Introduction
Recruiting and retaining an adequate medical workforce outside of major cities has been a longstanding, worldwide challenge1. Over the past 25 years, the Australian Government has sought to address the workforce maldistribution by investing significantly in rural medical workforce education and training. The many Commonwealth investments in rural medical workforce include rural clinical schools and regional medical schools, university departments of rural health, Australian general practice training with its rural pathway, the Prevocational General Practice Placements Program, regional primary health networks, rural workforce agencies, and rurally bonded medical places and scholarships.
Despite these government investments and an 86% increase in domestic medical graduate numbers since 2007, Australia continues to rely on large numbers of international medical graduates, in particular to fill positions in regional, rural and remote areas. The recent (2020) Health Workforce Queensland minimum dataset reports only 53% of rural Queensland’s medical workforce was trained in Australia2, meaning nearly half are trained overseas. Numerous other factors are contributing to rural and remote medical workforce shortages in Australia, including a lack of medical schools based outside of metropolitan areas, relatively few medical curricula focusing on teaching specific skills for rural or remote practice, and the realities of practising in geographically isolated and environmentally challenging rural and remote areas3,4.
James Cook University (JCU) was the first medical school in Australia to be based outside of a metropolitan area. The main campus is in Townsville, North Queensland, with a distributed network of clinical schools and other teaching sites across the north Australian region. JCU enrolled its inaugural MBBS cohort in 2000 with a mission to address the needs of North Queensland communities. These include the five northern hospital and health service (HHS) districts of Torres and Cape, Cairns and Hinterland, Townsville, Mackay and North West Queensland, as well as communities in the Central Queensland and Central West HHS districts, where JCU ‘shares’ some undergraduate student placements with other education providers. JCU’s student selection process is an integral component in realising this mission, with selection orientated toward local applicants from North Queensland and others with rural, remote and/or Indigenous backgrounds. Indeed, the school’s tracking database shows over 57% of graduates come from North Queensland communities at their time of application to the JCU medical school, and 74% from non-metropolitan areas in general.
JCU’s 6-year undergraduate program is also focused on producing a workforce experienced, motivated and trained to practise in northern Australian communities. The curriculum has significant rural, remote, Indigenous and tropical health content, and includes 6 weeks of general practice placements and at least 20 weeks of rural and remote community placements for all students, undertaken mostly in northern Australia. Since 2016, JCU has also offered postgraduate training in general practice and rural medicine as part of the Australian General Practice Training Program. JCU General Practice Training covers almost all of Queensland except for the south-eastern corner and forms another important part of the pathway to non-metropolitan practice.
The targeted selection process, the extensive rural placement experiences and the curriculum focused on local health issues and developing fit-for-purpose clinical skills all appear to be influencing later graduate practice in the intended areas. The JCU medical school’s tracking database shows that, in 2019, JCU graduates were practising in half of the 80 towns within the five North Queensland HHS and Central Queensland and Central West HHS districts having a hospital and/or medically led medical centre (Fig1). Many JCU graduates are also practising in regional, rural and remote areas of Australia outside of these Queensland HHS districts (Fig2). However, it is unclear which aspects of the selection process, curriculum, clinical placements, and later postgraduate experiences are driving these promising rural medical workforce outcomes.
The year 2020 marked the 20th anniversary of the first student enrolments in JCU’s innovative rurally focused medical education program and 15 years since the first graduating cohort. This study describes the JCU medical school’s graduate practice location and career outcomes for the first 10 cohorts (postgraduate years (PGY) 5–14), with a focus on identifying the key underlying demographic, selection process, curriculum and postgraduate training factors associated with mid-career practice in regional, rural and remote areas of Australia.
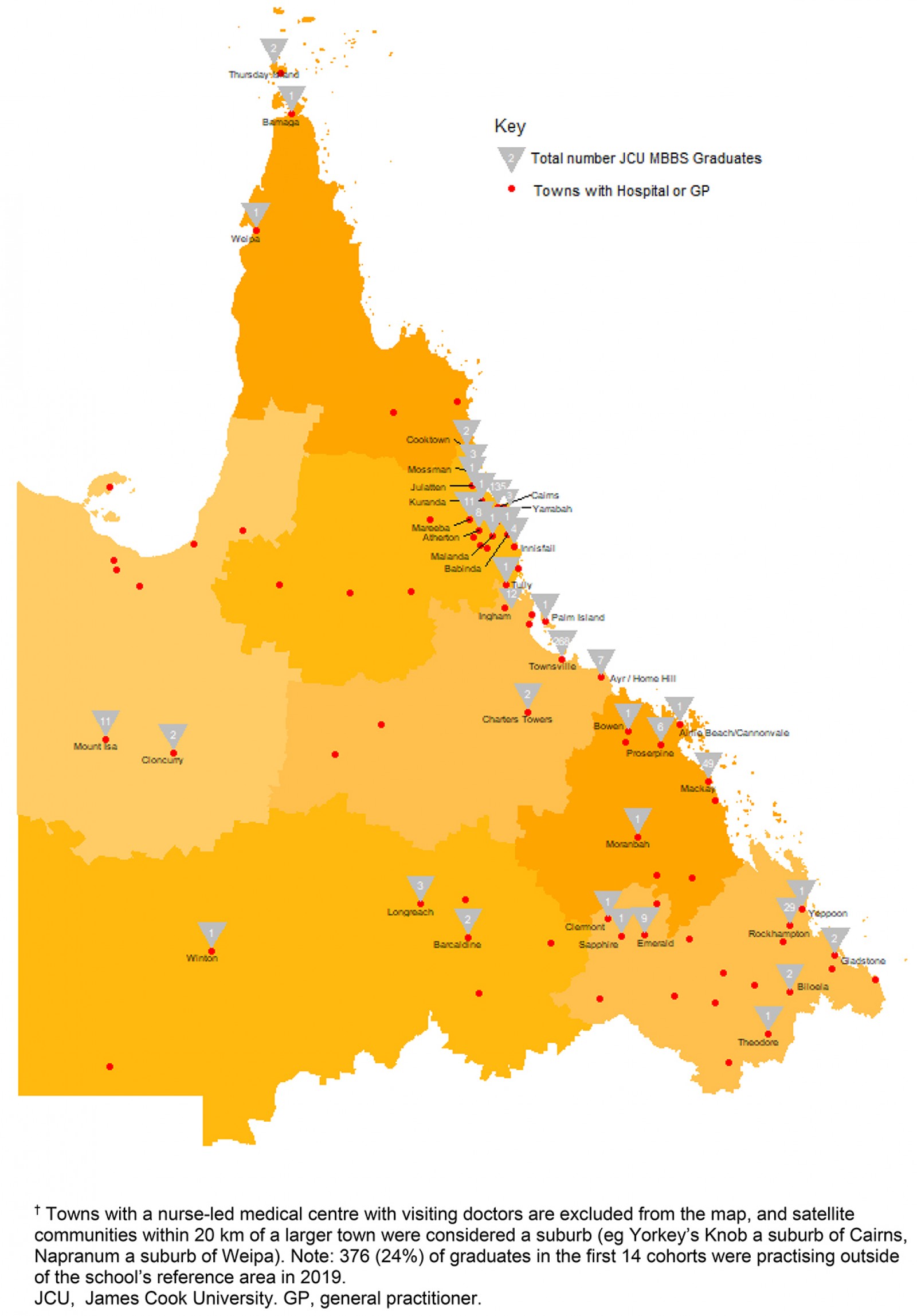 Figure 1: Practice locations and practitioner numbers (2019) for 1217 JCU medical graduates from the first 14 cohorts across James Cook University medical school’s reference area of North and Central Queensland (the five north Queensland hospital and health service (HHS) districts, as well as Central Queensland HHS, and Central West HHS) in towns with a hospital and/or medically led medical centre (red dots).†
Figure 1: Practice locations and practitioner numbers (2019) for 1217 JCU medical graduates from the first 14 cohorts across James Cook University medical school’s reference area of North and Central Queensland (the five north Queensland hospital and health service (HHS) districts, as well as Central Queensland HHS, and Central West HHS) in towns with a hospital and/or medically led medical centre (red dots).†
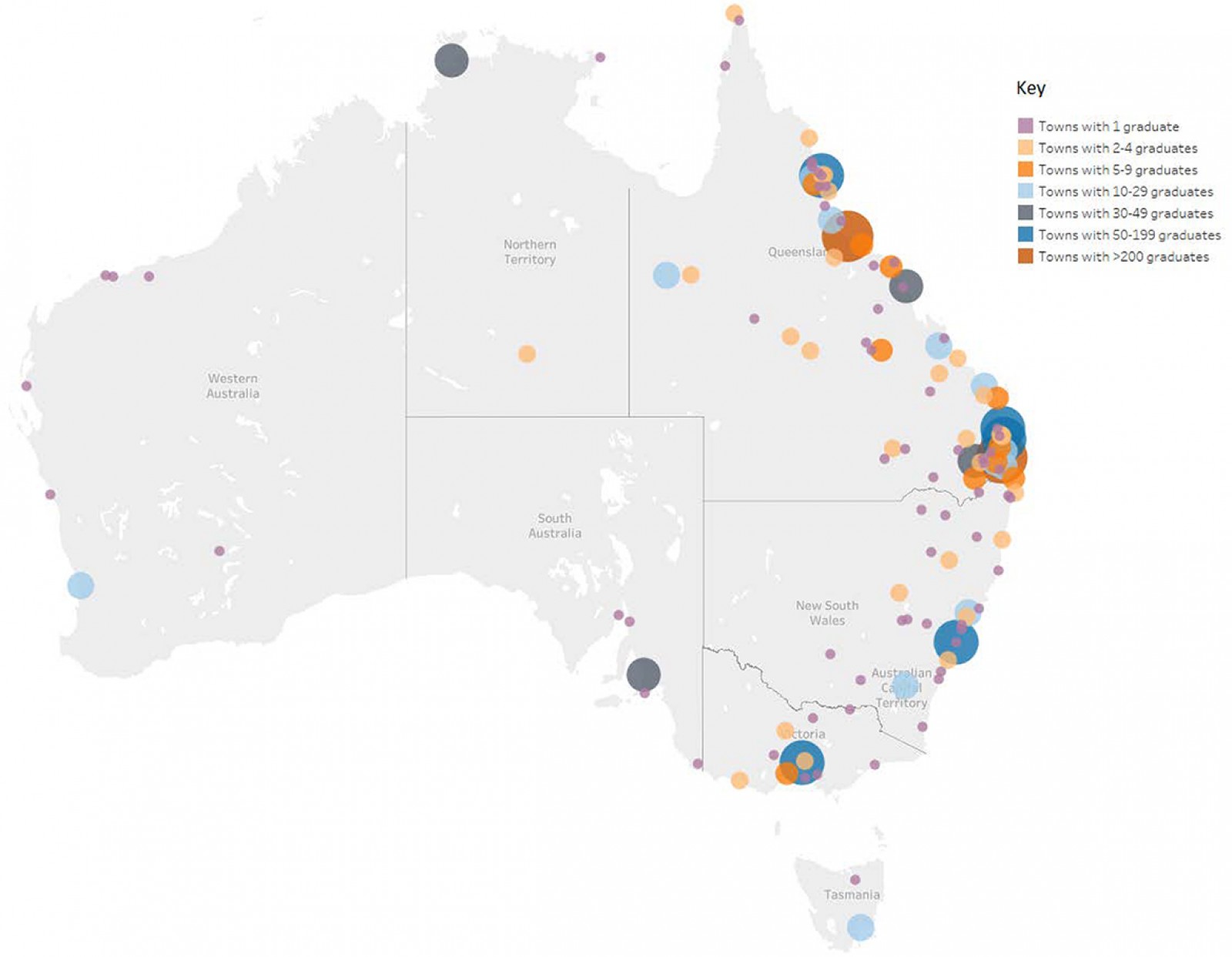 Figure 2: Map of Australian cities and towns where the first 14 cohorts (n=1593) of James Cook University medical graduates were practising.
Figure 2: Map of Australian cities and towns where the first 14 cohorts (n=1593) of James Cook University medical graduates were practising.
Methods
Design
The JCU MBBS program has now produced 16 graduate cohorts from 2005 to 2020. This analysis of practice location and career data for the first 10 cohorts is part of a larger longitudinal cohort study to provide information about JCU MBBS graduate outcomes. This particular study focuses on graduates who have reached PGY5+, where many have chosen their specialty career paths and are becoming more stable in their practice location.
Participants and data sources
In 2019, a total of 900 JCU MBBS graduates had reached PGY5 (ie the 2005–2014 graduating cohorts) and had a known practice location in Australia during 2019. Excluded from the analysis were a further 29 who were practising internationally or had leave (eg maternity leave), and two who were deceased. This study therefore represents 97% of graduates over the first 10 cohorts. JCU medical graduate practice location data were accessed from the medical school’s longitudinal graduate tracking database5, which primarily sources practice location data yearly from the Australian Health Practitioner Regulation Agency (Ahpra) for which the JCU medical school is a current user of the multiple registration checks service. The selection of PGY5+ graduates as the beginning of mid-career was based on observed changes in JCU medical graduate practice location rurality across cohorts 1–14 (Fig3), which shows more stable patterns of practice location rurality from PGY5 – as for most Australian medical graduates, the first few years after graduation are usually undertaken in large teaching hospitals.
The tracking database contains demographic factors (including age, gender, hometown at entry, Indigenous status, rurally bonded scholarships awarded at entry or during the course, awarded advanced standing (ie entry at year 2 or later), experiences throughout the course (clinical school attended, undertaken extended rural placements) as well as postgraduate factors (location of internship, specialisation, undertaken the postgraduate JCU GP training program).
The DoctorConnect website was accessed online from the Australian Government Department of Health to identify the Modified Monash Model (MMM) classification for the practice location. The MMM is a widely accepted system for classifying metropolitan, regional, rural and remote areas according to geographical remoteness and town size. The MMM has seven rurality categories (Table 1).
Specialty career choice was determined primarily using the Ahpra multiple registration checks service, which lists fellowships awarded in both overall specialty (such as general practice, surgery, anaesthesia and as a physician) and specialty field (such as general surgery, general medicine, neurosurgery and urology). A general practice speciality field was categorised into ‘general practitioner’ or ‘rural generalist’ depending on fellowship obtained (Fellowship of the Royal Australian College of General Practitioners, Fellowship of the Australian College of Rural and Remote Medicine or Fellowship in Advanced Rural General Practice). Categorisation into ‘generalist specialist’ or ‘specialist’ career choice was undertaken based on the 2012 Australian Medical Association position statement ‘Fostering generalism in the medical workforce’6, which notes that a generalist specialist retains a broad and undifferentiated scope of practice (eg emergency medicine, obstetrics and gynaecology, general physician, general surgeon, general paediatrics). However, if no specialty data were listed for any JCU graduate in the first 10 cohorts, an internet search was conducted to identify any further graduates reported as advanced trainees or registrars in a specialty training program, or working in a general practice without a general practice fellowship, and these were categorised accordingly. Those found on the internet designated as a junior house officer, senior medical officer or principal house officer were categorised as hospital non-specialists.
Table 1: The seven rurality categories of the Modified Monash Model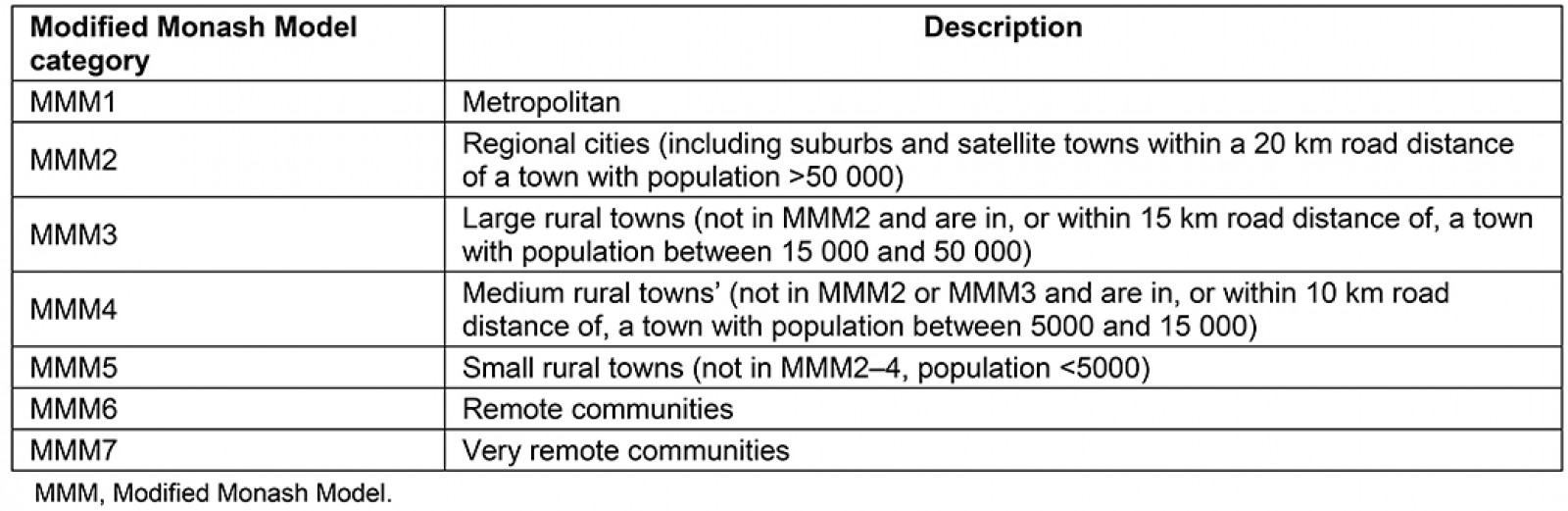
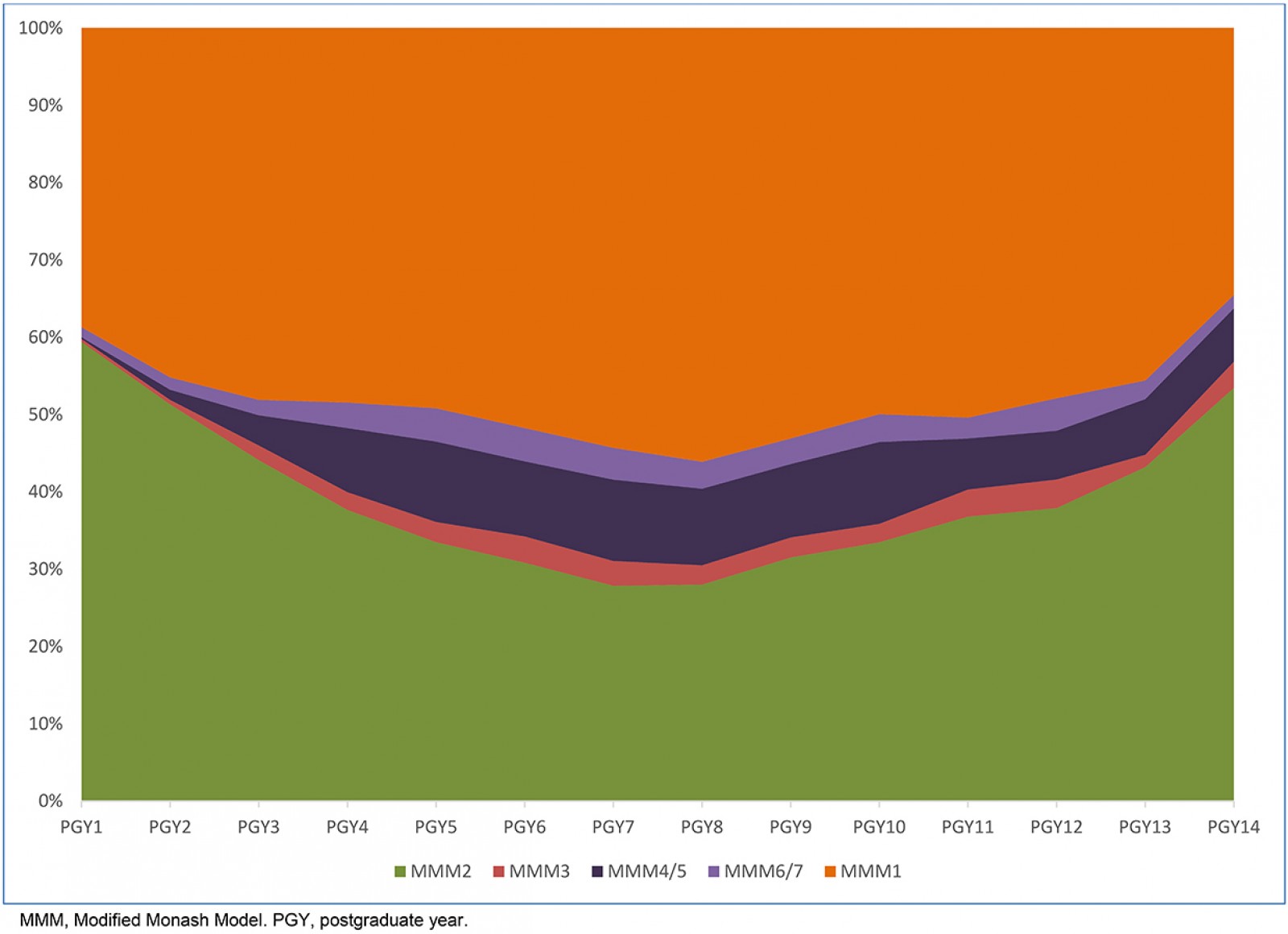 Figure 3: Rurality of main practice location (Modified Monash Model categories) for the first 14 cohorts of James Cook University medical graduates (n=1593).
Figure 3: Rurality of main practice location (Modified Monash Model categories) for the first 14 cohorts of James Cook University medical graduates (n=1593).
Data analysis and statistics
Descriptive analysis was used to describe patterns of practice location rurality across the first 10 JCU graduate cohorts (excluding cohorts 11 onwards because many of these graduates undertook junior doctor training in MMM1–2 teaching hospitals – as evidenced in Figure 3). Bivariate analysis involved multinominal logistic regression to identify individual factors associated with the rurality of the 2005–2014 graduates’ practice location in 2019 (Table 2). Multivariate analysis, also using multinominal logistic regression, was then used to describe all key independent predictors of practising in regional cities (MMM2), rural towns (MMM3–5) and remote communities (MMM6–7) in 2019 (Table 3). Statistical tests were considered significant with p<0.05, while the strength of the association was described using prevalence odds ratios (POR) and 95% confidence intervals (95%CI).
Ethics approval
Ethics approval for the study was obtained from the JCU Human Research Ethics Committee (approval numbers H1804, H3194 and H6921).
Results
Under the MMM classification, the first 10 cohorts of JCU medical graduates’ 2019 practice location rurality included 486 (54.0%) graduates in MMM1 (metropolitan cities), 262 (29.1%) graduates in MMM2 (regional cities), 32 (3.6%) graduates in MMM3 (large rural towns), 94 (10.5%) graduates in MMM4–5 (medium or small rural towns), and 26 (2.9%) graduates in MMM6–7 (remote communities). Most of the graduates practising in MMM2 areas were located in the four largest northern Australian cities: Townsville (n=121), Cairns (n=56), Mackay (n=17) and Darwin (n=14). The first 10 cohorts were found to have chosen careers in general practice (n=300, 33%), rural generalism (n=96, 11%), as generalist specialists (n=87, 10%), subspecialists (n=217, 24%) or hospital non-specialists (n=200, 22%).
Individual demographic, selection process, curriculum and postgraduate training factors associated with the 2005–2016 JCU MBBS graduate cohorts having MMM2, MMM3–5 and MMM6–7 practice locations in 2019, compared to JCU graduates practising in MMM1, are described in Table 2.
Statistically significant, independent predictors of 2005–2016 JCU MBBS graduates having an MMM2 practice location (ie in a regional city) in 2019 were graduation from JCU General Practice Training (p<0.001, POR=5.0), internship training in a hospital in a regional city (p<0.001, POR=3.6), hometown at application to the medical school being a regional city (p<0.001, POR=2.6) or rural or remote town (p=0.033, POR=1.8), and choosing a career in general practice (p=0.010, POR=1.9) or as a generalist specialist (p=0.011, POR=2.2) (Table 3).
Statistically significant, independent predictors of JCU MBBS graduates having an MMM3–5 practice location (ie in a rural town) in 2019 were being awarded an Australian Government undergraduate Medical Rural Bonded Scholarship (MRBS) (p=0.004, POR=3.5), graduation from JCU General Practice Training (p=0.001, POR=3.9), internship location in a regional city (p=0.003, POR=2.4) or in a rural or remote town (p=0.033, POR=5.0), hometown at application to the medical school being a rural or remote town (p=0.021, POR=2.5, and choosing a career in general practice (p<0.010, POR=4.4) or as a rural generalist (p<0.001, POR=26.4) (Table 3).
Statistically significant, independent predictors of JCU MBBS graduates having an MMM6–7 practice location (ie in a remote community) in 2019 were being awarded an Australian Government undergraduate MRBS (p=0.017, POR=7.3), graduation from JCU General Practice Training (p<0.001, POR=20.1), undertaking an extended 20- or 35-week undergraduate placement in a rural or remote town during year 6 (p=0.014, POR=8.9), and internship training in a hospital in a regional city (p=0.049, POR=4.3) or in a smaller regional, rural or remote town (p=0.002, POR=54.6) (Table 3).
Table 2: Demographic, undergraduate and postgraduate predictors for 900† James Cook University MBBS graduates having a 2019 practice location in MMM2, MMM3–5 or MMM6–7 areas, with MMM1 being the reference category (Modified Monash Model classification)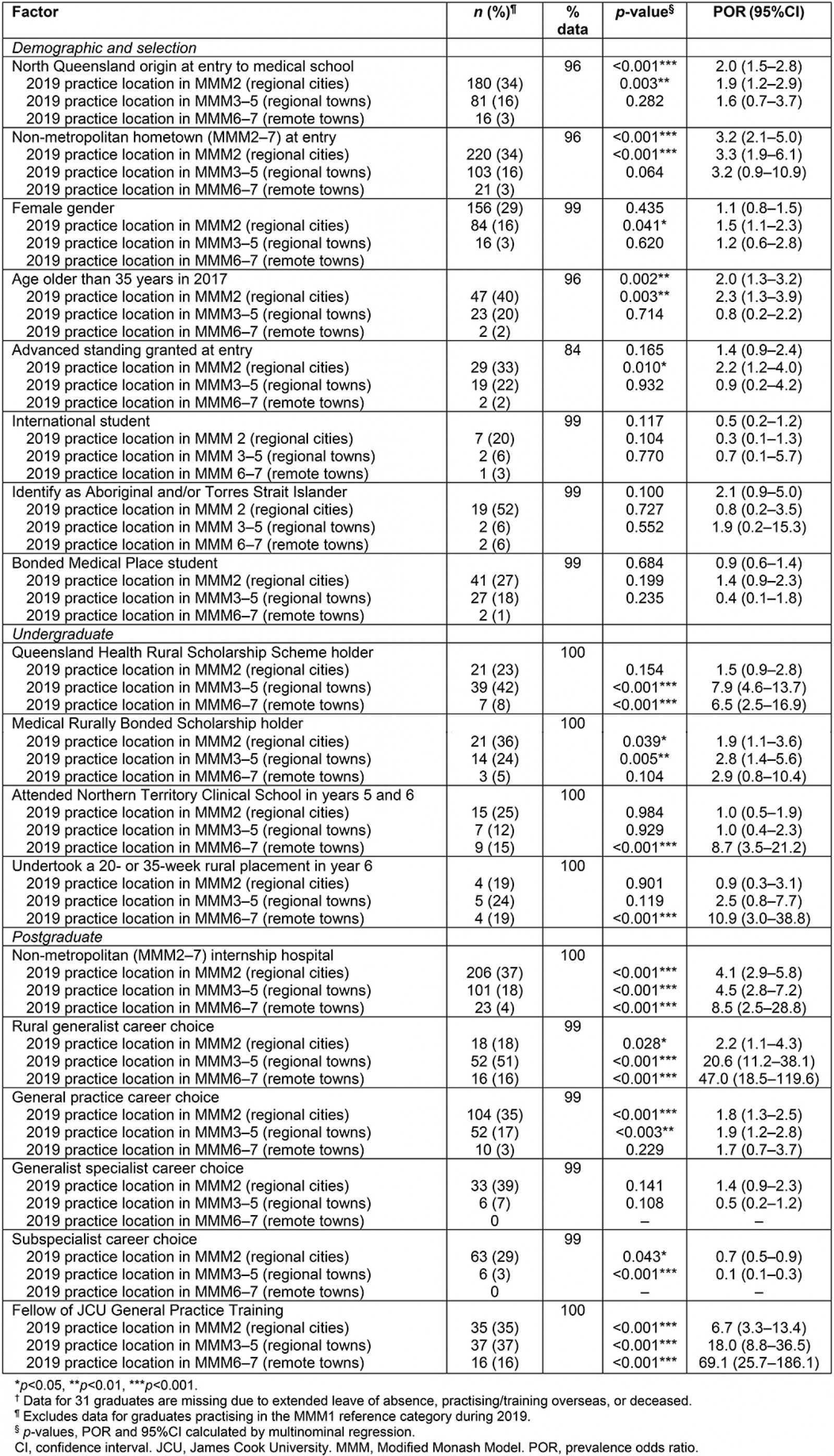
Table 3: Multinominal logistic regression analysis describing independent predictors of James Cook University MBBS graduates (2005–2014) having a 2019 practice location in MMM2, MMM3–5 or MMM6–7 areas, with MMM1 being the reference category (n=826†, with 433 practising in MMM1 locations)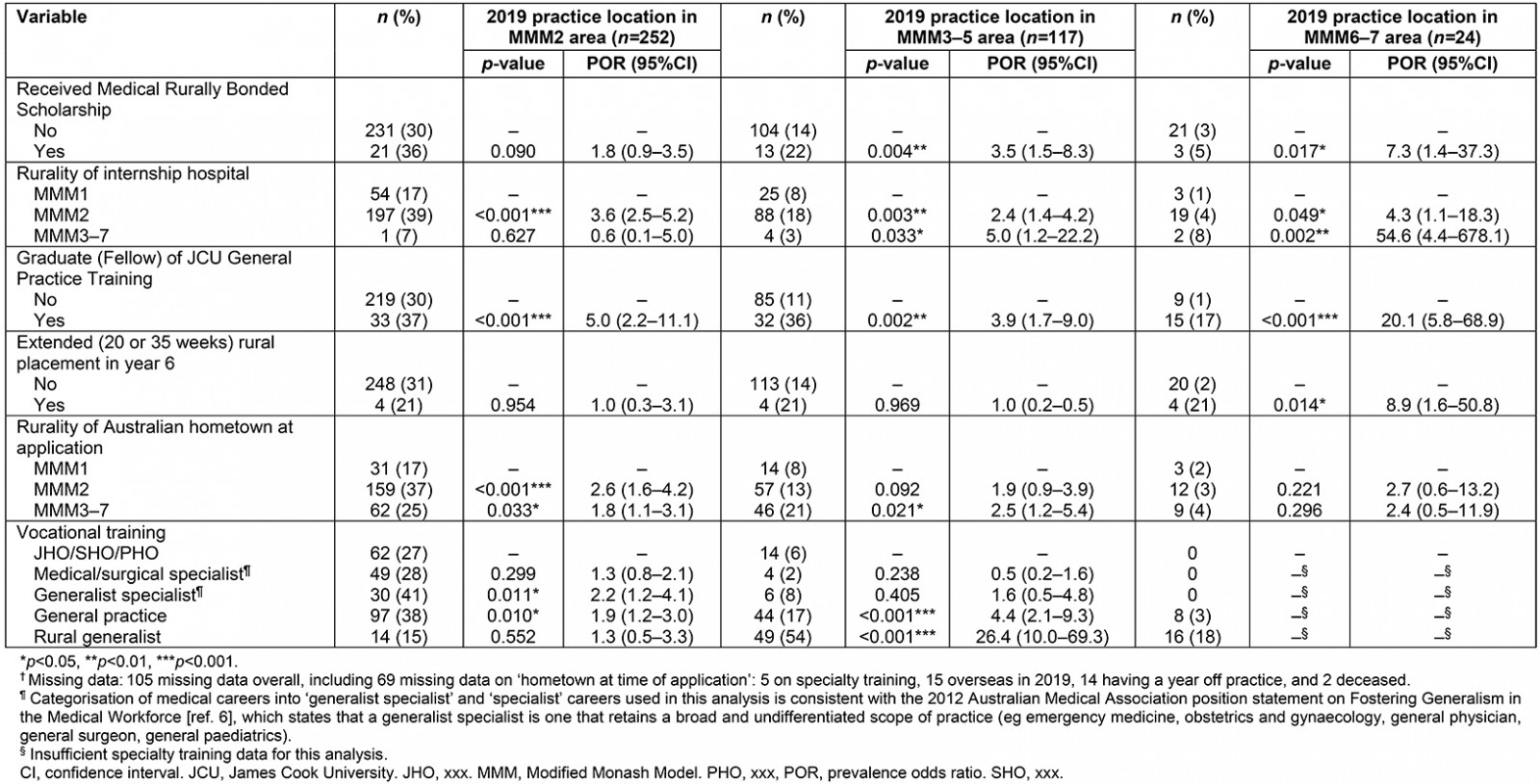
Discussion
This summary of graduate outcomes for the mid-career JCU medical cohorts shows very positive graduate practice outcomes for PGY5+ for the large regional cities of northern Australia: Townsville, Cairns, Mackay and Darwin. Indeed, the National Health Workforce Australia dataset shows the proportion of JCU medical graduates working in regional areas (29%) in 2018 is significantly higher (p<0.001) than the proportion of graduates from all Australian medical schools (9.2%)7. The proportions of JCU MBBS graduates practising in rural (MMM3–5) and remote (MMM6–7) towns are significantly more than graduates from all Australian medical schools in the 2018 National Health Workforce Australia dataset: 14.1% versus 10.4% (p=0.003) and 2.9% versus 1.3% (p<0.001), respectively. Of note, the proportions of PGY5–14 JCU MBBS graduates practising in rural (MMM3–5) and remote (MMM6–7) towns are very similar to the proportions of the overall Queensland population living within these rurality categories: 14.1% versus 14.6% and 2.9% versus 3.0%, respectively (derived by the National Rural Health Alliance (personal communication), based on 2011 Australian Census data linked to the percentage of the population in each state and MMM zone). In other words, the proportion of JCU graduates working in smaller, more remote locations reflects the Queensland population distribution. Similarly, 20% of Queensland’s population live in MMM2, where 29% of JCU graduates in this study practise, reinforcing the non-metropolitan pattern of workforce distribution.
Over half of PGY5–14 graduates have also chosen to become general practitioners, rural generalists or generalist specialists. There is growing evidence that health systems having a generalist orientation consistently achieve a better and more equitable distribution of health outcomes across the population, regardless of patient socioeconomic and geographic constraints7-13, and help curb the rise in healthcare costs through greater integration and less expensive services per individual and per visit14. Of particular relevance to the rural and remote context is the evidence that a primary care-oriented workforce can help to prevent and manage the growing burden of chronic disease in poorer and/or more rural community settings15, as well as better address the needs of ageing populations with growing multi-morbidities16.
Thus, these 2019 mid-career practice location and specialty career data make a strong case that JCU graduates are having a significant impact across a high proportion of communities within the JCU medical school’s reference area of North, North West, Central and Central West Queensland. Although positive, these findings do argue for more investment in undergraduate and postgraduate training posts across more rural and remote Queensland towns for these regions to more equitably benefit from the increasing supply of JCU graduates.
It is worth noting that practice location and even career specialty are often not up to ‘pure’ graduate choice, but may also be driven by a range of personal and professional factors. Many trainees are subject to constraints of specialty college entry conditions, training requirements and job availability, all which may be further exacerbated by historic patterns of maldistribution. This is particularly true for Australian postgraduate vocational training positions in medical and surgical specialties, which are typically located in metropolitan areas, with relatively few in rural and remote towns17. In addition, the majority of specialty colleges do not have any rurally focused selection criteria – potentially disadvantaging applicants who have or want to have rural experience18.
In addition to confirming positive regional, rural and remote medical workforce outcomes from mid-career JCU graduates, the findings from the multivariate analysis also identify the specific selection process, demographic, undergraduate training and postgraduate factors that affect the likelihood of mid-career JCU graduates choosing non-metropolitan practice. Some of these can be influenced by the JCU medical school, although a number are somewhat more distal – outside the school’s direct control. The significant proximate factors over which the JCU medical school has some control include the age of an applicant, hometown in a regional or rural area of Australia at time of application to the medical school, and two recent rural training programs: JCU General Practice Training and the extended (20 or 35 weeks) undergraduate rural placements in year 6.
JCU has an undergraduate-only medical program, accepting more than 90% of applicants directly from secondary school, and has developed a selection process designed to identify candidates best suited to the program. For example, the selection process gives preferential weighting to applicants who identify as Aboriginal and/or Torres Strait Islander, and those from northern Australia and/or with a non-metropolitan background, as well as how well applicants’ values, personal characteristics and intentions align with the values of the school19. While applicants from metropolitan and international backgrounds are accepted if they score well on communication skills, personal resilience, and values based on community service and intentions towards rural practice, over half the sample (57%) in the present study are from northern Australia, and three-quarters (74%) are from rural areas from outside Australian urban areas.
Having an appropriately targeted selection process is an established predictor of subsequent practice20-23. Indeed, the multivariate analysis findings show choosing applicants from rural areas of Australia (MMM3–7) is a key independent predictor of later practice in both regional cities (p=0.033, POR=1.8) and rural communities (p=0.021, POR=2.5). Also selecting applicants from around Australia and the world for their values related to community service has the additional benefit of enhancing the diversity of the student body. The school hopes this geographically and culturally diverse student body with common values toward community service and rural practice will have positive influences on all students, and that graduates will see all patients as equal, regardless of background, when they begin their clinical practice.
Involving predominantly small rural or remote towns, the school’s year 6 extended rural placement programs – the 20-week integrated rural placement and 35-week longitudinal integrated clerkship – were found to be associated with later rural or remote practice (p<0.001, POR=5.6). Although this is a strong finding, these extended rural programs have only been running since 2012, with limited student uptake in the early years (28 graduates from 2012 to 2016), although they are becoming more popular. While small numbers precluded direct comparison of these two programs in the present study, this will be subject to future analysis.
The success of the extended undergraduate rural placement programs in promoting rural and remote practice is not unexpected. Many rurally interested students will self-select, and the length and intensity of community-based placements has previously been shown to be an important factor in the later recruitment and retention of medical graduates in underserved areas24-29, as well as with a later career in primary care29,30. Research has also shown extended rural or urban clinical placements have advantages over much shorter hospital-based clinical blocks with respect to improved academic results31-33, enhanced patient-centredness31,32, greater exposure to common conditions34, more meaningful learning relationships with patients and academic mentors35, quality of student feedback36, and enhanced social connectedness through the establishment of professional and community networks and community involvement24,37,38.
This study also demonstrates the positive outcomes from JCU General Practice Training for regional, rural and remote medical workforce. JCU General Practice Training was established in 2016 to provide postgraduate training for general practice and rural generalist medicine across all of Queensland excluding the south-eastern corner, and to provide relevant education, support and career advice. Previously, postgraduate general practice training in Australia has been outside the control of medical schools. The findings of this study show graduation from JCU General Practice Training as a Fellow of the RACGP or ACRRM is significantly associated with regional (p<0.001, POR=5.0), rural (p=0.002, POR=3.9) and remote practice (p<0.001, POR=20.1), suggesting this recent innovation will become increasingly valuable in promoting the numbers of JCU and other medical school graduates choosing a rural or remote career.
This study also shows there are key factors predicting rural and remote practice that the JCU medical school cannot control, such as being awarded Australian Government undergraduate MRBSs (POR 3.5 and 7.3, respectively). Undertaking internship in a regional or rural/remote hospital also positively predicts both rural (POR 2.4 and 5.0, respectively) and remote practice (POR 0.3 and 54.6, respectively). Lastly, choosing a career either in generalist specialist medicine or general practice both positively predicted regional practice (POR 2.2 and 1.9 respectively), while choosing a career in general practice or rural generalism positively predicted rural practice (POR 4.4 and 26.4, respectively). Together, these findings argue for having adequate intern places available across underserved regions like North Queensland, especially in more rural and remote hospitals. Currently, relatively few internship places and short-term rotations are available in MMM3–7 hospitals across this region. As a result, many medicine graduates pursuing specialist careers become lost to northern Australia due to colleges requiring the majority of training in large metropolitan teaching hospitals, with far fewer positions available in northern Australia both during and after fellowship training.
In an attempt to overcome this issue of losing graduates due to vocational college training requirements, funding has recently been obtained to improve retention and recruitment of JCU and other Australian PGY2+ junior doctors for specialist training in North Queensland hospitals. Similar to the JCU General Practice Training, but with a focus on hospital-based specialist practice, Northern Queensland Regional Training Hubs was established in 2016 across six Queensland districts (Cairns, Townsville, Mackay, Torres and Cape, North West and Central West) to provide an ‘integrated pipeline of medical training across the training continuum that provides a high quality, self-sustaining medical workforce responsive to the health needs of northern Queensland’39. Northern Queensland Regional Training Hubs is one of several regional training hubs established across Australia to better coordinate regional hospital training opportunities for medical students and build local medical graduate training capacity in non-metropolitan hospitals, as well as support additional places on specialist training programs targeted specifically toward non-metropolitan practice40.
Overall, of the key factors identified by the current study as predicting JCU medical graduates’ current rural and remote practice, one has been under the direct control of the medical school since inception (preferential selection of non-metropolitan students), two are relatively recent (JCU General Practice Training and the extended undergraduate rural placement programs), while the remaining three are outside of the direct control of the school (Australian Government undergraduate MRBS, undertaking internship in non-metropolitan hospitals, and choice of postgraduate vocational training). While this analysis of the first 10 JCU graduating cohorts shows positive outcomes for North, Central and North West Queensland communities, it is hoped that the postgraduate JCU General Practice Training and the year 6 extended rural programs, along with the more recent innovation of Northern Queensland Regional Training Hubs and the increasing clinical experience of the cohorts, will further improve the practice outcomes of JCU graduates in the more rural and remote areas of northern Australia over time.
Limitations
The database is mostly complete; for example, ‘postgraduate practice location in 2019’ has approximately 1% of data missing. However, the 74 missing data on ‘hometown at application to the medical school’ may be a limitation for the multivariate analysis model, as this accounts for an overall 8% reduction of graduate data in the model. Another limitation of this study is that the findings are specific to JCU medical graduates, as the nature of the JCU MBBS program – an undergraduate course that preferentially selects students with a rural background – is not representative of all medical students or graduates across Australia. In addition, student hometown was self-defined as ‘your hometown at application to medical school’, which may not always reflect where students had spent the majority of their life before medical school.
Additionally, while care has been taken to ensure the accuracy of graduate destination data of the JCU medical school’s first 10 cohorts, it has been collected from a variety of sources, with the majority of graduate practice location data now being obtained from the Ahpra website, which, based on correlations between data from this website and data from personal contact, is estimated to be around 90% accurate41.
Another possible limitation is the arbitrary selection of PGY5 as the beginning of a graduate’s mid-career. Many graduates are already on a career path at this point as evidenced by the stability of graduate practice locations from PGY5 for the overall cohorts (Fig3), so this was felt to be a reasonable choice. However, in specialty training, practice locations are often determined by the training college rather than graduate choice. Of note, by PGY5, many of those training as a general practitioner or rural generalist are no longer working in hospitals as they would at PGY3.
Furthermore, year 6 medical students can self-select into the undergraduate extended rural placements, internships in rural and remote hospitals, and the postgraduate JCU General Practice Training. Thus, their increased likelihood of practising in a remote location may be more influenced by prior motivation for remote practice rather than from their additional rural and remote placement experiences. However, a recent study at the JCU medical school has identified that later remote practice outcomes from students undertaking an extended rural placement were a combination of influences from both a prior motivation for rural practice and the extended placement experiences42, and similar combinations may also exist for postgraduate rural internships and the JCU General Practice Training.
Specialty choice was mostly based on fellowship data from Ahpra with an internet search conducted for any graduate not recorded as obtaining a fellowship. However, it is not possible to verify the accuracy of this information. Some graduates may subsequently change their career choice (in particular, from junior house officer/senior house officer/principal house officer to ‘advanced trainee’ or ‘registrar’ in a specialty training college), while others may have obtained a fellowship not listed on the relevant website.
Conclusion
The JCU medical school outcomes are strongly positive in regards to producing graduates who choose generalist medicine and later practise in regional Queensland cities. Outcomes are also positive for producing graduates who choose to practise in smaller regional, rural and remote towns, with the number of JCU graduates practising in smaller rural and remote towns representative of the overall Queensland population distribution. Graduates are currently based in 50% of all North and Central Queensland towns having a hospital and/or medically led medical centre. These findings argue for more investment in undergraduate and postgraduate medical training posts across North and Central Queensland so these regions can more equitably benefit from the increasing supply of JCU graduates.
Further, the JCU medical school’s extended undergraduate rural training programs and the postgraduate JCU General Practice Training are showing positive early results in improving rural and remote generalist medicine practice outcomes across northern Australia. Additional government measures such as the Northern Queensland Regional Training Hubs initiative will also be important to support and advocate for increased intern places in non-metropolitan hospitals, and in establishing more local training places for JCU and other medical school graduates who wish to train in generalist specialist or subspecialist pathways across north Queensland hospitals.
This study adds to the understanding of predictors of medical graduates’ non-metropolitan practice from the first of Australia’s ‘new’ medical schools by providing evidence from a near-complete dataset containing actual career and location data. This data also show the importance of health professions schools implementing a systematic graduate tracking process with an analytic database to provide quality information regarding the many nuances in workforce planning, and understanding the importance of all aspects of the training pathways, and their multiple interactions. It further reinforces the importance of all components of the training pathway – every ingredient in the recipe is important – and the need for further investment in regional, rural and remote medical education across the training continuum.



