Introduction
The US state of Kansas had 36 268 live births in 2018. Access to maternity care services has become an issue for many citizens of frontier and rural counties in Kansas due to decreased numbers of Kansas hospitals offering those services in the past several years. It has been well-established that the farther mothers travel from their homes to give birth the greater the rate of pregnancy complications, premature birth, and the higher cost of care1-4. The one-third of the population of Kansas that lives in non-metropolitan areas are responsible for 9853 (27.3%) births annually5. However, the current distribution of obstetrics providers and their plans for continuation of obstetrics services was not previously described in Kansas. Although anecdotal, there are reports suggesting that access to obstetrics and maternity services for the rural population may be at risk.
In Kansas, the quantification of maternity care services is not a straightforward process. The location of providers of maternity care – certified nurse midwives (CNMs), family physicians, and obstetrician/gynecologists (OB/GYNs) – is not just a simple task of locating such providers in the Kansas Board of Healing Arts database. CNMs are not yet listed in this database, and the Kansas Board of Nursing only lists home addresses of CNMs and not practice location. The location of family medicine and OB/GYNs is listed in the board database, but their scope of practice is not. This makes it unclear if they deliver babies or not. Birth certificate data does have the delivering physician, but due to regulations in Kansas this information cannot be released on a wide scale. The Kansas Hospital Association publishes an annual survey of its membership and includes the number of births at a particular hospital, but not the name or level of training of a particular provider.
To further study the issues of access, the Kansas Rural Obstetrical Access Task Force (KS-ROAT) was formed in September 2015. The members of the KS-ROAT designed an annual survey of physicians in non-urban counties to directly answer two primary questions: ‘Who delivers babies in Kansas?’ and ‘What are the future plans for providing maternity care services?’
Methods
Much of the data on health care is reported at the county level in Kansas. Kansas has 105 counties. They are roughly similar in size at about 1620 km2 (625 square miles). Only 10 counties in Kansas do not have a hospital. There are 85 critical access hospitals in the state. Counties are divided into population density peer groups for the purposes of describing their relative rurality (Fig1). Urban counties are defined as those with greater than 150 persons per square mile (psm), Semi-Urban counties are those with 40–149.9 psm, Densely-Settled Rural counties have 20–39.9 psm, Rural counties have 6–19.9 psm, and Frontier counties have fewer than 6 psm6. Many of the population and healthcare facilities in Kansas are in the eastern one-third of the state. Given the predominance of comparative data in the state using this scheme, the authors decided to use county level data and sort results into cohorts using the population density peer groups.
Physician survey recipients were identified through licensure with the Kansas Board of Healing Arts’ public records. An attempt was made to survey all providers of obstetrics care in non-urban counties in Kansas. The board’s public licensure list was first filtered based on Kansas residence and active practice status. Then the list was segregated into specialty and limited to family medicine, general practice, and obstetrics/gynecology. Next, physicians were sorted based on the population density peer groups of the county listed of their primary practice location. The researchers then requested confirmation from the Kansas Department of Health and Environment Office of Vital Statistics records for physicians of the relevant specialties in rural counties in which they provided maternity care. The department stated that providing a list of physicians signing birth certificates would represent an ‘identifying use’ of the data that is not allowed under their regulations. Instead, the list of hospitals reporting births in their institution and their active medical staff was used. Researchers were able to cross-reference summary statistics for the number of births in rural counties and the numbers delivered by these physicians. It was then possible to create a list of maternity care providers (MCPs) from this cross-reference. No other MCPs were identified who were not already on the filtered list after comparison, validating completeness of the list of possible obstetrics providers. Medical students from the University of Kansas enrolled in a rural clinical elective were given contact lists from these physicians in their respective regions to administer a 72-question mixed methods survey about various aspects of their maternity practice and their future intention to provide maternity care services.
The mixed methods survey was designed following recommendation and revisions by faculty at the University of Kansas School of Medicine and members of the KS-ROAT. This questionnaire was developed after a pilot survey in 2014 and modified based on multiple source feedback. Questionnaire content encompassed physician demographics, training, obstetric care factors, knowledge of midwifery practice in their area, and future intentions to continue providing maternity care. Surveys were collected and accumulated over three consecutive summers in 2016, 2017, and 2018. Physicians who had not previously participated in the survey were identified for contact in subsequent years. Survey responses were directly entered into a secure RedCap database. The principal investigator then de-identified surveys for distribution to the study team for analysis.
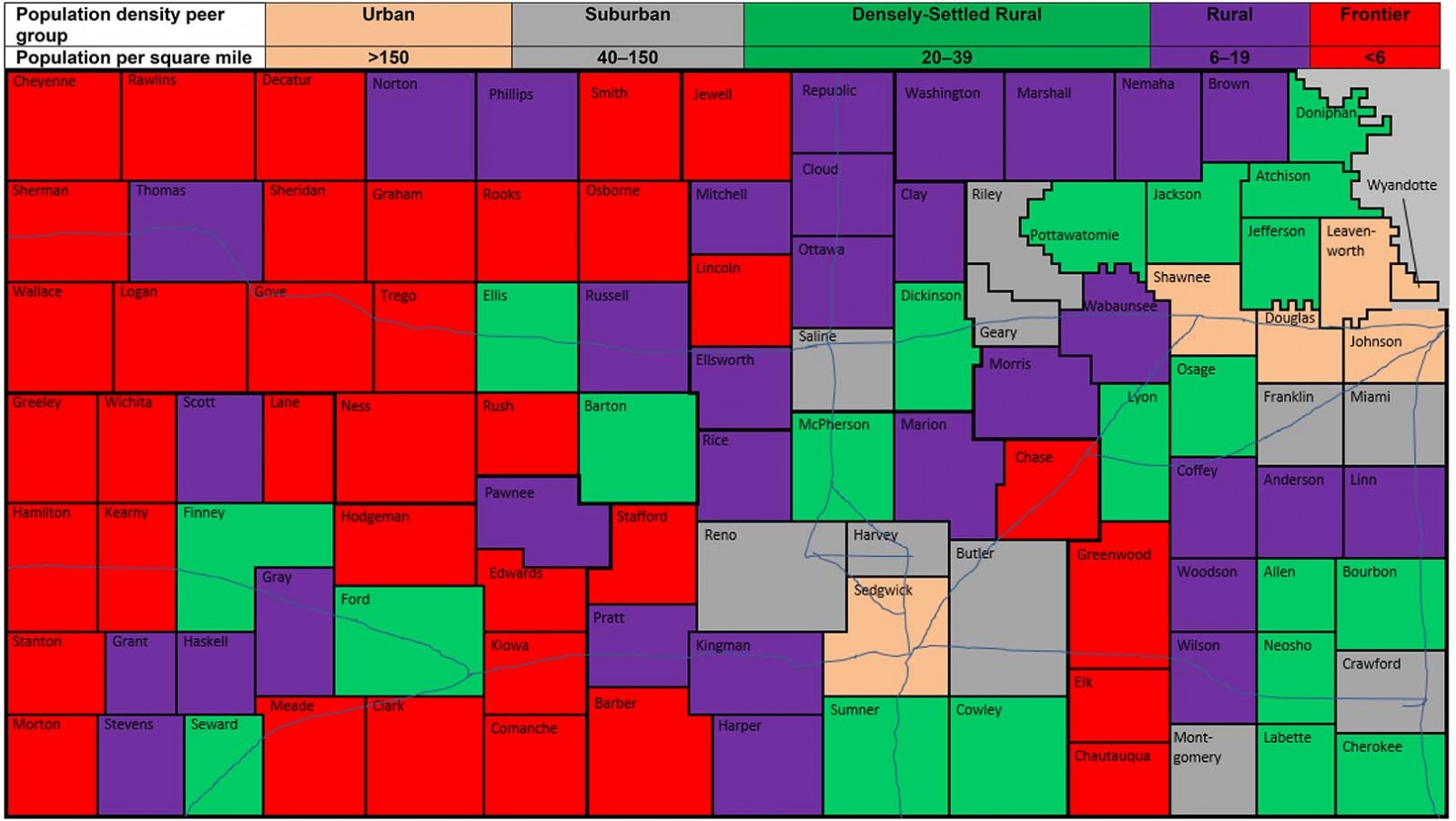 Figure 1: Counties are divided into population density peer groups for the purposes of describing their relative rurality. (Urban is defined as >150 persons per square mile (psm), Semi-Urban are counties with 40–149.9 psm, Densely-Settled Rural are counties with 20–39.9 psm, Rural have 6–19.9 psm, and Frontier have fewer than 6 psm7).
Figure 1: Counties are divided into population density peer groups for the purposes of describing their relative rurality. (Urban is defined as >150 persons per square mile (psm), Semi-Urban are counties with 40–149.9 psm, Densely-Settled Rural are counties with 20–39.9 psm, Rural have 6–19.9 psm, and Frontier have fewer than 6 psm7).
Data analysis
Survey results were filtered based on provision of maternity care (Fig2). Projections from providers were then mapped onto a county map of Kansas for 2018, 2020, and 2030. Counties without a single provider were given the designation of ‘maternity desert’8. Projections were made based on survey responses depicting intent to retire and based on physicians reaching average age of retirement for physicians in Kansas (age 67 years). ‘At-risk’ counties were determined based on practice changes identified through the survey.
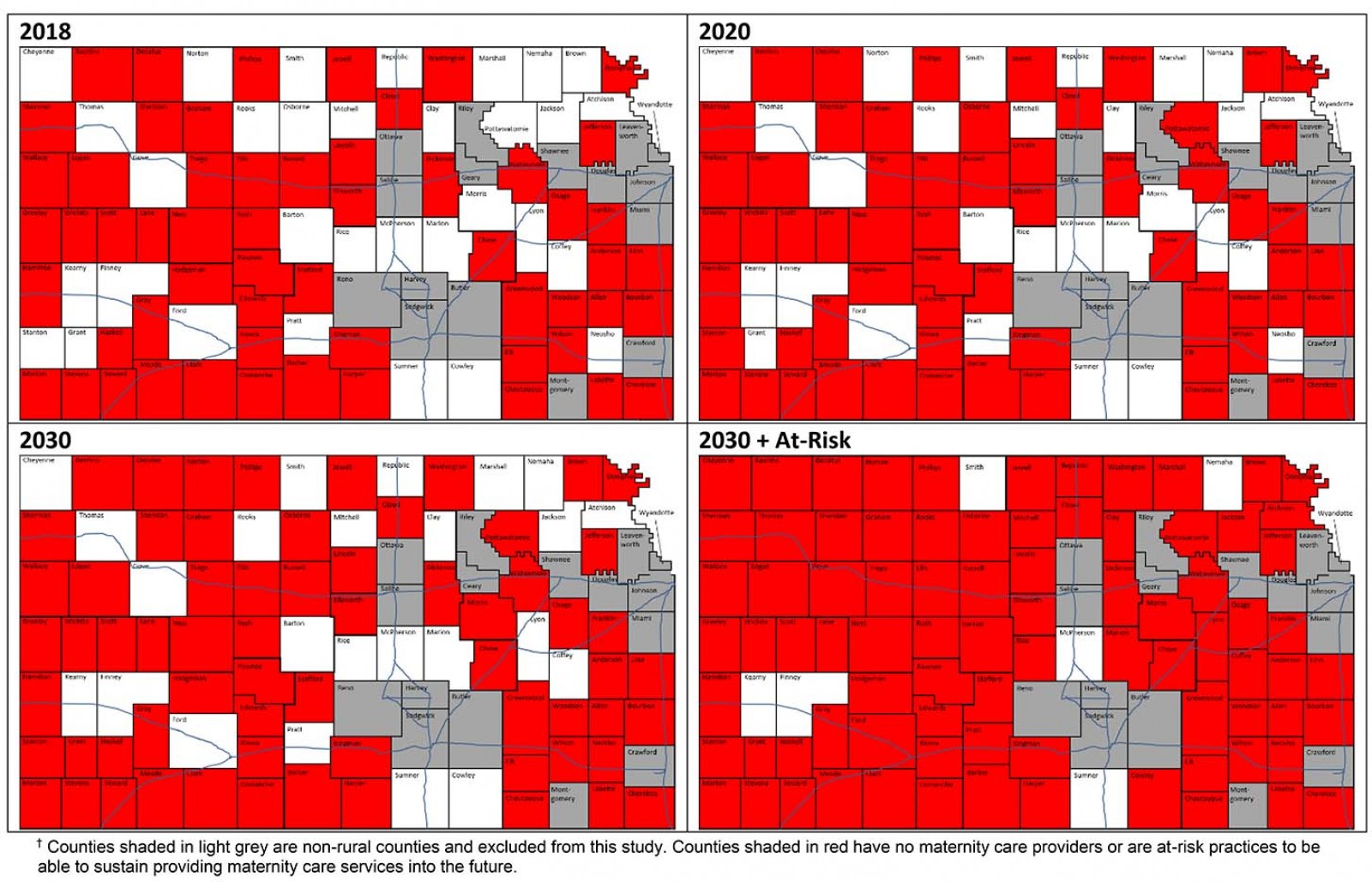 Figure 2: Current and projected maternity deserts in USA.†
Figure 2: Current and projected maternity deserts in USA.†
Ethics approval
This study was reviewed by the University of Kansas Medical Center Institutional Review Board and determined to be exempt, IRB Study #00004198.
Results
There were 869 active physicians in frontier, rural, and densely settled rural Kansas. The authors also summarized physician activity based on the population density peer groups to compare between Frontier, Rural and Densely-Settled Rural counties. These results are summarized in Table 19.
- Frontier counties had 96 active physicians, 94 of whom identified as family medicine physicians, and there were no OB/GYNs. Among these, 19 were MCPs. Surveys from 18/19 (94.7%) MCPs were collected.
- Rural counties had 212 active physicians, 115 of whom identified as family medicine physicians, and there was one board-certified OB/GYN who was not offering maternity care services at the time of the survey. Among the family medicine physicians, 43 were MCPs. Surveys from 31/43 (72.1%) MCPs were collected.
- Densely-Settled Rural counties had 561 active physicians, 164 of whom identified as family medicine physicians; there were 30 listed as general practitioners, and there were 26 OB/GYNs. Among family medicine, 36 were MCPs and 33 (91.7%) participated in a survey. Among OB/GYNs, 19 delivered babies and 15 (78.9%) returned surveys.
In total, this led to a total of 202 non-urban respondents (23.2% of all practicing physicians). 184 of these, 184 fully completed the questionnaire. More important for this study are the 117 maternity care providers among these counties. Of these 117 MCPs, 97 completed a survey over the 3-year period (83% response rate among MCPs), and 94 were providing maternity care services. Amongst all respondents, only two counties noted the presence of active CNMs. Demographics and practice information for physicians providing obstetric services are summarized in Table 2 and Figure 3.
The provider maps in Figure 2 were generated using the data from the 3 years of the survey. It is evident that a significant portion of the population must travel to the next county to access maternity care services and is therefore outside an 80 km drive to the nearest obstetric provider. Currently, only 32 of the 89 non-urban counties have at least one provider for obstetric care. The authors anticipate that over the next 2 years the number will decrease to 28 counties because four counties will likely lose their maternity care provider. By 2030 there will continue to be a decrease to a projected 24 counties.
There is an additional hidden risk as healthcare systems lose maternity care providers. Ultimately this will result in a practice that is unsustainable due to the burden of call. For example, a physician retiring from a practice of only two or three physicians could lead to an on-call situation every night or every other night. This is clearly not sustainable long-term. Prior studies have shown that practices with one obstetrics provider are likely to close in less than 12 months and that practices with fewer than two providers are unsustainable long term10-12. It has been previously published that solo providers and hospitals that deliver fewer than 240 babies per year are more likely to stop providing obstetrics care due to staffing and financial challenges. Additionally, four rural hospitals in Kansas have closed in the past 4 years due to financial difficulty; low census of both obstetric and non-obstetric patients has reinforced the instability of these at-risk counties13-17. Taking these facts into consideration, the situation begins to look dire. Using the criteria of sustainability, the 2030 projection would be that only 6 of the 89 non-urban counties would have sustainable maternity care practices maintaining reasonable access to services.
Current obstetrics providers expressed reasons for their motivation to provide maternity care services. The most cited reason was professional enjoyment/passion/fulfillment (43 of 94), followed by community need/service/duty (41 of 94), and 10 did not answer. No providers cited increased income as a motivation, although 71 of 94 noted that obstetrics services provided a monetary boost to their practice.
For the 25 providers who intended to stop providing obstetrics services within the next 10 years, motivation for stopping was assessed. Excess hours/call duty (7/25) was the most frequently cited reason for planning to quit. Retirement (5/25) and burnout/lack of enjoyment (5/25) were the next most common. Other reasons for planning to quit included cost/liability/low volume (4/25), hospital/facilities/anesthesia (2/25), and moving from current area of practice (2/25).
Table 1: Known obstetrics providers and survey response rates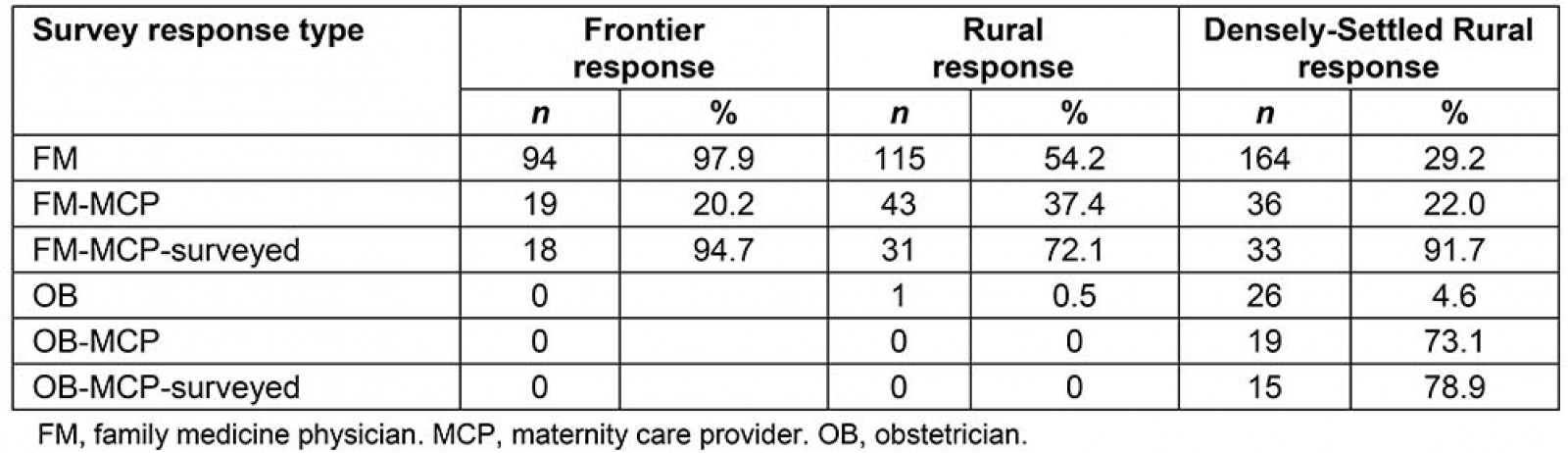
Table 2: Respondent demographics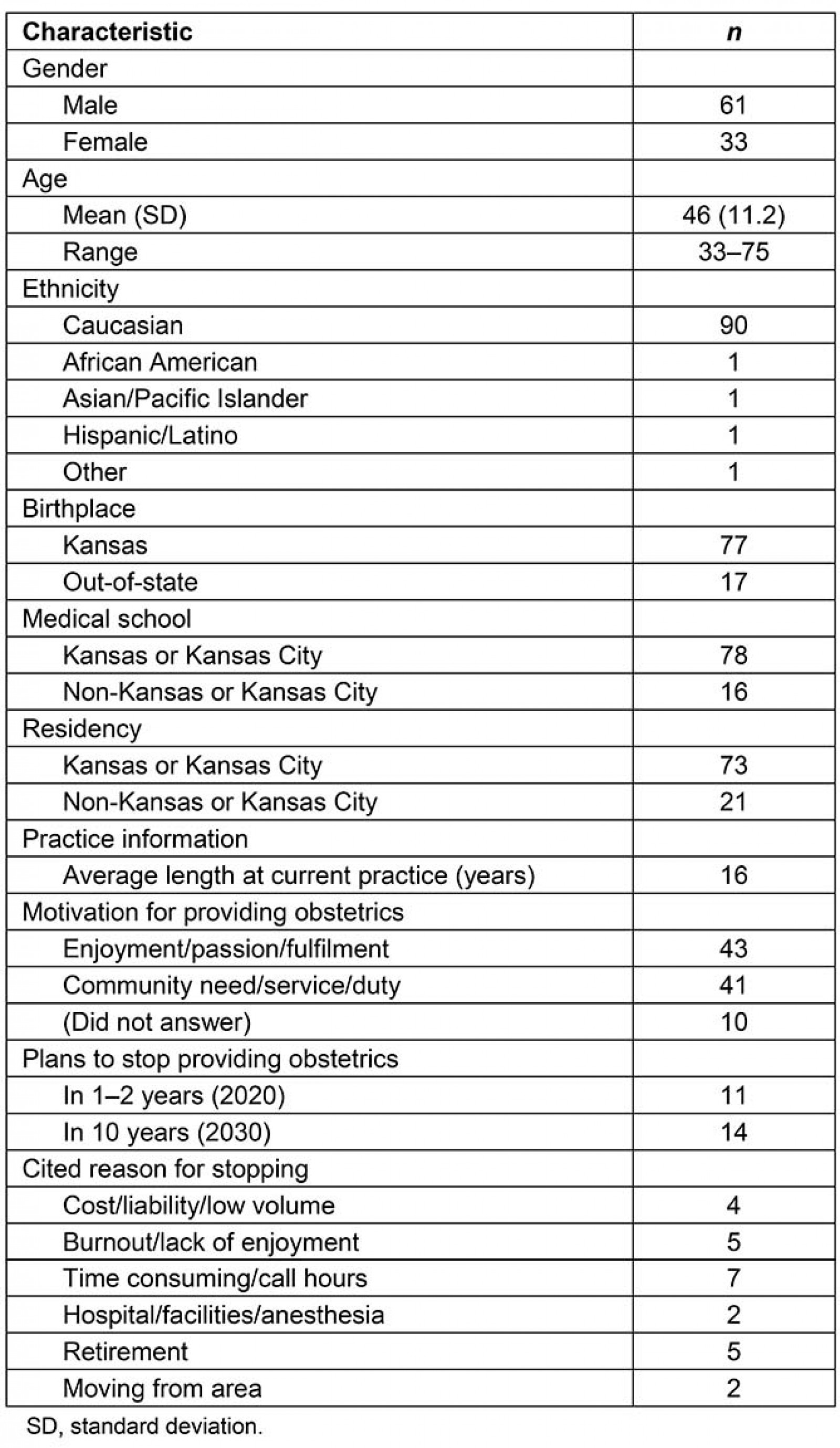
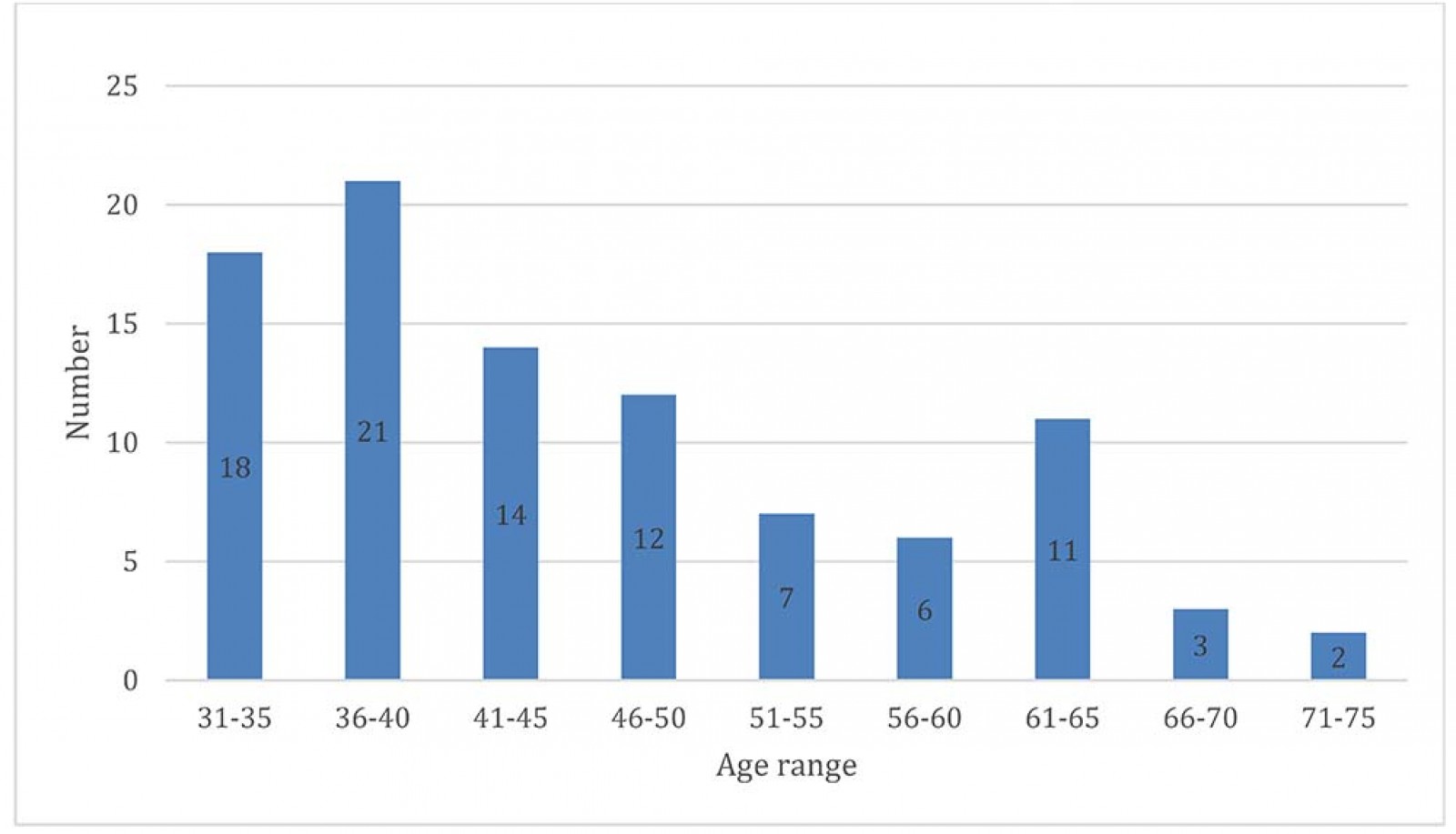 Figure 3: Age distribution of current obstetrics providers.
Figure 3: Age distribution of current obstetrics providers.
Discussion
The distribution of the availability of maternity care services in rural Kansas was previously undescribed. Through the data collected in the present survey over a 3-year period, the potential risk for loss of access to maternity care services in rural Kansas has become clear. The current state and future projections for the year 2030 reveals the likely expansion of maternity deserts making access more challenging. Even in the current situation, poor access to care may be contributing to unnecessary pregnancy complications and increased cost of care for rural obstetric patients, as has been shown in other predominantly rural states2,18.
Several studies have been conducted on how to improve maternal and birth outcomes in underserved areas in other countries. However, these studies did not attempt to map obstetric providers or evaluate individual providers’ likelihood of ceasing to provide care in the future. A potential source of future research would be to evaluate practices utilized by others to design initiatives in policy, healthcare practice, and education to intervene in the dire predictions made in present study. Residents and medical students will need to be surveyed on where and how they intend to practice. Kansas already has leading programs to address rural healthcare workforce challenges. Over the next 10 years the authors predict a significant loss in rural workforce due to attrition primarily from retirement. There are also significant financial challenges in rural and frontier hospitals.
The state medical school in Kansas has several successful programs that incentivize rural practice. There are programs that provide tuition forgiveness in exchange for rural service, programs for early acceptance into medical school, and programs emphasizing rural medicine with several rural training experiences in family medicine and obstetrics and gynecology. The locations of graduates are actively tracked and although the school enjoys high rates of placement in rural areas, it is concerned about the imbalance between annual attrition of physicians and supply. In addition, these programs do not currently focus on improving the situation with access to maternity care. It is the authors’ hope that by quantifying the issues in rural maternity care access a renewed effort can be made to address these potentially very serious concerns.
A recent initiative by the state of Kansas allows for independent practice of CNMs. In January 2020, Kansas passed a statute allowing for the independent practice of midwifery. This new license will allow certified nurse midwives to obtain a license through the Kansas Board of Healing Arts, provide care to women, perform vaginal deliveries, and provide initial care of the normal newborn. Over the next few years, it is anticipated that the database of independent CNMs will provide more information about practice locations and maternity care services.
One possible reason for the severity of the expansion is the distribution of physicians by age. Over the next 10 years, the majority of the Baby Boomer generation will reach retirement age7,19,20. According to this survey, the vast majority of current providers were born and received medical training in Kansas or the Kansas City area. Additionally, approximately half of respondents cited the theme of community need/service/duty as their motivation for providing obstetrics care. This may suggest a contributing factor to higher rates of burnout and intolerance of increased hours. An additional arm of KS-ROAT is seeking to better understand these factors, particularly in leading more directed efforts to develop programs and policies to provide coverage over current maternity deserts and prevent the projected expanding deficit. Nevertheless, the maternity deserts identified in this study have described a dire need for rural obstetric providers in Kansas. Further dedicated study and intervention will be required to prevent the potential adverse obstetrics outcomes that this study outlines.
Study limitations
Lay midwives are not characterized and there are no central registries to be able to assess their activity in rural counties. This study relies on self-reporting of future behavior from physicians in terms of their intentions on retirement. An assumption was made that physicians will retire at their average rate in Kansas at age 67 years. Some physicians may retire from providing maternity care before they retire completely from patient care. Many other factors were not considered in this study. Hospitals are under significant financial pressure and providing birthing services in the hospital requires maintenance of a significant infrastructure. Birthing units in small-volume hospitals may not be cost neutral let alone a benefit financially. The authors did not survey hospital administrators in this study. This will be an important addition to future studies regarding access to rural maternity care services in Kansas.
Conclusion
The majority of babies born in rural Kansas are delivered by family medicine physicians providing full-service maternity care services. CNMs are currently active in only two non-urban counties. The activities of lay midwives were not addressed in this study and remain unknown21-23. OB/GYNs are located primarily in larger cities/counties in Kansas. This is consistent with the average need for a patient base of approximately 10 000 and the fact that lower birth-volume areas will not provide enough patient care activity for a viable practice.
There are 89 non-urban counties in Kansas. Only 32 of these rural counties currently provide maternity care services. By 2030, the authors predict that this number will decrease to 24 counties. This means that the remaining 65 non-urban counties in Kansas would meet the definition of a maternity care desert. Women in these 65 counties will need to drive to an adjacent county or farther to obtain access to maternity care services, including for deliveries. Using a model of unsustainability, the authors predict a severe shortage with only six non-urban counties providing maternity care services. In western Kansas, the additional issues associated with severe weather during the winter will increase the risks.
Future areas of study regarding the development of further incentives for rural maternity care are needed. In addition, careful planning of maternity care networks including the development of access nodes for prenatal care services would be a beneficial area of study. Other areas of study under current consideration include CNMs, maternal satisfaction, adequacy of prenatal care, and birth outcomes related to distance traveled in Kansas to access services24,25.
There are significant areas in rural Kansas that qualify as a maternity care deserts according to the definition of the March of Dimes, a US advocacy organisation for the health of women and their babies8. Access to maternity care in Kansas is already a significant issue for many women in non-urban counties in Kansas. The authors predict that the size of these maternity deserts will continue to enlarge over the next 10 years. This may, in turn, impact maternal and newborn health deleteriously due to the distances traveled to access pre-pregnancy counselling, pre-natal care, and delivery services. Further study is needed to quantify the current health consequences for those individuals who must drive excessive distances.

