Introduction
Access to healthcare services is a major rural health issue globally1, with medical resources, including staff, frequently concentrated in urban areas1,2. Healthcare provider shortages in rural and remote areas have resulted2-4 and the WHO estimates a global health worker gap of 18 million by 20305. Specifically, lack of access to health services affects rural and remote Scotland, where 29% of the population resides6,7. Recruiting enough healthcare workers with skills required for rural practice proves challenging7, with general practitioner shortages noted, alongside an ageing GP workforce and retention difficulties8. Targeting rural recruitment issues through medical education, multiple studies show three factors that strongly predict a medical student’s intention to practise rurally: (1) a rural background, (2) positive undergraduate rural clinical rotations, and (3) targeted rural training at undergraduate and postgraduate levels9-13. Medical educational curricula that include rural health issues also create student interest in working rurally9-11,13. Medical education involving immersion in rural communities guided by good role models and curricula that integrate rural content promotes rural recruitment of recent graduates14,15.
Medical schools have a social accountability to their communities16. Canadian research demonstrates that rurally oriented undergraduate programs grounded in social accountability have positive impacts on recruiting and retaining rural practitioners17-19. While some evidence base confirms that curricula components encourage rurally oriented medical students, their mechanism of action is not entirely clear. One possibility is that they alter medical students’ existing perceptions of rural practice; however, little current research explores this.
The University of St Andrews has two medical programs: a BSc Medicine and a graduate-entry MBChB (ScotGEM). The BSc program is an integrated, systems-based three-year BSc Honours degree, with graduates transferring to partner schools to complete their primary medical qualification. The BSc program delivers the scientific basis of medicine via lectures, guided studies or small-group workshops, alongside clinical skills teaching and short placements within primary and secondary care. The ScotGEM program was commissioned to address Scotland’s rural generalist workforce crisis20. The program, Scotland’s first graduate-entry medicine course, runs in partnership with the Universities of Dundee and the Highlands and Islands, and NHS Scotland21. It employs high-quality mentorship and role modelling, and a 40-week immersive longitudinal integrated clerkship (often in rural locations) to achieve its aims. This curricula contrast provides a unique opportunity to explore rural practice perceptions in medical students exposed to different programs. This pilot study examines the perceptions of University of St Andrews’ medical students about rural and remote practice and how these perceptions influence their interest in future rural practice.
Methods
This pilot study deductively applied Feldman and Ng’s ‘Careers: mobility, embeddedness, and success’ framework to the data22. The framework assesses factors that motivate and encourage workers to change careers or occupations. Findings were assimilated into six perspectives influencing career mobility to explore the usefulness of the framework’s application to this novel context (see Table 1).
Sample
The sample included 10 participants from University of St Andrews BSc and ScotGEM medical education programs, recruited through online advertisements and snowballing. The recruitment strategy aimed to enhance variation in rural and remote practice intention, geographical backgrounds, gender and career interests. Researchers assumed that the type of student who studied at the University of St Andrews was a preselected group. Sufficient homogeneity of perceptions related to practising rurally was expected to be reached with this sample size.
Data collection and analysis
Semistructured interviews with participants took place between June and July 2020; they explored themes around geographical and familial history, perceptions of practising rurally, lifestyle preferences, education, and future career intentions. Pre-interview, participants provided a diary response, informing the researcher’s initial questions. The researcher audio recorded and transcribed all interviews, then generated codes within Feldman and Ng’s theoretical framework22. These were discussed among the research team to finalise them. The different research perspectives (development practice, medical education and rural primary care) in the research team created a robust and reflexive process. Transcripts were coded using NVivo v12 (QSR International, 1999, https://qsrinternational.com/nvivo/nvivo-products).
Ethics approval
The Graduate School of Interdisciplinary Studies Ethics Committee at the University of St Andrews approved the research protocol (GS14941).
Results
For information on participants’ courses and intention to practise rurally, see Table 2. Interviews informed several key perceptions among medical students regarding rural practice within the Feldman and Ng framework, detailed in Table 1. An additional conceptual theme was generated to highlight the perceived mechanisms through which educational experiences informed these perspectives22.
Structural/organisational perspective
Participants noted that rural patients’ geographical isolation impedes convenient access to urban-located specialised or secondary care. This was especially concerning for doctors in areas with older patients and limited public transport (ScotGEM6 (1)). Supporting quotes for all subthemes are detailed in Table 3.
Participants perceived limited resource provisions, including technology, in rural health care, deterring some from rural practice. Others perceived that rural physicians took on more roles. One participant mentioned the use of virtual consultation platforms as an alternative to increase rural areas’ connectivity to urban hubs (ScotGEM4 (1)). All participants perceived that rural settings have fewer staff than urban locations, leaving rural physicians without additional support to check their work. This lack of support meant rural clinicians had greater responsibility (Occupational perspective theme), which was positively viewed by some (BSc4 (1)).
Occupational perspective
Participants perceived the urgent need for more rural generalist clinicians, and many were excited by the role’s versatility (ScotGEM4 (2)). Most students defined urban-style, secondary care specialists as having more depth of focus in a specific aspect of medicine, making them impractical members of the rural health workforce (BSc2). Most ScotGEM participants understood that rural generalists could subspecialise in an area of interest. Perceptions concluded that generalists could explore parts of medicine in depth, while providing broadly needed general services in rural communities (ScotGEM3). Educational experience, including exposure to generalist tutors, informed these views.
The uncertainty of ‘not knowing what will come through the door next’ and learning a wider array of skills as a generalist was favourably perceived by some participants. This adaptation to handle uncertainty was perceived as a learned behaviour, established during GP placements through the hidden curriculum (subconsciuosly transmitted information such as attitudes and beliefs), and reinforced by positive role modelling (ScotGEM6 (2)). In addition, working in isolation, with the particular expectation to respond to any undifferentiated emergency presentation, is perceived as a rural generalist’s responsibility (ScotGEM2).
Working group perspective
Most participants commented that a rural medical practice is unable to perform additional tasks because of limited staff, a smaller physician-to-patient ratio, and the increased time required to deliver services in rural areas. Some participants stressed the importance of social support within the workplace (BSc3). Some participants perceived a more relaxed medical hierarchy in rural settings, meaning teamworking was easier. While some perceived urban hospitals as a natural environment for teamwork, others perceived urban hospitals as competitive workplaces, constrained by the hierarchy of medicine (ScotGEM1 (1)).
Personal life/personality perspective
Some participants perceived that rural communities observed their physician’s everyday life, while city living allowed physicians to remain anonymous to the population. Others maintained perceptions that rural areas promote ‘tight-knit communities’, wherein residents care for each other (ScotGEM4 (3)).
Curricula changes cannot explicitly address the personality perspective, but admission policies can. Some students stressed the importance of flexibility and adaptability in rural doctors’ handling uncertain environments and cases (ScotGEM6 (3)). Medical students referenced the need to be confident and ‘sure in yourself’ regarding competence and knowledge in rural areas, given the lack of support workers and the increased clinical uncertainty synonymous with working in rural or remote locations. Some students mentioned how the variety of rural medicine is aligned with their personality (BSc1 (1)).
Experience mechanism
The authors developed a mechanism theme to explain the process by which participants viewed how certain experiences shaped their perceptions. For both BSc and ScotGEM participants, education was influential in shaping perceptions of rural medicine.
The BSc undergraduate program provided clinical consolidation blocks to students, exposing them to rural medicine. BSc participants viewed these summer placements positively, some specific rural locations being highly sought after (BSc1 (2)). Clinical consolidation blocks and placements throughout the year appeared to be the only rural medicine exposure for BSc students. Participants did not reference dedicated rural content within teaching. Consequently, specific knowledge of rural healthcare issues and rural medicine was not viewed as ‘core’. Implicitly, future rural practice was not expected in the program (BSc4 (2)).
Conversely, all ScotGEM participants had significant exposure to rural medicine education through lectures, small-group teaching with a dedicated clinical generalist, and rural clinical placements (ScotGEM6 (4)). Students perceived that this generalist education provided practical training and knowledge (ScotGEM1 (2)), along with a realistic view of what rural practice entailed. Participants perceived that the consistency of small-group, immersive learning allowed them to build a relevant foundation in clinical, consultation and procedural skills, while providing exposure to positive rural, generalist role models (ScotGEM5).
Table 1: Feldman and Ng’s six perspectives of career mobility and embeddedness22 and resulting subthemes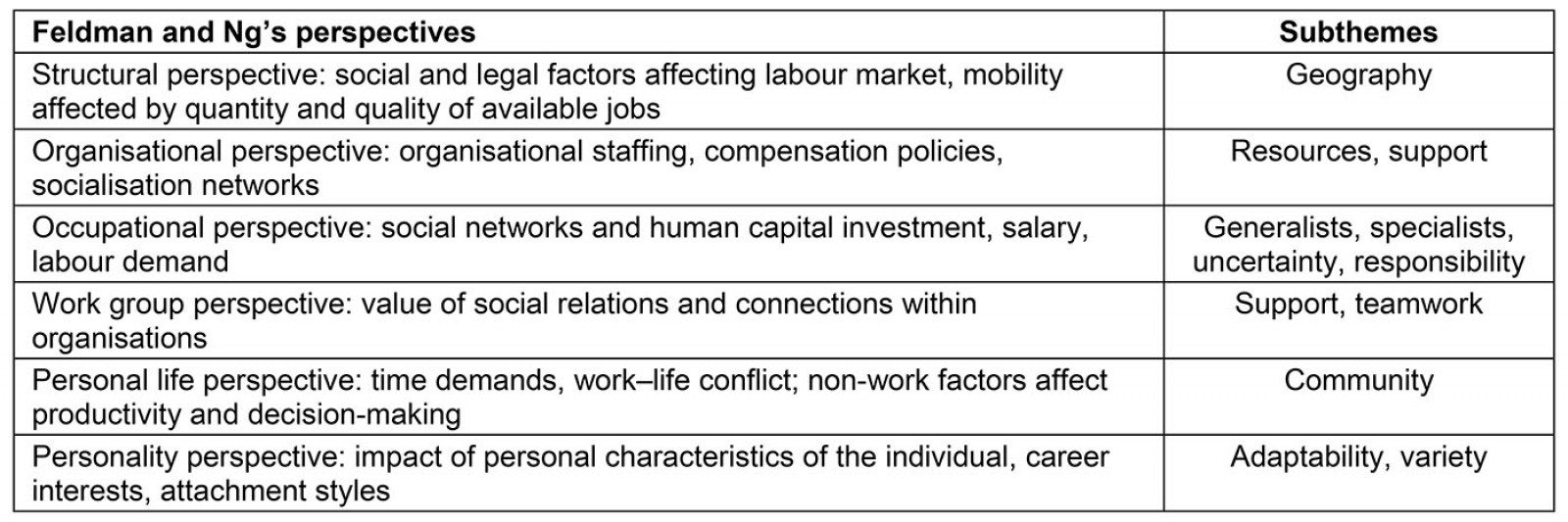
Table 2: Intention to practise rurally by course of study of participants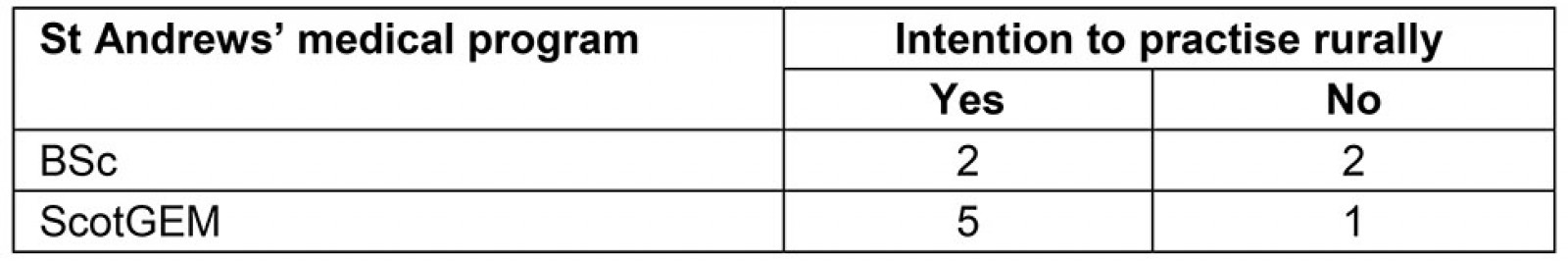
Table 3: Supporting quotes for themes and subthemes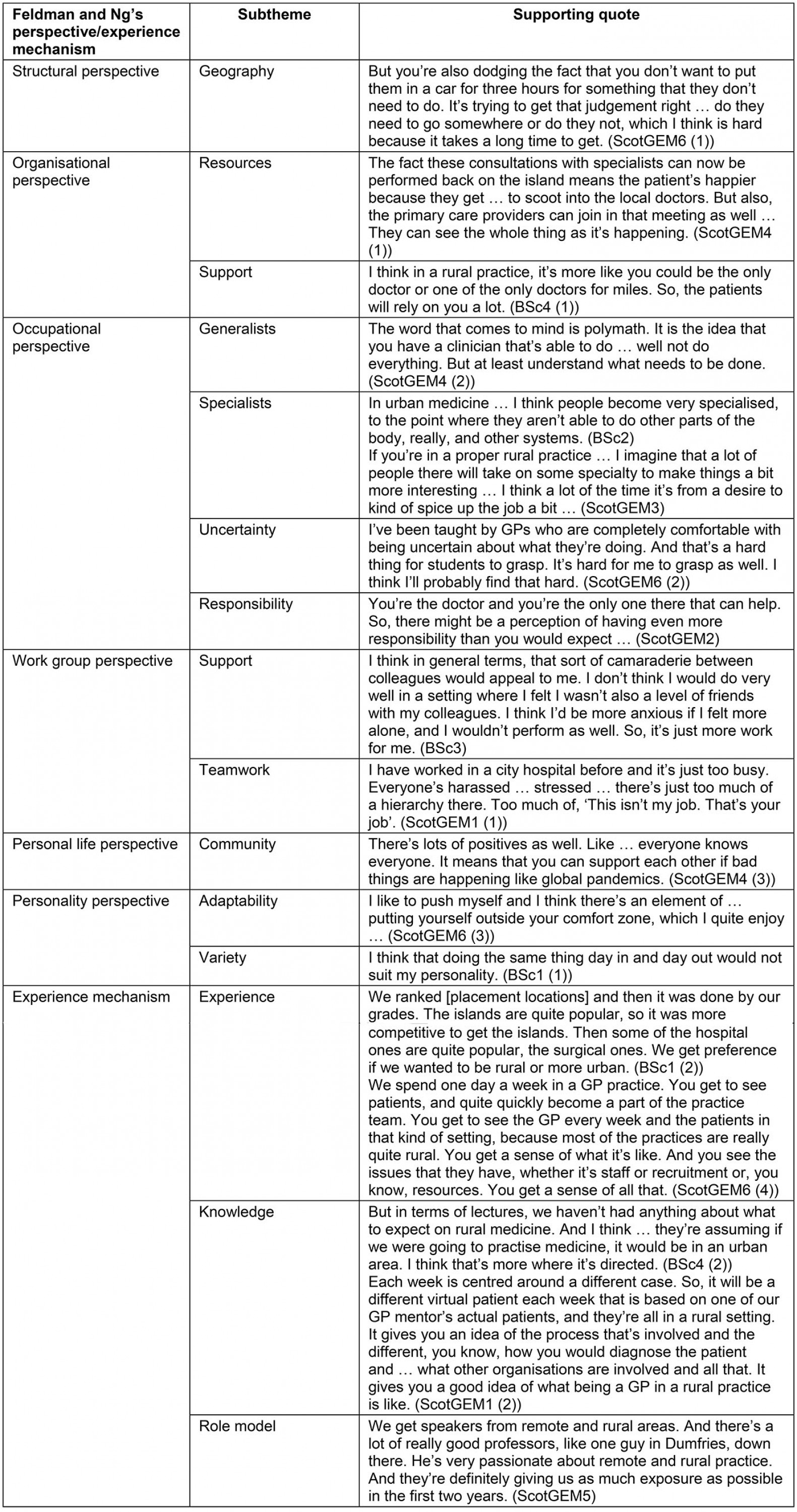
Discussion
Social accountability
Social accountability is defined as ‘an approach … in which citizens participate directly or indirectly in demanding accountability from service providers and public officials23’. Medical schools are obligated to directly address priority health concerns within their local communities16 and to deliver high-calibre education and medical graduates attuned to societal needs24. Mandated by social accountability, community-oriented medical education requires authentic partnerships between health services, academic institutions and local knowledge25. This principle should be at the core of medical undergraduate curricula, particularly in low- and middle-income countries with more pronounced health inequalities.
Examining medical students’ perceptions of rural practice through Feldman and Ng’s career mobility and embeddedness framework22 allowed the authors to view these perceptions from perspectives that lend themselves to educational intervention, providing guidance on how medical schools can deliver their social accountability mandate.
Structural/organisational perspective
The WHO Global Observatory for eHealth series identifies telemedicine as a tool to increase the accessibility of medical care and enhance health service provision by providing clinical support irrespective of geographical barriers, thereby improving health outcomes26. The structural perspective highlighted the impact of geographical isolation on rural practice, perceived to be exacerbated by the limited allocation of medical resourses and reduced access to virtual technology in rural areas. Professional and social isolation due to rural location is unattractive and deters health workers from working rurally27.
Increased virtual technology utilisation is reducing patient and practitioner isolation in rural areas. Prior to the COVID-19 pandemic, all Scottish Health Boards (regions) were tasked with expanding NearMe, a virtual consulting platform designed to increase healthcare access connectivity for patients and physicians in rural areas28. In 2019, 9000 NearMe consultations were conducted across Scotland. Since the COVID-19 response in March 2020, up to 17 000 virtual NearMe consultations occurred per week in Scotland29.
Only one medical student referenced virtual technology, and its alleviation of patient/physician isolation in rural settings. Educational experience in a rural clinic shaped their knowledge of NearMe. Medical students’ minimal knowledge of virtual consulting platforms is concerning, because increased virtual connectivity to urban medical hubs for networking, collaboration and continuing professional development may challenge the views of isolation in rural practice30. Medical education can challenge the common perception of rural isolation through experience mechanisms that emphasise the use of virtual technologies for a variety of uses.
Occupational perspective
ScotGEM participants, who were more routinely exposed to generalist clinicians both in the classroom and on placement, referenced role modelling repeatedly. Role models actively influence medical students’ career choices by integrating them into clinical settings31, and passively influence through their passion and excitement for their work32. Role modelling in the ScotGEM curricula may have specifically enhanced students’ recognition of the ability for generalists to subspecialise in an area of interest, altering their occupational perspective, which can assist in recruitment33.
BSc undergraduate students were not aware of the ability to develop extended clinical roles as a generalist, making their perception of generalist versus specialist much more rigid and rooted in geographic location. Low generalist representation in medical education might instil this perception. Generalists account for 50% of the UK physician workforce, but only 6% of medical educators34.
Participants commented that rurality might complicate diagnosis or treatment given geographical isolation and lack of technology, contributing to a rural practitioner’s clinical uncertainty. Greenhalgh and colleagues suggest that practitioners must learn to work within complex systems, which are open, dynamically evolving, unpredictable and self-organising35, the ‘grey-scale space’ of medical practice36. The prominence of uncertainty in primary care is attributed to patients presenting with a wide array of problems, early phases of disease, and comorbidities37. Medical curricula should actively address uncertainty to ensure students are not dissuaded by its prominence in rural practice.
Uncertainty affects a physician’s anxiety levels and work-related stress and can cause burnout38,39, yet experienced physicians learn to handle uncertainty40. In medical students, uncertainty affects their wellbeing, career choices and attitude towards patients41,42. Given the significant uncertainty associated with practice during the COVID-19 pandemic35, experienced physicians, especially now, must be encouraged to share experiences and methods of overcoming uncertainty with all medical students, but particularly those considering rural practice. Some participants clearly had positive views towards uncertainty and identified curricula mechanisms to help develop this43.
Personal life perspective
For some participants (often those who originates from rural areas or had immersive, rural educational experiences), the association of rural practice with a greater sense of community was positive, with rural communities perceived as being better equipped to support residents. Other students negatively perceived rural communities as ‘tight-knit’ and commented on the anonymity challenges rural clinicians face in their social lives. There is good evidence that codesigned, immersive medical education opportunities, such as that developed by the Northern Ontario School of Medicine’s community-engaged education curriculum, results in medical students who are increasingly motivated to undertake rural practice44.
Strengths and limitations
There is limited qualitative research that explores perceptions of remote and rural practice of medical students (although the current findings align with the limited research that does exist45), specifically as it pertains to the intricacies of Scotland’s medical education and healthcare system. Moreover, the use of Feldman and Ng’s pre-existing framework22 to explore medical students’ perceptions of rural practice is particularly novel, because it has not been applied to students anticipating their future careers.
While a small sample, demographics were well distributed between BSc students (4) and ScotGEM students (6), allowing for examination of both medical education programs and their consequent perspectives. The gender distribution of the sample was representative of the 2018/2019 UK Higher Education student enrolment in medicine and dentistry46.
Limitations of the study persist. Self-selection of participants may have created unintended bias within the sample46. Qualitative research is heavily dependent upon the researcher’s experience and personal bias, potentially affecting data collection47; however, researchers from heterogenous disciplines were involved in analysis, mitigating this potential impact. The small sample size must be an acknowledged limitation of this study. The research aims were narrow, suggesting a large sample may not be necessary to achieve sufficiency. However, the group of participants held variable yet highly specific characteristics related to the subject. Sufficiency may be enhanced in future research by using a longitudinal or cohort study for a more in-depth comparison and exploration of medical education’s effect on future career decisions48.
Conclusion
Recruitment and retention in rural health care remains a critical global challenge, particularly in low- to middle-income countries49. The findings of the study are consistent with the rural medicine education literature. The study adds to that literature through using a theoretical framework to understand the findings. This pilot can be used to inform a larger study that examines the mechanisms identified as potentially influential in medical student perceptions of rural practice, including exposure to telemedicine, GP role modelling, training in overcoming uncertainty, and codesigned medical education programs. Approaching this challenge in a systematic and theory informed way allows policy-makers and governments to fully consider the impact medical education programs make on rural and remote healthcare recruitment and retention.
References
You might also be interested in:
2008 - Forty years of allocated seats for Sami medical students - has preferential admission worked?



