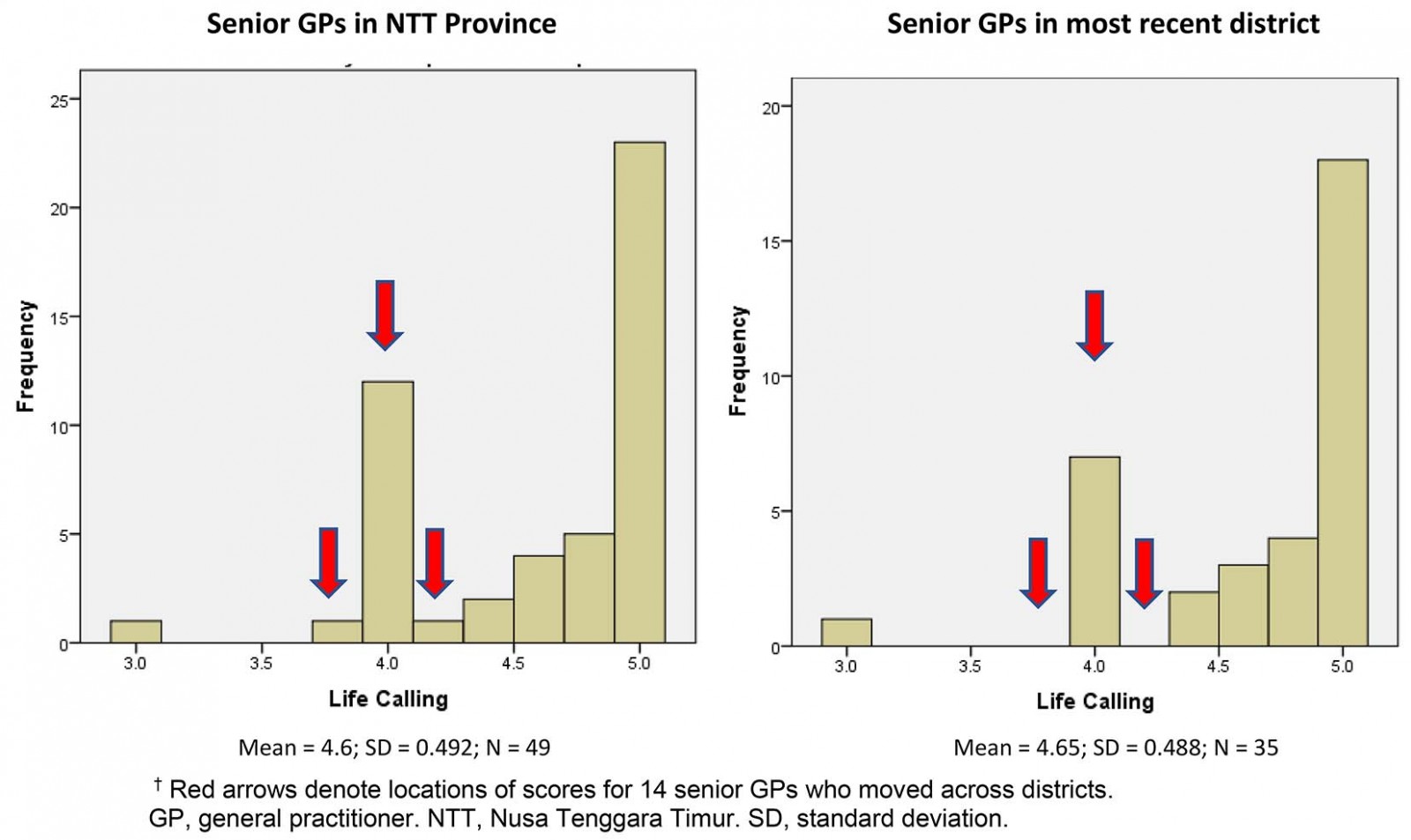 Figure 5: Histograms of life calling dimension for senior GPs in NTT Province and by most recent district.†
Figure 5: Histograms of life calling dimension for senior GPs in NTT Province and by most recent district.†
Discussion
This study examined the association between GPs’ resilience levels and the duration of rural practice. Two dimensions, endurance and comfort zone, showed significant associations between groups with >10 years of differences in rural practice. Their effect sizes are small for endurance and moderate for comfort zone dimensions. The guidelines for small and moderate are %u019E2 of 0.01 and 0.059 respectively38. This means that the practice duration differences between groups account for 2.4% and 5.9% of the change in the endurance and comfort zone scores, respectively.
Many factors not measured in this study have a role in rural doctors’ retention, such as extrinsic and intrinsic incentives39, intrinsic values, positive rural training experiences, rural infrastructure, professional development opportunities, work–life balance40, and having a rural background41,42 or a spouse with rural background42. Thus, the findings should be carefully interpreted by taking into account the possibility of the presence and interference of these factors.
In addition, because of the cross-sectional nature of the present study, it is not possible to conclude whether the high resilience levels caused the participants to stay longer or vice-versa. For example, natural attrition may have eventually led to attrition from those doctors with lower resilience, leaving the more resilient ones. Highly resilient people have the ability to survive, learn and find meaning from adversity43. Accordingly, resilience attributes are likely to support the participants’ capacity to thrive and stay longer in rural settings.
Challenging experiences and exposures to risks or adverse events theoretically support the development of resilience15,43,44. Experiences, especially in relation to adverse events, are likely to be essential to developing resilience. Each dimension of resilience develops for a specific context (eg task, culture, geographic location)45,46 through person–environment interactional processes46. However, an individual’s internal characteristics (eg cognitive, skills, affective, spiritual) play roles in resilience in different contexts46. From this perspective, it could be argued that the participants’ experiences over time assisted in nurturing resilience attributes for specific contexts.
Endurance enables one to withstand difficult situations without giving up. It is similar to the term ‘perseverance’ in other studies13,47,48. The positive association found between endurance and retention aligns with a previous study in which doctors were adapted to and kept working despite difficulties they faced during the Palestine conflict49. Limitations of rural practice, which include underdeveloped infrastructure, lack of recreational activities, inadequate accommodation facilities, high workload and feelings of isolation, may become negative predictors for retention40,50. Thus, the ability to endure these limitations is likely to support rural doctors’ retention.
The significant differences in comfort zone scores between the interns and all other groups suggest that a status change from interns to GPs might be important. It seems that these participants were adapting to the rural context and those who stayed longer were the ones reaching their comfort zone. A previous study suggests that more time spent in the rural community offers opportunities to develop an emotional connection to local people and rural living, which then facilitates the uptake of rural lifestyle51. In addition, by staying long enough, the doctors also have opportunities to develop a better private practice and businesses, such as a farm, a pharmacy or a hotel28. The ensuing better earnings may increase comfort zone level. This aligns with another study suggesting that increased remuneration and other monetary incentives are associated with higher retention of rural doctors40. Most importantly, satisfaction with earnings may prevent a doctor from leaving28. Job satisfaction also related to the retention of rural health practitioners52.
Although statistically significant, the actual score of the comfort zone dimension is only moderate and the lowest among other dimensions. The authors interpret this as reflecting the rural specific context with its limitations40. On the other hand, the high level of resilience on the other dimensions aligns with a previous study in which the doctors’ resilience levels are higher than those of the general population53.
Although not all dimensions show a significant association, most of the graphs show similar trends; groups with longer duration of rural experience show higher resilience levels, except determination. A possible explanation for this in the mid-career group is that they might have experienced multiple adversities and failures in achieving their goals during their 5–10 years of rural practice. For example, it was observed that most medical graduates sought specialist training but many were not accepted, even after several attempts. It is entirely plausible that some of them tried to make a change in rural areas, but the outcome was disappointing to them. Self-determination theory offers an explanation for this, suggesting that the fulfilment of needs for competence, autonomy and relatedness is needed for individuals to experience a sense of wellbeing54. In this case, experiencing failures is most likely to have undermined their sense of competence and caused them to set a lower goal/target to achieve10, leading to a lower determination score.
In contrast to comfort zone, the life calling dimension is not significantly associated with rural duration, but it holds the highest scores among other dimensions, even for the intern group. This might be due to a ceiling effect55 of all groups’ scores. The authors’ interpretation of this is that people who choose a rural career are likely to have a sense of personal meaning for this work. This aligns with some previous studies. Kim and Equivel identified spirituality and religion as resilience factors56. Resilience was developed through faith in the power of a person’s god44, which provides a purpose to life and assists one in finding meaning beyond the adversity experienced56,57, through the practice of sharing within a faith-based community, prayer and meditation57. Spirituality also helps in developing a sense of meaning in one’s life and shaping behaviour58. Another study found that doctors who work in underserved areas were more likely to have a sense of responsibility or moral obligation59. Work attitude (commitment, self-esteem and intrinsic satisfaction) among doctors is positively correlated with spirituality and religion58. Job dissatisfaction, on the other hand, has been the main reason for doctors leaving rural areas16. Another study found that helping people and following ‘God’s call’ provided intrinsic motivation and had an important role in retention28. Reliance on faith was one reason why doctors kept on working in the middle of the Palestine war49. However, according to the World Values Survey, there are differences in how societies see religion as important. In some societies, including Indonesia, the values and daily behaviour of its people are strongly influenced by religion60. So, life calling is likely to have a role in retention of doctors in rural areas in certain societies. But this interpretation is limited by the absence of the data on the resilience level of doctors who leave rural practice. Its generalisability is also limited by the cultural differences between societies.
The present study showed a different trend in the life calling graph when counting the participants’ experience only in the last district, excluding any previous experiences. A possible explanation for this is that those participants who moved across districts may have not yet found their life calling in the previous location and may have been looking out for a better place, which explanation would align with self-determination theory61,62, in which the highest and preferable motivation is intrinsic motivation. However, extrinsic motivation is important too, and these participants may have moved to another district, giving better extrinsic rewards. This aligns with behaviourism theory7 in which one conducts an action with an expectation of getting a reward. A combination of both extrinsic and intrinsic motivations is needed for an effective rural retention program39,63.
These findings are important for rural workforce interventions because they provide a basis for understanding resilience in regard to its impact on rural doctors’ retention. They suggest that the endurance and comfort zone dimensions are better developed in doctors who have stayed in rural areas for more than 10 years. This aligns with a previous study suggesting the need to increase resilience to help doctors deal with the challenges they face, avoid burnout, reduce staff turnover and recruitment costs64. Thus, it is also logical to assume that any attempt to increase endurance and comfort zone dimensions may have an impact on retaining doctors longer in rural areas. Further study is needed to prove this assumption.
Implications of findings
To the best of the authors’ knowledge, currently most developing countries’ rural workforce interventions implement behaviourist approaches by giving rewards or punishment (eg compulsory rural service, rural bound scholarship and high financial incentives)31,65-67. These interventions have been proven to increase recruitment but not retention6.
In the present study, the proportion of the participants studying in the city was increasing from elementary to medical school. This is logical given the limited availability of senior high school in the rural locations where none of the medical schools were located68. However, the proportions of participants who grew up in the province of the present study (NTT) was similar to those of participants who came to the province later after graduation from medical school, showing that the rural recruitment programs32,65-67 are quite successful in attracting non-local doctors. However, recruitment and retention are two different issues. Although recruitment of doctors was effective, in this study only 21% of the doctors stayed for more than 5 years. This means that incentive-based interventions are successful only in recruiting doctors, not in retaining them67, which makes additional strategies for longer term benefits, such as developing resilience during medical training, worth considering.
Some previous studies found that resilience was associated with certain personality characteristics20 and coping abilities43 of doctors and that these can be developed during clinical training to support resilience and wellbeing13,20,23,43. The UK General Medical Council also acknowledged the need for resilience training for medical students and doctors69 and has included resilience as one of the capabilities to be acquired by GP trainees70. Nevertheless, further studies are needed to explore how resilience develops among doctors in rural areas and how students can be better assisted to develop their resilience capacities, especially endurance and comfort zone dimensions.
It is logical to suggest that evaluating life calling in student selection may assist in choosing students with good potential for future rural practice. Examining humanistic factors during student selection has been identified as important for increasing the number of graduates59 with interest in a rural career. However, this suggestion may not be applicable to every culture and further studies are needed to explore the best way to do this and its impact.
Limitations
Because this is a cross-sectional study, it is not possible to draw inferences of causality and the individual longitudinal development of resilience. It is not possible to conclude whether high resilience caused GPs to stay longer in rural work or if the duration of their rural work was what contributes to the development of resilience. In either case, programs to support resilience development could be useful.
The strong Christian background (82%) of participants may limit the generalisability of the findings. For example, life calling was very prominent in this study’s participants, which may not be the case in other contexts. However, the demographics of the participants align with the proportions of religion in the general population in NTT Province, where the majority were Catholic (52%) and Christian (38%), with a small percentage of Muslims (9.3%) and Hindus (0.2%)30.
Conclusion
Although this is a preliminary study, it shows differences in the resilience profile of GPs with >10 years differences in rural practice. It also provides a basis for understanding the possibility that resilience is partly associated with the retention of rural doctors.
Acknowledgements
The authors thank all rural doctors who participated in the survey, Karol Octrisdey for his statistical assistance and Marselino Abdi Keraf for his help in understanding the survey result on resilience.
References
You might also be interested in:
2011 - Post-crisis: earthquake, tsunami, radiation leak and rural health crisis in Japan
2010 - Analysis of enhanced pharmacy services in rural community pharmacies in Western Australia





