Introduction
Social support and the role of social support in health has been studied in various contexts for decades1-6. More than 115 years ago, Emile Durkheim found that individuals with fewer social ties had higher rates of suicide3. Social support is considered to be a function of social relationships4, has been defined as support provided through relationships and social ties, and can be both positive and negative. While there is no agreed-upon theory explaining the mechanisms of social support in relation to health, in general two pathways are discussed: the main effect model and the stress-buffering model1,2,7. The main effect model posits that social relationships affect health through social influence and through provision of services and information whether or not individuals are under stress8. These first-level effects influence health-promoting behaviors that, in turn, impact on health-relevant biological influences and ultimately physical and mental health. Within the stress-buffering model, support functions by preventing debilitating responses to stressful events9. In this model, the perception that support will be provided when it is needed, rather than whether it is actually provided or not, is the key to stress buffering.
Under both models, there is strong evidence that social support – particularly perceived social support – functions as a protective factor for health10-12. Social support is associated with risk reduction factors, including alcohol reduction/abstinence, tobacco cessation/abstinence13, healthy eating and exercising14. Social support is associated with a variety of positive health outcomes, including normal blood sugar levels15-18, healthy weight, healthy cholesterol, healthy blood pressure19, healthy cardiovascular function20 and better immune function21. There is evidence from multiple longitudinal studies that social support serves a protective function against all causes of mortality22. Individuals with the highest levels of social support live the longest4. Conversely, a lack of social support is a risk comparable to or greater than smoking as many as 15 cigarettes a day, physical inactivity, or obesity22. Low levels of social support have been associated with coronary heart disease23 and increased risk for depression24,25 and suicide26-28.
The majority of large-scale studies of social support have been conducted in urban areas29,30, but social support has also been studied in rural settings4,12,31-33, most often with geography as a relevant variable. Examining rural settings is essential because, as House et al2 note, although the size of an individual’s social support network does not vary much when urban and rural individuals are compared, urban networks tend to comprise more non-relatives, whereas rural networks are more often based on family structures. Because the qualities of these social support networks differ, particularly in their different structures, relational demands, and potential role conflicts, the way that they enable or disable the social, psychological, and physiological processes of social support may differ as well. In Ecuador, nearly all empirical studies of social support have been conducted in urban settings34,35 or among populations such as college students36, healthcare professionals37, or prisoners38, who are qualitatively unlike the majority populations of Ecuador. The limited exception is a study of a single rural family to whom a social support intervention was applied39. Little, then, is known about social support in rural Ecuador. This study serves as an initial attempt to understand social support and its relation to health in rural Ecuador.
Social networks (and the positive or negative social support provided by them) are situated within a larger sociocultural context. Recent focus on upstream factors contributing to health outcomes parallel the expanding body of work on how social networks function in context and in the face of rapid social change, political upheaval, socio-economic distress, and natural disasters5. Social support has also been included in a growing body of research conducted in the aftermath of natural disasters40, specifically earthquakes25,36-39. Most of this research has been conducted in Asia and North America40-44, but a desk review conducted by Troya and colleagues45 indicates that social support may be a protective factor following natural disaster in Ecuador as well. Both the main effect and stress-buffering approaches to social support function after a natural disaster. Specifically, Troya and colleagues argue that, following a disaster, individuals who are socially integrated with a strong set of relationships should be able to draw on more sources of informational resources, tangible support such as food or shelter, appraisal support of feeling valued, and belonging support of being part of a larger community. This social support, in turn, should have a direct effect on physiological, psychological, and social processes that assist wellbeing. Moreover, those individuals who believe this support is available to them should have their stress buffered both in anticipating a disaster and following a disaster, because they will feel better able to respond to a disaster.
In April 2016, coastal Ecuador experienced a 7.8 magnitude earthquake, one of the most destructive in the history of the country46-48. The earthquake resulted in 663 deaths and 6274 injuries, and 28 755 residents sought emergency shelter. More than 1400 buildings were damaged and economic costs are estimated to be about US$3 billion45. Complicating the response to the earthquake, Ecuador, home to more than 16 million people, continues to face political upheaval and major public health challenges, including increasing wealth inequality, increasing rates of chronic disease49, and fragmented social and health services45. Manabí province (population 1.4 million), the location of the epicenter of the earthquake, lies on the coast of Ecuador and suffered the highest number of injuries, deaths, and damaged buildings. Three out of every four people (76.8%) in Manabí live in poverty and have unsatisfied basic needs50. In San Isidro, a rural parish in Sucre County, Manabí, this rate is 86.5%; and there is a high rate of rurality, poverty, and disease burden, as well as a low availability of health services51.
Within this context, social support may serve to buffer individuals against the health outcomes that often emerge from negative social determinants of health. To describe the potential role of social support on health outcomes and protective health behaviors in rural Ecuador, four research questions were posed shortly after the earthquake:
RQ1: What are the general levels of social support experienced by individuals living in rural areas of Manabí province?
RQ2: Do different demographic groupings in Manabí report different levels of social support?
RQ3: Is there a relationship between social support and health outcomes in this region?
RQ4: Is there a relationship between social support and protective health behaviors in Manabí?
Methods
Study design
To answer the research questions and to evaluate the influence of social support on health outcomes and risk reduction behaviors, a cross-sectional design was employed. An intercept survey of patients visiting a health clinic was conducted in June and July 2017. The clinic was located in San Isidro Parish, Sucre County, Manabí province, Ecuador (~0.3763°S, 80.1847°W) (Fig1). San Isidro Parish has a population of about 11 000 residents, 3000 of whom live in town. The research team carried out the surveys as part of a larger project. Specific data were collected by an oral interview method to complete the survey.
 Figure 1: Map indicating the location of the study site in San Isidro Parish, within Sucre County, Manabí province. Inset indicates location within Ecuador and South America.
Figure 1: Map indicating the location of the study site in San Isidro Parish, within Sucre County, Manabí province. Inset indicates location within Ecuador and South America.
Participants
Participants were told the general purpose of the study (to understand various contributors to health and wellbeing in their community), read an approved consent form, and were asked to participate in the study. Participants either signed the form or provided their thumbprint to indicate consent.
A total of 416 individuals participated. The population was largely representative of the region, apart from sex; men constituted about one-third of the sample and women a little more than two-thirds. Participants were predominantly mestizo, ie of mixed Spanish and Indigenous descent. The mean age of the participants was about 50 years; the youngest participant was 18, the oldest participant was 101. Education levels clustered around having some primary school or having completed primary school. Most participants were self-employed or worked within the home, and most households consisted of two people. About one-quarter (92) of the participants lived in the municipality of San Isidro, while the remainder lived in villages and communities on the periphery of this municipality. Full demographics are reported in Table 1.
Table 1: Study participant characteristics (n=415)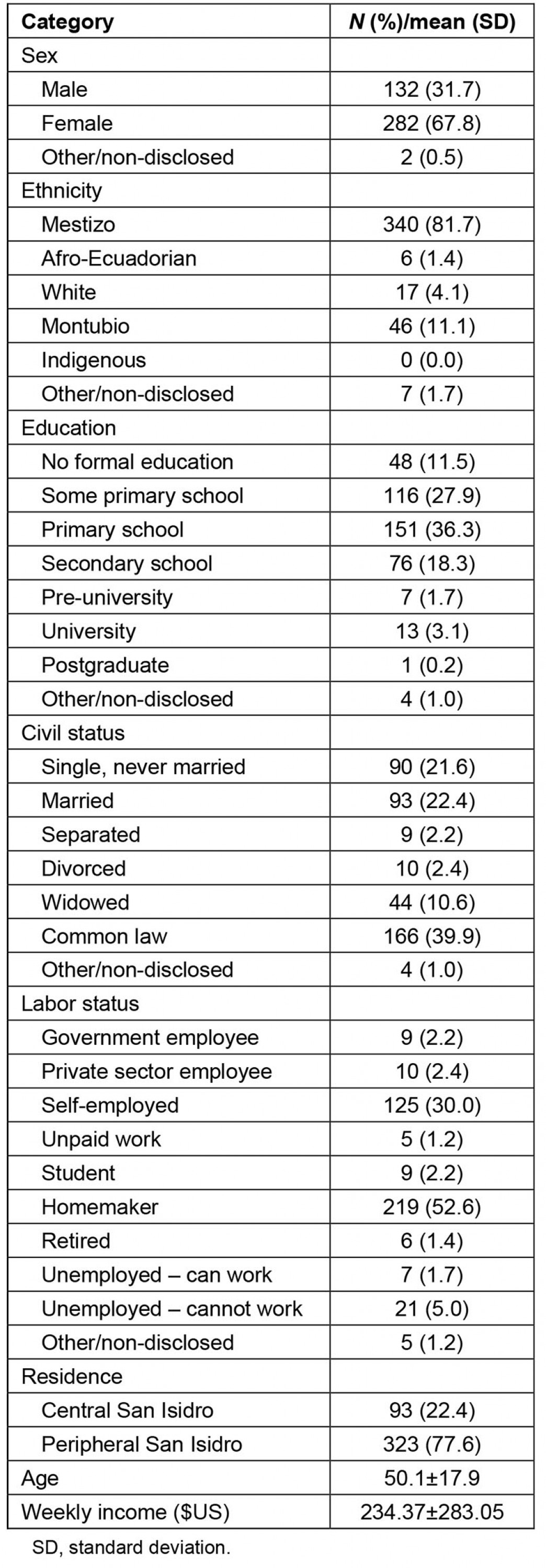
Instruments
Perceptions of social support: Participant perceptions of the social support they received were measured using the Spanish-language version of Cohen and colleagues’52 Interpersonal Support Evaluation List (ISEL-12). Participants were asked 12 questions, using Likert-type measures, with scores ranging from 0 (definitely false) to 4 (definitely true). Following Merz and colleagues30, who found that the ISEL-12 is unidimensional when employed among Spanish-speaking populations, the instrument was not divided into subscales.
Sources of social support: Participant perception of the sources from which they received social support were measured using the Spanish-language version of the Multidimensional Scale of Perceived Social Support53 (MSPSS). Because this version had not been tested in Ecuador, a pilot test was performed in Puyo, Pastaza province, Ecuador. Minor modifications to the number of response options on the scale were made. Following Arechabala and Miranda’s54 adaptations for a Chilean population, participants were asked 12 questions, using Likert-type measures, with scores ranging from 1 (almost never) to 4 (always or almost always). The MSPSS measures three sources of social support: from a significant other, from family, and from friends.
Healthy weight: Participant healthy or unhealthy weight was assessed using body mass index (BMI). The BMI assesses the relative leanness or corpulence of an individual through an assessment of a ratio between height measured in meters and weight in kilograms squared. Standard World Health Organization (WHO) cut-off scores55 were used (underweight BMI<18.5; normal BMI range 18.5-24.9; overweight BMI range 25-30; obese BMI>30). Weight was measured using a SECA weight scale (model SECA 213, Hamburg, Germany).
Blood pressure: Blood pressure was measured using an Omron Cuff (M2-HEM-7121-E, Los Angeles, CA). WHO’s definition55 of elevated blood pressure was used to classify people as having low, normal or elevated blood pressure (cut-offs: systolic blood pressure ≥140 and/or diastolic blood pressure ≥90).
Cholesterol: Participant fasting cholesterol levels were measured by biochemical analysis. WHO’s definitions55 were used to classify people as having either normal (≤199 mg/dL) or high (≥200 mg/dL) levels of total cholesterol.
Blood sugar: Fasting blood sugar was measured by biochemical analysis. WHO’s55 definitions were used to classify people as having normal (70–100 mg/dL), low (<70 mg/dL), or high (>100 mg/dL) glucose blood levels. In order to analyze the data, glucose levels were classified as normal (≤124.9 mg/dL) or diabetic (>125 mg/dL).
Risk reduction factors: To assess risk reduction behaviors, participants were asked to report their smoking status (ie smoker or non-smoker), drinking status (ever drinker or never drinker), fruit and vegetable consumption (daily consumption of fruit or less than daily, daily consumption of vegetables or less than daily), and attainment of physical activity recommendations (three or more days/week where moderate or strenuous physical activity is performed for fewer days per week).
Analysis procedures
All data were analyzed using Statistical Package for the Social Sciences (SPSS) v14.03 (IBM; www.spss.com). Pearson’s product-moment correlation coefficients were computed to assess the relationship among sources of social support and with overall perceived support. Analysis of variance tests were performed to determine whether demographic differences in perceptions of total social support received and the sources of that support emerged, and, later, to determine whether there were differences in social support received by individuals with different health outcomes.
Ethics approval
Survey procedures were conducted according to a protocol approved by the Institutional Review Board of the Pontifical Catholic University of Ecuador (CEISH-308-2017) and the Ecuadorian Ministry of Health (MSPCUR1000216-3-etapas 1, 2, 3 y 4).
Results
Social support
The first research question asked about the general levels of social support experienced by individuals living in Manabí province. Participants reported moderate levels of overall social support on the ISEL-12 (mean (M)±standard deviation (SD)=1.99±0.57, Chronbach’s α=0.71). On the MSPSS, each dimension reflected a reliable subscale comprising the four items associated with each dimension, and, on each dimension, participants reported moderate to high levels of social support (significant other, 2.35±0.65, α=0.71; family, 3.17±0.91, α=0.79; friends, 2.58±1.00, α=0.82). All three sources of social support and overall support received were correlated, and all correlations were positive and significant (see Table 2).
Table 2: Correlations among sources of social support and total perceived support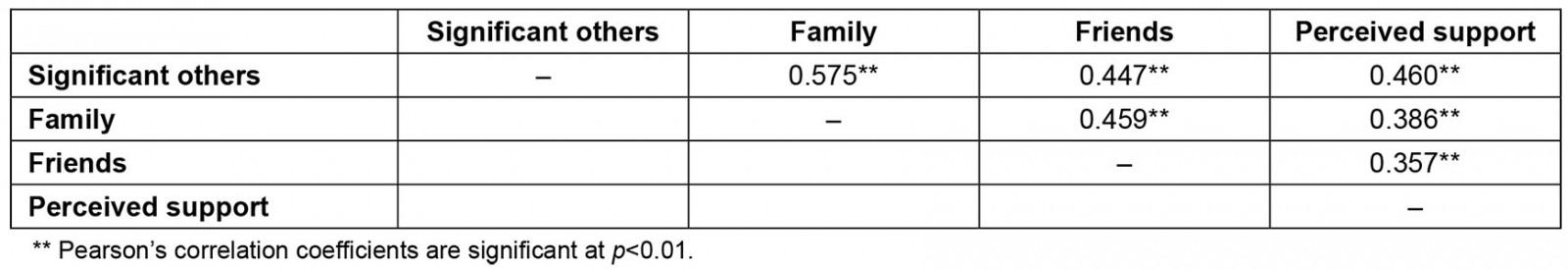
Demographic differences
The second research question asked whether different demographics groupings in Manabí reported different levels of social support. Generally, there were few relationships between demographic factors and different forms of social support (see Table 3).
Sex: Men and women did not significantly differ in their report of social support received from significant others or from family or in total social support received. Men (M=2.72) reported receiving slightly more social support from friends than did women (M=2.57). Although the sex difference was statistically significant (F(1,408)=4.31, p=0.03), the effect size was very small (η2=0.01).
Ethnicity: No differences emerged in the effect of participant ethnicity on either sources of social support or the total amount of social support received.
Education: Participant level of education did not affect the amount of social support received from friends and family but did affect the amount of social support participants reported receiving from significant others (F(5,401)=6.00, p<0.01) and the total amount of support received (F(5,354)=5.68, p<0.01). As indicated in Table 3, the overall differences were that individuals with no formal education reported the least support from significant others and the least amount of social support overall, and, as educational levels increased, so did the reported level of social support from significant others and amount received overall. There was a small but respectable effect of educational level on both variables (significant other, η2=0.07; ISEL, η2=0.08).
Civil status: Participant civil status did not significantly affect their report of social support received from friends or in total social support received. However, it did affect the amount of social support received from significant others (F(5,402)=4.52, p<0.01) and from family (F(5,401)=5.56, p<0.01). As indicated in Table 3, people who were separated or divorced received the least support from significant others and family, those who were single and never married received middling support from these sources, and those who were in formal or common-law marriages received the most. There was a small but respectable effect of civil status on both variables (significant other, η2=0.05; family, η2=0.07).
Workforce participation: Participant workforce participation did not significantly affect their report of social support received from significant others or family, or the total amount of support received. Some differences did emerge in the amount of social support received from friends (F(8,398)=2.16, p=0.03). Table 2 illustrates where differences emerged, but there are few interpretable patterns. The effect of labor participation on support received from friends was small (η2=0.04).
Residence: Individuals who resided in the municipality of San Isidro and those who lived in peripheral communities did not significantly differ in their report of social support received from significant others, family, or friends. Members of peripheral communities (M=1.94) reported receiving less overall social support than did residents of San Isidro (M=2.15). The difference was statistically significant (F(1,408)=9.214, p<0.01), and the effect size was small (η2=0.03).
Age: Participant age, grouped in decades, did not have a significant main effect on social support received from family, friends, or significant others. Minor differences, without pattern, emerged among some age groupings. Participant age, however, did have a main effect on the amount of total social support received (F(7,349)=2.69, p<0.04). As indicated in Table 3, people who were 80–89 years old differed from all other decades, and no other decades differed from one another. This indicates that the nadir of social support is in the 80s, and that the effect is small (η2=0.05).
Table 3: Analyses of variance in social support sources and total support received by demographic groupings†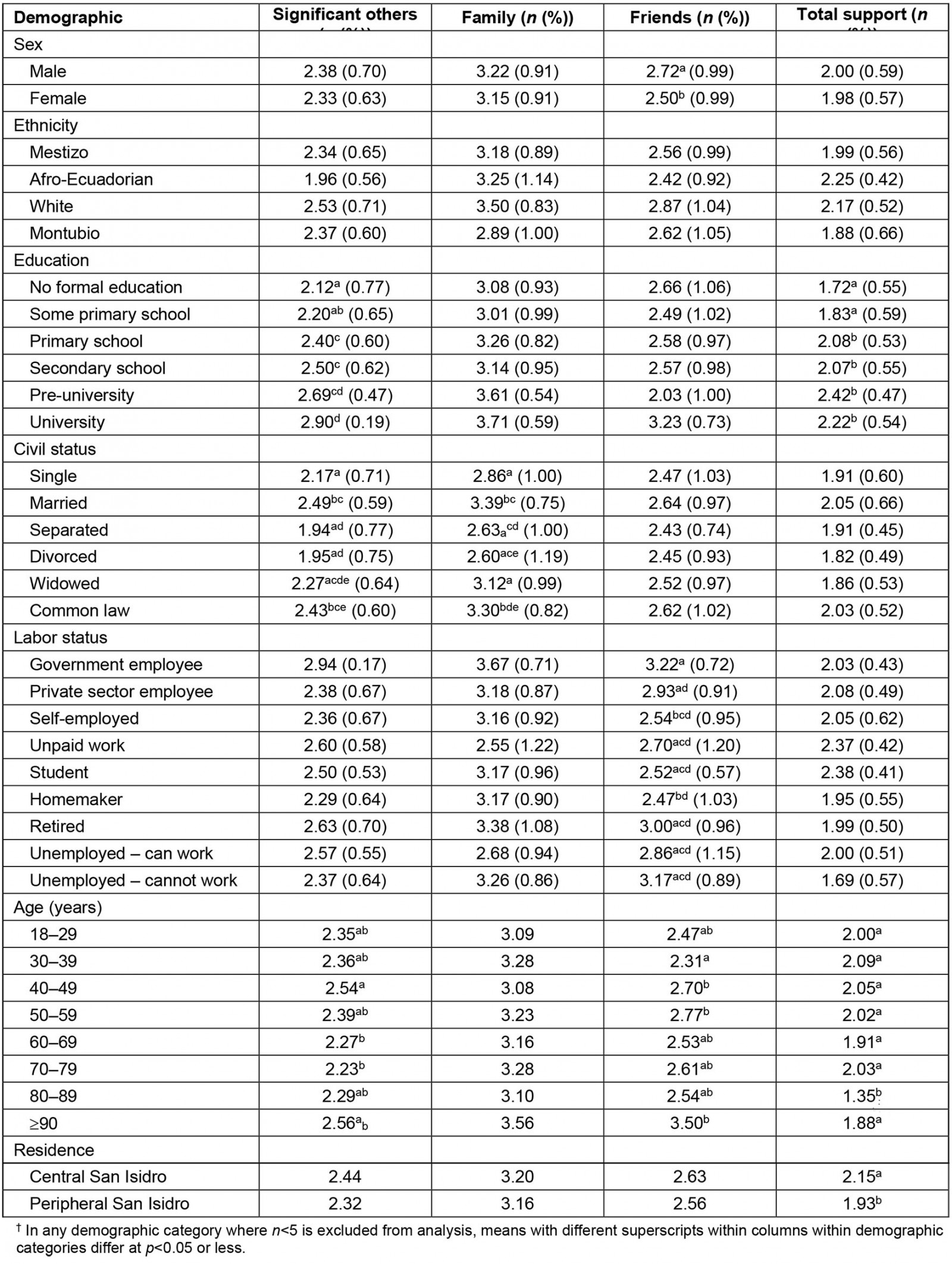
Health outcomes
The third research question asked if there was a relationship between social support and health outcomes in Manabí. No statistically significant differences emerged in sources of social support or the total amount of social support for any of the four health outcomes measured.
Risk reduction factors
The fourth research question asked if there was a relationship between social support and protective health behaviors in Manabí. Again, some relationships emerged between different forms of social support and risk reduction factors (see Table 4 for full results).
Participants who smoked (n=24) did not significantly differ from non-smokers (n=379) in the amount of social support they reported receiving from friends. Smokers (M=1.99) reported receiving less social support from significant others than non-smokers (M=2.37; F(1,401)=7.99, p<0.01). Similarly, smokers also reported receiving less social support from family (Msmoker=2.71, Mnon=3.21; F(1,401)=7.03, p<0.01) and less social support overall (Msmoker=1.75, Mnon=2.00; F(1,355)=4.05, p<0.05). Although these were statistically significant, the effect sizes were very small (η2=0.02 and 0.01, respectively).
Participants who drank alcohol (n=95) did not significantly differ from non-drinkers (n=284) in the amount of social support they reported receiving from any source or in the total amount of social support they received.
Participants who ate fruit daily (n=207) did not significantly differ from those who did not (n=192) in the amount of social support they reported receiving from friends or family. Fruit eaters reported receiving more social support from significant others (Mfruit=2.47, Mnon=2.22; F(1,398)=7.53, p<0.01) and more social support overall (Mfruit=2.10, Mnon=1.88; F(1,352)=7.19, p<0.01). The effect sizes of these differences were small (η2=0.04 and 0.04, respectively). No statistically significant differences emerged between those who ate vegetables daily (n=99) and those who did not (n=302).
No participants reported performing strenuous or moderate physical activity three days a week or more. Therefore, no comparisons between exercisers and non-exercisers were possible.
Table 4: Analyses of variance in social support sources and total support received by behaviors†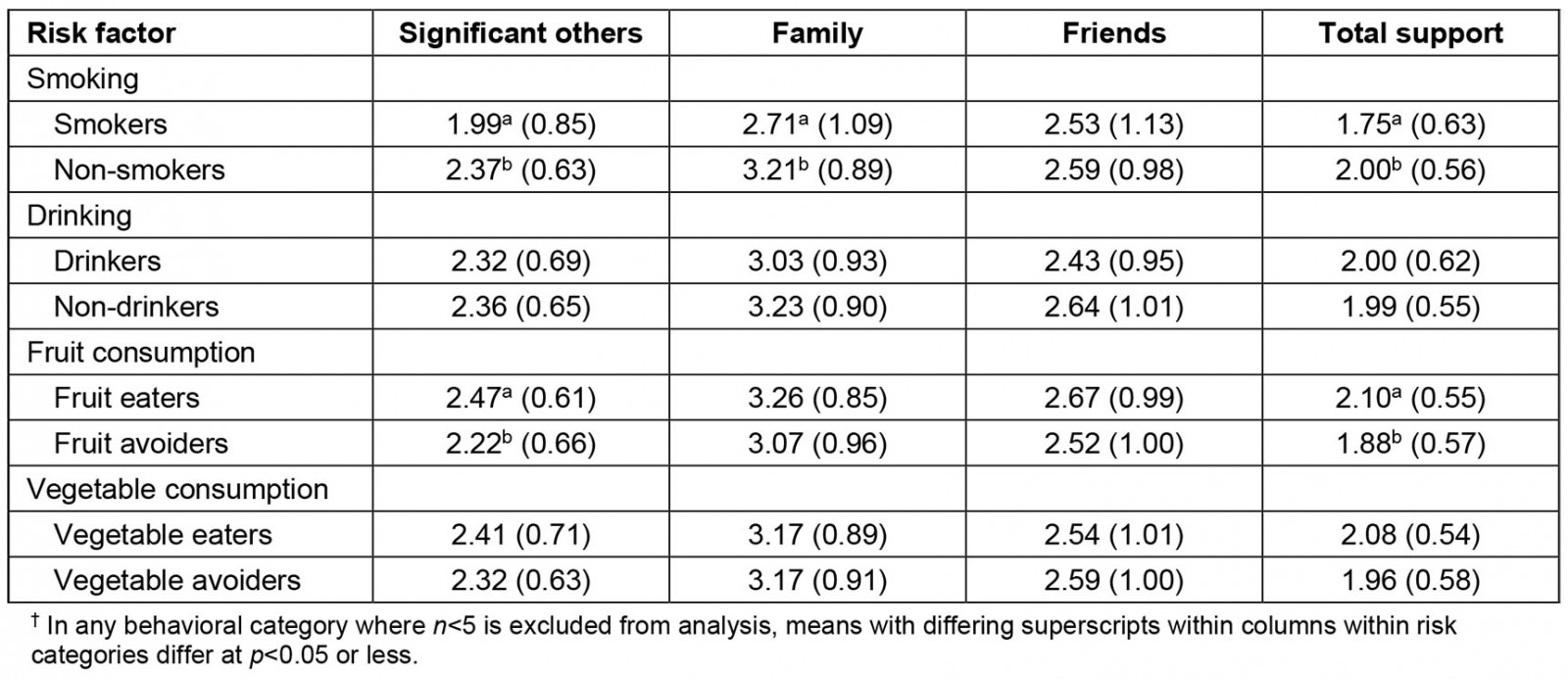
Discussion
The first research question asked about the level of social support experienced by individuals living in San Isidro, Manabí province. Levels of social support were moderate. No ceiling or floor effects were observed.
The second research question asked whether different demographic groupings in Manabí reported different levels of social support. In some studies, what is not found to be significant is as interesting as what is found to be significant. In this study, few meaningful differences were found among demographic groups. Generally, marriage/partnership, education, and labor participation were associated with some areas of increased social support, but the effects of each are limited. Unlike findings from urban areas, where certain demographic groups such as men or unemployed people are markedly different in the amount and kinds of social support they receive, there were few patterns in the data in this study. This indicates that, if an intervention wants to increase social support in a community such as San Isidro, it cannot target demographic variables alone. Instead, a whole-community approach would be preferred, with the aim of increasing social support for all.
To address whole communities, scholars and practitioners may wish to draw on the experiences of the Latin American Network for Perinatal and Reproductive Research (LANPER)56-59 Similar to the current findings, LANPER researchers found that asking individual women in Argentina, Brazil, Cuba, and Mexico to draw on individual-level support and educating expectant mothers was not associated with improvements in maternal behaviors, perinatal outcomes, or utilization of health services when compared with expectant mothers in a standard care group56. In a second intervention, having social workers or trained health workers provide health education and information about social support, but also providing direct emotional support, enhancing and extending social support networks, and connecting women to social and health services from the clinic and government greatly improved perinatal and postnatal outcomes for both mother and child57,58. Moreover, women who were not targeted by the intervention as expectant mothers and who later became pregnant also benefited because the social support network and integration into health systems was generally strengthened and common stress points were identified and ameliorated across the community, not just for the women pregnant at the time of the intervention59. Rather than focusing solely on the relationship between social support and individual health outcomes, the LANPER group sought to identify social stressors that could potentially affect all women, social networks that could be strengthened for all women, and clinical and social services that would assist all women. The possibilities suggested by this urban intervention might inform whole-community approaches in rural areas. If we, in preparing communities before a disaster or assisting in responding to a disaster, adopt a similar community-strengthening approach of identifying common stressors, enhancing social support networks, and bolstering health and social services, we may be better able to activate the social buffering properties and main effects of social support.
The third research question examined potential relationships between social support and health outcomes. No relationship was found between health indicators and social support in this rural community in Ecuador. A simplistic explanation would be that the extremely high levels of poverty and rurality in the region may have created a stronger main effect on health indicators than could be attained through adjustments in social support. If this were the case, widespread poor health outcomes would be expected. It is possible, however, that the associations among health outcomes and sources of social support may function differently in a rural and/or Ecuadorian context. The participants in this study were mostly healthy individuals living in a rural social environment where families tend to be united and there are plentiful opportunities for conversation with neighbors and community members. In the authors’ qualitative research (reported elsewhere60), participants related that, despite their poverty, they had quiet lives without major problems and that they possessed a generally positive outlook on life. Poverty and rurality, as social determinants of health, may be outweighed by the tranquil everyday life experienced by inhabitants of rural communities; the presence of safe streets, united families, and nearby neighbors may be protective of health. These social features are common to many rural areas of Ecuador. However, the quantitative components of the authors’ previous research found that chronic malnutrition and anemia in children from rural coastal communities is correlated with family incomes of less than US$80 per month, and that maternal height <150 cm correlates with residence in a household with more than four children60. Although a basic link was found between poverty and malnutrition, when other members of the research team re-analyzed the data with additional information from the Social Capital Assessment Tool (SCAT), it was found that higher degrees of social capital are associated with lower rates of malnutrition61. Because SCAT measures resources beyond family, friends, and significant others, to include governmental, community, charitable, and religious organizations, it may be that the definition of social support should be expanded beyond the sources in the MSPSS. Moreover, because SCAT includes social capital as a feeling of support availability, and not only directly identifiable instances of support, the ISEL-12 may not capture how perceptions of a generally supportive community and general feeling of support availability may influence wellbeing. Thus, research needs to be conducted in other areas of Ecuador, including urban centers, to assess how social support might be conceptualized differently or might function differently in non-rural contexts. It would also be useful to assess social support experienced by individuals in rural Ecuador who are suffering from ill health, not just those who feel generally healthy.
The final research question examined potential relationships between social support and protective health behaviors. No relationships were found in alcohol consumption, physical activity, or vegetable consumption. Lower levels of social support are associated with smoking; it may be that lack of social support leads individuals to smoke tobacco or that smoking tobacco drives away potential providers of social support. Future research should consider a time-series design to investigate this relationship. Similarly, fruit eaters report more social support; given there are few reasons to think that abstinence from fruit consumption would drive people away, it is likely that greater support from one’s social network enables a healthier diet, at least in the limited context of fruit consumption.
Conclusion
This study is among the first to describe social support and its relation to health in a rural community in Ecuador. Previous research on social support in Ecuador has been in urban areas and/or among unrepresentative populations. These findings, generally, indicate that social support, as a construct, may operate differently or be understood differently in rural Ecuador as compared to urban Ecuador. Studies attempting to link social support to health in Ecuador, other than the authors’ previous work on overall social capital60,61 and Walcott’s community-based intervention delivered by nursing students to a single rural family39, seem to be absent, attesting to the novelty of these findings. Although the instruments used in this research were previously validated in native Spanish-speaking populations in Latin America, it is possible that there are differences between the understanding of what comprises social support in rural Ecuadoran communities and in the urban areas of Latin America that have been investigated before. For example, in Colombia, researchers found the same structure of the MSPSS that the current study did among urban youth, but called for considering schools, health organizations, and religious groups as potential additional sources of social support62. This explanation seems limited, however, because studies among Ecuadorian emigrants to Spain show little difference between Ecuadorian and Spanish respondents or among subgroups of Ecuadorian respondents in their experiences and definitions of social support63-65. Moreover, studies of the MSPSS among urban youth in Chile54,66 and Peru67 found the same factor structure and did not call for additional dimensions. Although it is possible that an adult rural population in Latin America would draw on additional sources of social support, expanding these sources does not ensure the identification of a lever of social action that can be pulled in the case of a disaster.
Although this study did not find many significant impacts of social support, it does provide a general outline of social support in these communities. Although this study provides a general outline, providing future research directions for research may help address some of the limitations of the study. Because the sample for this study was drawn from patients visiting a health clinic, it is possible these participants differ from individuals who do not seek health care in general health status and risk reduction behaviors. Recruiting through the remaining few community institutions in San Isidro other than the clinic, such as the church or the market, may allow a broader sample. From a measurement perspective, the MSPSS only considers three sources of social support (significant other, family, friends), whereas there could be other sources that were not measured by this instrument, such as those included in SCAT. It is possible that, in rural Ecuador, social support is delivered more by churches, non-governmental organizations, and other sources than in urban Ecuador. Similarly, the ISEL-12 only operates along the appraisal, tangible, and belonging dimensions of social support. It could be that informational support (which ISEL does not measure) or general feelings of support not tied to a specific dimension of social support have an outsized effect on health outcomes and healthy behaviors in rural Ecuador as compared to the effects of other kinds of support. Future research should examine both of these possibilities.
Acknowledgements
The authors thank Carlos Erazo-Cheza from the Facultad de Medicina, Pontificia Universidad Católica del Ecuador, for assistance in obtaining clinical information, and Cesar Yumiseva for construction of the map. The authors would like to thank the assistance of Manuel Gilces, San Isidro municipality, and of David Macias, Daniel Guerrero and Cecilia Velasco, Ministry of Health in San Isidro.
References
You might also be interested in:
2018 - Promoting delayed umbilical cord clamping: an educational intervention in a rural hospital

