Introduction
Paederus dermatitis (PD) is an acute irritant contact dermatitis caused by contact with a toxin principally found in the body fluid of a beetle of the genus Paederus (Fig1). The toxin is released when the beetle is crushed against the skin1. PD is characterized by vesicles and pustules on an erythematous base with sudden onset burning sensation on exposed areas of the body2. Paederus species are found worldwide, except in Antarctica3. Paederus is more common in tropical and subtropical countries. PD is diagnosed in general practice throughout the year at the authors’ center; however, data specific to PD in Thailand remain scarce. Accordingly, the aim of this study was to investigate the clinical manifestations and progression, seasonal variation, and environmental factors associated with PD among patients attending the outpatient dermatology clinic of Siriraj Hospital, Thailand’s largest national tertiary referral center.
 Figure 1: A beetle of the genus Paederus.
Figure 1: A beetle of the genus Paederus.
Methods
This prospective cohort study included patients diagnosed with PD at the Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand during the October 2017 to July 2018 study period. Patients with suspected but inconclusively diagnosed PD were excluded. Sociodemographic and environmental data were collected by questionnaire. Clinical data were collected at physical examination and from medical records.
Statistical analysis
Patient characteristics were summarized using descriptive statistics. All data analyses were performed using the Statistical Package for the Social Sciences v18.0 (SPSS, http://www.spss.com).
Ethics approval
This study was approved by the Siriraj Institutional Review Board of the Faculty of Medicine Siriraj Hospital (approval number 503/2560(EC1)). All patients provided written informed consent before enrolment into the study.
Results
Twenty-five PD patients (16 females, 9 males) were included, with a mean age of 40.9 years (range 17–69 years). More than half of patients (60%) had an education higher than secondary education. Eight patients (32%) had underlying disease, and the most common disorders were hypertension (20.0%), diabetes mellitus (16.0%), and dyslipidaemia (16.0%). Lesion locations and characteristics are shown in Table 1. The most common sites were the upper (6, 24.0%) and lower (6, 24.0%) extremities. The neck and face were affected in five (20.0%) and three (12.0%) patients, respectively. Erythema, linear, and kissing lesions (where two skin surfaces contact) were found in 100%, 32%, and 28% of patients, respectively. Vesicle lesion was found in four (16.0%) patients, and pustule lesion was found in four (16.0%) patients. Central necrosis and bullous lesions were observed in two patients and one patient, respectively. Seventy-six percent of patients demonstrated more than one lesion.
Eighty percent of patients lived in Bangkok, and 44% of patients had a home near a farm or forest (Fig2). Three out of 25 patients lived in a multi-floor building, which was defined as more than 10 floors in this study. Fluorescent lighting was used in the homes of 24 patients. All 25 patients were treated with topical steroid, and some received other supportive regimens (Table 2). Supportive regimens that were given included antihistamine, topical antibiotic, wet dressing, and/or oral prednisolone. Two patients had post-inflammatory hyperpigmentation as a complication; only 7 of 25 patients attended the scheduled follow-up visit. No family members of patients had a history of PD symptoms. December was found to have the highest incidence, and January had the second highest number of cases. The mean time to complete cure was 12.6±1.3 days (min 5, max 21).
Table 1: Location of Paederus dermatitis and lesion characteristics of 25 Paederus dermatitis patient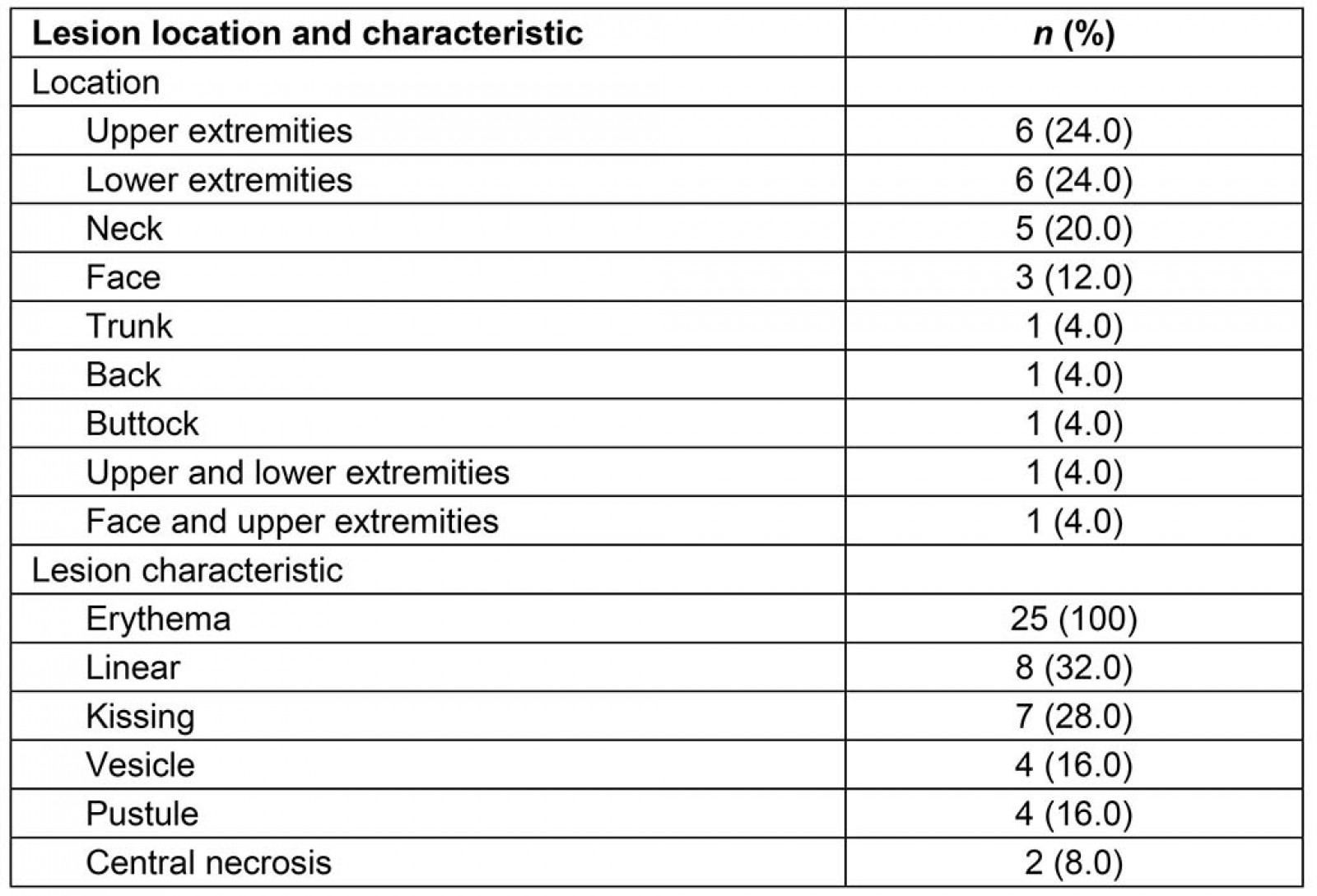
Table 2: Treatment-related data, environmental factors, time to cure and last known status of 25 Paederus dermatitis patients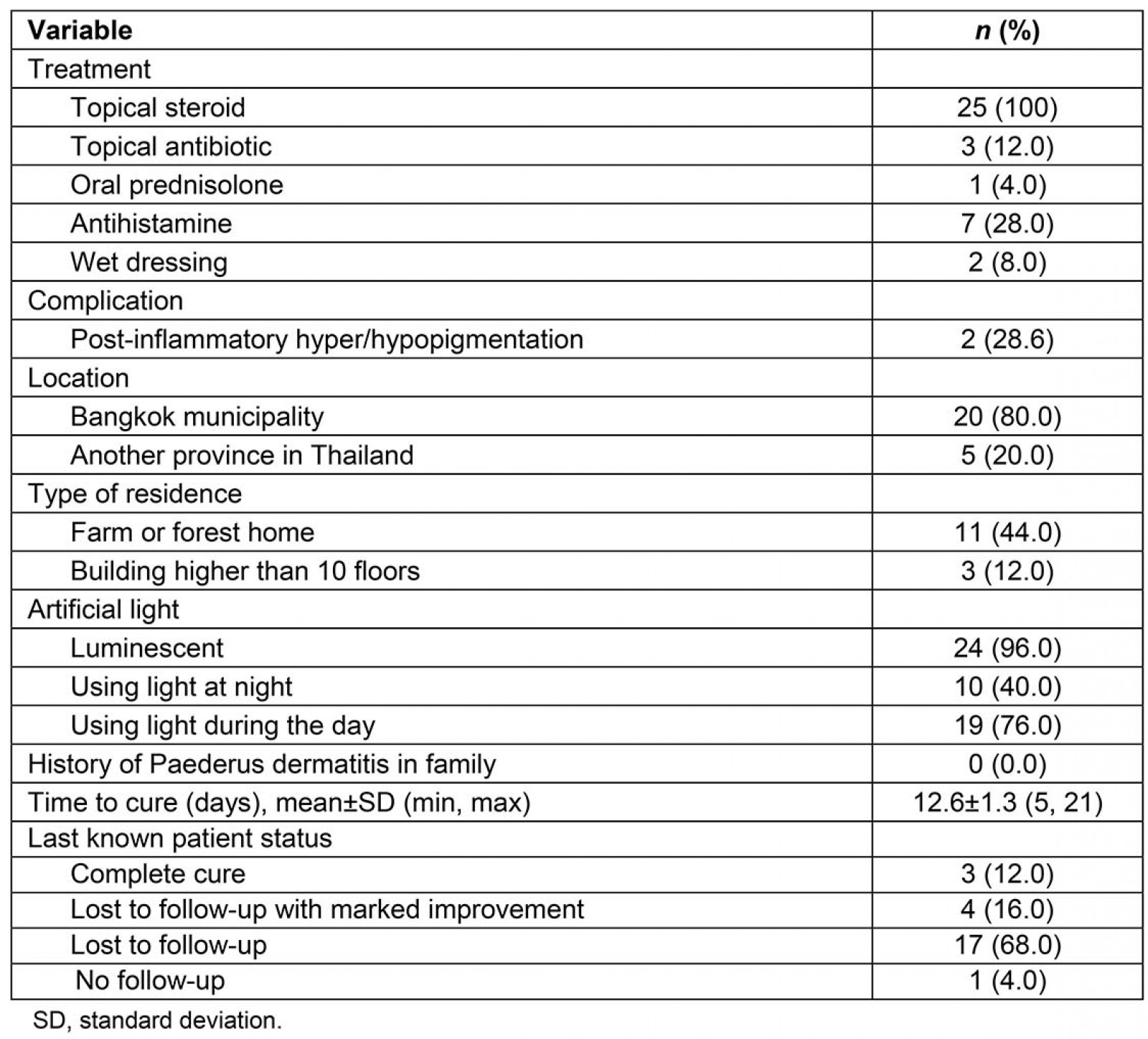
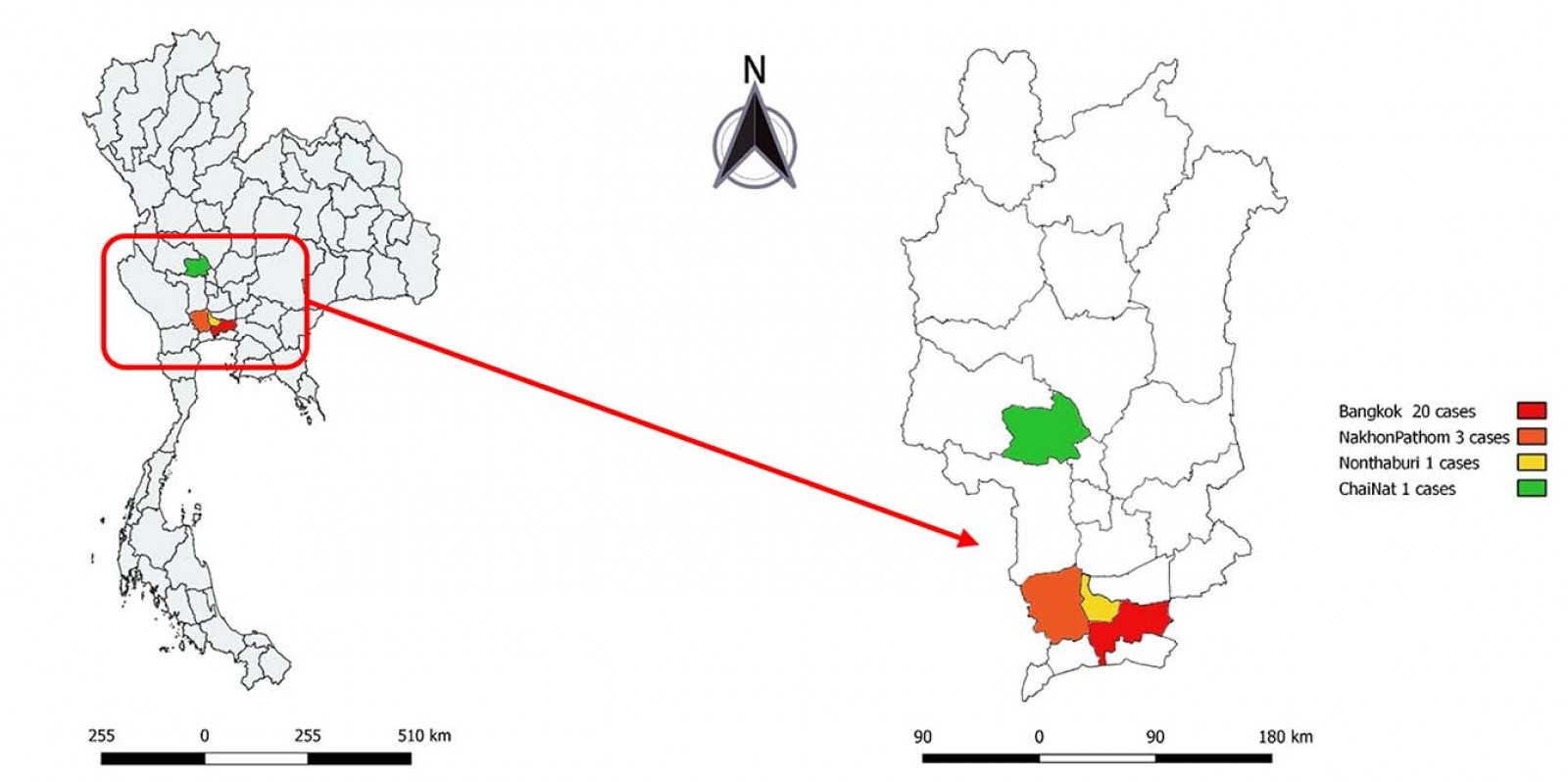 Figure 2: Location of Paederus dermatitis cases in central Thailand in present study.
Figure 2: Location of Paederus dermatitis cases in central Thailand in present study.
Discussion
The genus Paederus (family Staphylinidae, order Coleoptera, class Insecta4) consists of more than 600 species distributed worldwide, especially in hot, damp climates5. These small flying insects usually appear at night and are attracted by artificial light. The beetles do not sting or bite. Transfer of the beetle’s toxin to humans occurs accidentally via the inadvertent crushing of the beetle while on human skin. PD patients normally notice the symptoms of PD upon awakening in the morning6.
In the present study, all 25 PD patients had erythematous skin lesions, which are a sign of inflammation. This correlates with a study from Turkey that found erythematous lesions to be the most identified lesions7. Kissing lesion, a classic sign of PD, was found in only 25% of patients. The clinical signs of PD range from mild to severe. The severe form in this study was central necrosis. Skin lesions usually present on an uncovered part of the body, such as face, neck, or the upper and lower extremities2,8. Some patients also have lesions on unexposed areas, such as back and buttocks. In these cases, it is presumed that Paederus was crushed under the clothes. The clinical manifestations of PD mimic others diseases, such as herpes simplex, herpes zoster, allergic contact dermatitis, and liquid burns5,9. Diagnosis of PD is suggested by lesion characteristics, exposed sites, seasonal incidence, and case history.
Regarding the type and location of residence, more than half of patients lived near a forest or a farm, and three patients lived in a high-rise building. A 2016 study by Maryam et al found bright light sources and higher levels (ie multi-floor buildings) to be the main factors that attract Paederus to residential areas10.
Although PD presents all year round, it has variable seasonal incidence. In the present study, the month of December was found to have the highest incidence. In contrast to this study, Gnanaraj et al11 and Zargari et al9 found the incidence of PD to be highest in the months of April and September, respectively. These observed differences in peak incidence are likely explained by variations in humidity, season, latitude, and climate change. Paederus is not active when the temperature is less than 18°C. In Thailand, December is the month with the lowest average temperature. The observed high incidence during December in this study may be due to people opening the window instead of using the air conditioner, which facilitates entry of Paederus.
PD is a self-healing disease. However, supportive treatment may be helpful, such as topical steroids, oral antihistamines for itching, and wet dressing for wounds. In severe irritant dermatitis cases, systemic steroid is often required. Secondary bacterial infection, which can be treated by topical or oral antibiotics depending on severity, is a complication that may develop. The symptoms appear after 24–48 hours after contact and take a week or more to disappear. The mean time to complete cure in the present study was 12.6±1.3 days (min 5, max 21), which is consistent with the findings of Gnanaraj et al11.
PD can be prevented by avoiding human–beetle contact such as by closing windows and/or installing insect screens on windows and doors. Turning off the lights at dusk, which is the time when beetles are the most active, is another effective prevention measure. In addition to avoiding contact with beetles, PD patients should be advised to avoid rubbing, scratching, or otherwise touching the primary lesion.
Conclusion
PD is a form of irritant contact dermatitis caused by skin contact with the toxin of Paederus beetles. PD presents throughout the year, but the most active month was found in this Thailand study to be December. Skin lesions vary from mild irritant dermatitis to severe dermatitis, and the average time to complete cure is 12 days. History and clinical manifestation are essential for accurate diagnosis.
Acknowledgements
The authors would like to thank the patients that agreed to participate in this study, and Assistant Professor Dr Chulaluk Komoltri for assistance with statistical analysis.
