Introduction
Gastroschisis is one of the most common congenital abdominal wall defects, with an incidence of 4–5/10 000 newborns worldwide. It was once considered fatal if a large defect could not be closed primarily, or if postoperative mechanical ventilation were not possible. However, a survival rate of up to 90% is now achievable in many settings due to use of various types of silos for staged reduction of the intestines into the peritoneal cavity, and good general supportive postoperative care. The management of large gastroschisis still remains a challenge in low-income settings, with the need for prolonged hospital stay, and the frequent occurrence of malnutrition and infections.
In Papua New Guinea (PNG) there are 240 000 births annually, which means there are about 100 babies born with gastroschisis. PNG has 0.7 doctors and 5 nurses per 10 000 people. Most babies with life-threatening congenital abnormalities do not survive, and many are not referred.
Case report
A preterm male at 34 weeks gestational age weighing 1750 g was admitted to special care nursery with a diagnosis of gastroschisis. He was born to a 26-year-old healthy woman, para 3 gravida 4. The mother had a vaginal delivery of her last child, just 11 months before the preterm baby delivered. At birth, the baby was identified to have the entire small bowel and entire colon exteriorised. The defect diameter was 2 cm × 4 cm on the anterior abdominal wall lateral and the right on the umbilicus. No other anomaly was detected.
The herniated organs were initially covered with sterile gauze and bandages soaked in warm saline and prepared for surgery. Within 6 hours of delivery, the child was taken into the operating theatre for attempted primary reduction and silo bag application. A nasogastric tube was inserted for evacuation of gastrointestinal secretions. Intravenous fluids and antibiotics were given. A rectal tube was inserted, with much return of meconium. Under general anaesthesia, after sterile skin preparation and full draping, the rectus sheath was liberated from the skin and the umbilical cord vessels were isolated and ligated. Enclosure of the herniated viscus into the abdominal cavity was achieved using a silo bag application and stitched to the fiscal margins of the defect using four-stitch technique with synthetic (polyglactin 910) 3/0 suture (Fig1). Following the silo application, the baby was nursed in the special care unit, on intravenous fluid for 3 days prior to commencement of enteral feeding with expressed breast milk (Fig2).
On the sixth day, he was taken into theatre for secondary skin closure. Under aseptic preparations and general anaesthesia, the silo bag was removed; the bowel was mobilised and gently reduced into the peritoneal cavity with minimal difficulty (Fig3). The rectus sheath was left open, and transverse skin closure was done with proline 5/0 suture.
The baby breathed spontaneously after reversal from anaesthesia and maintained normal oxygen saturation. He was then returned to the special care nursery and was given intravenous fluids. The baby’s bowel started functioning 2 days after secondary closure. Oral feeds were restarted on post-operative day 3 and the baby was able to tolerate full oral feeds on day 5. He was discharged on day 6 with no complications. He was reviewed on day 15 and the sutures were removed. The baby on day 15 weighed 2.1 kg, having gained 350 g since birth.
The infant underwent a third surgery at 2 months of age where closure of the rectus sheath completed the repair. He is followed monthly, has gained weight steadily and is feeding well with no apparent problems.
Written permission and informed consent were given from the parents of the neonate.
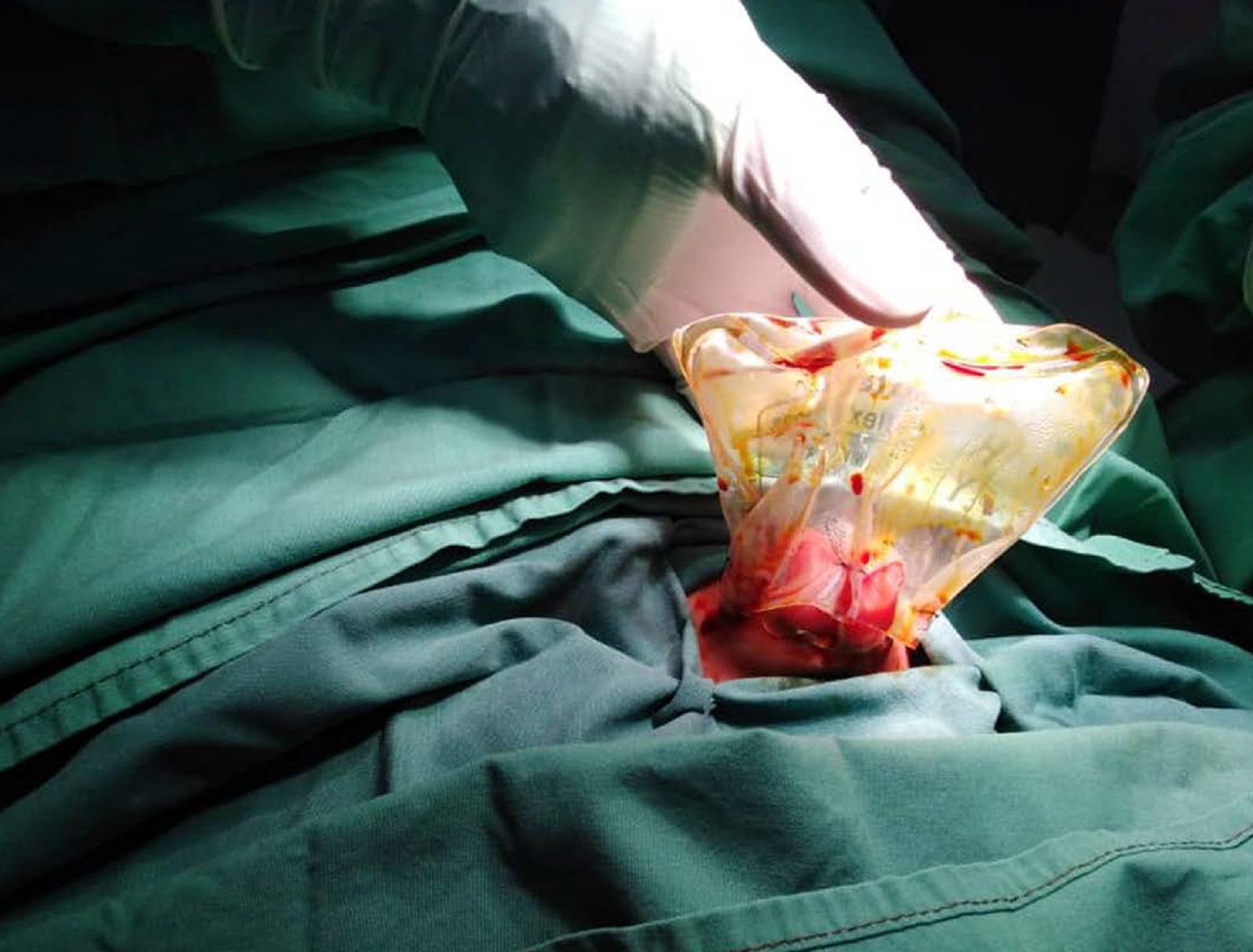 Figure 1: Attachment of normal saline bag silo.
Figure 1: Attachment of normal saline bag silo.
 Figure 2: Normal saline bag silo in special care nursery on day 3.
Figure 2: Normal saline bag silo in special care nursery on day 3.
 Figure 3: Skin closure of defect on day 6.
Figure 3: Skin closure of defect on day 6.
Discussion
We treated a preterm baby with gastroschisis at the Port Moresby General Hospital. Because the baby was small and primary closure was not possible, we used a normal saline plastic bag as a silo in which to enclose and protect the intestines. Successful reduction with skin closure was achieved in 6 days, and the baby could breathe spontaneously in the immediate postoperative period. Final rectus muscle closure was achieved at 2 months of age.
Gastroschisis is a congenital abdominal wall defect located at the right of the umbilicus with herniation of the mid-gut. It was first described by Calder in 17331. It is mostly an isolated anomaly and surgical management of repositioning of the bowels is either primary if the abdominal cavity allows it or more commonly a staged surgery as in the present case2,3. Gastroschisis is associated with malrotation of the midgut and atresia of the bowel in about 10% of these cases4. The patient in the present case does not have atresia.
There are several reasons for acute and chronic complications in gastroschisis. Damage can occur to the intestines because of prolonged exposure to amniotic fluid in utero, resulting in adhesion formation, and thickening and matting of the bowel. This can lead to poor peristalsis and a motility disorder, and intestinal mucosal dysfunction. Early management after delivery at peripheral centres is crucial to a good outcome. In PNG, most neonates being referred have their intestines wrapped in gauze or cotton wool. Such dressings become soaked with exudate and are prone to bacterial contamination. A better method is that the intestines are enclosed in a sterile normal saline plastic bag immediately after birth and the outer surface of the bag is adhered to the abdominal wall skin with tape5. This will reduce the risk of bacterial contamination and fluid loss, and improve postoperative outcomes.
We have managed three infants by this method, and two survived. Primary fascial closure is not possible in most cases due to the limited size of the abdominal cavity and oedematous intestines3. A high-technology option as primary treatment of gastroschisis is to use a spring-loaded silo, which can be applied in a neonatal intensive care unit. However, spring-loaded silos are expensive and not widely available in developing countries. Custom silos have been fashioned from a wide variety of materials such as silicon, Gore-Tex, blood collection bags and urinary catheter drainage bags, which are sutured to the fascial defect and used for progressive reduction of the bowel before final fascial closure2. The degree of the visceral-abdominal disproportion and the condition of the herniated viscera play important roles in surgical decisions and timing. We used a sterile normal saline bag to enclose the herniated bowel loops as a cheap and effective alternative.
In PNG, most infants with serious congenital anomalies do not receive treatment; more reporting of congenital anomalies and success in treatment will encourage referral. Healthcare workers should understand the initial first aid for a baby with a gastroschisis and need for urgent referral. Over time, increasing the number of mothers who receive an ultrasound antenatally may help gastroschisis be diagnosed antenatally, and enable maternal transfer so that birth can take place at a referral centre where paediatric surgery is available.
Conclusion
The use of normal saline bags for staged reduction of the intestines in gastroschisis in preterm neonates can be an effective treatment method for this serious condition. It is cheap and easily available and can be used even in smaller centres in settings where cost and technology are limiting factors. We recommend the use of saline bags as the preferred method for the initial treatment of gastroschisis in primary care settings, as our experience demonstrates it is safe and does not have the risk of gauze or cotton wool dressings.
