Introduction
The number of older adults (ie adults aged ≥ 65) worldwide is expected to double over the coming two decades1. As a result, we can expect to see a growing number of older patients living with increasingly more complex and often interrelated health (eg comorbid conditions) and social issues (eg loneliness) that can threaten their independence and wellbeing2,3. All older adults, but especially those experiencing complexity, can benefit from a geriatric care professional’s medical expertise and their knowledge of resources to better support healthy aging4,5.
Many older adults live in rural and remote communities that are experiencing population aging at a faster rate than more urban communities. This is largely owing to the increasing out-migration of younger individuals to urban communities, often for economic and social reason6. Furthermore, these communities often experience higher rates of chronic diseases compared to their non-remote counterparts, which adversely affects later-life function, independence, and overall life expectancy7-10. There is no standard definition of rural and remote communities11. For this review, we define these communities as localities with populations under 25 000 persons11. Existing literature reviews have highlighted the benefits seen by older adults living in rural communities when an emphasis is placed on better meeting their individualized care needs12. These needs are often met best by those who specialize in the care of older adults; however, this workforce is shrinking5. Currently, Canada has approximately 376 certified geriatricians (representing ~0.004% of its overall physician workforce) and 1800 certified geriatric nurses (representing ~0.0055% of its registered nurses)13-15. Only a small proportion of these specialists work in its more rural and remote areas14. Similar findings have been noted worldwide16, including in the USA5 and Israel17. Some geriatric virtual care models have been found to assist with capacity limitations in rural communities, allowing specialists to see a greater volume (number) of patients, resulting in improved patient care18,19. This is just one example of an attempt to adapt to the challenges of providing geriatric care in rural and remote settings, but little is known about other models of care, particularly those in remote communities without the technological infrastructure to support virtual care20.
The best models of care for older patients in rural and remote settings have not been defined. Existing reviews do not highlight the unique components of geriatric models of care that can be implemented widely across rural and remote settings. Therefore, identification of the components that make up current geriatric models of care must occur. To inform the development of a geriatrics outreach model of care for remote or rural populations, we conducted a systematic review of the existing geriatric models of care literature to identify key operational components that should serve as the basis for the development of future evidence-based outreach models in these communities.
Methods
Design
The purpose of this systematic review was to identify key operational components that could inform future geriatric models of care serving rural or remote populations. A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria21,22. This study was also guided by qualitative case study methodology as it allows researchers to conduct an in-depth exploration of models of care within the specific context of rural settings23. For the purposes of this article, we broadly defined a model of care as the implicit structural processes that make up healthcare service provision24. As with other health service reviews, we did not rely on a single definition of ‘rural’ and/or ‘remote’, and thus accepted the range of definitions used in the literature, to avoid limiting our literature search to particular regions25. Ethics clearance for this study was not sought, as this research did not involve human participants. A protocol has been registered (osf.io/fnr2u). No amendments were made to the protocol.
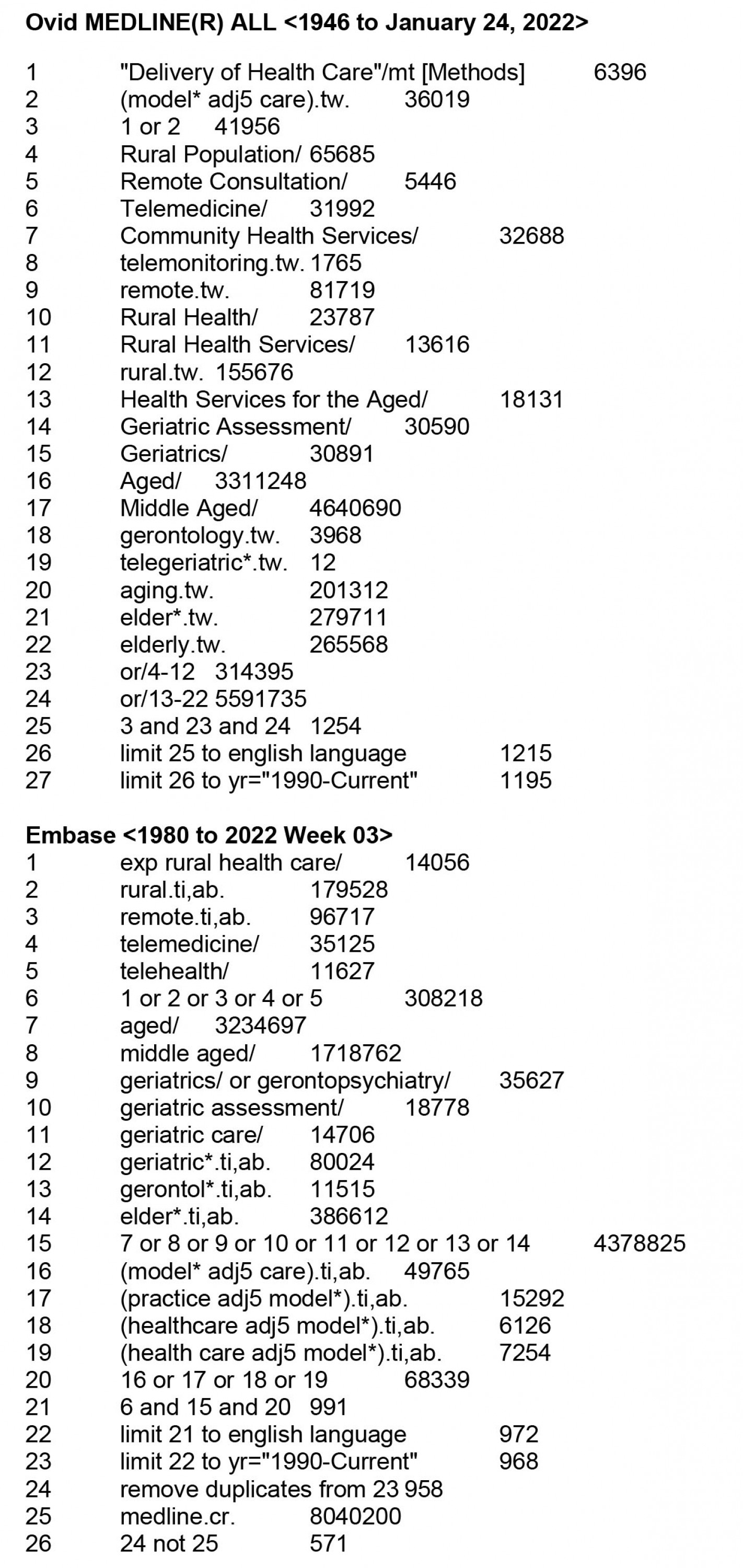
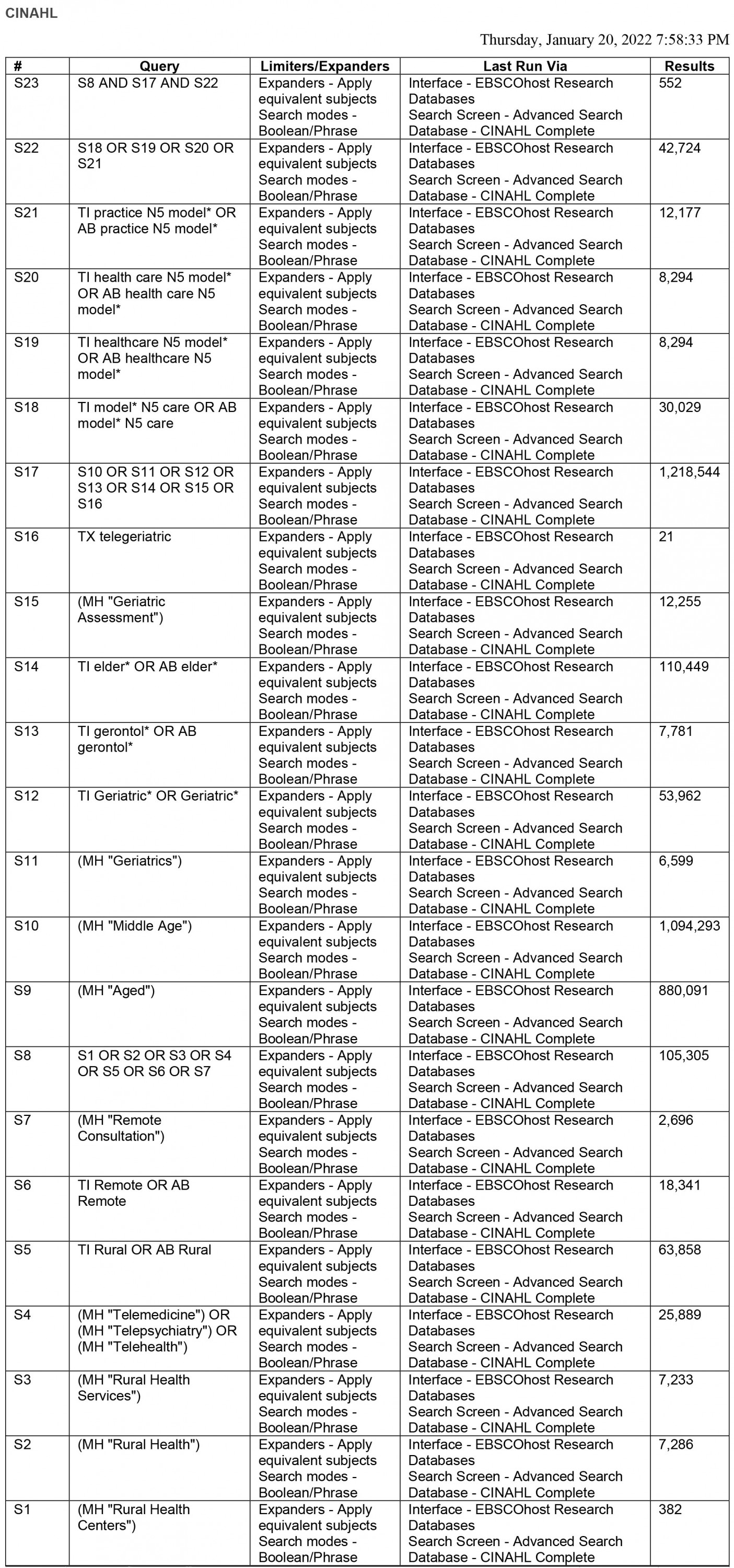
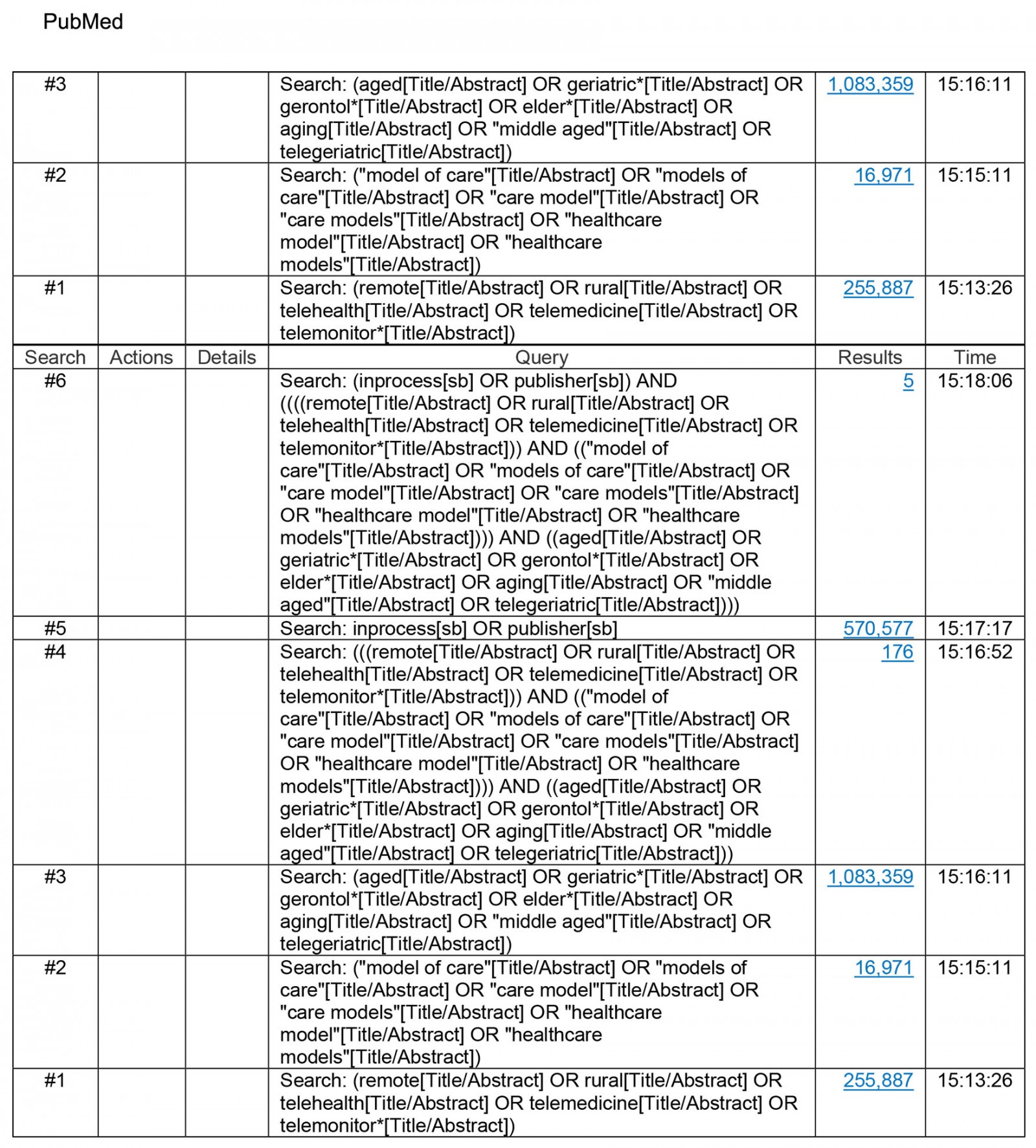
Data sources and search strategy
This study identified English-language, peer-reviewed research articles that describe a geriatric model of care for remote or rural populations. Searches for articles were identified through MEDLINE, CINAHL and EMBASE from 1994 until 2022. We limited our searches to 1994, as we identified this period to be when seminal work in geriatric models of care began to emerge26,27. Medical Subject Headings (MeSH) and subject terms or keywords related to geriatrics were used in combination with ‘model(s) of care’, ‘delivery of care’, health service’, ‘delivery of healthcare’, as well as ‘rural’ and ‘remote’. To ensure a comprehensive search and ensure we did not unintentionally miss any articles, MeSH terms for ‘implementation’ and ‘components’ were not used in the search. Lastly, the reference lists of all articles that met the inclusion criteria outlined below were reviewed to identify any missed relevant articles. The full list of search terms can be found in Supplementary material 1. All search strategies were developed by the authors in collaboration with a medical information specialist. Two medical information specialists ran the searches and removed duplicates using the Bramer method in EndNote software28.
The search strategy for grey literature (reports and information not published commercially) was done in consultation between the research team and a medical information specialist. Searches for grey literature included the websites of rural city-specific ministries of health, by searching the Dissertations and Theses database as well as searching for relevant abstracts from conference proceedings via the Conference Papers Index. We last updated searches of the peer-reviewed and grey literature on 24 January 2022.
Study selection
Articles were included if they described an implemented model of care (for any duration) for adults aged 65 years and older in rural or remote settings. To encompass the spectrum of models of care, articles reporting on models of care could, but were not limited to, preventative care, disease management, rehabilitation and palliation models, as long as medical care was described (ie care provided by a physician). Models of care could range from community- and home-based models to primary, secondary, and tertiary facility-based models. Articles were excluded if they were published before 1994, in languages other than English, or solely described a conceptual model of care (ie a hypothetical model such as those in commentaries, opinion pieces or study protocols). Articles were also excluded if they did not have enough information on the model to extract components (eg conference abstracts that lacked a full publication) or if they included a target population not exclusively adults aged 65 years or more. Finally, we excluded articles that did not include a medical assessment (eg occupational therapist-led models of care).
Citations were downloaded from the databases into EndNote, a citation management tool, and duplicates were removed28. Two reviewers (KK and KMK) screened abstracts to identify potentially relevant articles (level 1 screening). If the reviewers could not determine whether to include or exclude an article based upon title and abstract alone, it was included for full-text reading. Discrepancies were resolved by consensus with a third reviewer (SS). Next, the authors reviewed a subset of the same articles (75%), until an agreement was reached. An agreement was evaluated by kappa scores (the kappa score for inter-rater agreement was 0.92). Next, the same two reviewers reviewed the rest of the full- text articles (KK and KMK) and consulted a third reviewer (SS) if unsure of inclusion or exclusion.
Data extraction
Data were extracted independently from all included articles by two authors (KK and KMK) using an Excel spreadsheet that contained the following data variables: their authors, country, year of publication, patient inclusion and exclusion criteria, model of care design (including key findings according to the conceptual framework domains), and any objective results and subjective observations (eg patient intermediate clinical outcomes). A third author (SS) reviewed the extraction of a random sample (n=4 articles, 50%) of the final selected articles for quality control purposes.
Risk of bias screening
Two reviewers (KK and KMK) independently assessed the risk of bias using the Downs and Black Checklist, a validated and reliable generic risk of bias tool29. Qualitative studies were appraised using the validated Quality Assessment for Qualitative Research Reports (QAQRR) tool. The scale assesses 24 items related to the risk of bias in qualitative studies30. The level of agreement between the two reviewers was estimated with Cohen's kappa and was determined to have good agreement31. Discussion with one other reviewer (SS) helped to evaluate individual domains within the respective tool used, assign an overall risk-of-bias judgement, and determine inclusion. Articles with a low risk of bias were included in our final synthesis.
Analysis
To describe and compare diverse models of care, a systematic qualitative case study analytical approach, modeled by Baxter and Jack23 and Huberman and Miles32, was further used to identify the core operational components constituting each model of care to establish an objective method of comparing the various models. A qualitative case study analysis approach considers individual cases (eg articles, models of care) to capture the complexity of the description of that case33. This involves considering how each case is unique as well as how various cases are similar through an analysis of the various components of the models being examined33. First, two authors reviewed each article (KK and KMK), identifying the core organizational (eg leadership), structural (eg processes of care delivery), and clinical process (eg details on provider–patient encounters) components of their described design and clinical interventions. This approach starts with listing every possible model component identified within each design, then determining whether individual articles were using the same terms to describe different components or different terms to describe the same components. This process ultimately enabled a set of categories (eg ‘high-risk screening’ or ‘local provider leadership’) to be conceptualized by the research team32.
After a comprehensive list of identified components had been determined, each model was reviewed again by the first author (KK) and identified as either adhering to or not adhering to each component, through a process known as component adherence. This adherence analysis was done by incorporating methodological rules for evaluating criteria adherence described by Sinha et al34 and others35-37. Adherence was largely determined by whether written evidence of such adherence existed. For example, a study that alluded to the selection of higher risk older patients as being important but did not specify a screening procedure used within their model would have been listed as non-adherent to using a ‘high-risk screening’ selection process. Any uncertainty was arbitrated through a discussion among all the investigators.
As component adherence served as the basis of our qualitative analysis, we attempted contact with all eight principal investigators (PIs) to assess their level of agreement with our interpretations of their study’s component analysis. They were also invited to list other distinct model components they believed to be included in their model that we may not have considered or overlooked. Of the eight PIs we contacted, 3 (n=3/8, 37.5%) responded. All three PIs agreed with our interpretations.
Results
Our database search yielded a total of 2323 citations, from which 1794 were selected for further examination by title and abstract review. A total of 43 full-text articles were subsequently reviewed. Overall, eight articles describing unique geriatric models of care serving rural or remote populations were included in the final analysis38-45. Figure 1 displays the process involved in study selection.
The eight included articles involved patients aged greater or equal to 65 years from three countries: the USA (n=5, 62.5%), Australia (n=2, 25%), and Canada (n=1, 12.5%). Our analysis identified three staffing models and eight operational components across the included models of care. Findings are presented below using a modified version of the template for intervention description and replication (TIDieR) checklist as a guide (eg description of providers, modes of delivery, components essential to the interventions)46. Two models looked at populations over 75 years of age42,43. All models served rural geriatric populations ranging from 995 to 12 250 people over a geographical distance ranging from 80 km to 2800 km. The number of patients served ranged from 51 patients over 13 months to 660 patients over an undifferentiated number of years. Of those who reported gender, the majority had largely female cohorts between 63.8% and 78%, except one model among older veterans that consisted of 99.8% male patients42. All models provided initial patient characteristics such as age, sex, and reason for referral. Five of the eight articles (n=5/8, 62.5%) described some form of initial patient description or intervention data, which included the number of or types of recommendations, referrals made for patients, or services recommended38,40-43.
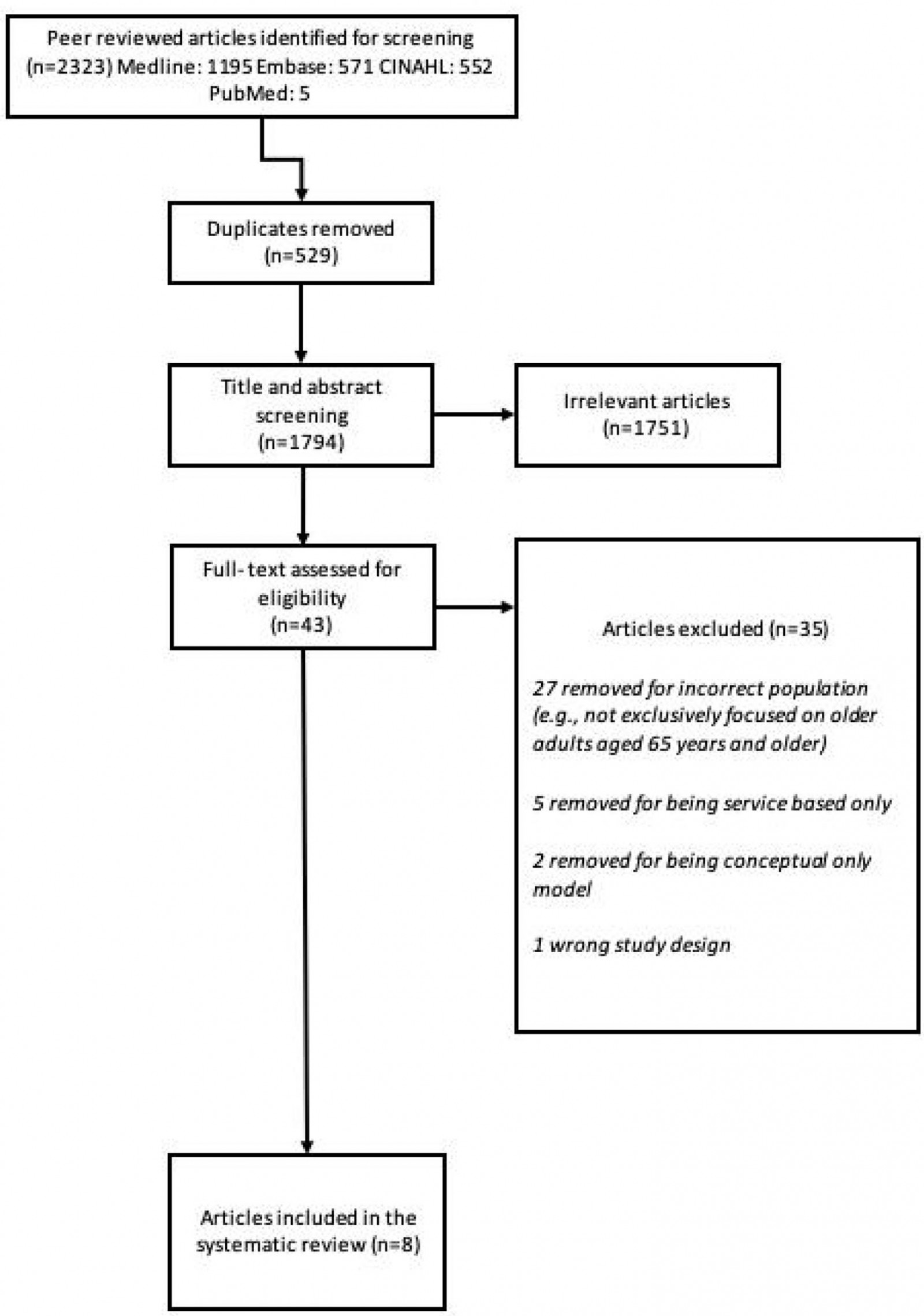 Figure 1: PRISMA diagram for study selection.
Figure 1: PRISMA diagram for study selection.
Interprofessional staffing models
Within the eight articles, three main staffing models were identified, and are described below. Three articles38,39,45 (n=3/8, 37.5%) had geriatricians directly involved in conducting the assessment of the older patients being served (model 1: geriatrician-led assessment ± nursing and allied health support). The form of this assessment varied between articles. Two models38,45 described all patients being assessed by a geriatrician regardless of their level of complexity. One of these models involved telemedicine to connect older adults with dementia to geriatric behavioral supports45. The third model39 described a process whereby a specialist geriatrics nurse practitioner (SGNP), who worked under the direction of a geriatrician, saw all patients and determined whether there was a need for a full assessment by the geriatrician. The second model design (model 2: nurse-led assessment with peripheral geriatrician consultation ± allied health support) was identified in three articles (n=3/8, 37.5%)40,42,43 and described having either an SGNP or general practice nurse (GPN) having exclusive contact with patients, but having access to a remotely located geriatrician to review all or some of the patients via teleconferencing or in-person meetings. While two of these models used a SGNP to conduct comprehensive geriatrics assessments (CGAs)40,43, one model used a GPN to conduct the primary CGAs42. Finally, the third model design (model 3: geriatrician-independent nurse-led assessment ± allied health support) identified in two of the articles (n=2/8, 25%) used GPNs to independently manage older patients41,44 with no additional geriatrician support.
Key operational components of geriatric models of care
Our qualitative case study analysis identified eight distinct operational components across geriatric models of care that help facilitate their goals of providing care to older adults. These components encompassed:
- local provider leadership
- local provider education in geriatrics
- community engagement
- model integration into the existing local healthcare system
- high-risk screening principles and methods
- home and environmental assessments
- longitudinal care and support
- direct geriatrician consultation.
A synthesis of study characteristics and model characteristics, including adherence of each described intervention to the eight identified characteristic components, is presented in Table 1. These model components are narratively described below.
Table 1: Overview of study characters and key operational component characteristics of identified rural and remote geriatric models of care38-45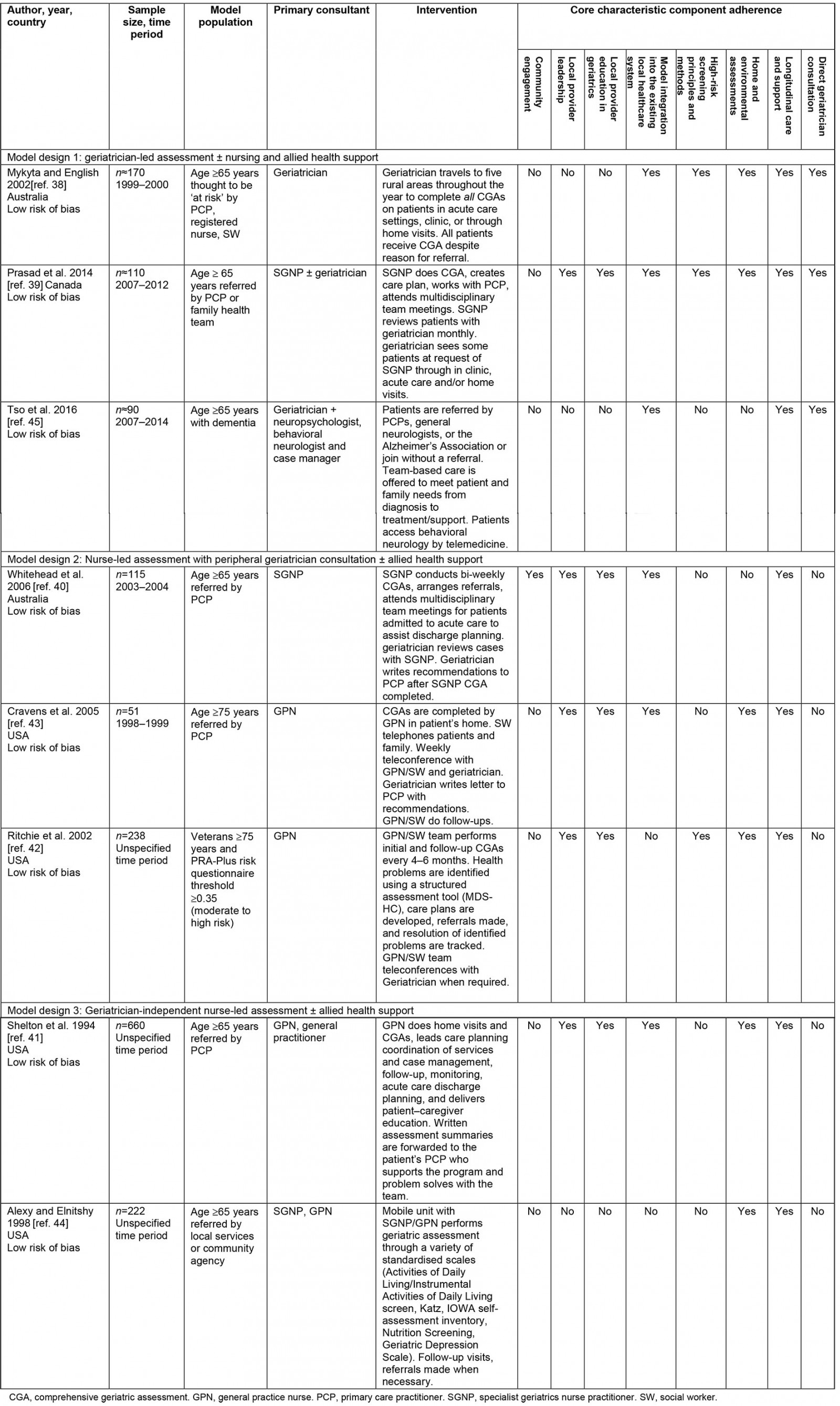
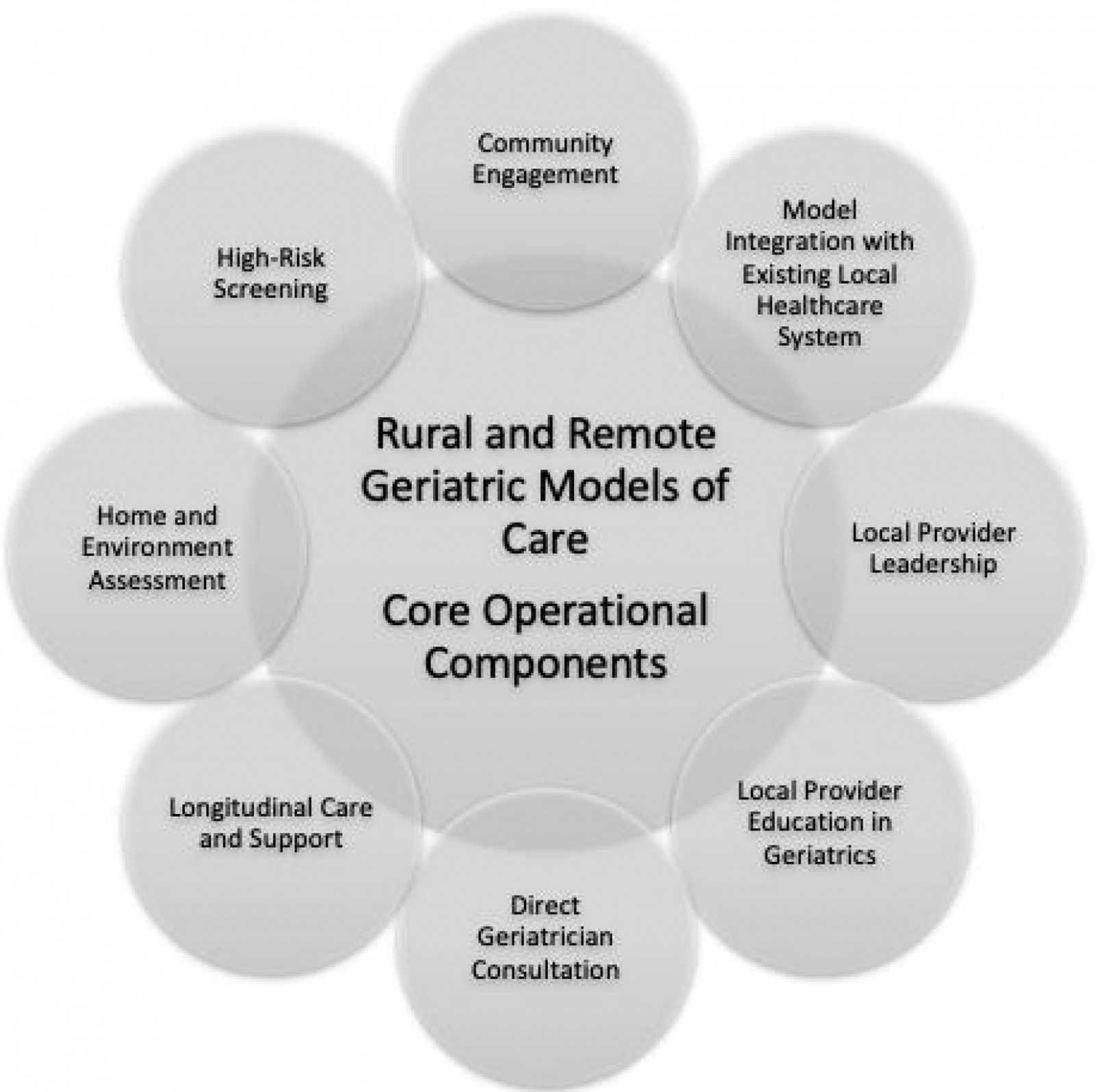 Figure 2: Proposed framework for a geriatric model of care serving rural and remote populations.
Figure 2: Proposed framework for a geriatric model of care serving rural and remote populations.
1. Local provider leadership: In line with community engagement and understanding of local needs, five studies (n=5/8, 62.5%) emphasized the importance of having local provider leadership39-43. It was identified that new models of care that are championed by a trusted local provider that can liaise between the community itself, local community providers, and the geriatric outreach model personnel can help to maintain fluid and productive connections. Local provider leadership also appeared to be vital towards creating local ownership of the model itself39. While local leaders can come from any professional background, leaders were frequently a local SGNP or GPN as they were familiar with community dynamics and their patients41,42. The SGNP or GPN could act both independently and in tandem with physicians, effectively streamlining communication between services41,42.
2. Local provider education in geriatrics: Gaps in knowledge around caring for older patients can result in misdiagnosis and missed opportunities to improve the care of the target population. Local provider education was perceived as being able to greatly improve knowledge, skills, attitudes, and overall confidence in caring for complex older patients in five of the models39-43. It was noted that local providers who had a solid base of geriatric knowledge better identified the specialized needs of their older patients and initiated appropriate care practices faster40. In addition, the provision of continued educational support to local healthcare teams was seen as facilitating ongoing long-term, high-quality care42.
3. Community engagement: Only one model incorporated active community engagement into its design40. Community engagement was defined as specific outreach activities including meetings with local healthcare providers, community leaders, and invested parties to discuss a proposed model of care before its initiation. The creators of one model of care employed local healthcare providers to help develop a model that best supported their local practices40. The engagement activities focused on providing familiarity with the proposed model’s goals, adapting feedback on the model from local parties, and obtaining ‘buy-in’ from local healthcare providers and the community at large40. One article (n=1/8, 12.5%) noted that distrust in a new model of care is common, but once the community is engaged or if a previous therapeutic relationship exists, a new model can exist more easily39.
4. Model integration into the existing local healthcare system: New models will not succeed if they operate independently of the existing healthcare delivery framework39-43. Thus, an understanding of how a model can be implemented, but not place additional strain on established healthcare services, needs to be considered. Prasad et al highlighted their use of an ‘ecosystem approach’ in the development of their model, which valued a local SGNP as the ‘glue’ between the consulting team, local primary care, and other healthcare providers, allowing for integration into the local healthcare environment. We identified six articles (n=6/8, 75%) that aimed to integrate their model of care into the existing local healthcare system39-43,45.
5. High-risk screening principles and methods: Regarding appropriate care delivery, three models utilized high-risk screening principles and methods to target their interventions to those with the greatest need38,39,42. Given the clinical heterogeneity of older patients, high-risk screening can allow the most ill patients to be identified and triaged for assessment and intervention first. This is especially important in rural and remote communities given the limited staffing and resources available42. Universal screening mechanisms can further ensure that the most ill patients are not overlooked38.
6. Home and environmental assessments: Five articles (n=5/8, 62.5%) described the importance of home and environmental assessments39-43. Knowing about a patient’s environment is key to being able to assess how well an older patient is functioning in the community39. Understanding home and environmental experiences are crucial when deciding if an individual is appropriately equipped to live independently or if the individual requires additional support that can allow the person to function more independently42.
7. Longitudinal care and support: All models described longitudinal care and support. As the issues of complex older patients often evolve, having access to ongoing care and support can aid in the development of a more meaningful patient–provider relationship and allow more successful interventions to be implemented45.
8. Direct geriatrician consultation: Three articles (37.5%) included direct geriatrician consultation38,39,45. This model component specifically refers to patient consultations that are done directly by a trained geriatrician with expertise working in multidisciplinary teams. Geriatricians have the capacity to address the intersection of social, functional, and medical issues with patients, particularly those with dementia45. Direct geriatrician consultation could be facilitated through telemedicine. The use of telemedicine may be particularly helpful in rural settings where geriatricians may not often be practicing45. It is worth noting that three other articles (n=3/8, 37.5%) did offer indirect geriatrician support40,42,43.
Discussion
Our systematic review of the literature revealed eight articles describing geriatric models of care serving a multitude of rural and remote populations. The identified models came from three countries: the USA41-45, Australia38,40 and Canada39. This was not seen as a shortcoming, but rather a reasonable jurisdictional representation for this review, as these countries represent large geographical areas in the English-speaking world with numerous rural and remote populations, having limited access to care, particularly geriatric care.
Three articles (n=3/8, 37.5%) (all from the USA) specifically characterized their populations as lower income, from ethnic minorities, or living with multiple chronic health issues41-44. To date, many rural and remote communities described in the geriatric literature have older adults with more limited financial means4,47, living with higher than average rates of chronic disease, frequently with limited access to consistent healthcare providers48-50. Gaps in patient care for those with multiple chronic medical and social issues make them particularly vulnerable to system overuse51. Gaps in patient care may result in more serious care challenges for the ‘oldest-old’ (ie older adults aged 85 years and older), who are most likely to need healthcare, financial, and physical support due to complex age-related needs52-54. As time-intensive geriatric care interventions have been often shown to be most valuable in frail older adults with the capacity to benefit from additional support55, future models of geriatric care must allow for the appropriate time to provide these services. Similarly, long-term follow-up of older patients by a multidisciplinary team has been shown to improve health perception and aid in the sustained improved social and psychological wellbeing56-59.
In line with community engagement and understanding local needs, many of our articles (n=5/8, 62.5%) emphasized the importance of having local provider leadership (component 1), providing training for local providers in geriatric care principles and practices (component 2), as well as integrating the new model of geriatric care into the existing local healthcare system (component 4) as important components to best serve their rural and remote populations38-44,60,61. Outreach care models can be sustained by appointing local provider leadership (component 1), which can ensure the contributions of more itinerant providers of care can be understood and supported. For example, having local provider ‘champions’ (eg nurses62) with an established relationship with other resident health providers and patients can ensure novel models of care are not only understood but facilitated and integrated at the local level63-67. While local leaders can come from any professional background, we identified that a local SGNP or GPN frequently took on this role as they were familiar with local community dynamics and could act both independently and in tandem with peripheral physicians, effectively streamlining communication between services41. Too often the creation of different models creates additional ‘silos’ of care that remain minimally integrated, hence becoming additional barriers to the delivery of quality care39. To help support champions, our review highlighted the need to train local providers in geriatric care principles and practices (component 2). Cochrane reviews have highlighted the importance of providing local education to improve health outcomes and provide more efficient use of services55,68.
Future research
In addition to model design, more research is needed to determine the best person to provide specialist geriatric care and support in rural communities. While two models did not involve geriatricians or those with expertise in geriatrics41,44, the remainder provided either direct geriatrician consultations (component 8)38,39,45, or indirect geriatrician support40,42,43. While there is insufficient data from this review to determine which type of provider is most effective, there is a growing body of evidence to support that the active involvement of a geriatrician is more likely to result in better health outcomes (eg improved overall functional status) and reduced hospital admissions and institutionalization57,69-71. Conversely, there is insufficient evidence to suggest that nurse-led programs are less effective. This is important to consider when limited resources may only permit the creation of an intervention using the peripheral support of a geriatrician or a purely nurse-led design.
Finally, as active community engagement was only described in one article included in this review40, future research is needed to explore how to foster active community engagement so that it leads to the development of more locally effective models of geriatric care. The Program of All-Inclusive Care of the Elderly (PACE) model in the USA60 was established at the PACE Summit, where the groundwork for understanding what services were needed and how best to deliver them took place60. This summit included representatives from local community organizations, healthcare providers, and policymakers who were invited to discuss adaptations required of the original PACE service delivery model to enhance its effectiveness for rural populations being served61. Our review found that employing local healthcare providers can help develop a model that supports their local practices and actively engages healthcare communities in rural settings40. Prasad et al also note that distrust in a new system is common, but once the community is engaged, or if a previous therapeutic relationship exists, a new model can exist with less effort39. Thus, policymakers and researchers looking to adopt new models of care are encouraged to engage local communities and healthcare providers in their implementation strategies. Furthermore, the identification of best-practice strategies for fostering community engagement in the context of older adults and rural communities is encouraged.
Limitations
Our study must be considered in the context of its limitations. As with any literature review, publication bias and the potential for incomplete identification of relevant articles are considerations. Only English-language peer-reviewed articles were considered and thus we may have excluded relevant articles published in other languages or those not in journals. Our search strategy was potentially limited by the selection of key terms utilized in our review. For example, we did not utilize terms such as ‘interprofessional’ and ‘community’, which may have resulted in us excluding some clinical models of geriatric care. Further, ‘third sector’ services (eg those provided by charitable organizations) and residential care services run by social care providers that meet the needs of rural older adults would likely have been excluded, although these were not necessarily the intended focus of this review. In our review, we performed a qualitative analysis and drew inferences about the applicability of these models to all rural and remote communities assuming some form of homogeneity. This is arguably an oversimplification of what may be a very diverse population. We tried not to make inappropriate value assumptions based on the frequency with which a core component was found within articles. Previous studies have used similar methodologies to inform the development of clinical models and health services interventions34,65.
Conclusion
This review proposes that any future geriatric care delivery model designed to serve rural or remote populations utilize an evidence-based framework based on the eight distinct model characteristics we identified through this review that aim to support the ideal provision of effective and accessible geriatric medical care. This review can inform future research to better serve these populations. We also hope the development of this evidence-based care framework will lead to broader information dissemination and refinement efforts, especially because an increasing recognition is finally occurring around the need to better support these rapidly aging rural and remote communities.