Introduction
The supply of new general practitioners (GPs) sufficient to meet a population’s health needs, particularly in rural and remote areas, continues to be a major global workforce distribution challenge. In Australia, this remains a concern despite substantial investment in rural workforce support1. While approximately 40% of Australia’s current registered specialists are GPs2, this proportion is falling and relies on recruitment of international medical graduates to address local undersupply. Recent exit surveys of Australia’s graduating medical students have found only 15% list ‘GP’ as their first-preference career3, indicating a potential for the GP workforce to decrease further.
Specialty training pathways in Australia commence after at least one mandatory internship year of clinical ‘prevocational’ service. This is almost wholly completed in hospital environments in metropolitan or large regional settings, with rotations through narrower specialties such as internal medicine, surgery, obstetrics, anaesthetics and emergency medicine. Many graduates also complete some additional years of hospital-based experience before formally joining a specialty training program. Final career choices are often deferred until after gaining broader clinical workplace experience, weighing up which professional and non-professional aspects best fit with their interests4,5. While there is now a formal curriculum for the ‘gap’ between undergraduate (medical school) learning and specialty training6, opportunities for postgraduate experience in general practice or other community-settings remain limited. This is a critical time for making long-term decisions about preferred specialty and work settings5,7,8. On the other hand, programs that provide meaningful experience in general practice may either reinforce prior interest or even initiate interest and uptake among junior doctors, potentially redistributing specialty interests in line with community need5.
The availability of general practice rotations as part of internship training has been reported since the late 1990s, both in Australia and the UK9,10. Evidence suggests these programs successfully met their objectives and complement traditional hospital-based programs10,11. Participants generally were supportive of these programs, with increased interest in general practice and rural practice expected outcomes12. This builds on broader evidence of positive exposures to general practice encouraging doctors to choose that specialty13. From 2005 to 2014, Australia’s Department of Health supported the Prevocational General Practice Placement Programme (PGPPP), which was available to junior doctors 1–3 years after exiting medical school and built on the success of the smaller Rural and Remote Area Placement Program14. However, a 2013 national review of rural health workforce programs found the PGPPP had a ‘success’ rate of only 25% participants enrolling in general practice specialty GP training15, which partly justified its closure shortly thereafter.
Opportunities to gain early postgraduate experience in smaller rural settings, where medical workforce maldistribution is most significant, are also commonly limited. Exceptions include programs like Victoria’s Murray to Mountains rural community internships16, where participants are embedded within primary care and small community hospitals, and ‘rotate in’ to the larger regional hospitals for their core rotations. Similarly, the Queensland Rural Generalist Pathway coordinates rural experiences from medical school to completion of specialty training in rural medicine17,18. Other longitudinal clinical placement models in smaller rural communities are available at most Australian rural clinical schools19,20 with results suggesting improved location distribution of graduates21, but their full impact may be eroded by more recent large hospital training.
Weak evidence of other specific benefits from training prevocational doctors in community and GP settings includes experience of a wider variety of presentations of different acuity, opportunities to improve communication skills and learn different doctor–patient relationships, exposure to the interface between primary and secondary/tertiary care, experience of chronic disease management and preventative interventions, and opportunities to understand the role of social and psychological factors in illness9,11,22-24. Importantly, there is exposure to child health and mental health, specialties with both limited availability and very different scope of practice in teaching hospitals25,26. Further, a placement of several weeks in general practice allows junior doctors to participate in the provision of continuing, comprehensive care, based on seeing patients repeatedly and for a broad range of conditions27,28. In contrast, limitations include that general practices must provide the workspace, workload and clinical supervision, and manage potential disruptions to workload management and fee-for-service funding streams. Costs for travel and accommodation are higher where practices are at some distance from the hospitals, with hospitals needing to manage the impact from staff absences to meet training and supervision requirements. Concerns about perceptions of lesser quality experience have been somewhat discredited23,27, although this may linger due to the absence of a voice within hospitals to champion general practice29.
In late 2015, funding was committed to replace the PGPPP with the Rural Junior Doctors Training Innovation Fund (RJDTIF) program30. This new program enables interns (and some in their second postgraduate year) already undertaking their training year in a large regional setting, to replace one training rotation (approximately 10 weeks) with a rural general practice setting. Many such placements require a relocation to the rural community, thus to both live and work in the community for those 10 weeks. The RJDTIF program is hypothesised to increase the proportion of doctors (who are already training in a regional setting for their intern year) to consider primary care as their preferred specialty and to strengthen their consideration of rural and remote communities as their preferred location to work, irrespective of preferred specialty. It complements the Rural Generalist Pathway programs17, whose participants (unlike those of the RJDTIF program) have already made a commitment to both specialising in general practice and to be skilled to practise in smaller rural communities.
For any new policy or program, it is important to conduct an evaluation of its effectiveness, otherwise the appropriateness of this use of public funding remains unknown. This study aims to evaluate the educational and potential workforce impacts of the RJDTIF training term on participating interns. It builds upon new evidence from Tasmania that found their RJDTIF placements were good learning environments and reinforced desires to be rural GPs31.
Methods
This study was conducted in the large state of Queensland, Australia. It was designed as a prospective evaluation of the new RJDTIF training term, across the calendar years 2019 and 2020. The evaluation team had no other connection to program participants or the health services and clinicians involved in its delivery.
The intervention
All Australian doctors newly graduating from medical school undertake a 1-year internship, which mostly consists of five or six rotations in different departments of the employing large hospital. From 2018, the Australian Government began funding for the RJDTIF program, which enables regional-based interns to have access to training rotations in rural primary care settings. This rotation is approximately 8–12 weeks in length, with funding for Queensland enabling 50–60 such rotations (up to 12 sites, one intern per site over five rotation periods) in each of 2019 and 2020. For the most part, interns are allocated to such rotations based on the submitted preferences of all available rotations. Intended outcomes of the RJDTIF program include (1) improved retention of medical graduates and junior doctors in rural medical practice, (2) increased rural medical training capacity and (3) a contribution to the development of a rural pathway continuum for medical education and training in expanded settings. Interns training in metropolitan hospitals are excluded from the RJDTIF program. This study was funded only for the evaluation of intern placements, thus second-year postgraduate doctors completing RJDTIF training terms were excluded from this evaluation.
All participants of Queensland’s RJDTIF program were undertaking their intern training at one of seven large regional hospitals in Cairns, Townsville, Mackay, Rockhampton, Bundaberg, Hervey Bay and Toowoomba. Of the 12 utilised general practice sites, four were within a 15-minute drive of the main hospital location, four were within 45 minutes road travel and the remaining four were up to 3 hours from the main hospital location. In 2021, approximately 272 of Queensland’s 784 intern positions were in these seven hospitals. Thus, at full capacity approximately 22% (60/272) of regional-based interns participated in general practice rotations under the RJDTIF program.
Participants and data collection
This study was designed around all program participants (maximum n=110) being invited to complete both a pre-rotation and post-rotation survey. However, due to COVID-19 no survey invitations were distributed for two full rotations in 2020 (n=24). All invitations were distributed by email, with a direct link to the information sheet and the electronic survey (completed using SurveyMonkey and Qualtrics), and a single reminder was sent for each survey. The surveys captured key background information, self-evaluation of career intent (focus on rural and general practice outcomes), their motivations and enthusiasm for the rotation, reflections on the value of the rotation, positive and negative features of the experience and impact of the rotation relating to the program’s objectives.
Semi-structured interviews (post-rotation) were intended for up to 20 participants. However, COVID-19 had a major impact on continuing this evaluation, including that the original lead academic researcher overseeing data collection left the project to support COVID-19 related public health activities and clinical supervisors at each rotation being heavily burdened with COVID-19 activity. For these reasons, only four interviews were completed in the project’s timeframe, although this still provides important piloting of this part of the evaluation. These interviews included questions that reflected on participants’ reasons for choosing the placement, how it contributed to their clinical abilities, its influence on career choices, what they gained professionally and socially, and what might improve the program.
Data analyses
Quantitative data analyses used Stata SE v15.1 for Windows (Stata Corp, http://www.stata.com). Descriptive statistics of counts and proportions were used to present the basic patterns among respondents of their pre-rotation interest and career intent, and their post-rotation evaluation and career intent. Surveys were intentionally identifiable, enabling matching of the pre- and post-rotation data where applicable. The survey also collected open-ended (free-text) responses, which were analysed using thematic analysis. Relevant free-text responses were integrated with the quantitative findings.
Data from four semi-structured interviews were separately analysed using thematic analysis in NVivo v12 (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software). These small numbers prevented justification to apply a theoretical framework. All audio-recordings were transcribed verbatim, and an inductive, reflexive thematic analysis approach was adopted32. This approach included an initial stage of familiarisation with the interview transcripts, listening to audio-recordings, and generating initial codes. Further, analytic themes were developed using initial codes. All themes were reviewed by the authors to ensure the appropriateness of each theme and narratives were selected to illustrate the themes and highlight key points.
Ethics approval
This study was approved by the University of Queensland Human Research Ethics Committee (application 2018/HE002343).
Results
In total there were 50 completed pre-rotation surveys and 35 post-rotation surveys, with n=60 completing either survey and n=25 able to be matched for both surveys. After adjusting for non-invites, response rates were approximately 60% (pre-rotation) and 42% (post-rotation). Most respondents participated in 2019 (65%), with an even spread across each rotation term (Table 1).
Table 1: Demographics: all survey participants (n=60)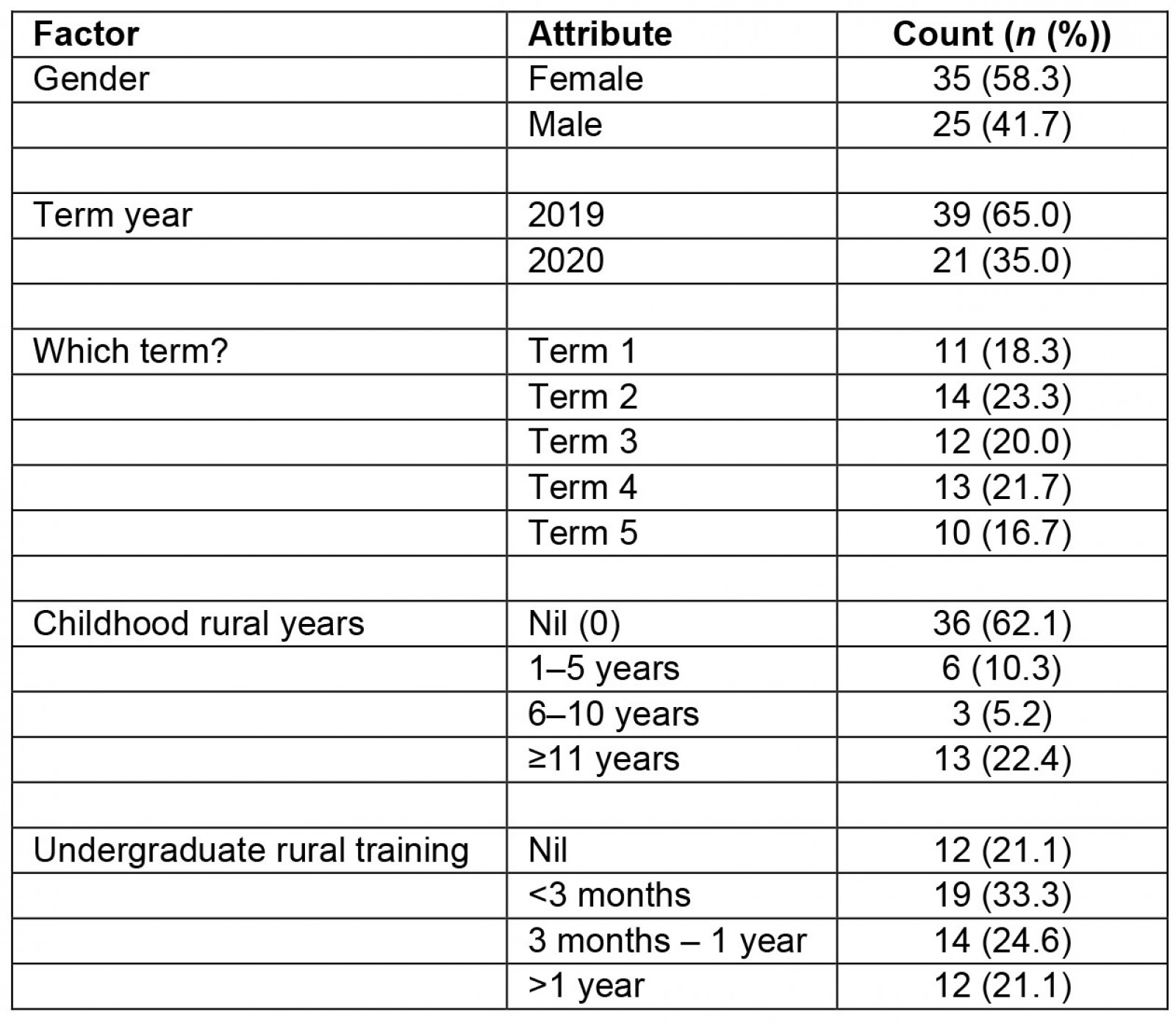
Pre-placement preferences and enthusiasm
Approximately half (48%) of respondents indicated they preferenced the rural GP term, 22% indicated partial preference while 30% indicated it was not their preference. Similarly, on a 10-point scale for enthusiasm for the rural GP term, 48% rated 8–10, 33% rated 6–7 and 19% rated 1–5. General practice was indicated as the most likely career option for 50%, other general specialty 28% and subspecialty 22%. Likelihood to be working in a regional/rural location in 10 years was indicated as ‘likely’ or ‘very likely’ for 40%, ‘unlikely’ for 24% and ‘unsure’ for 36%.
There were two standout reasons for preferencing a rural GP term: (1) experience training in a primary care setting (50%) and (2) gain more clinical skills through increased patient exposure (22%). The other five options (experience rural or remote medicine, learn from primary care clinical supervisors, work in small multidisciplinary team, enjoy the social/recreational opportunities of working rurally, and spend an extended period in a smaller rural community) were all selected by fewer than 10% of respondents.
Many participants noted the unique experience that the rural GP term would offer beyond what was normally available in their intern training. Interns reported they were most looking forward to the following aspects:
Gaining more clinical skills in a primary care setting, and trying to increase my exposure to conditions not seen in hospital.
This is a career that I am strongly considering so doing a term as a doctor rather than a student will give me a greater idea as to whether I would enjoy it or not.
Learning how to manage patients in the primary care setting. Time management in GP setting which is often limited despite patients having a list of many issues they want to address.
Experiencing continuity of care. Having just finished Acute medical and emergency terms, I am keen to experience the other end of the spectrum and follow many of these patients up.
Post-placement evaluation and impact on career interests
Overall assessments of the rural GP term were strong, with 86% indicating they would recommend it to their peers. Most rated the term as ‘excellent’ (59%) or ‘good’ (28%), while most found the experience of living and working in the community rewarding (‘excellent’ 34%, ‘good’ 48%). Specific assessment of different values of the rural GP term were mostly strong (Table 2). A majority agreed with all stated values, with 57% agreeing that it had stimulated their interest in rural general practice as a career path and a high majority agreeing to have increased understanding of the context of rural health care and specifically rural general practice, the private sector and working in small multidisciplinary teams.
Overall impact on pursuing primary care was self-assessed as ‘much more likely’ 41%, ‘little more’ 26%, ‘no impact’ 19% and ‘much less’ 15%. In comparison, overall impact of working in a rural area was self-assessed as ‘much more likely’ 11%, ‘little more’ 44%, ‘no impact’ 37% and ‘much less’ 7%. Matched data indicates that all participants rating the term poor or average had a low (5 or less) pre-placement enthusiasm for the term. Those much more likely to pursue primary care were mostly (63%) those with some pre-placement career preference for general practice while none were those with a pre-placement preference in a subspecialty. Those more likely to work in a rural area were similarly split between those with a pre-placement preference to work either regional/rural (56%) or metropolitan (44%).
Most concerns of the GP rotation related to (1) difficulties sorting out practice logistics, orientation and poor supervisor availability; (2) limitations of not having a provider number for billing; or (3) isolation from family, friends and peers. However, these were generally balanced against other gains from the placement. In particular, many participants noted the increased opportunity to develop clinical skills from the GP setting:
Building rapport with patients; Clinical reasoning and differential diagnosis; Management of common presentations i.e. colds, sinusitis, diabetes, musculoskeletal injuries, etc.
Diagnostic skills without being able to rely on extensive investigations.
Patient relationship, ability to connect with individuals. Paint the bigger picture and manage them holistically by addressing all aspects of their life.
Patient history, exam and management. Procedural skills. Communication and working with patients in hospital and GPs in small towns.
Many participants appreciated the benefit of such rotations in smaller rural communities:
I would definitely recommend learning what it means to live somewhere rural and understand the limitations of specialties offered in the region, but also how this can be navigated. I would encourage my peers so that they can learn general medicine knowledge that can be applied to every single specialty they choose to do.
If you are interested in a career in Rural Medicine this is an excellent rotation – good mix of hospital and GP. If you are interested in a career in General Practice this rotation provides a lot of insight into the challenges of General Practice/how to bill patients/ways to implement preventative medicine.
Some found it valuable to gain a more complete understanding of what general practice was like:
Getting a better understanding of the complexities of General Practice. Developing relationships with patients so that they take ownership of their health. Learning how to prioritise both the patient’s agenda but also the GPs in terms of preventative medicine – and learning how to do this in a time efficient manner.
Experience hands on, increased autonomy and responsibilities. Being challenged, getting involved in coordinating referral and stabilisation of urgent/emergency presentations.
For many, this rotation was able to consolidate their specialty intent, although some concerns were expressed regarding difficulties of general practice in smaller communities.
It was an amazing 10 weeks. I would not have a changed a thing and I am definitely more keen to pursue GP Training in the future.
It has consolidated many of the things I enjoy about primary health care and working in rural settings.
Primary care is a good fit for me. From the work life balance to the type of work, it all resonated with me perfectly. I am grateful I have had this opportunity now because now I know that this is right for me.
I have fallen in love with GP [general practice] and would love to pursue it as a specialty ... however I would have to weigh the pros and cons for rural/regional GP as a career for mental health and wellbeing in the long term.
Separate thematic analysis of the semi-structured interviews resulted in two themes that highlighted the impact of RJDTIF training on participating interns. Both themes – importance of the rural GP term for interns and potential improvements to rural intern GP rotations – align closely with findings from the survey responses.
Table 2: Overall assessment of the value of the rural general practitioner term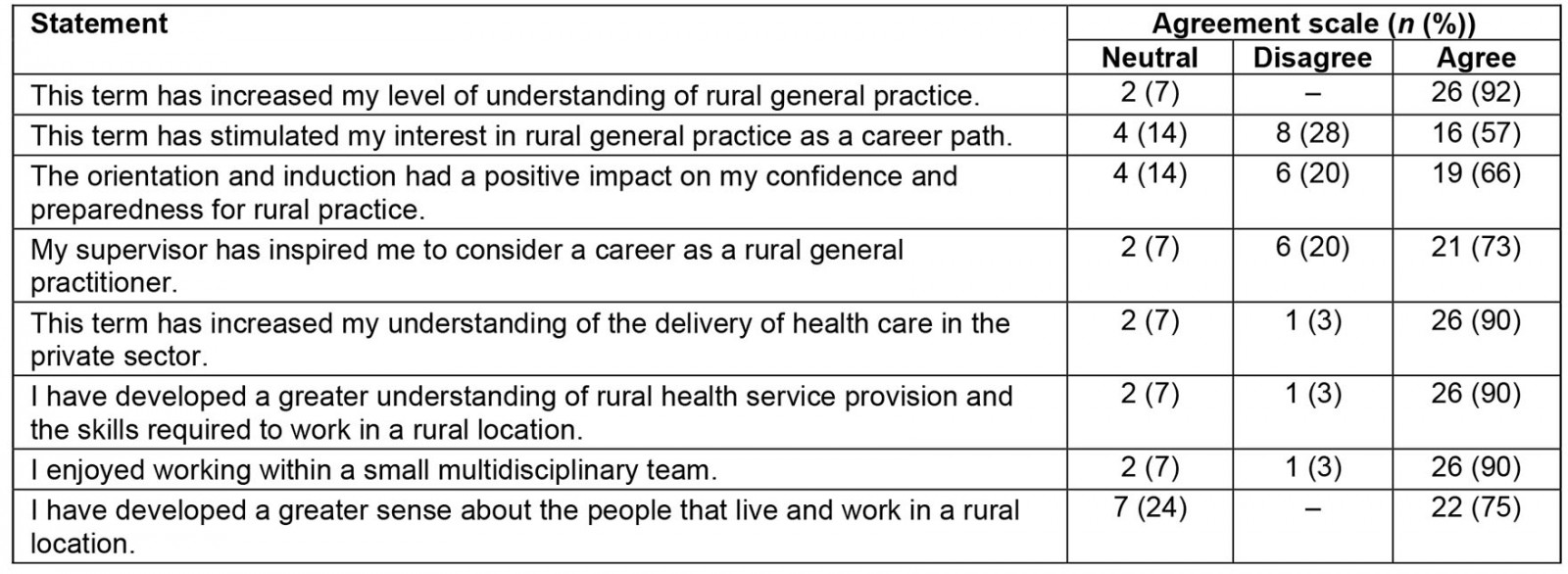
Theme 1: Importance of the rural general practitioner term for interns
Four subthemes within this broader theme were identified: hands-on learning, skill improvement, influence on future career choices, and engagement with the local community.
Hands-on learning: When discussions around the interns’ experiences of the rural and remote training started, several participants indicated that they were learning more about GP training from the hands-on learning environment in the rural/remote area than when they were in the medical school. For instance, ‘K’ mentioned that:
I think hands-on learning is one of the very few things that in medical school you don’t get to do … I wanted to actually feel like what it would be like [to be] a GP rather than watch the GP or observe the whole situation … Here [remote/rural practice] I get to practice my skills in history taking and examination in a live setting.
Skill improvement: The interns also explained that, by engaging in the RJDTIF program, they can see an improvement in their skills such as time organisation and history-taking skills. For instance, ‘J’ mentioned that:
I really learned a lot in terms of communication and yeah, empathy … I mean I learnt how to be able to communicate things to the patients that they don’t necessarily expect … This is something I did not learn much about in the medical school.
Influence on future career choices: Participants also mentioned that, through attending the RJDTIF program, they gained clarity and were surer about their future career choices. For instance, ‘A’ shared that:
By attending this training, I am much more encouraged to become a GP and stay in a regional area.
Engagement with the local community: Participants shared that, while interning rurally, they were able to engage with the local community and learn about different cultural expectations, views and beliefs of their patients. Participants indicated that engaging with culturally diverse patients will benefit them in the long term. For instance, ‘S’ shared that:
I learned a lot about the community itself. Earlier, I never thought that this would be a part of my job [engaging with people from different cultural backgrounds].
Theme 2: Potential improvements to rural intern general practitioner rotations
The participants also discussed potential improvements for future intern GP rotations that may benefit future junior doctors. Participants suggested that by making the RJDTIF program more readily available and random allocation of students into the program will provide opportunity for more students to engage and experience rural GP. The potential to promote general practice as a great place to learn medicine was also noted:
I probably would improve this rotation or improve the outcome of this rotation by making it more available, so it is more hospital time that is available.
I think people would be way more inclined to do GP, and would also just – even if it wasn’t something they particularly went out of their way to preference or they wanted, if by chance they were allocated it, I think that they would learn so much and just actually enjoy doing GP [general practice] in a rural setting.
I think even if you’re not interested in general practice, there’s so much to learn, because you have that exposure to patients … I think it’s just an awesome opportunity for interns to actually practice some medicine.
Discussion
Most participants of the RJDTIF program reported a positive experience from their rural GP rotation, with 86% recommending it to their peers. This evidence supports the Australian Government’s investment in junior doctors having opportunities to spend part of their intern year outside of large hospitals and urban settings as a way to stimulate interest in general practice as well as for increased rural community-based training experiences. It is complementary to existing evidence of the benefits of such placements, which have largely focused on the breadth of exposures to clinical conditions rather than any career choice impacts11,24. Given that a high proportion of intern doctors are yet to consolidate either their choice of specialty or likely practice location8, programs like the RJDTIF would appear to be vital to helping address key medical workforce distribution shortages in both general practice and rural practice.
By far the leading reason for preferencing the rural GP term was to ‘experience training in a primary care setting’. A common gap of the current prevocational structure of medical training is that it normally does not include general practice, despite this being the leading specialty required to meet population need. Siloing prevocational doctors within large hospitals may influence career decisions away from both rural settings and primary care33,34. It is well recognised that choosing a specialty is a complex and dynamic process, with interests and preferences often increasing following new clinical experiences. However, where experiences in community-based clinical fields such as general practice are omitted, such as in ‘traditional’ internships, there is little scope to either initiate or reinforce interest in rural primary care careers. Globally there remains a trend of specialisation away from primary care, thus the case remains strong for programs like the RJDTIF to provide positive primary care experiences in rural settings.
Primary objectives of the RJDTIF program include increased retention of junior doctors in rural areas and increased capacity/pathways for training in expanded rural settings. The latter part of this intent is successfully achieved through all participants being drawn from regional settings and enabled to partake in general practice training in similar or smaller rural communities. The first part of this intent is much harder to judge, with only a small proportion (11%) indicating they were much more likely to work in a rural area after their placement, compared with 44% who were a little more likely. The positive impact of location intent applied similarly to those with a pre-placement preference of either metro or rural. This suggests that such rotations may impact participants either as a confirmation or conversion, depending on pre-existing intent or interest35.
Many participants self-identified skills development values of training in general practice, particularly from training in smaller rural communities. They especially noted increased exposure to building longer term patient management and relationships, learning how to undertake clinical reasoning within the constraints of general practice consultation times and billing, improved patient history taking and diagnostic skills without ready access to diagnostic tests or support of other specialists’ feedback, as well as insights to the challenges of working in general practice. These findings are consistent with other research specifically drawn from the general practice setting9,22,23. Importantly, these were experiences not otherwise gained in their hospital-based training. In addition, many participants articulated that their GP immersion during intern training was a different experience to that when they were a medical student, thus suggesting the unique value of GP training experiences within their internship.
It is notable that around half of participants had not highly preferenced undertaking the rural GP term. It is unclear whether this related to a lack of interest in primary care as a career, a lack of interest in smaller rural community practice, lower expectations of the value of such a rotation in their overall career development, or perhaps less willingness to spend time away from their core hospital training setting (and its network of peers, clinical supervisors and educators, as well as family and friend networks). Clearly a challenge of the RJDTIF program is to grow interest among new interns. At its current size, the RJDTIF program is able to provide rural GP training opportunities to fewer numbers than are needed to meet future workforce needs in rural primary care, thus sustainable growth is desired.
Many of this study’s findings resonate with those reported from Tasmania under the same RJDTIF program31. The Tasmanian study found that the RJDTIF program was also successfully delivered, diversifying the intern training experience and helping consolidate rural career pathways. The present study’s findings additionally quantify the strong ratings and value placed by most participants in evaluating their experiences. Intern rotations in general practice have been reported to successfully meet their objectives over the last 20 years, but they remain an infrequent training option. While it was anecdotally seen to have increased general practice interest, Australia’s predecessor program, PGPPP, was ultimately ‘closed’ due to government evaluations finding it underperformed in terms of translating to sufficient enrolments in GP training. These new state-based evaluations of the new RJDTIF program provide promising early results, but translation to a sufficient uptake of one or both general practice and rural medicine remains to be seen.
Limitations
As with evaluations of most training interventions, program allocation is not random and thus it can be more difficult to differentiate between the effect of the RJDTIF program ‘intervention’ and pre-existing interest. In the present study pre-rotation surveys were conducted to enable some adjustment for this ‘baseline’ effect within the cohort. The study was substantially affected by COVID-19, disabling two (out of 10) rotations, and the departure of the original lead clinical from academia mid-project, having only completed four interviews. The authors recommend that future evaluations of rural intern GP rotations replicate interviews with participants, but also extend to practice managers, GP supervisors and their hospital-based internship managers. While this survey’s response rates were relatively good compared to similar research (42–60%), there were fewer matched participants completing both pre- and post-rotation surveys (n=25) than originally planned. It will be important for future evaluations to measure long-term (sustained) impact, rather than this study’s short-term impact.
Conclusion
The findings of this study showed that Queensland’s participants successfully completed GP rotation terms as rural interns under the RJDTIF program. Self-assessed ratings of the value of these terms were generally strong, with encouraging workforce distribution intent reported post-rotation. The need remains strong for the provision of prevocational opportunities to experience rural primary care practice before having to select a preferred specialty training pathway, as this may reinforce interest in primary care careers, particularly within rural communities. These findings support investment in programs that provide opportunities for junior doctors to experience rural general practice in these formative postgraduate years to stimulate interest in a career pathway for which doctors are much needed. More conclusive evaluations on recruiting success from the RJDTIF program will only be possible after at least 5 years, when several cohorts of participants will have completed rural primary care training.
Acknowledgements
This project was partly funded by Queensland Health, which is responsible for internship training in Queensland. The project team in particular acknowledge the support from Queensland Rural Medical Service, which oversaw the funded RJDTIF program training terms.



