Introduction
Over 270 000 individuals have been diagnosed with inflammatory bowel disease (IBD) in Canada1, and this number is expected to continue to rise. IBD is an umbrella term for two gastrointestinal (GI) illnesses (Crohn’s disease and ulcerative colitis) characterized by inflammation and ulceration. These immune-mediated, lifelong, chronic illnesses have unpredictable periods of exacerbation (active disease) and remission (inactive disease). Symptoms of active disease include frequent bowel movements, abdominal pain, weight loss, malnutrition, and fatigue1. IBD is most often diagnosed in early adulthood, but can occur in any age group1. Goals of IBD care include inducing and maintaining disease remission with medication and enhancing quality of life1,2. Factors that contribute to quality of life include achieving stable physical and mental health, contributing to society through work and school, participating in activities of daily living, connecting socially with others, and accessing healthcare services when needed1,2. Indirect costs associated with IBD include both short- and long-term work losses and out-of-pocket patient expenses, such as travel for medical care and caregiver support1. Individuals with active IBD are more likely than those in remission to require clinic visits, diagnostic procedures, hospitalizations, and surgeries, and these frequent health system interactions result in high care costs1.
Not all rural individuals with IBD have access to GI specialist services and therefore their IBD care management tends to fall upon family physicians, general surgeons, and nurses. Individuals living with IBD in rural areas are more likely to access acute care services through emergency room visits and hospital admissions3,4. In one study, 23% of patients residing in rural areas who required care for a variety of illnesses reported increased difficulties accessing specialist care; for patients with such access, 66% travelled 120–200 km to see the specialist5. Lack of patient access to and greater geographical distance from specialist care can lead to gaps in care and increased risk for IBD-related complications, such as the need for surgery3,6,7.
Researchers examining perspectives of access to IBD care in rural areas of Australia found individuals perceived decreased quality of health, limited access to multidisciplinary care, and poor communication and continuity of care between specialists and general practitioners (GPs)8. In the same study, rural healthcare providers (HCPs) indicated they were comfortable caring for persons with IBD, but some felt their IBD knowledge was lacking and their comfort level varied with respect to offering different medication therapies. They also believed outcomes for rural persons with IBD were worse than for their urban counterparts8. Persons with IBD and HCPs have reported barriers to care in rural areas, citing factors including increased distance to specialists, financial costs, and lack of rural multidisciplinary teams8. A recent study on perspectives on access to IBD specialist care in Nova Scotia highlighted barriers such as long wait times, limited resources, and poor communication9.
Research to address the provision of services to meet the needs of persons living with IBD in rural areas is critical to increase quality of care and quality of life. To the best of the authors’ knowledge, no studies have examined access to care experiences of HCPs or persons living with IBD in rural Canada. These individuals are the experts in recognizing the services needed to enhance care delivery. This project aims to build access and support for individuals living with IBD in rural Canada by identifying the services and resources they most commonly use and highlighting the priority services and resources perceived as missing. Ultimately, strategies with great potential to enhance the health and wellbeing of patients while decreasing direct and indirect costs to the healthcare system can be developed.
Purpose
This pilot study examined healthcare utilization and access to care in individuals with IBD who reside in rural areas within one Canadian province. The research questions explored in this study were: What are the care experiences of HCPs and persons living with IBD in rural areas? What are the enablers and barriers to optimal IBD care in rural environments? What strategies are necessary to enhance care delivery for these individuals with IBD? The goal was to enhance outcomes and quality of life of persons living with IBD in rural areas.
Methods
Research design
This patient-oriented, mixed-methods study followed a convergent design (QUAN + QUAL) where both qualitative and quantitative data share equal priority10. This article describes the qualitative findings. The conceptual framework guiding this study is a person-centered care framework11. Within this framework, the authors propose evidence-based strategies to integrate person-centered care within healthcare organizations and patient–provider teams with the ultimate outcome of greater access to care11. Qualitative description methodology12,13 was utilized for this study and was chosen due to its exploratory nature and naturalistic philosophical underpinnings. This methodology allows findings to be summarized and interpreted, but also allows them to be reported as close to participants’ natural experiences as possible12, ultimately honoring the participant perspective. This study was patient-oriented, with both patient and family advisor team members active and equal members in decision-making throughout the entire research project. Early on, patient and family advisor teams contributed expertise towards the development of the research questions and study design. They co-created, reviewed, and edited participant recruitment materials and interview guides, and agreed on the codes and themes to ensure rigor within the data analysis process. All research team members had the opportunity to review the research findings and contribute to manuscript development.
Setting and sample
The setting was one western Canadian province with a population of about 1 million. The provincial prevalence of IBD doubled between 1999 and 2016, from 341 to 664 per 100 00014. According to the estimated incidence rate, at least 150 individuals are diagnosed with IBD every year15. Currently, about 6500 adults live with IBD in the province, approximately 30% of whom live in rural areas15.
Inclusion criteria for persons with IBD were those who had a diagnosis of IBD, were aged 18 years or more, currently resided in a rural area (population <15 000) for any length of time, and spoke English. HCP participants were individuals who cared for rural persons with IBD, including physicians (GPs), registered nurses, or registered nurse practitioners who worked in rural areas (population <15 000), as well as GI specialists.
Recruitment, data collection, and analysis
Various recruitment strategies were used to reach rural individuals with IBD, including distributing study information through Crohn’s and Colitis Canada national and provincial social media outlets and local events, hanging posters in rural pharmacies, sending posters and letters of invitation to rural HCPs to share with rural-residing patients, snowball sampling, and word of mouth. HCPs were recruited through study information mailed to HCP offices, advertisements in professional association newsletters, and snowball sampling. Persons interested in the study contacted the research team directly via phone or email to voluntarily opt in to the study. Participants provided informed consent prior to completing a demographic questionnaire and then a digitally recorded, telephone interview. Interviews lasting 30–60 minutes followed a semi-structured interview guide and focused on gaining an understanding of participant perceptions of healthcare utilization and access to care in rural communities. Open-ended interview questions addressed the study objectives. Interview data were collected between May and December 2019.
Inductive data collection and analysis occurred simultaneously and guided the research process by allowing researchers to add interview questions to seek out alternative associations, possible relationships, or exceptional circumstances. Interviews were transcribed verbatim by a transcription company. A member of the research team reviewed the transcripts for errors or omissions by comparison against the digital recordings prior to coding. Data were stored and managed using NVivo v12 (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home). Using the thematic analysis process, initial codes were generated and then themes were identified, reviewed, and named16.
Ethics approval
Research ethics approval was obtained from the University of Saskatchewan (blinded for peer review process) (REB # BEH-954) prior to study commencement and participant recruitment.
Results
Demographics
Fourteen individuals living with IBD and three HCPs volunteered to be interviewed for this study. The three female HCPs were nurse practitioners with professional experience ranging from 7 to 20 years. The persons with IBD consisted of four males and ten females ranging in age from 20 to 76 years. Most individuals with IBD perceived their disease to be under control and were satisfied with their current care. Tables 1 and 2 contain additional demographic data.
Table 1: Characteristics of study participants living with irritable bowel disease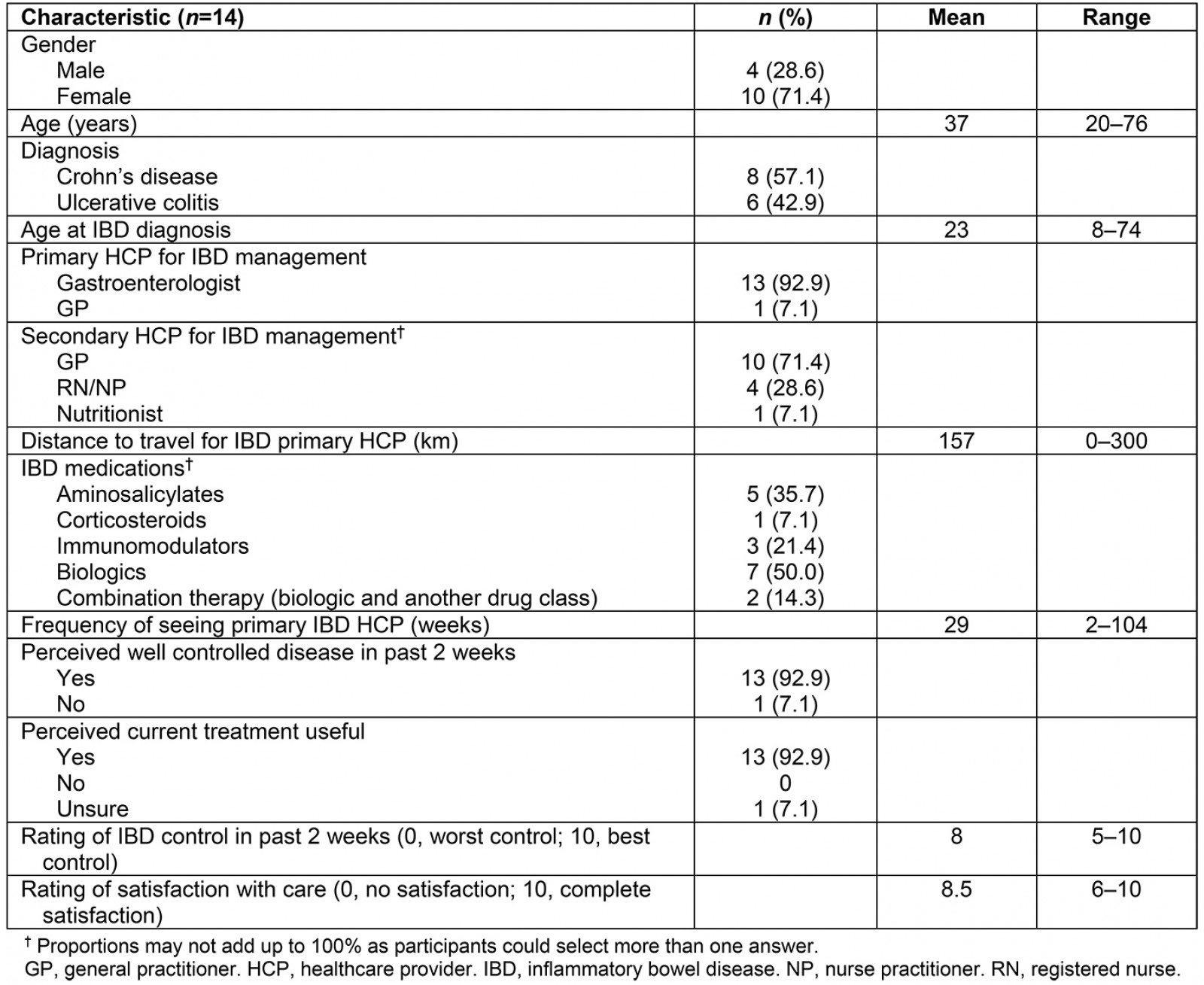
Table 2: Characteristics of healthcare provider study participants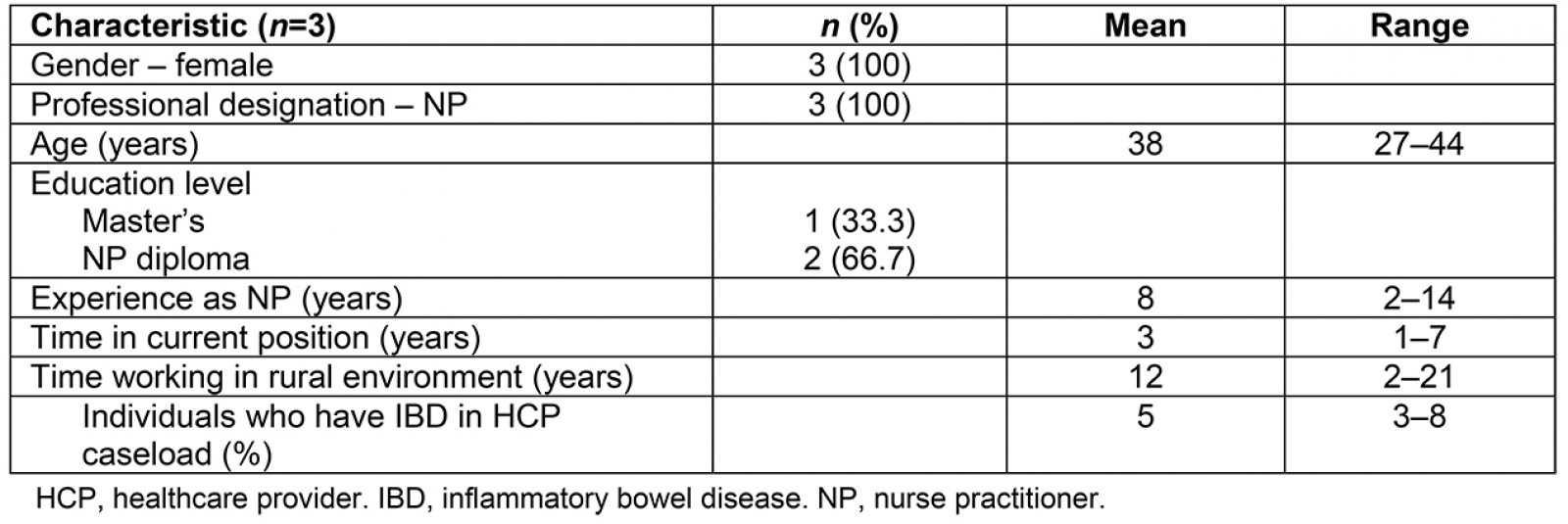
Interview themes
Three themes were identified from the qualitative data: communication, stressors and support systems, and coordination of care. Within these themes, participants described their IBD care experiences and healthcare interactions in rural areas. Enablers and barriers to receiving optimal care were discussed, along with strategies for enhancing care delivery.
Communication: Participants considered communication important for optimizing IBD care delivery in rural areas, and interacted with a variety of HCPs, including GPs, GI specialists, nurse practitioners, IBD nurses, ostomy nurses, pharmacists, dieticians, psychologists, and naturopaths. Most specialized HCPs worked in urban settings. All participants reported relying on clear, regular, and consistent communication with members of the IBD healthcare team to obtain optimal support for IBD care and management.
Remote communication with specialized IBD HCPs Lack of local specialized HCPs frequently meant participants required remote communication to coordinate ongoing care. The majority of specialized HCPs required individuals with IBD to travel to urban centers to communicate their care needs in person. Some persons with IBD were able to communicate certain care needs by phone and participate in remote services such as telehealth. However, for many participants, the inability to remotely communicate IBD care needs, relay important health information, and receive timely support were notable barriers for achieving optimal care.
The HCPs interviewed also noted timely, remote, collaborative communication with specialized HCPs was an essential factor in providing optimal IBD care in a rural setting. Ease of remote communication and collaboration with specialized HCPs varied, with some HCPs receptive to managing care based on blood work or symptoms and others requesting patients travel to urban centers for care.
Communicating emergent IBD care needs to local HCPs Many individuals reported concerns with the quality of emergent care received from local HCPs who were unfamiliar with their specific disease history or not acquainted with caring for persons with IBD. The inability to effectively communicate emergent IBD healthcare needs to local HCPs was identified as a substantial barrier to receiving optimal care in rural healthcare facilities. Participants expressed concerns that their experiences and expertise managing their IBD symptoms and exacerbations were often ignored and unvalued. For example, IBD participant 3 (PT 3) described a memorable experience with emergency services in a rural setting:
I couldn’t get in to see my doctor, so I went and sat in the emerg[ency] room for 17 hours and then finally saw a doctor and they said ‘oh you’re fine’, and sent me home. Then I ended up going the next day again because I had passed out from the pain, and it was the second day that they had taken me seriously.
Some participants were unable to receive care for emergent IBD issues in local hospitals and walk-in clinics, with HCPs instead directing them to their GI specialist.
Remote communication strategies for rural IBD patients Virtual care technology such as telephone services, video-conferencing, and telehealth were used to varying degrees by study participants. All HCP participants recognized the importance of being able to contact and communicate remotely with specialized IBD support to provide optimal care to their patients. HCPs voiced concerns with respect to the lack of remote communication services for direct patient care. HCP 1 stated:
There’s really no programming set up for people to quickly call their specialist or if they need to have quick blood work done or imaging … everything is 45 minutes away … if there was a team of people … that could help if I had questions or whether it be like arranging an IV iron infusion or Remicade [infliximab], we don’t have that in place.
Virtual care was supported by all participants as a method to optimize IBD care in a rural setting. However, only a few had experience utilizing these services for communicating with specialized HCPs; several persons with IBD expressed concern that in-person office visits were the only available option. Participants stated that virtual communication would be more cost effective and patient-centered because it would eliminate out-of-pocket expenses (eg fuel, hotel) and decrease lost personal and work time. Individuals who used Telehealth services were pleased with the quality of care they received. HCPs also suggested virtual care technologies were a reasonable solution to facilitate timely patient access to specialist services. HCP 2 noted:
[Province name] has a hard time recruiting enough specialists as it is, but if they could better utilize the ones we have with telehealth services and those kinds of things, I think that would make a big difference.
Stressors and support systems: Most individuals identified stress as a significant trigger for the exacerbation of IBD symptoms. Participants identified stressors as ‘worries’ or ‘uncertainties’ of IBD exacerbations and treatments, concerns about timely access to IBD healthcare services, feelings of isolation, lack of quality psychosocial support for managing their IBD, and daily and major life events. Both formal and informal support systems played a role in contributing to optimal IBD care.
Stress and IBD symptoms Several participants indicated that living in a rural community presented noteworthy challenges. When articulating what impact living in a rural area had on her quality of life related to IBD, PT 3 shared,
… my IBD is set off by stress 90% of the time, so being in the middle of nowhere can be relaxing … So there’s some good there. But again, having to travel everywhere can stress you out just as equally.
Isolation in rural areas The majority of rural participants noted that residing in a rural area meant being far from various supplemental IBD support services (ie support groups and networks, counseling, integrative healing therapies) that could assist with optimizing their care experience. Many individuals expressed that being chronically ill and having IBD are already isolating. For some participants, living in a rural community often magnified these perceptions. Summarizing their experience of having IBD and living in a rural area, PT 2 stated:
I think that it’s important to emphasize the additional isolation that comes from being in a rural setting where there isn’t really a larger community of people with IBD …
Living in a rural community meant less opportunity to connect with other individuals with IBD, and this lack of community contributed to feelings of isolation. More than half of the participants acknowledged IBD came with a certain amount of stigma, which made it difficult to publicly identify themselves as a person with IBD and speak candidly with others about their disease, thus further compounding feelings of isolation.
Formal support systems Some participants felt it imperative to have greater access to formal mental health services such as psychologists and psychiatrists. Approximately half of the participants had accessed formal counseling to help better manage their IBD, but not within their rural area. PT 1 spoke about her experience attempting to access counseling services through her local GP:
… they don’t factor in your physical illness affecting your mental illness … they make you go through kind of hoops to get somebody to help you … it takes a long time to get help … it’s usually someone within the city …
Informal support systems Most participants were engaged with various informal support systems that were primarily utilized to help expand their knowledge on managing their IBD and gain valuable peer support. The primary support systems used by participants were family, friends, peers, social networking websites, and online forums. Very few participants engaged with or had knowledge of local support group services in their rural area. Several participants suggested that access to local support group services would optimize their rural IBD care and management.
Coordination of care: Persons with IBD rely on a team of specialized HCPs and a combination of specific health services including pharmacy, infusion clinics, medical diagnostics, laboratory, and nutritional/dietary services to optimize wellness and maximize health outcomes. Although some pharmacy and basic lab and/or diagnostic services were available in a few local areas, most IBD-specific HCPs and supportive services were concentrated in urban centers.
Coordinating GI specialist care Many participants with IBD stressed the importance of regular monitoring, support, and guidance from a GI specialist to treat and manage their exacerbations and symptoms. Most individuals with a GI specialist and those awaiting referral reported long wait times for appointments. All GI specialist services for participants with IBD were in urban centers. The HCPs interviewed reported the coordination of optimal IBD care for patients was often dependent upon the timely guidance and support of their patients’ GI specialist and associated healthcare team. HCP 2 summarized the experience of providing care for patients with IBD in rural areas:
… depends which specialist we’re working with and how … receptive they are to giving orders over the phone and especially if the patient is having an exacerbation based on blood work and symptoms, if they’re willing to help treat them over the phone. We do have some that are very good at it and some that are quite resistant to it …
Local physician services for rural IBD care Most individuals with IBD reported using the services of a local GP to assist with their IBD care and coordinate medication refills, facilitate diagnostic services and lab work, provide basic health monitoring, and communicate pertinent health information to the GI specialist in between specialist appointments. Participants indicated local physician consistency varied, and described a high turnover of local GPs in their area or the need to change GP because the GP had retired or the practice had moved. Participants with access to a local rural healthcare clinic or hospital shared similar stories of high turnover rates of GPs providing care.
The frequent turnover of local GPs was highlighted as a potential barrier to ensuring regular follow-up care, preventing gaps in care, and enabling optimal care for persons with IBD. HCP 1 described the current physician turnover rates in her rural area:
… there seems to be a trend, especially in this area of the province, there’s a high turnover of providers. So then these patients are often left in limbo waiting for a new provider to come or a new provider to replace their previous provider. And in that time period kind of Russian roulette for them, hopefully their health is good during that time.
Some HCPs encountered lengthy time periods during which their communities were without the services of a local GP. One HCP reported more people using emergency services for regular health monitoring because of recent local GP turnover. Participants who experienced more consistency with local physician and healthcare staff expressed more satisfaction with the quality of locally provided IBD care.
Bypassing local health services Many participants with IBD reported bypassing local health services, indicating this results in greater access to specialized IBD care available in urban centers. Participants expressed concerns over some of the IBD care received from local GPs who were unfamiliar with IBD management in general, in addition to their individual IBD history and/or personal care needs. Specifically, over half of the participants with IBD expressed anxieties and worries about utilizing their local rural emergency healthcare services. Some participants reported not receiving the best medical solutions locally for their exacerbations and symptoms compared to health services in urban centers. When speaking about his experience seeking help for an exacerbation of IBD with a local GP, PT 6 stated:
The doctor literally told me, ‘I’ll give you whatever drugs you want’ because he didn’t know … he just said ‘I’ll be honest with you. I don’t know the disease. I don’t know what to give you’.
Distance to care The most frequently reported obstacle to achieving optimal IBD care for rural participants was the need to travel to obtain specialized and supportive health services (eg medication infusions, procedures, bloodwork, diagnostic tests, follow-up appointments). The distance to care also impacted individuals with IBD in other ways. The uncertainty of timely bathroom access while travelling to appointments and seeking emergent care was a noteworthy challenge. Many participants also reported experiences of driving to obtain medical services while enduring significant physical pain and subsequent distress. PT 7 described the discomfort of travelling the distance needed for specialized IBD care services: ‘… you’re in pain and had to travel two hours and … that two hours just feels like forever’. Participants also required the assistance of others to attend these appointments and incurred additional costs for fuel and hotels.
Bridging care to rural persons with IBD Participants proposed several solutions to address access to specialized HCP and support services. Most felt access to in-person specialist services in rural locations was unrealistic, and some suggested IBD HCPs could conduct satellite rural clinics. HCPs noted that if mobile GI specialist services were not practical, providing access to a mobile IBD nurse would likely improve access to care. Due to the limited supply of specialists, participants agreed that using virtual communication services (ie video-conference, telephone, or telehealth) would be a reasonable, cost-effective method to facilitate IBD-specific care services. A hotline or similar resource for rural HCPs to call for support with their patients’ IBD care needs was suggested as a potential enabler to optimize local IBD care.
Other suggested IBD services included enhanced pharmacy services and local infusion clinics. Many participants indicated access to nutritionist or dietary services specializing in IBD management would greatly enable optimal IBD care for patients in rural areas. HCP 3 expressed that nutritionist and dietary services often did not meet the specific needs of her patients with IBD:
[The regional dietitians] did not have any understanding of those patients with that level of inflammation and that level of disease and what dietary specific recommendations that they require.
Discussion
Interviews with individuals with IBD and HCPs identified communication, stressors and support systems, and coordination of care as key themes related to rural healthcare use and access to care. Most described challenges associated with living in these areas and identified suggestions to make the health system more responsive to the needs of individuals living with IBD. This section includes detailed strategies for health system delivery, providers, and persons with IBD that could be pursued to allow for greater access to care in rural areas using a person-centered care approach and is based on study findings.
Health system delivery: For all individuals with IBD, ready access to multidisciplinary integrated models of care is deemed essential and best practice17. Distinguishing features of patient-centered, multidisciplinary team care models include biopsychosocial assessment, coordination of child and adult services, active follow-up, and patient education17. Evidence from this study shows individuals in rural areas encounter significant access barriers, with integrated models of care not typically available. Initiatives to encourage access to specialized care delivery models should be strategized at the health systems level. Access to multidisciplinary models of care improves quality of life, particularly from a holistic biopsychosocial perspective18; exposure to integrated care is also associated with a lower risk of IBD-specific hospitalizations and surgeries19. Study participants identified increased access to mental health supports and IBD specialist dietitians as priorities. Individuals living with IBD have increased rates of anxiety and depression20,21, and ready access to online and in-person mental health services should be promoted to screen and manage psychological distress and promote mental wellness18. Individuals living with IBD frequently had dietary questions, so access to a reputable source of dietary information (eg a dietician) is recommended and key to evaluating nutritional status, preventing nutritional deficiencies, and to managing IBD-related symptoms and malnutrition associated with active disease22,23. Participants in this study believed they would benefit from a dietician’s expertise to manage their IBD, but access was inadequate due to the limited number of dieticians and the few who specialize in IBD care.
Participants with IBD welcomed and encouraged the use of distance healthcare delivery options, including virtual care measures such as telehealth, online clinics, telephone clinics or advice lines, web-based video-conferencing, and email communication. These offer a cost-effective alternative for persons with IBD and their caregivers that reduces out-of-pocket expenses and time off work to travel to and attend in-person appointments. Within the UK, distance delivery options are a part of standard care for persons with stable IBD24. Utilizing distance delivery for IBD care can increase perceived quality of life in persons with IBD25,26 as well as decrease outpatient visits and hospitalizations27,28. While distance delivery options are promising for IBD-related care, the issue of physician billing and reimbursement for e-health services may limit its use by some HCPs in some provinces or countries29. Underutilization of distance virtual technologies for IBD care is not uncommon and similar barriers are noted globally30. Since the COVID-19 pandemic was declared, telephone appointments for virtual IBD care have seen the biggest increase in utilization worldwide compared to other virtual technologies30. Nurse-led telephone advice lines are another distance management strategy to increase access to care for persons with IBD and are considered a standard in care within the UK23,31,32. Advice lines have become increasingly common and provide patients with ready access via phone or email to IBD nurses who can provide assessment, organize investigations and treatments, and facilitate access to clinics23. IBD nurses on advice lines can independently manage the care needs of patients and resolve patient questions 60–89% of the time32,33. Due to the quick response and patient-centered nature of advice lines, patient satisfaction is high33. Formally established nurse-led advice lines offer a promising strategy to increase access to care for individuals with IBD in rural communities.
Participants with IBD were frustrated when their expertise related to their condition was not valued or recognized by HCPs. This lack of patient-centered collaboration can lead to distrust and lack of optimal use of the healthcare system. Shared decision-making between HCPs and individuals with IBD should be encouraged to achieve quality care34,35.
Providers: Recruitment and retention of local rural HCPs is an ongoing challenge identified in this study and others36. A lack of rural HCPs creates significant challenges related to access to care in rural areas, which can lead to gaps in care and poor health outcomes for individuals with IBD. Participants in this study utilized their local GP HCPs for important chronic care management, such as medication refills and general health monitoring in between specialist appointments. Factors that encourage rural recruitment and retention include previous exposure to rural environments through upbringing or workplace experience, personal characteristics, financial incentives, and integration into rural communities37. Communities and health authorities must continually work to recruit and retain rural HCPs.
Interestingly, some study participants reported they bypassed local health services due to previous experience with HCPs who were not knowledgeable or comfortable with IBD management. While rural HCPs are not expected to be IBD specialists, some opportunities exist to strengthen their knowledge base related to IBD care. The lack of ongoing professional development opportunities for rural HCPs has been noted38, yet such opportunities could help rural HCPs feel more comfortable caring for individuals with IBD. Web-based, self-guided learning opportunities are available for HCPs who prefer to learn on their own39. Virtual information sessions led by IBD specialists is another alternative to provide education on current IBD management practices within the province or country.
Persons with IBD: Feelings of isolation within the rural environment, due to lack of psychosocial supports and disease stigma, were shared by participants. This is not unusual and such feelings are experienced by most individuals with IBD at some time40. Strengthening formal and informal support systems and enhancing psychosocial supports can reduce isolation, stressors, and stigma41. Awareness and participation in formal or informal IBD-related support groups should be encouraged. For example, connecting electronically through online platforms with other individuals who live in various rural areas with similar conditions or experiences can help form a sense of community. Individuals within the study reported limited experience with or knowledge of local IBD support services. Reputable organizations, such as Crohn’s and Colitis Canada, have provincial and regional volunteer chapters within the province under study, but these supports were not consistently identified by study participants. Involvement in a provincial Crohn’s and Colitis Canada chapter can provide informal peer support and connection with others. Online meetings should be a consistent offering of these organizations so that individuals in rural communities can join.
Various online and in-person individual and group educational initiatives were encouraged by participants in this study as well as in others8,35,41. These educational opportunities can encourage greater disease self-management, facilitate communication and connection between HCPs and individuals with IBD, and provide opportunities to connect with peers34. Main sources of IBD-related information include HCPs (eg GI specialists, IBD nurses, GPs, dieticians, psychologists), the internet, and other individuals with IBD41. Education-focused individual or small-group IBD clinic appointments are one strategy to provide information from reputable sources and connect clients with peers41. A pharmacist-led virtual clinic for medication-related questions is another possibility for additional education and information42. Online and printed education materials are valuable for meeting individual learning preferences34. The educational needs of individuals with IBD are variable and change over time based on disease stability, and therefore the information provided should be based on a needs assessment, cover a range of topics, and be provided by multidisciplinary HCPs43. Educational topics can include, but are not limited to, disease-related knowledge, dietary management, assessing credible websites, mental wellness, and strengthening support systems. Educational opportunities that encourage caregiver and support person attendance are also recommended40. All of these educational strategies can promote informed health-related decision-making and, ultimately, positive health outcomes and satisfaction with care.
Study limitations and future research
These qualitative findings result from a larger mixed-methods study undertaken in one Canadian province and therefore the generalizability is limited. Experiences of HCPs and persons living with IBD in other parts of rural Canada or beyond may differ. HCP participation was limited to only three nurse practitioners who volunteered to be interviewed. The perspectives of rural GPs are missing and identified as an area for future research. Future research should also include national- and international-scale studies on access to rural IBD-related health care from both HCP and patient perspectives. Reimagined design of existing rural health systems with patient input to increase the proactiveness and responsiveness to the needs of persons with IBD is recommended, with subsequent implementation and evaluation. An evaluation of health system redesigns that offer innovative virtual care access to rural IBD care is also warranted. Research findings that identify strategies to enhance access to care in rural areas should also be assessed in terms of transferability to other chronic illnesses.
Conclusion
This study provided a preliminary understanding of healthcare use and access to care by individuals with IBD in rural environments. The barriers and enablers to optimal IBD care were described along with strategies that can support greater access to care and improved health and wellbeing. Access to multidisciplinary care teams for individuals in rural areas is encouraged, as is the use of virtual care delivery options such as telehealth, online clinics, telephone clinics or advice lines, web-based video-conferencing, and email communication to increase access to care. Continued efforts to recruit and retain rural HCPs with knowledge of IBD are deemed necessary to provide continuity of care within rural environments. Strengthening formal and informal support systems and enhancing psychosocial supports in rural communities are warranted to ensure optimal wellbeing. Online strategies to provide individual and group education related to IBD are strongly recommended. Facilitating improved access to care in rural environments could have many benefits including increased disease remission, decreased direct and indirect care costs, and improved quality of life in individuals with IBD in these settings. These health system and access-to-care strategies can serve as a foundation to begin to address the unmet needs of individuals with other chronic illnesses in rural environments.
Acknowledgements and funding
We are appreciative of all of the individuals living with IBD and the healthcare providers who participated in this study. We also thank Michele Jungwirth for research coordination support during this project. Sprout Grant funding from the Saskatchewan Health Research Foundation and Saskatchewan Centre for Patient-Oriented Research is gratefully acknowledged.
References
You might also be interested in:
2018 - Lack of Medical Resources and Public Health Vulnerability in Mongoliafs Winter Disasters
2014 - The right staffing mix for inpatient care in rural multi-purpose service health facilities
2014 - 'Heart attack' symptoms and decision-making: the case of older rural women

