Introduction
An expanded role for pharmacists, although emerging in Australia, has been a priority for pharmacy associations globally1. Terms including ‘expanded practice’, ‘extended practice’ and ‘pharmacists’ full scope of practice’ describe the extension of the pharmacist’s role2-4. Expanded services are described as tasks usually provided by other health professionals (HPs) and offered in addition to pharmacists’ usual medication-management services4. Rural Australian community pharmacists have been recognised as being well positioned to expand services to address adversities of healthcare access for rural and remote populations5.
The Australian National Rural Health Commissioner (ANRHC) has suggested that rural allied health workers, including pharmacists, already work across an extended scope using generalist and specialist skills to meet diverse community needs with limited infrastructure6. The Pharmacy Guild of Australia (PGA) has recently submitted an article to the ANRHC describing the benefits of pharmacists practising to their full scope, particularly for rural and regional communities, where healthcare resources are limited and health outcomes are far worse than in metropolitan areas5. Access to quality health care, regardless of how remotely people live, should be equal to that available in metropolitan areas, and, as a result, cost-effective, innovative, needs-based models should be given due consideration5.
Low acceptance by other healthcare providers, in particular general practitioners (GPs), has been described as a major barrier to pharmacists’ ability to provide these expanded services1. Considering that a shared care, multidisciplinary, person-centred approach has been proposed by the ANRHC to improve access, distribution and quality of health care, understanding HPs’ perspectives of expanded pharmacy services is important6. There is also a need to identify expected barriers and enablers for expanded practice in Australia. Predicting informal and formal factors that shape both individual and organisation behaviour and ultimately practice outcomes when implementing new services is challenging7. The macro-, meso- and micro-analytic frame can be effective in health research to understand these complex interactions7. Current literature examining HP perspectives of potential expanded pharmacy services has largely reported on the GP–pharmacist interaction8-11, while perspectives of other HPs are underrepresented. For the pharmacy profession to undertake a paradigm shift to expanded practice, perspectives of other HPs on how to design the extended role in a collaborative way is important to understand7. Thus, this study aimed to explore rural and remote health HPs’ (doctors, nurses and allied health) perspectives of expanded pharmacy services in rural and remote settings.
Methods
Study design
A descriptive qualitative study with an ethnographic lens of rural culture was conducted12. In-depth semi-structured telephone or face-to-face interviews with 23 rural HPs were completed. ‘Rural and remote’ is defined using the Modified Monash Model, and all participants working in MM3–MM7 (large, medium and small rural towns and remote and very remote communities) were included13.
Participants, setting and recruitment
Ninety-two Australian rural HPs participated in a questionnaire about expanded pharmacy practice during July–September 201914. Participants, who were recruited through various Australian rural health networks and invited to participate in a subsequent interview, received no incentives for participating in the survey or interview14.
Procedure and semi-structured interview
All HPs who expressed an interest in participating were provided with a description of the project, and, on agreement to participate, written consent was obtained14. The interview was scheduled for a time and location convenient to the participant. Previous and current research in the area and examination of the literature informed the schedule of interview questions (Appendix A).
Interviews undertaken by an experienced rural pharmacy academic were audio-recorded and de-identified in the transcription process. Participants provided basic demographic data, including, age, gender, occupation and postcode.
Data analysis
All interviews were transcribed verbatim. Data were analysed by multiple readings of the transcripts, with coding and categorising into emerging themes. To ensure that objectivity, assumed knowledge and bias were minimal, a second member of the research team reviewed the first five interview transcripts and coding. Member checking was also undertaken by five participants, to support credibility and validity of the data. These participants were provided with a coded transcript and code book, to determine if the code/theme interpretations were fair and representative and to ensure an accurate portrayal of their voices. Participants were given the opportunity to make changes to their transcript and provide suggestions for data interpretation; however, none chose to do so. Data saturation was achieved after 15 interviews; however, the researcher continued to interview (and include in analysis) the remaining eight participants who had volunteered to ensure that there were no discernible new themes or linkages between themes.
Preliminary conventional content analysis of eight transcripts and field notes allowed the development of an initial list of codes, which were inserted into a coding manual with codes that were conceptually similar grouped together using an ethnographic technique of domain analysis12. The preliminary analysis was undertaken manually and a refined analysis using a hybrid approach of inductive and deductive coding and theme development was followed for all the transcripts using NVivo v12 (http://www.qsrinternational.com/nvivo)15. The World Health Organization (WHO) framework for integrated people-centred health services provided the theoretical model with the multi-level lens of macro- (policy level), meso- (health professional level) and micro- (consumer and community level) perspectives applied to the analysis16. Within the WHO framework, five strategies have been proposed to address the vision that all people have equal access to quality health services16. These strategies have then been aligned with macro- (strategies 2 and 3), meso- (strategies 4 and 5) and micro- (strategy 1) levels to provide a framework for the thematic analysis (Figure 1).
Ethics approval
James Cook University Human Research Ethics Committee granted ethical approval (H7845).
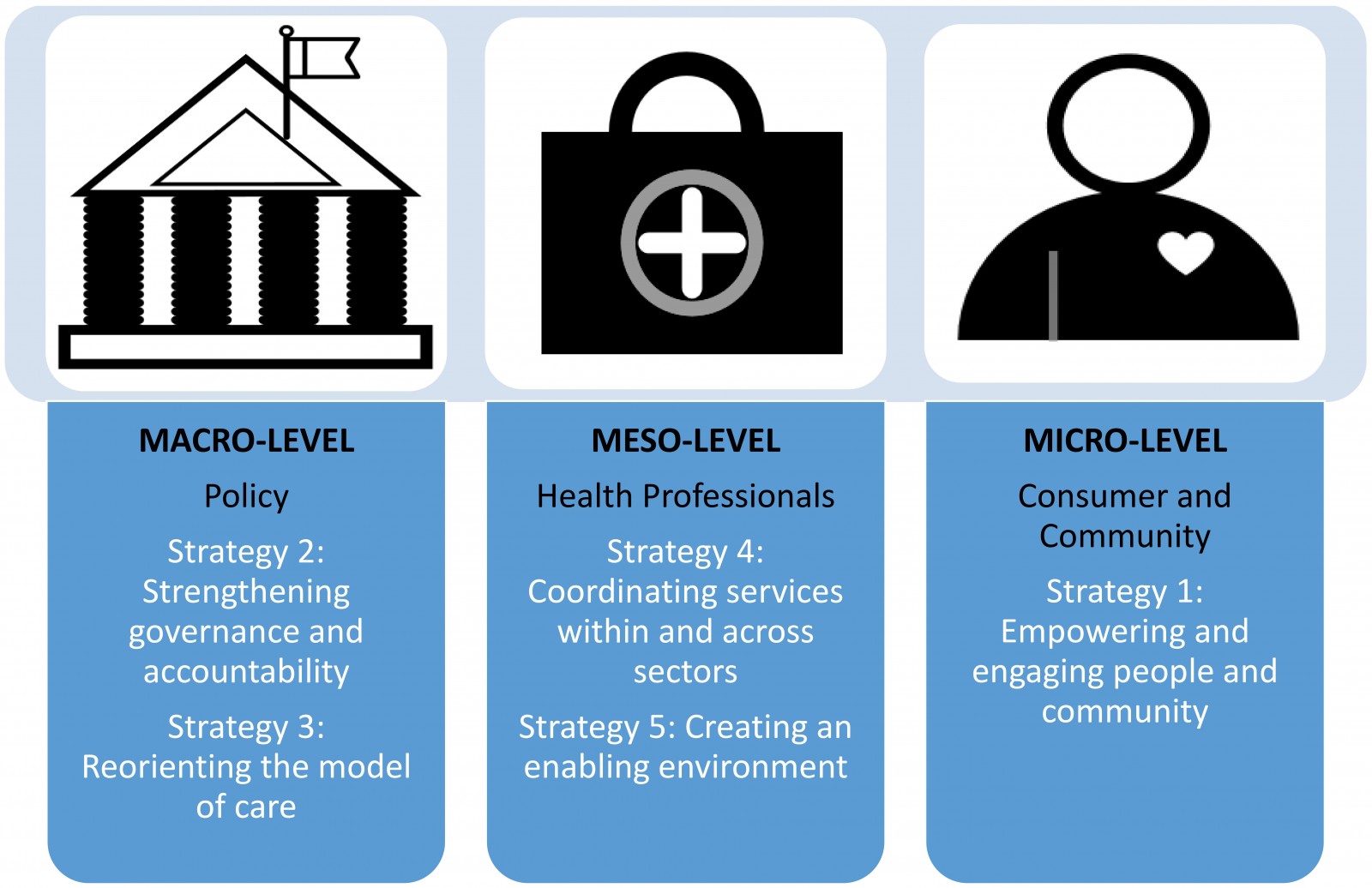 Figure 1: Thematic analysis framework based on the WHO Framework on integrated, people-centred health services16.
Figure 1: Thematic analysis framework based on the WHO Framework on integrated, people-centred health services16.
Results
Of the 92 HPs who participated in the questionnaire, 29 provided contact details to participate in an interview; six were unable to be contacted. Twenty-three interviews were conducted of duration 17–50 minutes, averaging 29 minutes. Participant demographics are summarised in Table 1. Participants were located in Queensland (17), New South Wales (1), Victoria (2), Northern Territory (1) and South Australia (2). A broad range of allied HPs (n=11) participated, with no more than two from each discipline. Disciplines included occupational therapy, physiotherapy, speech pathology, exercise physiology, public health nutrition, podiatry, and Indigenous health. Medical professional specialities (n=8) included general practice (7), emergency retrieval (2), women’s health, Indigenous health, and mental health with some doctors specialising in more than one area. Nursing specialities (n=4) included midwifery (3), chronic disease, remote practice, and emergency retrieval.
Data categories derived from the thematic analysis are provided in Table 2, together with a description of the codes incorporated. HPs’ direct quotations are numbered (PX-) and their primary occupations are provided.
Macro-level – policy
Strategy 2: Strengthening governance and accountability16: This overarching strategy includes the following themes: accountability, resources, integration and coherence.
Supportive governance from pharmaceutical, medical and allied health associations, in addition to government backing, was described by participants as essential for the effective development of expanded pharmacy services.
The Government would have to be on board with it, more support for the pharmacist and the community. You’ve got a specialist person there, why wouldn’t you give them the extra training to utilise them in other areas? … There is not enough doctors … Why can’t they use a pharmacist? (P22 – Aboriginal health worker)
Participants felt that the Australian Government should be accountable to ensure equitable access to health care for rural and remote people and that an expanded pharmacy model would potentially provide this access for some services.
There is a lot of value in the idea [expanded pharmacy practice], … the roll out would probably be hard … government could support it in remote areas … consumers would benefit from it, ultimately consumers would benefit from pharmacists being able to do more screening and identifying of issues. (P14 – physiotherapist)
Integration of pharmacists into general practice and multidisciplinary teams was discussed by participants, as an alternative model of expanded pharmacy practice. Participants suggested this integration would ensure coherence of health messages and patient care.
Integrating pharmacists into GPs [general practices] where they could actually do medication reviews inside the practice would be much more useful than being separated … it should be part of a team … it should not be fragmented or stand-alone … one of the risks is that we are getting more fragmented with the silos … it makes it more confusing for the patients. (P10 – general practitioner)
Strategy 3: Reorienting the model of care16: Reorienting the model of care to embrace expanded practice incorporated themes, including access, technology, defining health service priorities, holistic, preventative and comprehensive health care and expected outcomes of expanded services.
Isolation and the distance to healthcare providers, waiting 2–6 weeks to see a GP, visiting specialists two or three times a year and the inability to attract or retain allied HPs were described as common problems for rural and remote communities. Consequences of the limited level of service provision described by participants included visiting practitioners only being able to provide care to the most high-risk patients. Participants from remote communities frequently spoke about the dependence on nurses to screen and provide ongoing care for all conditions. Patients attending emergency departments for issues that could be easily managed in general practice was described as occurring regularly because of the difficulty and costs associated with accessing GPs.
To get an appointment the normal way like a phone call or the internet, about a six to seven week wait … I work in a rural community where we could quadruple the amount of GPs and we might just be able to meet demand. (P11 – general practitioner)
Allied health are not always stationed in a rural setting. Often they are fly-in-fly-out … or their caseloads are just ‘ginormous’ … they only see the children who are disordered as opposed to delayed. (P12 – speech pathologist)
Most participants saw the potential for pharmacists to expand their clinical practice to address the unmet need described. Strategies to support this included better utilisation of telehealth, including considering pharmacists as facilitators for telehealth appointments.
… whether it happens through the local hospital, pharmacy or doctor … it’s important for towns to have that telehealth service. That’s a very good service for patients so they don’t have to travel. (P6 – general practitioner)
Participants identified key considerations for developing an expanded pharmacy model. These included local healthcare needs, local health service capacity and deficits, and community demographics. This was described as particularly important in Indigenous communities. The importance of a community consultation process to develop any future expanded pharmacy service model was made. Participants felt the visiting nature of many allied health services and medical specialists was an enabler for the development of expanded pharmacy because pharmacists are often permanent members of the community, available extended hours and weekends.
Pharmacists providing preventative care services, including screening and education, was explored by a number of participants. The capacity for pharmacists to provide fast-tracked referrals to either visiting HPs or facilitate timely telehealth appointments was suggested as a model that could significantly improve patient access. Concerns about pharmacists being able to implement procedures to ensure appropriate communication to all health providers and recall systems to follow-up patients was also discussed.
We should be focusing on primary health care, first and foremost, stop treating the acute, start planning for primary care, maybe in 40 years, we will solve some issues … there are some primary healthcare elements that any HP can actually deliver … including a pharmacist, nurse, doctor or psychologist. (P23 – registered nurse/midwife)
The expected outcomes of pharmacists providing expanded services were seen as both positive and negative. There was optimism that pharmacist-delivered services would improve consumer engagement and health outcomes and increase the provision of collaborative care among health providers in rural and remote communities. There were expectations that pharmacists would be able to provide more appropriately directed referrals with adequate information for visiting specialists prior to them arriving in a community. In addition, an expected reduced demand on GP services was also a possibility that would allow GPs more time to provide quality health care and reduce patient waiting times.
The more that pharmacists are able to expand their services and use their skills the better. It will take the pressure off local GPs, emergency departments and hospitals. (P18 – registered nurse)
There was, however, some concern that pharmacists providing screening services for conditions such as mental health or diabetes would identify and refer more people into an already overloaded system, resulting in patients having longer waiting times to receive treatments. Alternatively, other participants expected a positive outcome because it would demonstrate true health need and potentially increase funding for these services.
Meso-level – health professionals
At the meso-level challenges and enablers to implementing expanded services that require further consideration were described.
Strategy 4: Coordinating services within and across sectors16: Coordination and collaboration among HPs was a core discussion point. All allied HPs and nurses expressed support for expanded pharmacy practice; however, GPs were less accepting.
I have both fears but also hopes, so in areas where there is clear need to improve access to primary care services, I can see that an expanded role for community pharmacists would be fantastic. (P20 – general practitioner)
There was consensus among the allied HPs participating, that those working in resource-poor, isolated areas were regularly expanding their scopes of practice for the benefit for their patients, without additional training.
All allied health fields, nursing and medicine need to work in expanded practice format. Everyone just shifts a little bit further out to create more coverage … there needs to be a bit more of everyone being given more skills to do more. (P1 – public health nutritionist)
GPs were also supportive of pharmacists undertaking clinical measurements and altering medication regimens, provided it was in a collaborative manner, with rapid communication and referral back to GPs for ongoing care.
If I’ve got a patient who is consistently above target with their BP … I would be happy for a pharmacist that I trust to call me and say ‘we have done some out of clinic readings and they are consistently this’. That would be appropriate, or at least as long as they communicate it, maybe adjust medication and arrange appropriate GP follow-up. (P11 – general practitioner)
Participants described what they believed would improve the likelihood of success of implementing an expanded pharmacy model. These included strong professional relationships, common patient-centred goals and colocation of service providers to improve efficiency of resource use and referral pathways. Frequently discussed as a potential enabler was a model that included effective communication between providers and shared medical records.
If it’s in a rural community where you work collaboratively with your local pharmacy and you know that the patient, they are better off going to the pharmacy than they are to emergency, then they should be able to. (P11 – general practitioner)
Strategy 5: Creating an enabling environment16: Creating an enabling environment for expanded services included concepts of pharmacist accessibility, pharmacist and community connection, quality assurance and safety, HP resistance, time and space, pharmacist skills and knowledge, and funding considerations.
Pharmacists and pharmacies were recognised as widely accessible and well connected to people in rural and remote communities, with extended operating hours and various services attracting consumers.
The pharmacist we have here has a really good reputation … consistency of people already on the ground is important, utilising the current community pharmacist would be a big enabler. (P2 – occupational therapist)
I trust a good pharmacist, in a small town they are one of the most very respected people because they’re open on the weekends, they do little favours for you, they help you navigate the medical system. (P17 – general practitioner)
Quality assurance and safety was described as a concern by many participants. Risks of expanding scope of practice for pharmacists included the potential for providing incorrect information, inadequate quality of care and causing patient harm. Concerns over patients delaying seeing doctors in preference for pharmacist services and the consequence that this delay may cause (eg worsening conditions) were also described. Similarly, concerns around misdiagnosis due to underlying or complex health issues was discussed. GPs raised concerns over missing opportunities with patients to undertake comprehensive healthcare assessments if patients were not attending GP practices for services such as vaccinations. Equipment issues such as point-of-care testing inaccuracies, inadequate specificity, quality control and calibration requirements and costs were raised. The potential increase in antibiotic resistance from inappropriate prescribing of antibiotics was also highlighted.
Concerns about pharmacists not having the time required for complex patients, patients having health concerns identified without the capacity for management and patients disengaging from services due to receiving mixed messages and having too many people involved in care were also discussed.
I have seen in Indigenous health where too many people get involved in chronic disease and they get too many mixed messages and the patients give up. (P9 – general practitioner)
Conflict of interest was a theme described often by GPs and less commonly by allied HPs. Pharmacists’ financial interest through business models and a desire for profitability was highlighted as a competing interest that could be detrimental to patients involved in expanded services. Specific mention was made of pharmacists prescribing and the need for separation between a prescriber and the person profiting from providing the medicine.
Time and space considerations were described by participants who suspected that pharmacists would not have the required time to provide expanded services and noted an already evident shortage of pharmacists in rural and remote areas.
It’s about capacity too, we talk a lot about pharmacists doing extra stuff, but do they actually have capacity. (P7 – nurse practitioner/midwife)
Pharmacists’ skills and knowledge to provide expanded services was described as pertinent to the provision of expanded services. Participants’ confidence in the capability of pharmacists to provide expanded services varied depending on the service. Many participants mentioned that they did not know what level of training pharmacists received, and based their comments on professional and personal interactions with pharmacists.
I find it hard to comment on pharmacists because I don’t really comprehensively understand all their training … community pharmacists are probably better equipped than hospital pharmacists … they are highly trained, if you think about a pharmacist … I think they are the most medically minded of all the allied health. (P11 – general practitioner)
They have the skills to do some prescribing. I think they probably know the medications better than GPs so in terms of other assessments I don't really know what they learnt in their course. (P1 – public health nutritionist)
Participants suggested pharmacists providing expanded practice could have an additional title, to indicate additional training or skill to provide assurance to the community and other HPs.
There would have to be strict standards if you are saying you are providing extended services, you would have to have a title, expanded practice pharmacist, something behind them to make sure you have ticked all your boxes, so maybe it is an accreditation. (P8 – podiatrist)
Participants empathised with how difficult training and upskilling can be due to cost and isolation and suggested using other local or visiting HPs to upskill the pharmacist.
Most participants agreed that pharmacists should be remunerated for expanded services; however, they expected that consumers would not be willing to pay for the services. It was suggested that pharmacies often advertise free services and consequently consumers would expect expanded services to be provided at no cost also.
What I’ve seen is that pharmacies offer free screening, free this, free that. So I think that at least from my cultural background, I would expect for a service to be free at the pharmacy. (P12 – speech pathologist)
Ultimately at this point, either the pharmacist is copping it on the chin and just hoping that they picked up a few bits and pieces that they can put through their till. It’s going be the patient paying for the entire cost, but I think there is a role for Medicare stepping in and saying these are the item numbers that pharmacies have and can access, similar to the optometrists. (P6 – general practitioner)
Micro-level – consumer and community
The micro-level of the analysis examines HP perspectives of current rural health issues, specific expanded services rural pharmacists could provide and the potential of these services to empower and engage people with health.
Strategy 1: Empowering and engaging people and community16: Participants reported chronic conditions, including mental health, diabetes, cardiovascular, renal and respiratory disease, as the most prevalent health concerns in rural communities. Infectious diseases, including dermatological conditions, otitis media, rheumatic heart disease and bronchiectasis, were also common conditions for very remote participants. Many of these conditions are related to socio-economic disadvantage, cultural diversity of rural populations and limited access to health services.
A lot of it is socially related just because of some of the unique characteristics of the population out here, eg Indigenous population, shift work population, FIFO [fly-in-fly-out] population, the people who are living and working out here who are estranged from their families of origins and support systems and the high rates of alcohol abuse out here, which is the accepted culture in this town. (P11 – general practitioner)
Participants recognised that pharmacists are well positioned to engage with a large proportion of community members. Many participants were supportive of pharmacists providing screening services, including mental health, diabetes, cardiovascular disease, acute infections (urinary tract and sexually transmitted infections), and speech and language disorders, provided strong referral pathways were in place. There was also consistent support for pharmacists to provide patient education, particularly around health literacy and self-management. Allied health participants were generally supportive of pharmacists prescribing, and saw this as a way of reducing GP burden.
People come into your pharmacy two times a week if people are on multiple medications. You are making contact a lot more than what a speech pathologist or a physiotherapist or even sometimes a GP would see the patient so for that reason [pharmacists] would be really good to screen stuff. (P3 – physiotherapist)
Participants proposed that pharmacists’ connection to their communities and patients make them well placed to recognise changes in patients’ conditions and the need for further action. This connection is particularly important for Indigenous clients, who may be resistant to travelling for health care.
Some people don’t even realise anything is wrong or don’t think anything is an issue, they are home and that’s all that matters. If there was someone there, to identify an issue then you may be able to get a telelink set up. It’s just that you’re that go between, that link you know. (P22 – Indigenous health worker)
By having a relationship with the patient, pharmacists are in a much better position to actually recognise deterioration or change in that patient. (P23 – registered nurse/midwife)
Table 1: Demographic data for participants (N =23)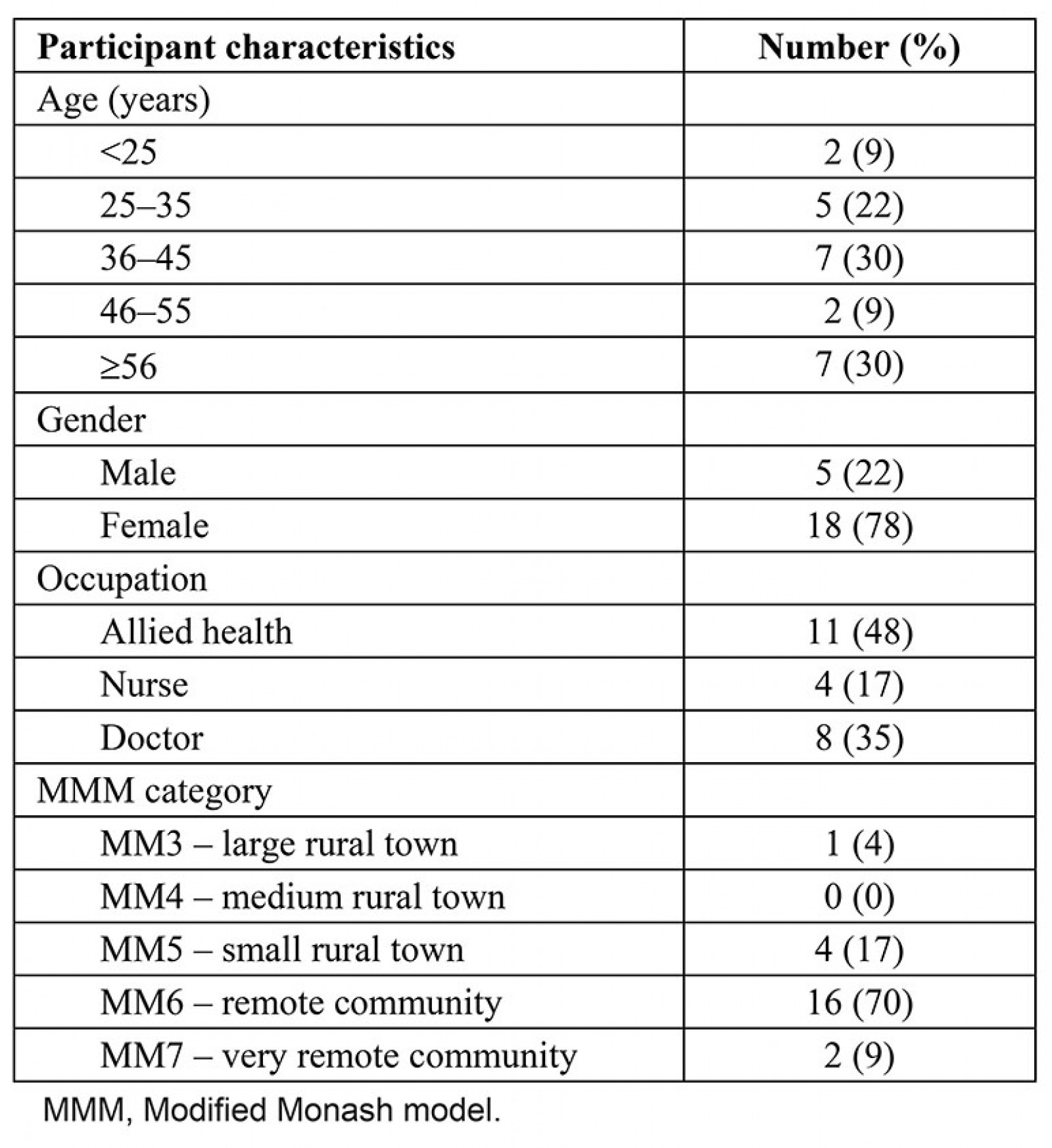
Table 2: Coding table aligned to the WHO framework on integrated people-centred health services strategies15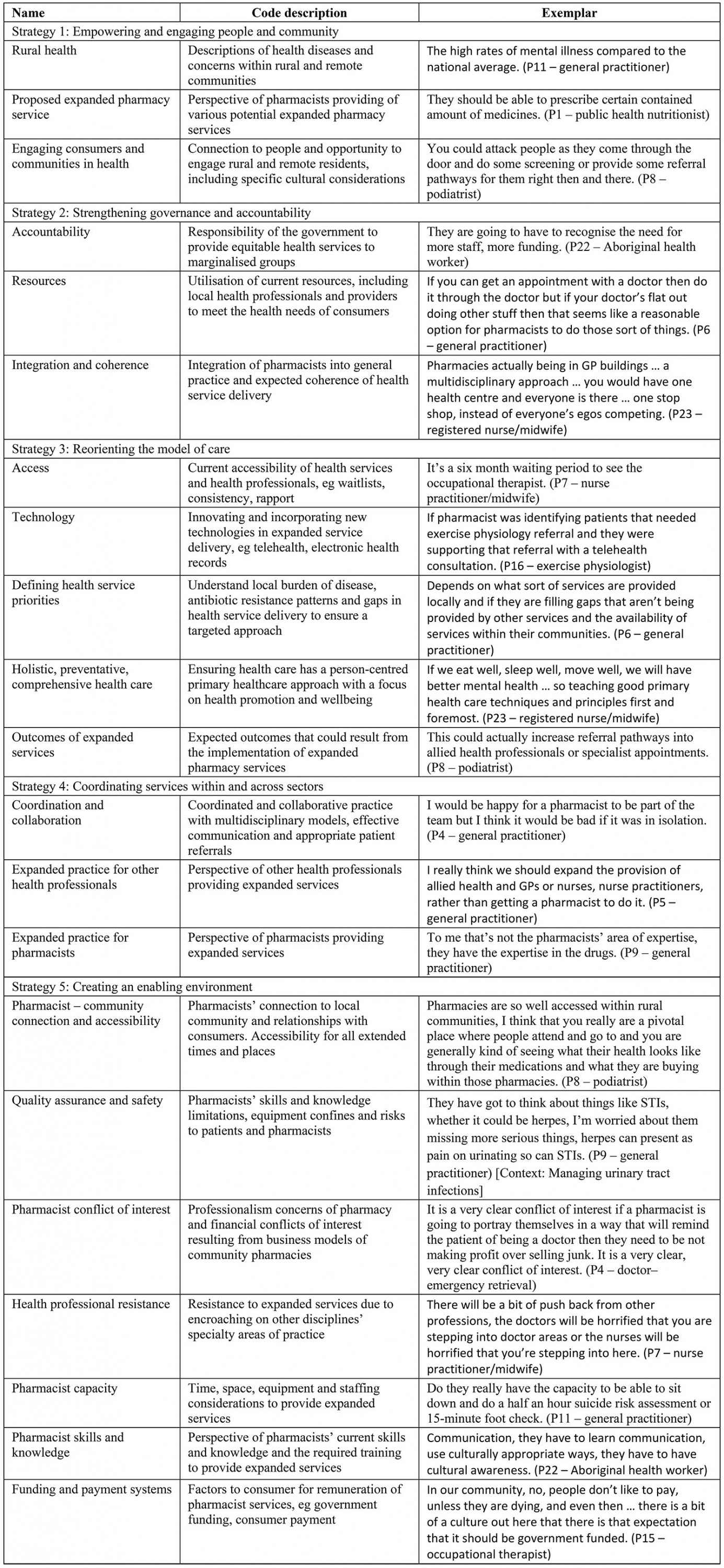
Discussion
Literature regarding rural and remote HP’s perspectives of expanded pharmacy practice is limited. Exploration of perspectives will therefore go some way to providing direction to guide the Australian pharmacy profession to develop effective and sustainable expanded pharmacy models in a rural and remote context.
Macro-level – policy
The first National Rural Health Strategy developed 25 years ago described the need for ‘innovative models of rural service delivery … to meet the diverse healthcare needs of rural communities’17. Although recognised, there is still no national strategy, and no specific mention of the current or potential contribution of rural community pharmacies to meet the healthcare needs of Australia’s rural and remote communities17. This highlights the need for the Australian pharmacy profession to raise their profile and progress rural community pharmacy on the national health agenda17.
Expectation that the Australian Government provide support and governance for expanded pharmacy services was raised as pertinent to the success and financial sustainability of expanded models. The PGA has proposed that pharmacists should have access to Medicare Benefits Schedule funds when delivering services to consumers, irrespective of where the pharmacist is practising (within community pharmacies, GP practices or multidisciplinary teams)18.
Results from this study have highlighted the importance of community consultation to ensure that development of an expanded pharmacy model is based on individual community needs. This local problem-solving approach would be likely to ensure that expanded services were filling gaps, and not duplicating current health services. It is a regular frustration that much of the current health funding is ineffective and wasted in rural and remote communities as a ‘one size fits all’ approach is applied to service provision17. However, a local approach may not be conducive to macro-level advocacy. Strong community engagement in all aspects of the health service provision, particularly in Indigenous communities, is well recognised17. However, funding models and health system structures often do not support this level of innovation17.
Generally, HPs in this study were supportive of expanded pharmacy practice models that focused on preventative, holistic care as part of the primary healthcare team17. Expanded pharmacy models were identified as one potential strategy to resolve the barrier of rural health workforce mal-distribution and address health service gaps. This has been identified in international studies where pharmacy-based services and ambulatory care pharmacists have reduced GP burden and demonstrated significant economic savings19.
Meso-level – health professionals
This level encompassing HPs and health organisations was most frequently discussed. Although expanded practice for pharmacists was supported in this study, there was some lack of consensus from GP participants. There was agreement in the value of pharmacists performing medication-management tasks and particular mention of the value of pharmacists working within GP practices or primary healthcare centres. This aligns with previous studies that have demonstrated GP support for pharmacists to work within their current scope of practice to assist with tasks such as providing advice to patients, particularly about medicines and reviewing medications10. However, previous studies have also raised GP concerns about fragmentation of care, if pharmacists were to undertake additional roles, and this was also found to be a concern for some GP participants in this study9,10.
A wide agreement from allied HPs about the benefit of all rural allied HPs providing expanded practice for areas of need was found in this study; however, some GP participants only supported expanded practice for nurses.
Resistance from other professionals should, however, not deter innovation in this area. The physiotherapy profession globally has been progressing their expanded practice (advanced physiotherapy practice)20 to include diagnosis, triaging surgical candidates, ordering diagnostic imaging or laboratory tests and prescribing/injecting medicines19. This has been in response to GP shortages and rising healthcare costs20. Australian physiotherapists have expressed support for some of these models20. Likewise, rural pharmacists have also reported very high levels of support for the implementation of expanded pharmacy services for their rural and remote communities21.
The importance of coordination and collaboration to deliver patient-centred care cannot be underestimated. Canadian pharmacists working in expanded roles have described a lack of a team-based approach from other health providers and particularly GPs not valuing services pharmacists can provide1. This reluctance to work collaboratively was also identified in this study; however, many participants described this approach as achievable if the expanded models are developed in consultation with healthcare providers working in the practice. GP concerns about pharmacists’ skills and knowledge to provide quality health care were also identified. This is not specific to GPs or pharmacists, as a lack of understanding other professionals’ roles and competencies has been described as one of the main barriers to interprofessional collaboration in primary care22.
Environmental considerations of expanded practice were discussed in depth in this study. Concerns about pharmacists’ available time and ability to provide quality assurance and safety were put forward as major barriers. Many participants acknowledged the existing pharmacist shortage in the rural workforce and expected this to be a limiting factor to expanded practice. This concurs with other studies of expanded practice in rural areas internationally23.
Micro-level – consumer and community
Rural community pharmacies’ ability to empower and engage people in health through community pharmacy accessibility was described as an enabler to expanded practice. Rural pharmacists were described as well-respected HPs with strong connections to people in their communities. Participants recognised that pharmacies are often accessible at times when other providers are not and are well placed to provide patient education and empower patients to self-manage their health. The PGA reiterates this by stating that an average patient visits their community pharmacy 14 times per year24. A recent survey of rural and remote pharmacy consumers identified that 96% (N=406) were supportive of expanded pharmacy services and 94% expected that the expanded services would improve health outcomes of people in their community25. Viability, however, depends on high uptake to support any funding models or to substantiate claims for improved health access. Canadian pharmacists providing expanded services have identified low levels of understanding among the general public about expanded services as a major barrier1. This highlights the importance of community education and promotion as part of any implementation strategy for an expanded practice model.
Limitations
Although participants involved were from various health sectors, states and territories with differing rurality, a large number of interviewees were from Queensland, Australia. As a consequence, the results may be applied broadly to rural practice and not specifically to particular health settings or localities. In addition, other stakeholders, including pharmacists, policy-makers, local government planners and consumers, were not part of the interview panel and thus further study to explore additional enablers and barriers to expanded practice for rural pharmacy and provide a more in-depth analysis of macro factors is needed.
Conclusion
Expanding pharmacy practice in the rural and remote context has been proposed as an initiative to improve rural people’s access to quality health care. Barriers to expanded practice have been identified across all levels of health, including political support, funding considerations, environmental suitability, pharmacist capacity and community uptake. Despite these barriers, positive outcomes are expected, including a more cohesive approach to health care, improved referral pathways and increased empowerment of consumers in self-management. This study provides pharmacists and rural health leaders with the first insight into potential barriers and facilitators of expanded pharmacy practice in rural and remote Australia from the group perspective of other HPs. Expanded pharmacy practice will only evolve if both government and rural health providers are engaged to contribute to the design and development of models to deliver better health outcomes for rural communities.
Acknowledgements
The authors would like to acknowledge and thank all of the rural and remote HPs who gave their valuable time to contribute to the study and for their ongoing work in rural practice.
References
You might also be interested in:
2015 - Re-orienting a remote acute care model towards a primary health care approach: key enablers



