Introduction
Australians living in remote areas generally experience poorer health than their major city counterparts1. They have poorer access to and use of health services and higher rates of avoidable hospital admissions. The poor health status of Aboriginal and Torres Strait Islander Australians has been well recognised and accounts for a large portion of the health problems within remote areas2,3 and the 'gap' between Aboriginal and non-Aboriginal people in Australia is not closing3,4. There are far fewer doctors and allied health professionals in remote Australia, compared to urban areas, with around 65% less occupational therapists, podiatrists, optometrists and psychologists, 50% less physiotherapists and 40% less pharmacists compared to major cities5. Nurses are the most evenly distributed health professions, with a high distribution (unlike other professions) in very remote areas. In these remote areas the health professional workforce has difficulties with recruitment, retention6 and with advanced clinical practice, often in a complex cross-cultural environment7.
Preparing healthcare workers for rural and remote health work includes education about the unique characteristics of remote health, the overlapping roles of different health professionals, cultural awareness and interprofessional practice. Cultural awareness means being aware of, and developing sensitivity to, cultural difference and cultural diversity8. It is the first step toward culturally safe and responsive practice9. Cultural awareness is important for healthcare workers, particularly in the Northern Territory of Australia, where approximately 70% of health system users are Aboriginal or Torres Strait Islander peoples10. In the healthcare worker training environment, it is becoming more common to see cultural immersion programs as a way of increasing understanding and respect for Aboriginal and Torres Strait Islander cultures11-15.
Cultural immersion is based on the principle that full engagement with another's culture, and their practices and language, is an effective means of learning16. Smith et al describe 'cultural immersion' as a first quick dip into another culture, in a safe, supportive, educational environment13.
Interprofessional education is recognised as crucial for developing tomorrow's healthcare workforce and helping them be better prepared to adapt to local health needs17. Interprofessional education occurs when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes18.
The Katherine Remote Health Experience
The Remote Health Experience (RHE) 3-day activity has been conducted near Katherine, Northern Territory annually since 201119. It was initiated by senior educators within the Flinders Northern Territory Medical program (NTMP) and the NT University Department of Rural Health, which considered it important that students be exposed to and understand local Aboriginal and Torres Strait Islander cultures. While the individual educators have changed over the years, the enduring principle of promoting cultural safety among health professional students has been maintained. Since its inception it has involved first-year medical students from the Flinders NTMP, nursing, pharmacy and allied health students from Flinders University, Charles Darwin University and other universities throughout Australia, as well as Aboriginal and Torres Strait Islander health practitioner students from Batchelor Institute of Indigenous Tertiary Education. Led by Flinders University, it is run in collaboration with Indigenous Allied Health Australia, the Banatjarl Strongbala Wimuns Grup (BSWG), Sunrise Health Service Aboriginal Corporation, Batchelor Institute of Indigenous Tertiary Education, Katherine District Hospital, Charles Darwin University and St John Ambulance. All of these organisations had existing relationships with each other, given the remote location and small population of Katherine. Contributing to the program was not onerous, and the representatives of these organisations (which changed over time) felt the cultural education aspects of the program were important.
The RHE is designed to model the inter-professional training, practice and cross-cultural environment that students will encounter in their course placements and remote practice. It has three main objectives, 1) develop an understanding of remote health, 2) improve inter-professional communication and respect for other professions and 3) improve understanding and confidence in working with Aboriginal clients. The program format has been quite stable over the years. On the first day of the program each year, the RHE has included short presentations of 10 minutes each by experienced remote health professionals on the difference between rural and remote health and the role of different health professions in the remote context. In the evenings there were interactive cultural sessions with the BSWG, including kinship systems, Aboriginal stories and damper making, as well as a bush medicine session. The main full-day program on day 2 involves rotating through a series of different 45-minute 'stations', each focusing on different aspects of remote health including the treatment of common conditions usually observed in remot settings. Students were divided into six interprofessional groups on day 1 and kept these groups for the different activities over the 3-day event. First-year NTMP students, nursing students from Charles Darwin University and allied health professional students on placement in the region at the time are invited to participate. The organisations listed above all host and supervise the student clinical placements, so are invested in these students being culturally safe in their practice.
Aim
Previous evaluations have looked at cultural immersion programs from a participant's perspective13; however, the perspectives of staff and the Aboriginal and Torres Strait Islander people involved has not been examined. This evaluation aims to report the views of staff and Aboriginal and Torres Strait Islander contributors relating to a cultural immersion program, as well as the student perspective.
Methods
At the conclusion of each RHE event, all student participants were invited to complete a questionnaire that evaluated individual sessions and the three main objectives of the RHE (Table 1). Participants were asked to respond to a series of statements, including 'I found this session valuable'. Responses corresponded with a five-point scale ranging from (1) strongly disagree to (5) strongly agree, with higher scores indicating stronger agreement. Similar feedback was also sought on the overall satisfaction with the weekend.
Qualitative data was sourced from four areas:
- Participants made written responses to open-ended questions about their experience of the RHE overall, and for each of the specific activities of the weekend, on the evaluation form.
- People who had attended an RHE as staff, including Flinders University employees, Indigenous Allied Health Australia members and employees, Batchelor Institute of Indigenous Tertiary Education employees, BSWG members, Charles Darwin University employees and clinicians from local health services in Katherine were invited to participate in one-on-one interviews. The interviews were audio-recorded and then transcribed.
- A staff evaluation survey was conducted in 2020, which included written responses to open-ended questions, and ethics committee approval was given for the results to be included in this study.
- Interviews and talking circles were conducted by Aboriginal members of the research team with members and families of the BSWG. Copies of all questionnaires, data collection tools and annual reports can be obtained from the corresponding author.
Table 1: Summary of data collection approaches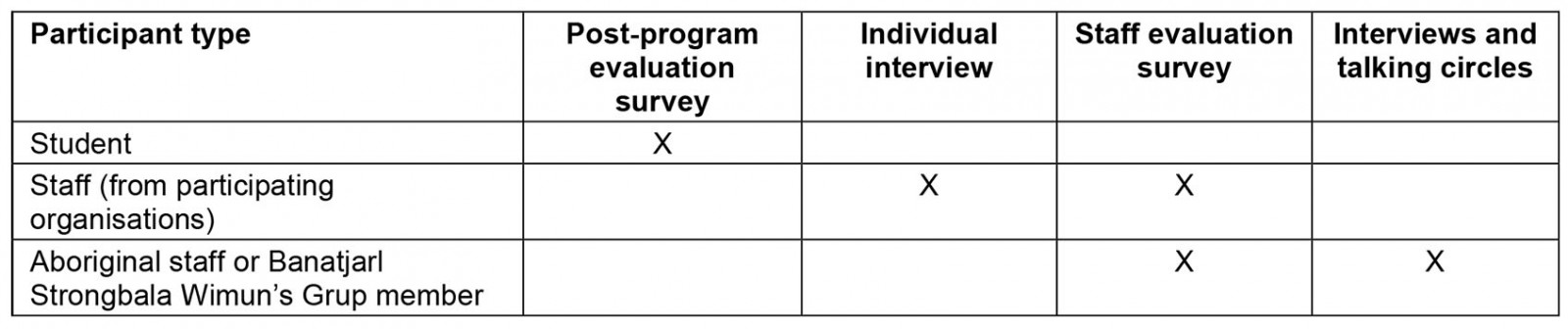
Analysis
Descriptive statistics (frequency, mean and standard deviation) were generated for the quantitative data using the Statistical Package for the Social Sciences v27.0.1 (IBM; https://www.ibm.com/au-en/spss). Student comments were analysed for each year by a research assistant using a thematic analysis approach, identifying major recurring themes. The text from both the staff and Aboriginal contributor interview transcripts and the 2020 staff evaluation survey were combined and thematically analysed. One member of the research team coded data and used an inductive approach to group under themes (LM). The first three themes were reflective of the questions asked, while the fourth theme evolved purely from the data. Another member reviewed codes and themes for accuracy (GR). Any disagreements were discussed, and a consensus reached.
Student survey completion
There were 138 students over 3 years who completed the evaluation form (2018–2020) with 45 (56% of attendees) in 2018, 33 (45% of attendees) in 2019 and 60 (80% of attendees) in 2020. Most students were female (70%) and non-Aboriginal (87%). Medical students formed the largest profession (n=58, 39%), followed by allied health students (n=23, 16%), Aboriginal and Torres Strait Islander health practitioner students (n=18, 13%), nursing students (n=17, 12%), pharmacy students (n=17, 12%) and clinical science students (n=5, 4%).
Staff participants
Seven staff members completed the 2020 staff evaluation survey and 14 staff members (including three Aboriginal staff members) participated in interviews, which were recorded using a mixture of Camtasia and Cisco Jabber. Staff interviews were transcribed using the Otter.ai v3.9.0 transcription program (Otter; https://otter.ai). Accuracy of transcriptions was checked by a researcher (GR) against recordings.
Three members of BSWG participated in the talking circles. These circles were recorded and transcribed by two Aboriginal researchers who spoke both English and Kriol, the language used by participants.
Ethics approval
Ethics approval was provided by the Flinders University Human Research Ethics Committee (No. 2199).
Results
Analysis of transcripts from staff interviews and text responses to surveys, identified four overarching themes: (1) understandings of remote practice, (2) Aboriginal culture, (3) working together and learning from each other, and (4) ongoing opportunities. The first three themes are consistent with the three key objectives and data from the quantitative results. Results from both qualitative and quantitative data will be presented under the four themes, with the station evaluations under remote practice, and overall satisfaction rates.
1. Understandings of remote practice
Ten-minute sessions on remote practice and the role of health professionals were presented by representatives of different health professionals (Table 2). Although ratings were strongly positive, these presentations were not as valued (ie had lower ratings) as the other more interactive sessions and stations, reflecting a tension between the content and the educational approach.
All the interactive clinical stations were highly valued (Table 3).
Table 2: Student quantitative ratings of understanding of remote health and professional roles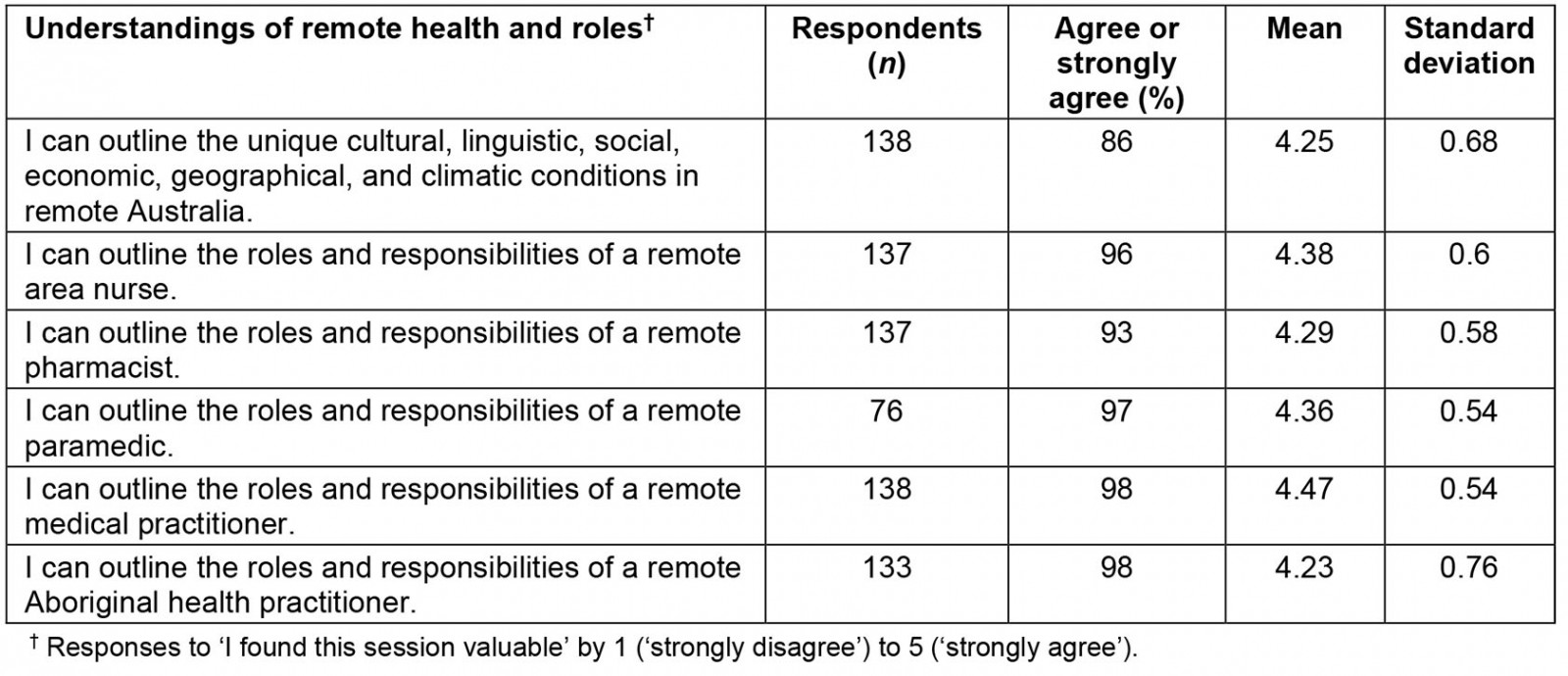
Table 3: Student quantitative ratings of the value of clinical stations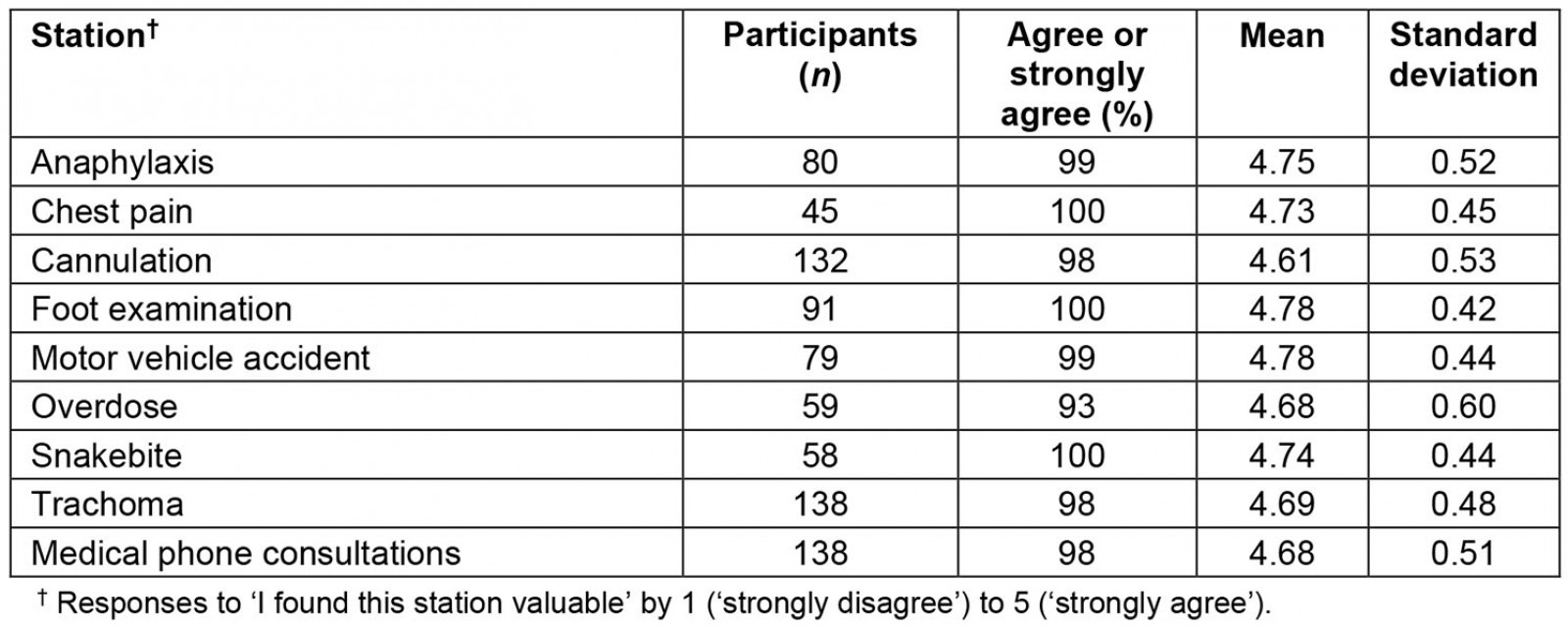
Student qualitative reponses: The introduction to remote health section helped set the scene for the different professional roles and introduced the idea of multidisciplinary roles and teamwork:
Getting to know about remote career roles of most health practitioners (and not just mine) allows me to understand the perspective of other health practitioners much better. (Student)
Definitely worth emphasising how all professions fit in – shows how complex it is. (Student)
Some participants were not aware of the role of the Aboriginal health practitioner or wanted more information on particular roles. Others felt there were too many professions covered and the content was not concise.
For the clinical stations, while some people had specific suggestions for improvements, most thought they were useful insights into remote health situations:
This activity helped me realise how vital it is to get necessary information fast over the long distances in the NT [Northern Territory] and how important it is to have the skills & training to think quick in emergencies. (Student)
Again – very practical and a great learning experience. Very relevant for the NT [Northern Territory] especially. (Student)
Staff responses: The weekend was seen as a positive way to introduce students to working remotely and provide some insight into the challenges and rewards involved. It was not considered to be definitive, as there are limitations to understanding through visiting as opposed to living in a remote context:
From my perspective I suppose as a facilitator of a field station, I think it's a great opportunity for students from a multi-faceted approach to sort of get together and experience not necessarily what would happen in a remote setting, but the situations that may arise. (Non-Aboriginal staff)
… they are able to get a glimpse of the rural and remote experience and to work with Aboriginal and Torres Strait Islander people. (Non-Aboriginal staff)
… the majority of students have limited experience thinking about health care in the remote context. So to take them away to a remote setting and have them physically thinking about it is a helpful way to add to their learning. (Non-Aboriginal staff)
With only 3 days allocated for the experience, there are limitations around how much can be taught about working and living remotely, and this was conveyed in the participant responses:
W[h]at's happening for us is [y]ou're coming to have a glance of our lived experience. We live this every day. You know, people that visit are not living this every day. So t[h]ey're there to do a job and then go. But you know, how do you convey that? How do you get that across? (Aboriginal staff)
… possibly (include) something on what people do, outside of work, to survive and thrive in remote areas (what do we possible [sic] do without large malls?) (Staff evaluation survey)
Several participants suggested including a visit to a community health centre but understood that this would not be practical with the large numbers of students, time limitations and travel that would be involved.
… if we could organise a group trip to a reasonably close by community such as Barunga, for example, it would give them a bit more of a sense of what remote living is really about. Like, is there a shop out there? Or, if there is, it's a very small, yes, small general store. But t[h]at's it. And realistically, they have to go all the way into Katherine to get anything of … anything substantial. So I think, you know, perhaps a day trip out to a community although difficult with a large group and in buses. (Non-Aboriginal staff)
2. Aboriginal culture
Student quantitative responses: Aboriginal and Torres Strait Islander students included Aboriginal and Torres Strait Islander health practitioner and allied health students and a few medical students. Evaluations were strongly positive (Table 4).
Table 4: Student quantitative ratings of Aboriginal cultural learning†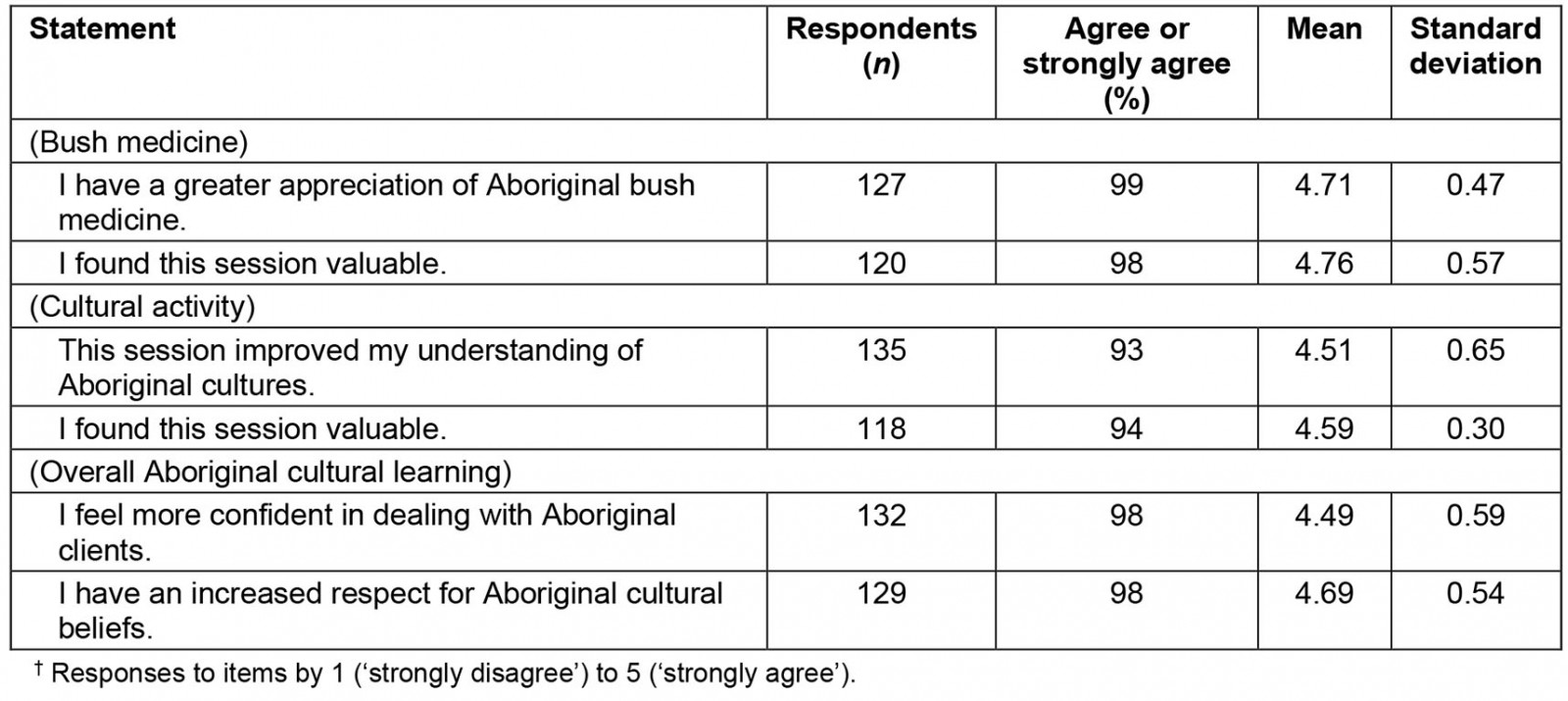
Student qualitative responses: The cultural activities and discussion of kinship were highlights of the weekend, although some participants struggled with the complexity of the kinship system and wanted it earlier in the weekend:
Extremely valuable session. I definitely have a better understanding of the complexities of kinship now. One of my favourite/most educational sessions. (Student)
It was great to listen to the stories. However, it would be better if we could interact or involve more with the Elders to increase our engagement with the story. (Student)
By far my favourite part of the trip was the Aboriginal cultural learning and listening to the Jawoyn ladies. (Student)
I am more confident in dealing with Aboriginal clients than before. (Student)
Aboriginal and Torres Strait Islander participants particularly valued the cultural components and respect shown to the Jawoyn presenters:
The Dreamtime stories were amazing. It reminded me of being home with my grandmother and I think it was received really well.
Staff qualitative responses: Staff participants saw great value in the inclusion and embedding of the BSWG and their families throughout the weekend. The sharing by the group of their local stories, a welcoming smoking ceremony, damper-making activities and bush medicine demonstration provided insights into current culture that benefited both staff and students:
I mean, the stories that she [Aboriginal Elder] told us that that night, it was a fantastic night … And then we had, we prepared some damper in the night … they were making damper and we were around that fireplace … Yeah, that learning you [c]an't get in a lecture hall. (Non-Aboriginal staff)
Although it sometimes challenged some students to step outside their areas of comfort, some activities – for example protocols that required students to take turns to serve meals to the Aboriginal Elders and families – were seen as positive learning experiences.
Listening to the presentations and participating in more casual conversations was thought to provide the non-Aboriginal staff and students with better understandings of their Aboriginal clients and co-workers.
And listening to some of the Elders explain some stories and how they found some parts of healthcare quite challenging, especially when they have a lot of family members who come into hospital and t[h]at's, you know, not that … it's quite unusual for, you know, patient in the public health setting, I think, to have like, a lot of … more than one relative visiting at the time. (Non-Aboriginal staff)
… what they say started last year and have improved on this year with the kinship system and obligations and stating that for Aboriginal people in their community we don't start at eight and finish at 4:21 we work 24 seven. So, our obligations to the job and then family members and extended it goes all hours, you know, sometimes we [d]on't get rest. (Aboriginal staff).
The members of the BSWG described enjoyment and pride in sharing their culture and knowledge during the Remote Health experience.
… yeah it was good um, meeting new students, yeah, and doing smoking and all that. Yeah, we had to go in the houses, doing smoking, the ladies. Me, [P1] and [P2] … Yep, we did it in a good way, so people can you know, sleep properly, yeah. (Banatjarl woman)
Ah, he gud wan that wan. [It's good the story telling session.] Yeah, we all you know, coming together. Then talking together about old people issue, especially about telling about our old people [inaudible] … and the land that we lived in and we share everything you know. (Banatjarl woman)
Over time, the RHE has evolved to increasingly include Aboriginal and Torres Strait Islander culture, workforce and health consideration throughout all components of the 3 days. This was invariably seen as a positive move that should continue to develop while being aware of the added responsibility and pressures this may add to Aboriginal and Torres Strait Islander people involved.
By having more Aboriginal and Torres Strait Islander students, staff and facilitators this will make it a safer space for learni[n]g – while remembering that it's not an Aboriginal per[s]on's job to educate you. (Staff evaluation survey)
3. Working together and learning from each other
Many of the activities, including all the stations, involved interprofessional groups not just learning together in the same room but interacting as a team (Table 5). Students tended to focus on their professional learning whereas some were able to appreciate the additional value of reciprocal learning from both a professional and social aspect.
Table 5: Student ratings of interprofessional learning†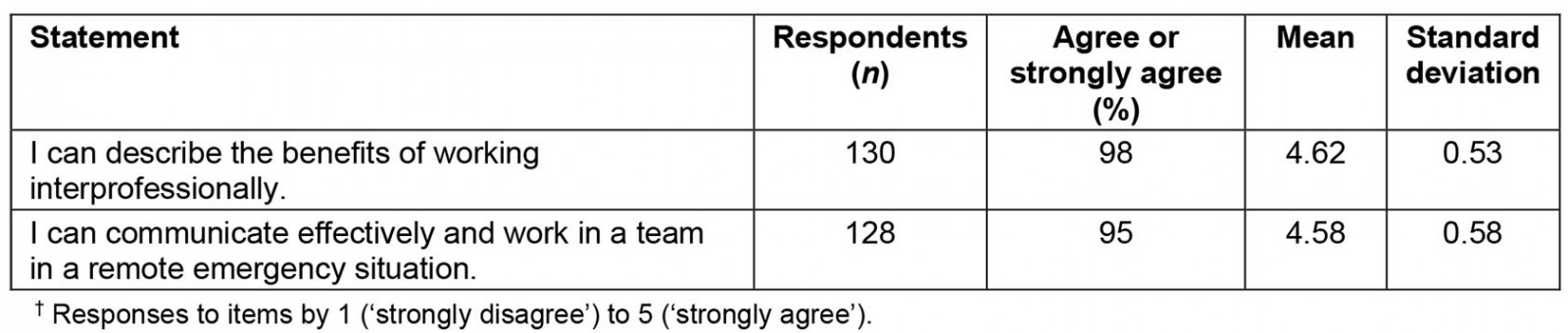
Student qualitative responses: Students appreciated learning about other professional disciplines, and the benefits of working together, and how important that was in a remote setting.
Learnt a lot about other professions and the benefits they provide when dealing with patients. (Student)
Liked how many disciplines were present and how all the workshops showed how interprofessional collaboration is important for remote medical practice. (Student)
Staff qualitative responses: Staff and BSWG members described many benefits of reciprocal learning and understanding between different group pairs ie student–lecturer, Aboriginal–non-Aboriginal, discipline–discipline, remote experience–metropolitan experience. The learning they described was both professional and social, with opportunities for both to be purposefully integrated throughout the RHE.
Positive on the first day, when they see professionals, again, in this setting, where we're not just introducing what we do out there, but when the panel comes together, that's very positive, because they can see how we, ourselves as professionals that have had the experience, how we complement each other's roles, that's very positive. (Aboriginal staff)
im rili gud wan [It's really good], for all of us you know. To learn more and get more information from it. We can tellim bla we people alabat [We can tell everyone about our people, Aboriginal people], what's happening you know Flinders mob [NTMP] you know and we all getting involved in that. Im gud that wan. (It's really good). (Banartjarl woman)
As well as shorter term social interactions, longer term relationship building between the university, other organisations and the local community was considered a critical component of the continued success of the RHE.
Typically, the mob that comes down from Barunga, and just being able to have time to listen and to make connections with them and then form relationships … and the consistency of having the same, some of the same, facilitators and staff return each year, it means that there's now a working relationship between organisations, such as IAHA [Indigenous Allied Health Australia] and the universities, which I think has provided some continuity and the ability to sort of reflect and then improve on things each year. (Aboriginal staff)
4. Ongoing opportunities for students
Several participants suggested that there should be some consideration of 'what next' for those students who, because of attending the RHE, had developed an interest in practising in remote areas. Integration into an ongoing program of cultural and interprofessional learning would be desirable. They suggested that there would be benefit in providing these students with information on employment opportunities and ways of initiating, or remaining in, contact with others who have similar interests.
For the third-year students, we often talk about grad[uate] programs. But like I said, they're always in acute areas. I think it would be good to talk to them about remote health. (Non-Aboriginal staff)
I don't know whether or not there should be things like, you know, at the end, give them information about other events that are similar or they can join into, or you know, like is, there webinars that they can all join up and be a part of and still follow this type of teamwork. (Aboriginal staff)
The medical students attended the RHE early in their first year of a 4-year graduate program. The other professionals were in their later years and generally more experienced. Often the most experienced health professionals were the Aboriginal and Torres Strait Islander practitioners. This was a deliberate strategy of the organisers to prevent power imbalances among the professional groups. The majority of students felt the course was at the right time in their careers. Generally, most felt it was not too early or too late (Table 6).
Overall satisfaction with the RHE was very high. The student assessment of the contributions made by the facilitators was not as high but still positive (Table 7). It should be noted that most facilitators were volunteers who gave up their time to contribute to the RHE.
Table 6: Student ratings of the timing of the Katherine Remote Health Experience†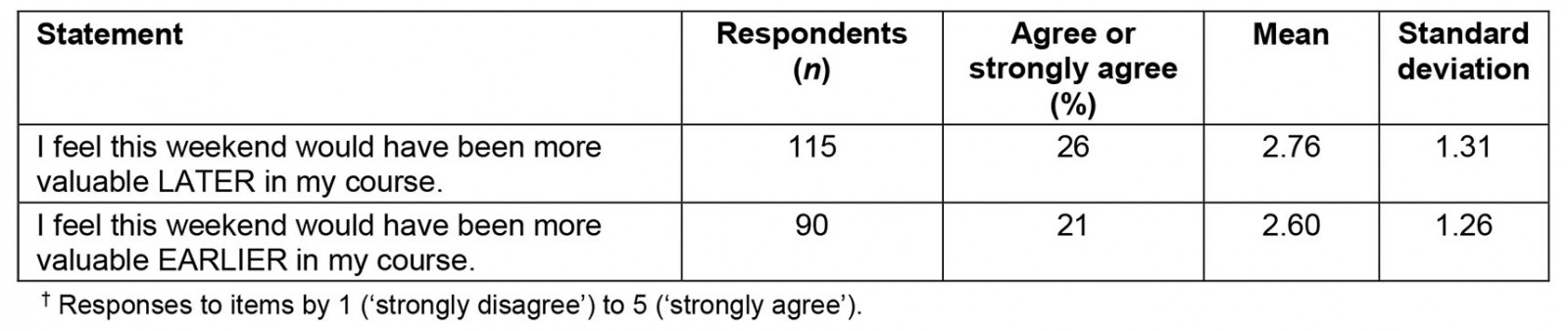
Table 7: Student ratings of overall satisfaction with the Katherine Remote Health experience†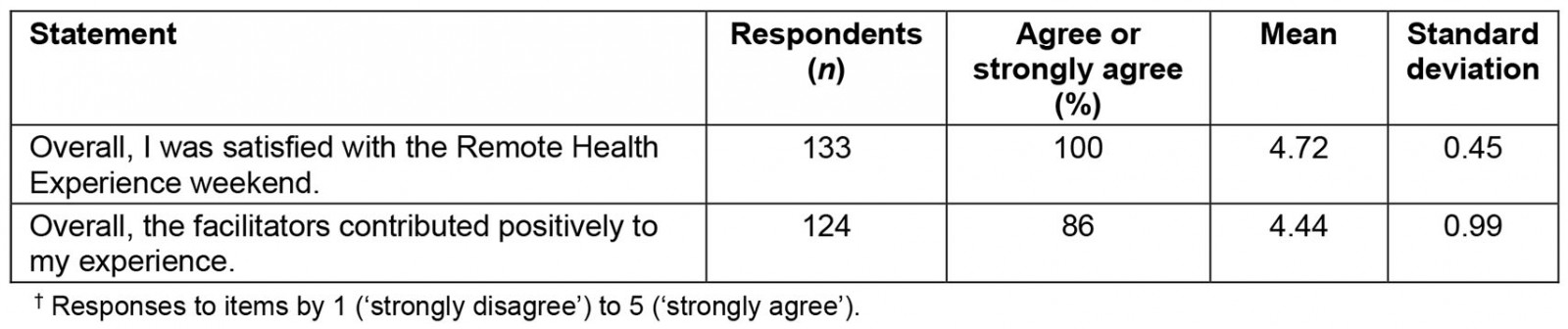
Discussion
The results indicate that the student participants and staff (including the Aboriginal staff) highly valued the RHE, with consistently high ratings of each of the components, especially the interactive sessions, and the experience overall. For many of the students this was their first exposure to the idea of working in a remote setting and what it might involve, and there is potential for an ongoing program of cultural and interprofessional education. The positive feedback is consistent with that of evaluations from other cultural immersion programs where the 'storytelling' was rated as the 'best thing' along with learning about culture12,13.
The Katherine RHE successfully combined both cultural and interprofessional immersion in a remote context. Interprofessional immersion programs have been implemented in Australia20,21, but less common is the cultural immersion component13,22.
While a cultural immersion program may be an important aspect of developing an understanding of remote health among students, by itself it may not be enough to support and attract health professionals to work in a remote setting15. Additional orientation and preparation before the RHE, and ongoing support after the experience, are needed to support the career direction of the multidisciplinary health students in attendance. These support strategies included ongoing Aboriginal cultural education, providing more detailed professional education about common remote health scenarios and bilingual communication. Understanding how to engage Aboriginal health workers, Aboriginal community workers and Indigenous interpreters in the remote health setting is also important. A clear and supported professional pathway to working remotely needs to be established17.
The RHE was designed to improve interprofessional communication and respect for other professions. All activities combined students from various professions and with a range of experience and focused on team problem solving and respect for team members. The strategy of mixing first-year medical students with more experience allied health and nursing students was an attempt to break out of the outdated traditional 'medical dominance model' of perceived hierarchy, which overemphasises the importance of doctors in a multidisciplinary team and introducing a power differential not conducive to interprofessional education teamwork23-25. This is a paradigm shift that has been understood since the 1970s, if not before26. In a remote setting there may not be a medical doctor available, or there is only one doctor covering a large geographic area, and health professionals need to complement each other's skills and work together to maximise patient outcomes, which is why interprofessional practice is so important. Also, timing of the RHE in terms of professional development is important, as in earlier years premedicine clinical science students were invited, but there was a consensus by the RHE organising committee that the experience was too early in their careers.
Embedding the BSWG members into the entire 3-day program was vital for fostering an interprofessional environment by creating a two-way learning situation27. Respect for and valuing of Aboriginal ways of knowing, being and doing and the knowledge of Aboriginal health practitioners was given space to blend with western medicine approaches.
This cultural input from the BSWG members, as well as the teaching input of the Aboriginal staff, was important for improving understanding and confidence in working with Aboriginal clients, and for creating a culturally safe environment9. Many of the health professional student participants had come from major cities and not had any close contact with Aboriginal and Torres Strait Islander peoples at all. The cultural divide can be very significant, and having direct contact is important for breaking down myths and misconceptions28.
Strengths and limitations
A strength of this evaluation is the collection of student data over 3 years, creating a robust assessment of different student cohorts. The collection of qualitative data from staff, students and Aboriginal people gives a full picture of how the remote health experience was perceived. The results are consistent with the program evaluation reports from the beginning of the program, with partner organisations demonstrating their appreciation of the value of the program by returning each year. Two local Jawoyn women are co-authors of this manuscript. A possible limitation of the study is that pre- and post-data were not collected. It would be instructive to follow up participants to assess the impact of the experience on their attitudes and professional practice.
Conclusion
The Katherine RHE has been a valuable learning experience for medical and health professional students over the past 10 years. It has contributed to an improved understanding of what remote health is, of interprofessional work practice, and of working with Aboriginal and Torres Strait Islander peoples. It is an important element of what needs to be a supported pathway into working in a remote context.
Acknowledgements
Thanks to Sarah Chalmers, Tim Earnshaw and Pascale Dettwiller for leading the original program and bringing together the partners. A special thanks to the members of the Banatjarl Strongbala Wimuns Grup who have consistently participated and provided the critical cultural education that has made the program so effective. Thanks also to the many volunteers each year who have made events go smoothly.
References
You might also be interested in:
2008 - Attracting psychiatrists to a rural area - 10 years on




