Introduction
Stress is a phenomenon that accompanies everyday life. Stressful situations activate both the central and peripheral nervous systems. The response of the central nervous system is the activation of the hypothalamus and brain stem, whereas the peripheral nervous system responds with the activation of the hypothalamic–pituitary–adrenal (HPA) endocrine axis and the autonomic nervous system (ANS)1. These systems interact with the immune system, therefore they are closely involved in the pathogenesis of stress-related diseases2. The distinct components of HPA are also under the control of various structures of the central nervous system, as well as of a wide variety of signal molecules and neurotransmitters3.
Salivary α-amylase (sAA) is an enzyme released in saliva during food consumption. Recent studies report that the levels of sAA are an adequate marker of stress-related changes in the activity of the ANS4,5, and the quantity of the enzyme in saliva is connected with mental health and stress6,7. The concentration of sAA does not depend on the quantity of saliva and it is considered as a readily accessible, non-invasive parameter to measure the individual levels of stress8-10.
Cortisol is a steroid hormone released from the cortex of the adrenal gland. It is assumed that the levels of the salivary cortisol correlate with the levels of cortisol in blood11. Therefore, the measurement of the levels of the salivary cortisol appears to be a convenient, non-invasive method to assess the levels of physiological stress and the adaptation of the HPA to stress12.
It has been reported that isolated societies that inhabit rural areas and have strong beliefs are less predisposed to chronic stress and the development of stress-linked disorders like coronary-heart disease13,14. On the other side, healthcare workers belong to a specific group that is constantly exposed to a large number of mental-health-affecting risk factors such as a risk of infections, physical fatigue, long working hours, and unpredictable and difficult-to-control situations.15,16. All these findings were used in the present study to evaluate the development of stress among general practitioners (GPs) who work in rural, sparsely populated regions in the Republic of Bulgaria. The study is based on the determination of the stress marker molecules sAA and cortisol in saliva samples, as well as on a questionnaire that tries to characterize the everyday life of the healthy participants in the research.
Methods
The study design and the questionnaire were presented to 128 GPs. The aim of the questionnaire was to assess their health conditions, habits, priority objectives and interests, as well as their moral and ethical relationships with patients. The main inclusion criterion was the population of the inhabited area. A town or village with population less than 5000 people and poor infrastructure, large distance from a municipal town and/or main road was considered as rural. The participants had to be free of psychiatric and somatic diseases. The exclusion criteria were the intake of medications that could affect the work of HPA, night-shift work, recent exposure to a high-risk situation and/or family conflicts. These requirements were covered by 40 people who took part in this research (n=40, mean age 55.92±8.8 years).
Since the activity of the sAA and cortisol show well described diurnal secretion17,18 four samples from each participant were collected: one on a Monday morning, at the beginning of the work day (between 7.00 and 8.00 am) and another at the end of the same day (between 5.00 and 6.00 pm). This procedure was repeated on Friday, the same week. All samples were collected by participants chewing cotton rolls, and placed in salivettes. The procedure was maintained in accordance with the manufacturer instructions and recommendations, avoiding the effects of food, drink, toothpaste and nicotine.
Blood pressure and pulse were measured after the salivary samples were collected. After centrifuging, the salivary samples were stored in Eppendorf test tubes at –80°C. The ELISA method was used for the quantitative determination of the sAA and cortisol levels in saliva.
All samples were brought to room temperature (mean temperature 22±2ºC) and centrifuged on the day of analysis. The laboratory tests for salivary α-amylase (Alpha-amylase saliva ELISA, BioVendor; https://www.biovendor.com/file/6286/RTC020R Alpha-Amylase Saliva ELISA.pdf) and cortisol in saliva (Human cortisol (saliva) ELISA, BioVendor; https://www.biovendor.com/file/9028/BV-MSDS Cortisol (Saliva) Human ELISA RCD005R_V9.0 04.05.2020.pdf?version=202105140836) were performed in accordance with the manufacturer recommendation. All samples of one person were analyzed in the same run. All samples were measured in one day.
The collected data were processed and analyzed using the Statistical Package for the Social Sciences v19.0 (SPSS Inc.; http://www.spss.com). The results were compared using the paired samples t-test and presented as mean±SEM. p values less than 0.05 were assumed as statistically significant, 0.05>p<0.1 as a trend and p>0.1 indicates insufficient difference.
Ethics approval
The study was performed in accordance with guidelines for research studies performed on humans. An informed consent was obtained from each of the participants. All necessary documents and the study design were present and reported to the ethics committee of the Medical University of Plovdiv (resolution of the ethic committee of Medical University-Plovdiv P-1122/23.04.2021).
Results
Changes in enzyme activity of salivary α-amylase
Results showed that the morning samples were characterized by lower activity of the enzyme sAA compared to the afternoon ones, although significant difference was observed only for the samples collected on Friday (p=0.246 for the Monday samples and p=0.018 for the Friday samples) (Fig1).
This dependence was established when all data collected from all participants were compared without any division based on their habits. However, interesting results were observed when results were separated and compared by groups (Tables 1, 2).
It was established that the morning values were without any difference in general (p=0.947). When separated in groups and subgroups, men who avoided smoking (n=12) showed no statistical difference but a slight tendency or trend to have lower levels of the enzyme on Monday morning (p=0.069). The afternoon samples on Monday showed the same slight tendency (p=0.069). The comparison between the morning and afternoon values for smoker/non-smoker groups showed no statistical difference (p>0.1). An almost identical situation was observed in the group of men who practiced sport for more than 150 minutes a week (n=7). The detected enzyme activity in the morning was statistically lower in the participants who practiced sport compared to the participants who did not (p=0.036). The afternoon values were without statistical difference, but tended to be lower in the group with participants who practiced sport (p=0.058). All these statistical dependences were not observed at the end of the work week. The afternoon enzyme activity in the participants engaging in sport compared to those who were not showed only a slight tendency (p=0.09 for the morning and p=0.068 for the afternoon values). The consumption of alcohol (n=9) did not determine any statistical differences between the groups (p>0.1).
Women showed similar results to those of men. Women who smoked (n=8) tended to have higher sAA activity on Monday morning compared to women who did not (p=0.08). This tendency had stronger evidence for the afternoon samples (p=0.014). The results obtained from the Friday samples showed that women who did not smoke tend to have lower sAA in the morning (p=0.089). No statistical difference was detected when the afternoon samples for these groups were compared (p>0.1).
Neither statistical difference nor tendency were detected when the groups of women who practiced sport (n=12) and those who did not were analyzed (p>0.1). The consumption of alcohol (n=7) did not determine any statistical differences between the groups; similarly for the results obtained for men (p>0.1).
Despite the fact that the studied samples of all participants showed the normal diurnal changes17 in the levels of sAA on Friday, but not on Monday, no statistical differences were detected when comparing the values within any of the analyzed groups and subgroups (p>0.1) (Tables 1, 2).
Table 1: Comparison of levels of salivary α-amylase and cortisol in male study participants, based on habits and everyday life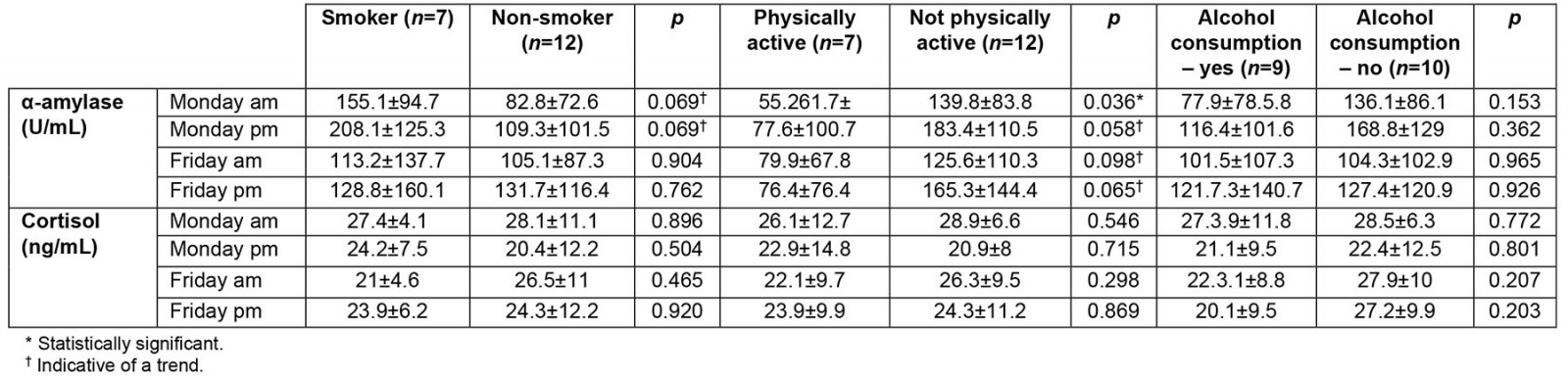
Table 2: Comparison of levels of salivary α-amylase and cortisol in female study participants, based on habits and everyday life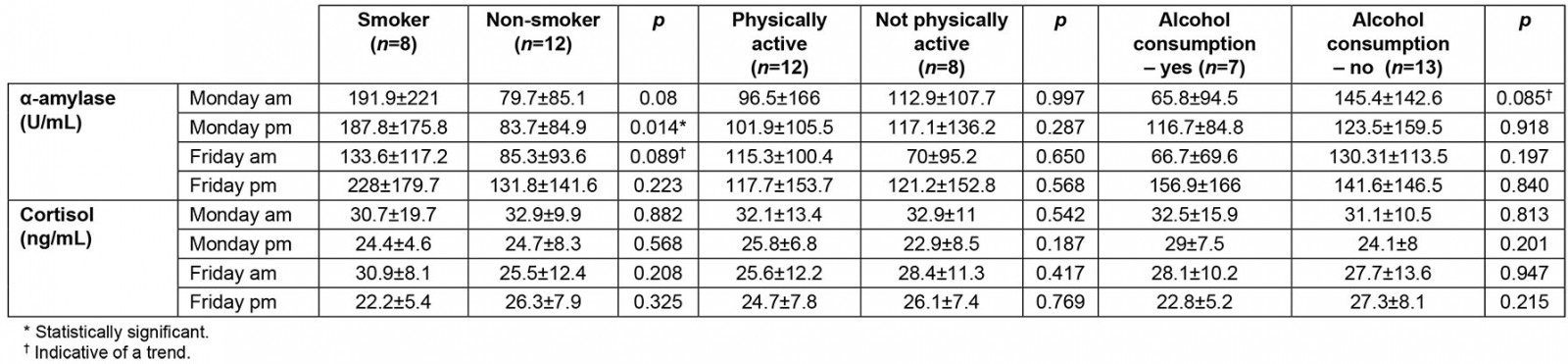
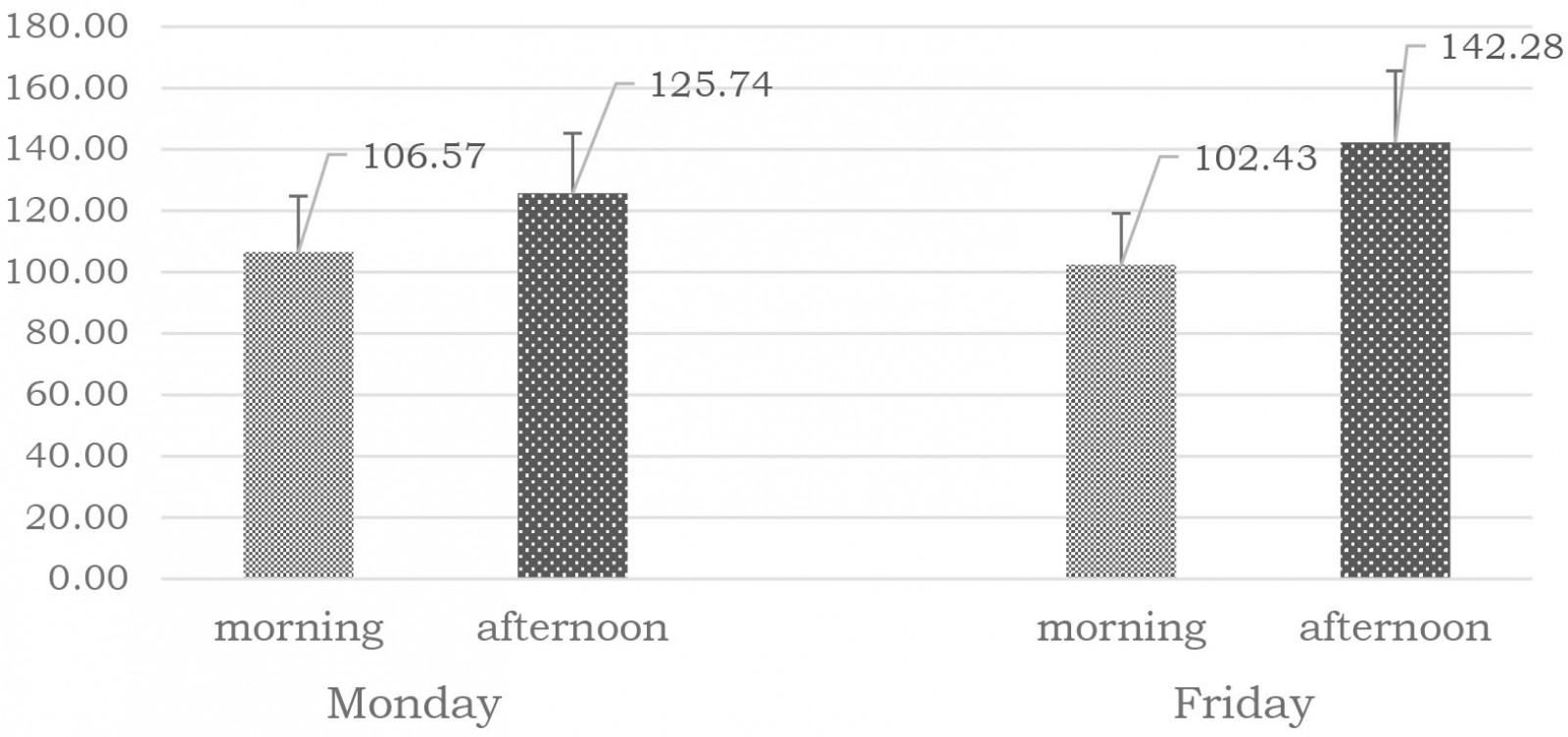 Figure 1: Activity (U/mL) of α-amylase in saliva (mean±SEM) of study participants.
Figure 1: Activity (U/mL) of α-amylase in saliva (mean±SEM) of study participants.
Changes in levels of cortisol
The levels of cortisol detected in all samples showed a statistically significant decrease on Monday afternoon, compared to the morning of the same day (p=0.006; * in Fig2). This dependence was not detected for the Friday samples (p=0.510). The levels of cortisol, measured only for the morning samples, showed a decrease at the end of the week compared to the beginning of the week (p=0.033; # in Fig2). A statistically significant difference was not established when the afternoon samples were compared (p=0.553) (Fig2).
Analyzing the results in the same way as for sAA, dividing the participants in the same groups and subgroups and comparing them, demonstrated a lack of statistical significance (p>0.1; Tables 1, 2).
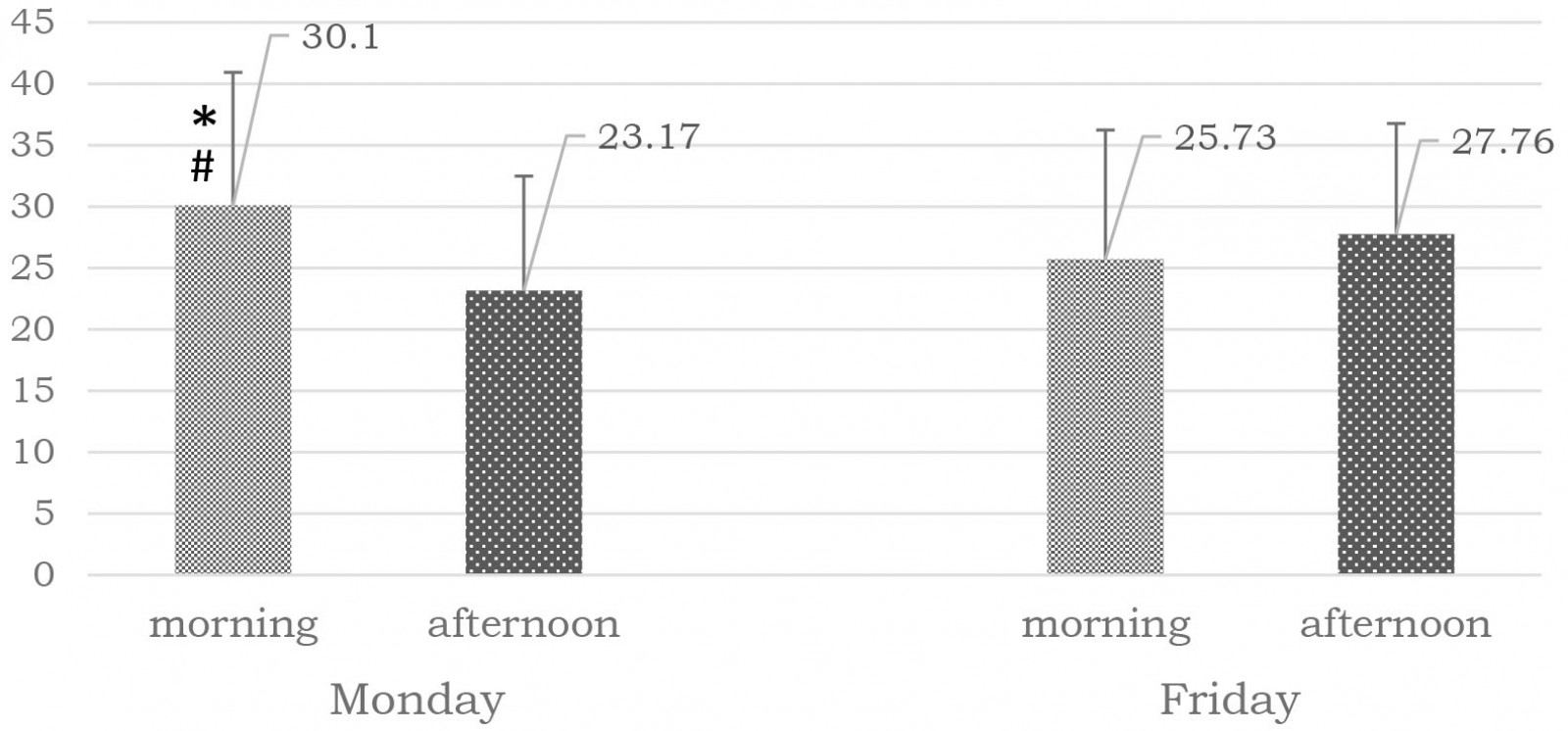 Figure 2: Cortisol levels (ng/mL) in saliva (mean±SEM) of study participants.
Figure 2: Cortisol levels (ng/mL) in saliva (mean±SEM) of study participants.
Influence of physical activity on the studied parameters
Half of the GPs (n=19; 7 men and 12 women) who took part in this research practiced sports for more than 150 minutes a week. The results showed that in general the physical activity did not affect the levels of sAA or cortisol (p>0.1). The only exception observed was in the levels of sAA on Monday. It was established that sport in general affects the overall sAA levels. They were lower in the group that practiced sports (88.07±22.06 U/mL) compared to the group with reduced physical activity (174.27±31.84 U/mL; p=0.032). This dependence was also detected when those who practiced sport were compared within the distinct groups (Tables 1, 2).
Influence of smoking
Our experimental group included 15 GPs (seven men and eight women) who were smokers, smoking more than five cigarettes a day, and 24 smoking five or fewer cigarettes a day. The analysis demonstrated that smoking affected the levels of sAA only. The levels of sAA on Monday afternoon (224.87±46.73 U/mL) in the group of smokers were statistically higher in comparison with those of the non-smokers (92.99±17.2 U/mL; p=0.002). An additional division of the participants into groups and subgroups and comparing these did not demonstrate any other significant differences (data not shown).
Influence of alcohol consumption
Participants who consumed alcohol more than once a week, drinking a volume of more than 300 mL of red wine or its equivalent, were considered as alcohol-consuming. It was established that alcohol consumption affects the activity of sAA only. The participants who declared alcohol consumption (n=16; 9 men and 7 women) had lower sAA values (45.9 U/mL (95% confidence interval (CI) 28.31–116.8)) than those classed as non-consumers (74.85 U/mL; 95%CI 88.27–194.91; p=0.036).
No other dependence was found, although additional comparisons were made (data not shown).
Because levels of sAA on Monday morning is the only parameter with abnormal distribution, these data are present as median and 95%CI.
Changes in blood pressure as a marker for assessment of daily stress level
Systolic and diastolic blood pressure showed neither significance nor tendency when comparing the beginning and the end of a week (p>0.1). However, diastolic blood pressure itself showed significant changes at the end of the week. Friday afternoon results were significantly higher than the morning ones (p=0.04; * in Fig3). On Monday afternoon both the systolic (120.9±12.2 mmHg) and diastolic (74.5±6.5 mmHg) blood pressures were lower in the subgroup of men who are not physically active, compared to those who practiced sport (135±5.7 and 81.4± 3.7 mmHg; p=0.028 and p=0.05, respectively).
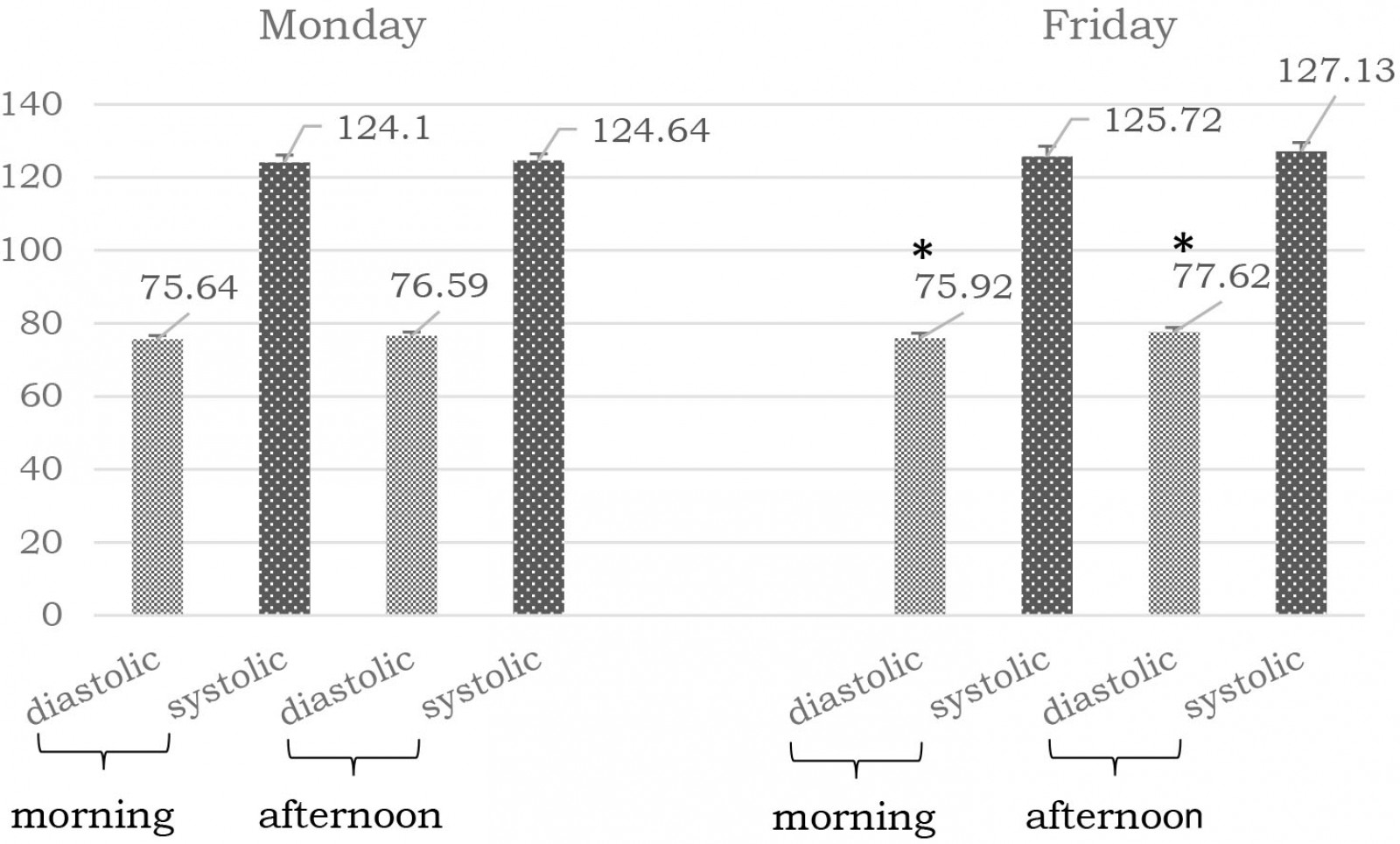 Figure 3: Blood pressure (mean mmHg±SEM) of study participants.
Figure 3: Blood pressure (mean mmHg±SEM) of study participants.
Changes in heart rate as evidence of stress development among GPs
A statistically significant increase in heart rate was determined on Monday afternoons in comparison to Monday mornings (p=0.001), as well as on Friday afternoons in comparison to Friday mornings (p<0.0001). Values for heart rate also show significant differences by sex in the studied group of physicians, with significantly higher values measured in men compared to women (p<0.05). No statistical difference was found when groups and subgroups were compared (p>0.1).
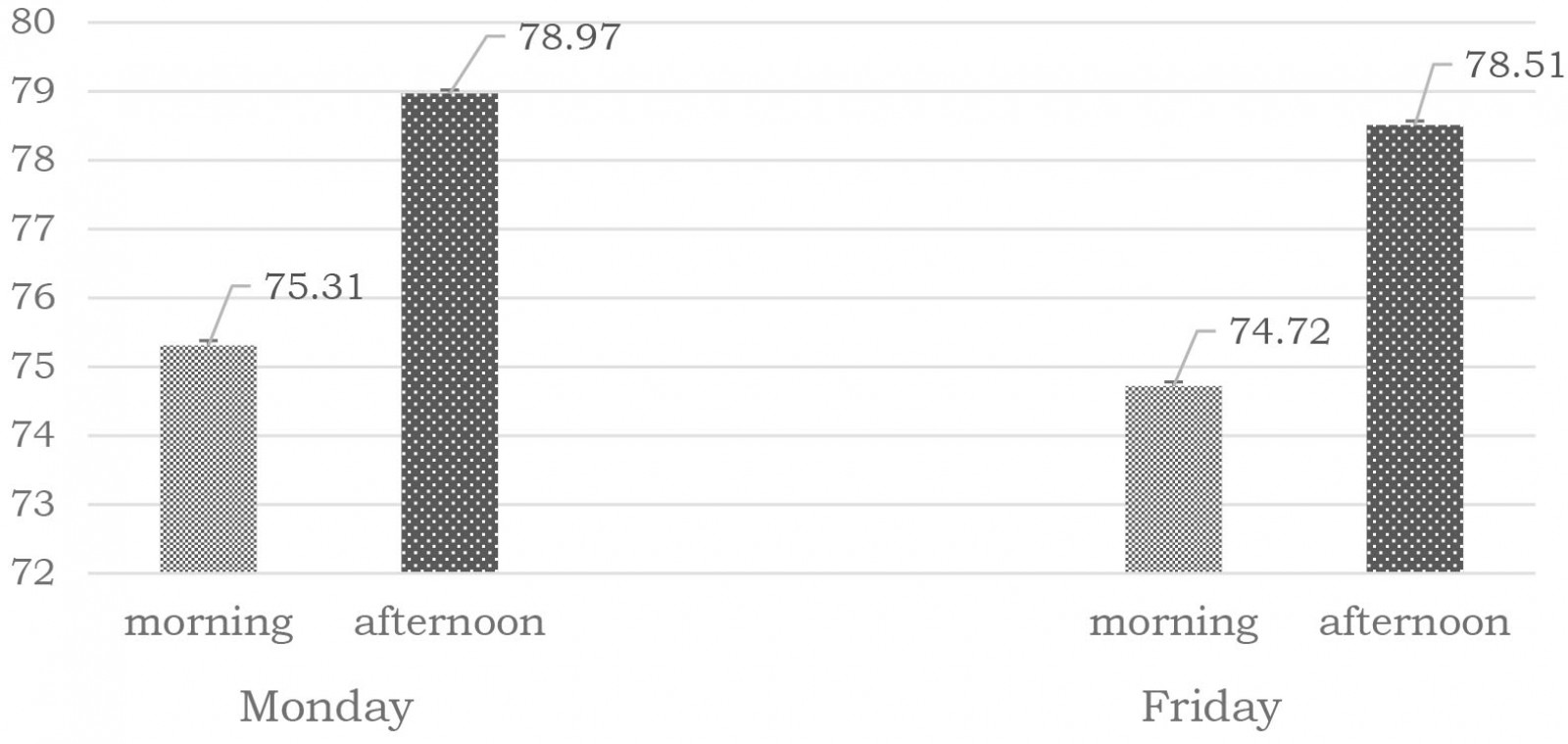 Figure 4: Heart rate (mean beats per minute±SEM) of study participants.
Figure 4: Heart rate (mean beats per minute±SEM) of study participants.
Discussion
The present study design hypothesizes that changes in levels of sAA and cortisol happen because the professional life and routines of the GPs can lead to the development of chronic stress.
Attempts to find the connection between hormonal changes and stress marker molecules provide controversial information. Many authors have reported a connection between the levels of catecholamines and the enzyme activity of sAA. Their articles state that the changed levels of the enzyme are the result of the changed hormonal environment19-22. Other authors assume that the sAA levels depend mostly on the work of the ANS. The acinar cells in the salivary glands are innervated by sympathetic and parasympathetic nerves, which regulate the release of sAA23. Thus, under conditions of psychological stress, the activity of the ANS increases and the levels of sAA increase. Nater et al reported that sAA increases very soon after the increase in the levels of adrenalin and noradrenalin. It seems that the changes in the sAA levels are the result of the activity of both ANS and HPA, providing information about their work and, respectively, the development of stress24.
It is important to know the diurnal changes in the levels of sAA in order to use it as a marker molecule to evaluate stress development17. The present study demonstrated that within the whole experimental group the diurnal course is more pronounced on Friday rather than on Monday. Moreover, participants comprised middle-aged GPs where the daily diurnal course tends to be less pronounced17. Based on this, the authors speculate that the Monday values are more likely to be the result of normal activity of the ANS and/or hormonal changes. The significantly higher levels on Friday with much clearer increases during the late hours of the day are evidence for an increased activity of the system. At the same time, no statistical difference was found when comparing the activity of sAA within the smaller subgroups, where the GPs were divided on the basis of their habits and everyday life.
Despite the fact that the detected afternoon enzyme activity was higher as an absolute value in these groups and subgroups, the lack of a statistically significant difference shows that the diurnal course is impaired, thus the organismal adaptation mechanisms to stress are also disturbed. The levels of sAA do not show significant elevation, but this could be due to single, mildly stressful situations rather than to chronic stress17.
The data obtained from the present experiment show that the professional life of the GPs is accompanied by stress development. This is the result of their everyday routines and engagements. It has been reported that psychological stress prevails in individuals who are in the middle of their professional life23, although other studies have reported an increased stress among younger specialists, with less experience25. A fast increase in the sAA levels has also been reported for individuals positioned in stressful environments such as those of skydiving, watching stressful video materials, psychosocial stress and waiting for surgery26,27. The present study shows that the work in peaceful and rural areas could also be considered as a stressful environment, although the levels of the sAA do not indicate acute stress.
The activity of the HPA is characterized by a well-depicted circadian rhythm. It is explained by an increase in the levels of cortisol early in the morning after waking up – a cortisol awakening response – followed by a gradual decrease during the day18. The constant exposure to stressful stimuli leads to the development of chronic stress and disturbance in this diurnal course28. At the same time, the activity of the HPA could be affected by various stressful situations where the degree of activation depends on the psychological components of the situation – such as unpredictability, uncontrollability, expectations and habits29.
The present study is based on the measurement of the morning and afternoon levels of cortisol30 in order to evaluate the development of stress.
The researchers in the present study established the normal diurnal cortisol course only on Monday and only when all samples were used in the statistical analysis. That is reason to speculate that the weekend could affect the restoration of the normal activity of the HPA. The levels of cortisol on Friday were higher as a value but without any statistical difference. This indicates a disturbance in the activity of the HPA and probably the development of chronic stress. The same dependence was detected when comparing the levels of cortisol within groups and subgroups. The lack of the circadian rhythm demonstrates that the activity of the HPA is disturbed by the everyday routines of the participants. This fact could be also explained by experiments made by Fernandez-Sanchez et al, whose findings support the idea that the cortisol levels vary and they depend on the stress levels and the duration of the situations31. They demonstrated that when the stressful situations are very strong and prolonged, leading to the development of burnout syndrome, levels of cortisol may remain unchanged and very close to those in healthy people. They also demonstrated that sometimes the levels of cortisol are extremely high, a result that indicates the development of acute stress31, whereas the levels detected in the present study indicate low-grade chronic stress.
Another possible explanation for the present study’s results is a normal night’s sleep, which is necessary for the maintaining of the circadian rhythms. It also aids homeostasis and adaptive mechanisms32, and hence it reduces the development of stress. This supports the study results showing a better working HPA at the beginning of the week compared to the end of it. The lack of information about the sleep habits of the participants could be considered as a limitation of this study. However, some of the studied parameters affect normal sleep.
Physical activity and stress
The present study data show that physical activity barely affected the levels of both marker molecules. The only dependence found was that the base levels of sAA are lower in those who practice sport. The researchers also detected a tendency for these diurnal changes to be closer to the normal course, but without statistical difference. This observation was more pronounced at the beginning of the week, showing that there might be a dependence among many factors within the weekend. Although the present findings do not provide clear facts about the beneficial effect of sport over the stress development, several studies have reported that there should be such effects, as well as effects on the development of health-threatening conditions such as obesity, diabetes and high blood pressure33-36.
Influence of smoking on activity of HPA and response to stress stimuli
Nicotine exerts a stimulatory effect on dopaminergic, cholinergic, noradrenergic and serotoninergic receptors37,38, as well as on HPA39,40. HPA could be activated through irritation of cholinergic receptors of the hypothalamus. This activation leads to the release of corticotropin-releasing factors. In turn, this activates the enzymes that split proopiomelanocortin to produce adrenocorticotropin and β-endorphins.
Smoking is also related to sleeping problems and stress development41. The influence of nicotine on sleep is due to the effects of nicotine on the central nervous system, as well as on HPA42. It could be assumed that such an influence could lead to changes in synthesis and secretion of the sAA and cortisol. Smoking disturbs normal sleep, leading to disturbances in circadian rhythms and the mechanisms that maintain homeostasis and adaptation to the environment32, including the response to stress factors.
Sleeping problems have an influence on the neuroendocrine systems, stress development43 and the levels of the stress markers. In general, smoking affects the levels of the stress marker molecules – levels are lower in the participants who do not smoke, and closer to their normal diurnal course.
Daily pressure on HPA reflects on pulse and blood pressure
The human organism reacts to the daily challenges releasing various hormones and mediators, including catecholamines. They affect cardiac activity, blood pressure and other physiological processes, being the mechanisms involved in daily adaptation to various stressful situations – from acute stress to comparatively weak routine activities, such as waking up. Thus, an organism copes with the challenges of everyday life44.
Stress changes cortisol secretion, which activates an organism’s adaptation and protective mechanisms. The cortisol molecule passes freely through the blood–brain barrier and has a direct effect on areas of the limbic system in the brain, exerting control on blood pressure45. Apart from in the brain, cortisol receptors are in the kidneys and smooth muscle cells of blood vessels, which also exerts a direct effect on blood pressure. Gold et al report a disturbed regulation of HPA in patients with slight hypertension – independent of their age, sex and body mass index46. All of these factors could explain the changes in the observed diastolic blood pressure that might be caused by changes in the function of HPA.
Cortisol influences blood pressure in a different way during individual development and between the sexes. Younger women have lower blood pressure and are more predisposed to diseases resulting from low blood pressure in comparison to older ones. This is probably due to the decreased ability of their vessel sympathetic neurons to cause vasoconstriction.
The blood pressure in women is constantly changing, and in middle age is of the same value as in men. During the eighth decade it exceeds the values measured in men. This could be due to the lower levels of estrogen after menopause, as a result of which the sympathetic activity increases, as well as the adrenergic vasoconstriction response47. That dependence was not confirmed by the present study, where all values were statistically lower in women.
Conclusion
The professional life of GPs is associated with constant exposure to stressful situations. The data collected during the present study give reason to state that GP work in rural areas of the Republic of Bulgaria is accompanied by the development of stress. The levels of stress are constantly changing as the working week progresses. This study’s results demonstrate lack of or insignificant stress at the beginning of the week. Stress development is more pronounced at the end of the week – the stress marker molecules do not or barely follow their normal diurnal course. Daily routines and habits such as alcohol consumption, smoking and physical activity could be considered as modulators of the organismal response to stressors.
Nevertheless, the results do not provide a solid evidence for the levels of stress. Some results are confusing, which means that the characteristics of the rural regions might also have an impact on stress development. These characteristics, in combination with professional life and habits, may modulate the activity of both the HPA and ANS, but describing this requires more experimental work.
The present study is the first of its kind in the Republic of Bulgaria. It was conducted immediately before announcement of the COVID-19 pandemic. The authors of the article intend to continue their study of stress in the present situation, as well as during the constantly changing health and economic environment.
Acknowledgements
This study is supported by the Bulgarian Ministry of Education and Science under the National Program for Research ‘Support for young scientists and postdoctoral researchers’.

