Introduction
Sustainability of evidence-based programs is a significant issue, a persistent challenge in all settings and an understudied area1-3. Sustainability is defined as ‘the ability to maintain programming and its benefits over time’ (p. 2)4. Sustainable programs (at least 1 year after implementation) are more likely to produce positive lasting outcomes4. In a recent review conducted on the sustainability of evidence-based interventions in health care, the authors suggested that funding, organizational factors, support and workforce characteristics (eg turnover) influenced sustainability. They concluded that there was a need for more research on sustainability to help us to better understand what factors and processes influence the sustainability of interventions to inform proactive planning of sustainability for these interventions1. As well, they recommended the use of a conceptual or theoretical framework to guide sustainability research1. None of the studies in the review focussed on sustainability of rural health programs. Rural communities have additional challenges to implementation and sustainability of programs as there is often a shortage of health professionals and health related resources5. As such it is important to explore the factors that influence the sustainability of rural programs.
In a review of sustainability frameworks and theories, Walugembe et al2 noted the Normalization Process Theory6 and the Dynamic Sustainability Framework7 included the importance of embedding and integration of the innovation within a social context. The ability to sustain a program over time means that there was successful program implementation followed by the uptake and embedding of the program in a setting5. However, the Normalization Process Theory and the Dynamic Sustainability Framework have reported limited utility2 and have not considered the importance of facilitation. One framework that is applicable for examining sustainability is the i-PARIHS (integrated Promoting Action on Research Implementation in Health Services). The definition of successful implementation in the i-PARIHS framework8,9 incorporates factors and processes that affect the program implementation and sustainability. The core constructs of the i-PARIHS framework consist of facilitation, innovation, recipients and context, with facilitation as the active element in integrating the other three constructs. As facilitation is the active ingredient in the i-PARIHS framework, it plays an important role in the sustainability of evidence-based interventions. Evidence-based interventions are defined broadly in the framework to be inclusive of emergent and inductive ways of generating evidence8. Following a scoping review of the original PARIHS framework it was revised to include a definition of successful implementation and a more comprehensive description of the innovation, recipients and context8. Although the framework has not been previously used to examine factors influencing sustainability, the newly revised i-PARIHS may be a useful guide to examine sustainability of an evidence-based intervention.
Nav-CARE (Navigation: Connecting, Accessing, Resourcing and Engaging) is an evidence-based program in which volunteers are trained in navigation to facilitate access to resources and provide social support to older persons with serious illness living in rural communities. It has been evaluated in several communities and found to be feasible and acceptable by older persons, volunteer navigators and community agencies and to improve the quality of life of older persons living with serious illness10,11. In a rural community in western Canada, Nav-CARE was implemented as part of a research project over 1 year (October 2016–2017). At the conclusion of the research project (post-implementation) Nav-CARE was integrated into the services provided by the local hospice society, continuing with training and mentoring of additional volunteers and visiting older persons, helping them to connect to resources and engage in their community for approximately 2 years (at the time of writing). The implementation of Nav-CARE began with nine volunteers visiting 23 older persons over a 1-year time period. Two years post-implementation, the program grew to 45 volunteers visiting more than 80 older rural persons. However, it is unclear what influences the sustainability of Nav-CARE after its implementation, particularly when it has had varying degrees of successful sustainability in other communities. Six out of eight communities reported Nav-CARE was integrated into their hospice society 1 year after implementation11. Using the i-PARIHS framework, the purpose of this study was to explore the key factors that facilitated sustainability of the Nav-CARE program in this particular rural hospice society. This article reports the findings of this study.
Methods
This study used Yin’s qualitative single case study design12 to address the study purpose as it is useful when trying to understand how or why a certain event occurred. This approach was appropriate to address the study purpose as, using this design, a researcher is able to study real-life, complex events to gain an in-depth understanding of the phenomenon being studied12. In this case the phenomenon under study is an actual complex event of sustainability of the Nav-CARE program in a rural community. Qualitative data from interviews and documents were collected before, during, immediately post-implementation and 2 years after implementation of Nav-CARE in a rural community. The data were organized using the i-PARIHS framework and then analyzed using Yin’s qualitative approach.
Data collection
Case study designs are flexible and utilize several sources of data13. Data were collected by trained research assistants through individual interviews with community stakeholders, the study volunteer coordinator and the Nav-CARE volunteer navigators. As well, it included meeting notes of volunteer debriefing sessions, meetings with stakeholders planning for sustainability of Nav-CARE and a written summary of reflections by the hospice volunteer coordinator (Table 1). Data were collected at different times: (a) pre-implementation (3 months), (b) during implementation (1-year time period), (c) immediately after implementation and (d) 6 months to 6 years after implementation. Data were integrated in the analysis stage.
Table 1: Study data sources and collection times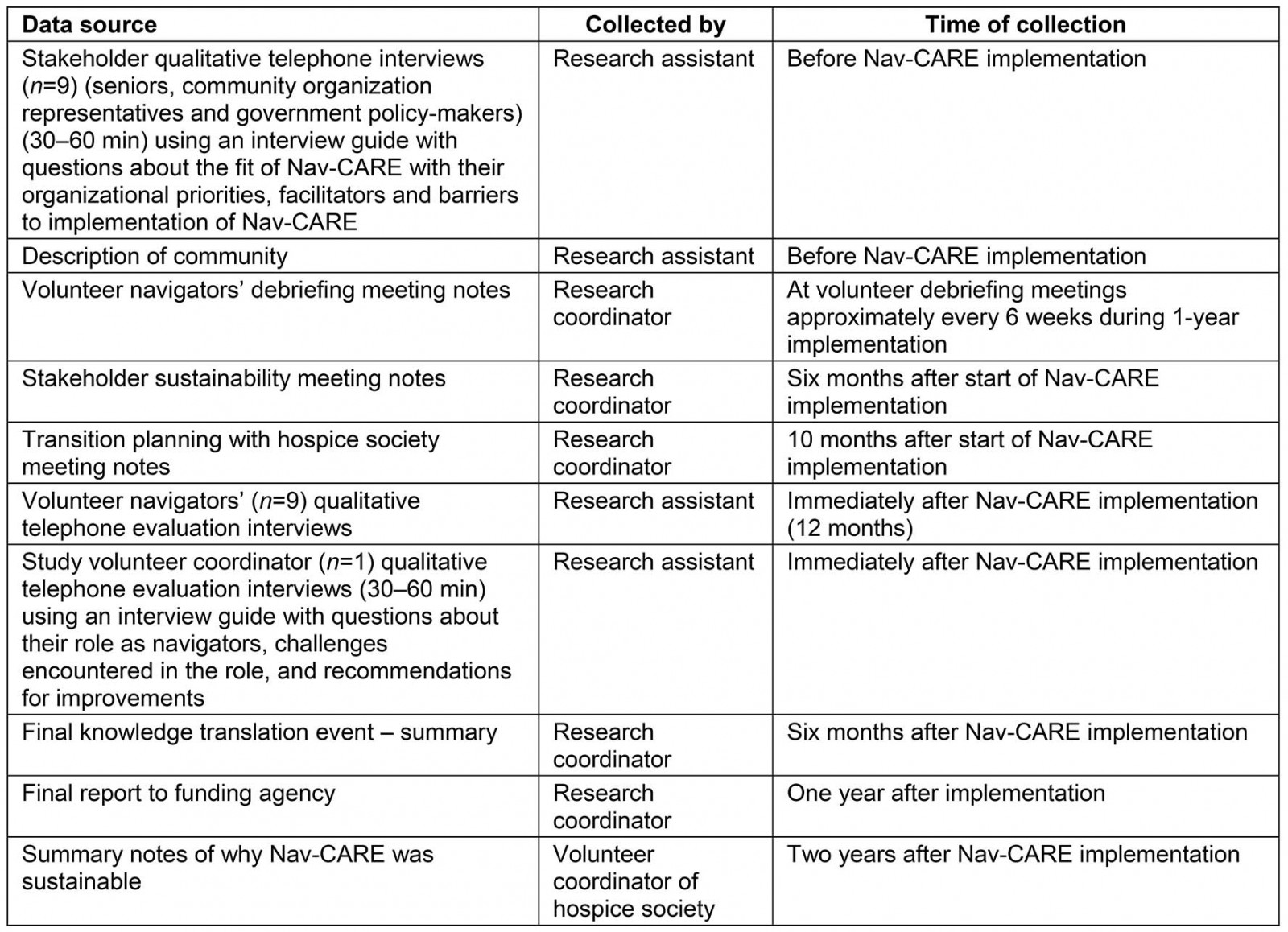
Data analysis
Yin suggested organizing case study data according to a descriptive framework12. Using this strategy, all data were organized into the i-PARIHS framework constructs (facilitation, innovation, recipients and context) using the definitions and characteristics outlined in Table 2. After the initial organization of the data was complete, data were analyzed using pattern matching. Pattern matching is an attempt to link two patterns, where one is theoretical (i-PARIHS framework) and the other is data collected. Within each of the i-PARIHS constructs, data patterns were inductively identified and organized into categories and then themes. The more that the patterns matched, the more support the findings provided for the use of the i-PARIHS framework to describe factors associated with sustainability12.
Following pattern matching, data were analyzed using explanation building. Explanation building is an iterative inductive and deductive process of making initial and tentative explanatory propositions and comparing the data from the case against the proposition to gradually build an explanation about how and why events occur12. During this process, the researcher must be open to and examine other potential rival explanations12. Plausible rival explanations were posed and data were compared to determine which explanation was supported by the data from the case. For example, Yin suggested that an intervention itself (in this case Nav-CARE) would usually be the initial explanation about how or why sustainability occurred12. A rival hypothesis based on the i-PARIHS framework would suggest that facilitation was the reason sustainability occurred. Both of these hypothesis were considered as well as to other hypotheses derived inductively from the data. Data within the i-PARIHS framework constructs were examined to determine which hypothesis had the most support. Yin suggested that it is the weight of evidence that determines which hypothesis best fits data12.
Trustworthiness of the data was achieved through processes of ensuring credibility, transferability and auditability14. Credibility was achieved through discussions of the findings with the research team, transferability through rich description of the data and auditability through record-keeping of analysis decisions in an audit trail.
Table 2: iPARIHS framework definitions and characteristics8,15 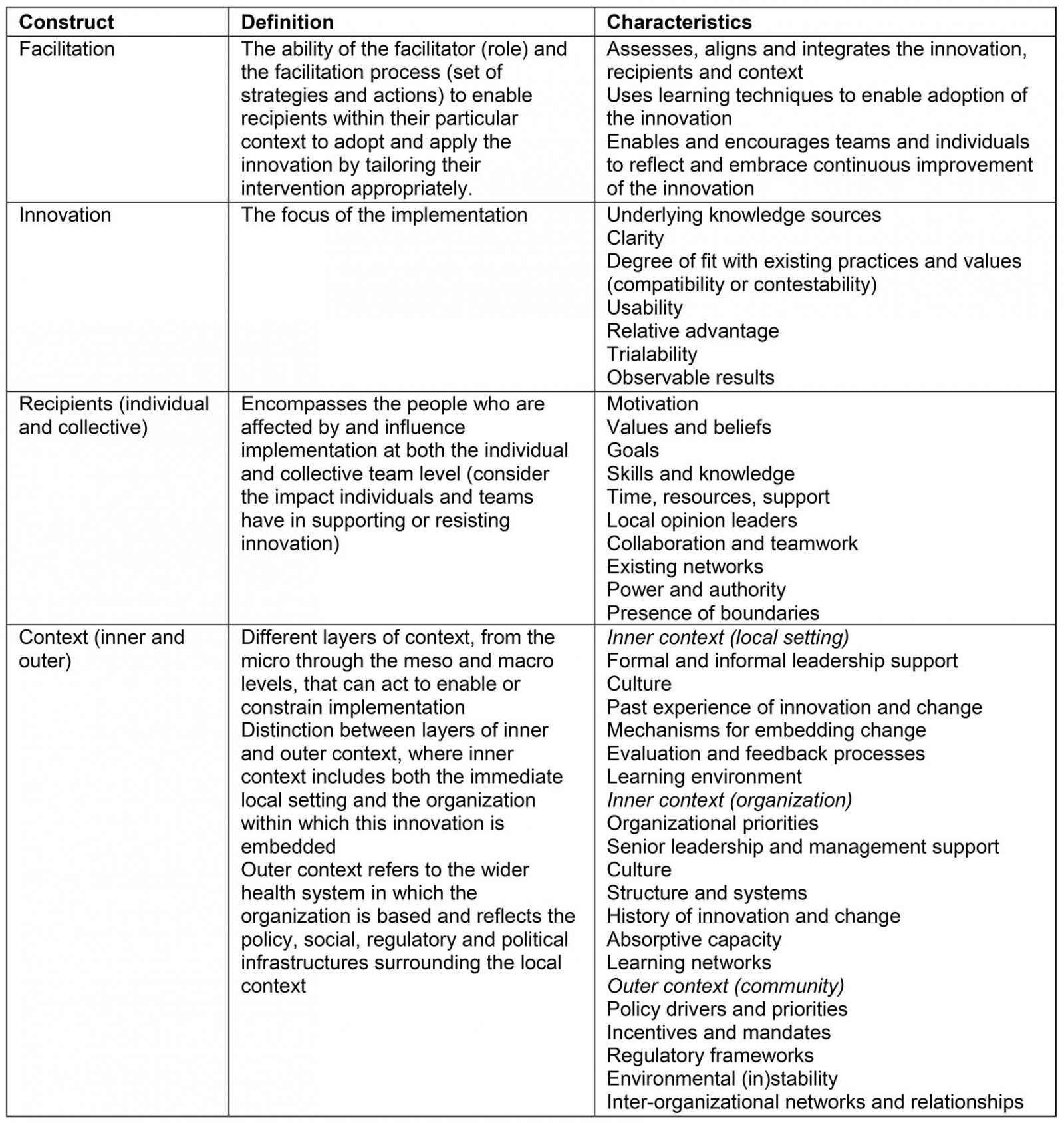
Ethics approval
The study was approved by the University of Alberta Health Research Ethics Board (Pro00059300).
Results
The community where Nav-CARE is sustained is a small rural city of approximately 18 000 people (29% are over the age of 65 years)16. It is located in a central prairie province in Canada. The implementation of Nav-CARE in this community was supported by the administrator of the community acute care hospital and the hospital community advisory board, which included representatives of community organizations such as the local hospice society. The 1-year implementation occurred within the community outside of any specific organization with the assistance of the hospital advisory board. However, during the process of the 1-year implementation the local hospice society determined that they would like to integrate Nav-CARE into their existing programs. This hospice society is community based and does not have a designated inpatient unit. It has a well-established hospice volunteer program in which volunteers are trained and visit persons with serious chronic illness in their homes. The integration of Nav-CARE into the hospice society began at the end of the 1-year Nav-CARE implementation.
The purpose of this posthoc analysis was to explore factors facilitating sustainability using the i-PARIHS framework. Data were present in all of the concepts of the framework (facilitation, innovation, recipients and context). The first explanatory hypothesis, as suggested by Yin12, focused on the i-PARIHS concept of the intervention. In other words, the Nav-CARE program (innovation) was the reason for sustainability. The i-PARIHS criteria for a successful innovation is that it is evidence-based, trialable (observable results), usable and has proven relative advantage9. Nav-CARE is an evidence-based intervention, built on a theoretical foundation17. It has been found to be feasible, acceptable and adaptable to different communities and showed promise in positive outcomes for older persons and navigators10,11. In the community understudy, Nav-CARE was evaluated immediately post-implementation and was also found to be feasible, acceptable and showed promise for positive outcomes. As such Nav-CARE met the criteria for a successful innovation.
Although the innovation itself, Nav-CARE, is important, a rival explanatory hypothesis was considered based on the preponderance of data in the i-PARIHS concepts of facilitation and inner context. The data (as described below) suggested facilitation and the organizations’ inner context were key to the sustainability of the Nav-CARE program in this specific rural community.
Facilitation
The facilitation concept from the i-PARIHS framework includes the role of the facilitator and the facilitation process itself8. The framework highlights facilitation (facilitator and process) as the key for the success of implementation and sustainability as it enables recipients within their context to apply the innovation.
Role of facilitator: During the implementation of Nav-CARE, a formal facilitator role was assigned to a study volunteer coordinator, who was hired through research funding. She was a nurse who had connections with the community and was responsible for recruiting volunteer navigators, assisting in their training and providing ongoing support. The study volunteer coordinator was also responsible for recruiting older persons with serious illness and matching them with volunteer navigators. Following the 1-year implementation and evaluation of Nav-CARE in this community, the hospice society determined it would integrate it into their existing program. At this point, the study volunteer coordinator was replaced with the hospice society volunteer coordinator who led the sustainability process.
Data from this study suggest that in this rural community the facilitator was considered the leader of the Nav-CARE program and it was important that this person was a member of the community. As one of the volunteer navigators suggested during their final evaluation interview:
I think it’s really, really important to have the right person leading the program, and to have the person from this community, because the needs differ from community to community. It was so good to have [name of person]; she lives here, she works here, she knows these people. (volunteer navigator 02)
This facilitator was considered to be key to the success of Nav-CARE, as one stakeholder said:
… but I see a bigger resource issue is having that [volunteer coordinator], having the supports and training in place and that constant mentorship of the volunteers. Cause they would need to be a very skilled individual. (stakeholder 04)
This quote also illustrated that the facilitator needed to be very skilled in training and mentoring volunteers.
The summary notes from the hospice society volunteer coordinator also suggested that she received ongoing mentorship from the co-founders of Nav-CARE during the post-implementation sustainability phase. She wrote:
We are truly grateful … for the ongoing support provided by [study co-principal investigators] We are also grateful for the sharing among the other Nav-CARE sites.
Ongoing support was provided through a network of Nav-CARE volunteer coordinators from different sites that were established by the research team.
Facilitation process: The facilitation processes for sustainability in the implementation phase included the initial training of the volunteers, their ongoing mentorship and support, and the sustainability planning and final knowledge translation events.
The nine volunteer navigators recruited for the study, the study volunteer coordinator and the hospice society volunteer coordinator attended a 2.5 day workshop (14–16 September 2016) delivered by the co-founders of Nav-CARE and an experienced nurse navigator. The training involved modules were developed and evaluated during a previous Nav-CARE pilot study18. At the training, workshop participants received a volunteer navigation learning manual to use during the training and implementation.
The workshop for volunteer navigators addressed the following evidence-based navigation competencies:
- understanding the navigator role
- screening for quality-of-life concerns
- advocating for clients
- facilitating community connections
- coordinating access to services and resources
- promoting active engagement.
The positive evaluation of the training has been reported elsewhere19. One volunteer navigator participant quote summarizes the evaluation:
Pretty well everything was of value: written word, video, different speakers, skits and role play kept everything interesting. (volunteer navigator 08)
All of the training resources were made available to the hospice society for ongoing training and support post-implementation. Seven of the nine trained Nav-CARE volunteers continued as Nav-CARE volunteers post-implementation.
Ongoing support and mentorship: The training, ongoing mentorship and support of volunteer navigators was identified as an essential element of Nav-CARE at the Sustainability Planning Event, which was held 6 months post-implementation. As part of the Nav-CARE program implementation, the study volunteer coordinator provided ongoing support for the volunteer navigators on an individual basis as well as at monthly group debriefing meetings. As one volunteer navigator participant said during the evaluation interview:
Just that I think that it most definitely was beneficial to have our monthly meetings, just to be able to share in confidence maybe some of your frustrations and rewards. And to have that coordinator where you could call and say, ‘I’m not too sure how to handle this’, or ‘Here’s the situation I ran into, and I didn’t feel very comfortable with it.’ So it was good to know that that person was there to say, ‘I didn’t feel good about this one.’ Or even the fact that, ‘Who do I go to here? I’m not too sure.’ So it was nice to always have that go-to person. (volunteer navigator 04)
The participants agreed that facilitation processes of ongoing training and mentorship of volunteers were important for sustainability of the Nav-CARE program. These processes of facilitation continued post-implementation in this rural community as documented in the summary notes provided by the hospice society volunteer coordinator
Sustainability planning community events: The summary of the first community sustainability planning event held 6 months from the beginning (16 March 2017) of Nav-CARE implementation described the purpose and outcome of the event. The purpose of the event was to begin discussions about the sustainability of Nav-CARE in the community. Eighteen people attended, representing different community organizations as well the study volunteer coordinator and volunteer navigators. At this event, following presentation of preliminary data and round table discussions, the essential elements of Nav-CARE were decided: older persons with serious illnesses requiring navigation services, and trained and supported volunteer navigators. Possible strategies for sustainability of Nav-CARE were discussed.
Following the sustainability meeting, the principal investigator of the Nav-CARE study was contacted by the chair of the hospice society board about their interest in integrating Nav-CARE into their programming. This was followed by a transition meeting with the hospice society director and hospice volunteer coordinator. As reflected in the summary notes of this meeting, a transition plan from the study to integration of Nav-CARE into the hospice society programs was discussed. This plan was then presented to the hospice society board for approval. This transition plan included a communication plan for the volunteers, older persons currently on the program, and the community suggested steps to implement Nav-CARE into their organization and how Nav-CARE could be adapted to the hospice society. Suggestions for adaptation included revision of the admission criteria to include those in residential facilities as well as the community and how to integrate the current hospice society intake and evaluation processes with the Nav-CARE processes.
The final knowledge translation event (6 months post-implementation) was identified by the hospice volunteer coordinator as important for sustainability of the Nav-CARE program in her sustainability notes. This knowledge translation event was held on 4 April 2018 with 53 attendees including hospice volunteers, interested community members, healthcare providers, home support workers and decision-makers. Attendees received an infographic created to highlight the main findings of the implementation study and viewed a 12-minute film describing the Nav-CARE program and work of volunteer navigators. As such the event highlighted the successful implementation of Nav-CARE adding to its feasibility for sustainability. Thus the role of the facilitator and the planned facilitation processes (training, ongoing support and sustainability planning events) were key factors in the sustainability of the Nav-CARE program.
Inner context (organizational context) of the hospice society
Another key factor for sustainability of the program was the inner context of the hospice society reflecting the organizations capacity to support Nav-CARE over time. The data that supports this finding were organized into three subthemes: fit of Nav-CARE with the organization’s priorities, the sustainability capacity of the organization, and the organizational structures and mechanisms to integrate Nav-CARE into the current programs. For example, in the stakeholder interviews it was clear that Nav-CARE fit with the organization’s priorities. As one stakeholder said:
Nav-CARE would also fit in conjunction with – we would provide a referral to Nav-CARE through our program. So the people that we have as clients, per se, would have the services provided by our program, plus volunteer services through Nav-CARE, so it would add to what people receive. (stakeholder 03)
As such, the added value of Nav-CARE to the current organization was also important to sustainability.
The hospice society had absorptive capacity as defined by the i-PARIHS framework13 as the organization’s ability to identify, assimilate and apply external knowledge. In this case absorptive capacity of the hospice society reflected its ability to integrate Nav-CARE into the current programming so that no additional resources would be needed. As one stakeholder commented:
If we do it right, the resources can be shared and we may find that existing resources can actually fulfill this. (S08)
The hospice society also had the structures and mechanisms for change that were needed for sustainability. For example, a stakeholder in an interview described the importance of a good operational system to support the navigators and facilitate linkages between navigators and older persons:
I think it’s the operational system, a good operational system to support the navigators and to help continue the support and facilitate these linkages [between older persons and volunteers]. (S04)
As the hospice volunteer coordinator said in her summary notes:
Our care volunteers within our Hospice Society are trained to be Nav-CARE, palliative, end-of-life and grief and bereavement companions. The volunteers move comfortably between these roles and provide a loving service to those in need.
The mechanisms were in place for Nav-CARE to be integrated into the hospice society programs. As well, the hospice society was well established in the community. The hospice volunteer coordinator wrote in her summary:
Some Hospice Societies struggle with having the community know what they do. Ours has experienced volunteers and good connections.
The support of the community for the hospice society was also evident with the numbers of stakeholders attending the final knowledge translation event.
Discussion
Nav-CARE was successfully implemented in a rural community in western Canada. Key factors that contributed to the sustainability of a rural community intervention, designed to improve the quality of life of older persons with serious illness, were identified as the organizational context (inner context) and facilitation (facilitator and facilitation processes).
Organizational context
The hospice society in this case study sustained Nav-CARE for more than 2 years since its implementation, in part because of its inner context (organizational context). Nav-CARE was congruent with the hospice society priorities. As well, the hospice society had absorptive capacity, and organizational structures and mechanisms in place to integrate Nav-CARE into existing programming. Other studies support the present study’s findings that the context or organizational setting is a key factor related to sustainability of evidence-based practice3,20-22. However, the present case study more clearly delineated the hospice society characteristics that contributed to the sustainability of Nav-CARE such as absorptive capacity, sustainability capacity and being well established in the community.
The hospice society appeared to have absorptive capacity to integrate the Nav-CARE program into existing programs without additional resources. This is important, particularly within rural settings where there is often a lack of resources5. Very little is written about absorptive capacity in the i-PARIHS framework. This could be because its focus has been on implementation of research into practice19 and not specifically sustainability. The term ‘absorptive capacity’ comes from business theory introduced by Cohen and Levinthal23. In their definition, absorptive capacity is the ability of an organization to assimilate and apply external knowledge. However, it was also defined as a limit of an organization to absorb this knowledge. Whether it is considered an ability or a limit to apply evidence-based knowledge, the present case study suggested that it is an important consideration for sustainability of evidence-based community programs.
The presence of organizational structures and processes that were in place for volunteer coordination, training and support were also important factors contributing to Nav-CARE sustainability within the hospice society. Schell et al have called this ‘sustainability capacity’ of an organization4; as such there are structures and processes that allow an organization to maximize resources to sustain an innovation. They also identified the core domains of sustainability capacity: environmental support, funding stability, organizational capacity, program evaluation, program adaptation, communication, sustainability planning and partnerships. Program evaluation and sustainability planning occurred during the implementation phase of Nav-CARE and as such possibly contributed to sustainability capacity of the hospice society.
The hospice society was well established and supported in their rural community. The characteristics of organizations that have the greatest chance of sustaining an intervention are those that are well established in their communities and have partnerships with external agencies20,21. Using the i-PARIHS framework, interagency connections are not considered an organizational context (inner context), but an outer context such as regulatory frameworks and policy drivers and priorities of other organizations. The capacity and mechanisms to form partnerships with other agencies and communities would seem to be an important characteristic of an organization’s inner context as well. As such, a limitation of using the i-PARIHS framework may be that partnerships with other organizations, which are very important to rural communities, are not considered an important part of the organizational inner context. The definition of sustainability capacity also includes partnerships. The present findings suggested that absorptive capacity is only one aspect of sustainability capacity. As such, sustainability capacity of an organization would be important for other organizations to examine if they wish to implement Nav-CARE. Future research should be conducted to more clearly understand how to assess and enhance sustainability capacity of organizations before implementation of evidence-based programs.
Facilitation
Facilitation was also a key factor in sustainability of Nav-CARE. This included the role of the facilitator as well as the facilitation process. The study volunteer coordinator was identified in the Nav-CARE program as having the role of the facilitator. This included having the skills to train and mentor volunteer navigators in a flexible way (individual and group mentoring). This is similar to findings from other studies that have suggested that the credibility, flexibility and competency (knowledge and skills) are important characteristics of facilitators24,25. Having the right individuals in the role as facilitator with the right level of skills, knowledge, support and mentoring is an important factor in successful implementation of evidence-based programs26. Since the role of the facilitator is important to sustainability, consideration should be given in the Nav-CARE program to providing additional training to the volunteer coordinator. It appears that ongoing mentorship of the facilitator, in this case the hospice volunteer coordinator, also contributed to sustainability. Mechanisms for the training and mentoring of Nav-CARE volunteer coordinators are important considerations to achieve sustainability.
The facilitation processes included training of the volunteer navigators, their ongoing support and mentorship, as well as sustainability planning and the final knowledge translation events. Shelton et al1 in their review of sustainability research suggested that little is known about the nature and influences of processes (training, planning, partnerships, evaluation and engagement) on sustainability. From the authors’ data in this case study, it appears that programs should include training, planning for sustainability in which stakeholders are engaged, as well as sharing of the program evaluation data at community events. The engagement of stakeholders throughout the facilitation process has been described as important for implementation26, and the present study’s data suggested that it is also important for sustainability. Harvey and Kitson suggested that facilitation makes it easier to implement evidence into practice8, but the present study’s findings suggest that facilitation was also a key factor in sustainability of the program following implementation.
Limitations
There are several limitations to this study. It is a single case study design. A stronger design is a multiple case study design where different communities would be compared to each other9. This would require the same components of Nav-CARE to be implemented in more than one community in the research study. Future research should plan for multiple case studies of sustainability of Nav-CARE. Also, this was a posthoc analysis of the Nav-CARE implementation data, with the addition of the summary provided by the hospice society volunteer coordinator post-implementation. In the interviews, specific questions were not asked regarding sustainability of the Nav-CARE program. Without current evaluation data of the hospice society Nav-CARE program outcomes, it is difficult to evaluate whether the sustainable Nav-CARE program continues to result in the same positive outcomes as the implementation did. Follow-up evaluation data would strengthen the design of this study. However, a benefit of the case study design is the utilization of several data sources, including meeting summaries, which provided a broader insight into the sustainability of Nav-CARE.
Conclusion
This single case study identified facilitation and inner (organizational) context as key factors contributing to the sustainability of a volunteer navigation program to support older persons living with serious illness in a rural community. Utilizing the i-PARIHS framework was helpful in identifying these factors. The knowledge and skills of the facilitator were important, and consideration should be given to incorporating additional training for the formal facilitator in the Nav-CARE program. The sustainability capacity of the hospice society contributed to the sustainability of Nav-CARE, as organizational structures and mechanisms were in place for Nav-CARE to be integrated in the current programming. Future research should explore how facilitation and sustainability capacity can be enhanced as part of the implementation of evidence-based programs in rural communities. This study provides a foundation for future research and adds to the discussion of the issue of sustainability of evidence-based interventions in rural community settings.
Acknowledgements
This project received financial support from the Covenant Health Network of Excellence in Seniors’ Health and Wellness. Thank you also to the research assistants who contributed to this work (Kaitlyn Muse, Marina Riccio, Vanessa Ritchie, Kathya Jovel-Ruiz), other members of the research team (Konrad Fassbender, Jayna Holroyd-Leduc, Deirdre Jackman, Terri Woytkiw) and the study participants.




