Introduction
The chronic lack of a qualified health workforce in rural and remote settings continues to pose a significant challenge in achieving universal health coverage globally1. The rural–urban health workforce imbalance persists partly because of ineffective rural placement and retention policies2,3. Human resources for health (HRH) policies need to be context specific and be informed by views from rural health workers, who know the local context best4,5. Therefore, exploring healthcare workers’ and policy-makers’ views is vital in formulating workable HRH retention policies3,6.
The health sector strategic plans of Malawi and Tanzania highlight the critical shortfall in the workforce required to meet the increasing demands of healthcare delivery. Both countries report a recent increase in the capacity and output of trained health personnel from the training institutions; however, the rural workforce availability remains low, and suffers frequent rural–urban attrition. Health authorities in both countries call for novel strategies to improve deployment and retention, especially in rural and remote locations7,8.
HRH studies have used several models (frameworks) to configure factors at play for health workforce retention. These include Herzberg’s motivation–hygiene theory9, partial least square structural equation modelling10, the root stem model11 and the social–ecological model (SEM)12. Each model contributes to the understanding of aspects of workforce retention. Public health research and programs are increasingly applying SEM to understand human behaviour in relation to public health and HRH interventions13,14.
SEM was applied to appraise the perspectives on retention and intention to leave among mid-level health workers (clinical officer (CO), nurse-midwife (NMW) and assistant medical officer (AMO)) and policy-makers from remote and rural areas of Malawi and Tanzania.
SEM hinges on the premise that health workers decide to stay or leave a location or job on account of individual factors or factors in the environment (ecology)12. The model encompasses five levels of influence: (1) individual or intrapersonal; (2) family – interpersonal or microsystem; (3) surrounding community – institutional or mesosystem; (4) society – exosystem; and (5) national/international regulations and policies or macrosystem12.
In appraising these perspectives, the authors considered the four key strategies proposed by the World Health Organization (WHO) for improving access to the health workforce in rural areas – education, regulation, incentive, and professional/personal support15 at each SEM level – and used SEM as a framework for analysing the qualitative data16.
Methods
Study design
A qualitative, longitudinal study spanning 3 years from 2014 to 2017 was conducted among health workers in Malawi and Tanzania who took part in an in-service training program entitled Enhancing Training and Appropriate Technologies for Mothers and Babies in Africa (ETATMBA). Senior health professionals from the University of Warwick in the UK and the Karolinska Institute in Sweden, and trainers from the University of Malawi and Ifakara Health Institute in Tanzania, implemented ETATMBA between 2011 and 2014. As a result, participants received training in emergency obstetric care, newborn care, leadership skills, and supportive supervision. A different study provides the details of the ETATMBA program17, and another study presents the follow-up process18.
Topic guides
Topic guides were developed for participants and key informant interviews with input from HRH experts at the Liverpool School of Tropical Medicine. First, the researcher drafted the interview topic guides, which included both open-ended and closed questions covering perceptions on retention and intention to leave among the study participants, using insights from SEM and the four WHO retention strategies highlighted above. Next, the topic guides were presented at the academic staff forum at the Liverpool School of Tropical Medicine for critique. Then, the revised topic guides were presented again in the academic staff forum and were approved. Finally, the researcher pilot tested the topic guides in each country and revised them before data collection.
Data collection
Participants were contacted through contact details held by the ETATMBA program. Consent was sought from each participant and key informant. Before the interviews, study information sheets were issued, which explained the study objectives, rationale, risks, benefits, the information that would be sought, and how the information would be collected.
Participants were informed and reminded at each follow-up interview that participation in the study was voluntary. Therefore, they were free to opt out at any time without any repercussions.
A total of 120 interviews – 111 participant and 9 key informant interviews – were conducted. In Malawi, 42 health workers were interviewed – all of them COs – and 4 key informants. In Tanzania, 69 health workers were interviewed – 38 NMWs, 31 AMOs – and 5 key informants. The titles of the key informant officials are shown in Table 1.
The authors conducted the initial set of interviews face to face. It is best practice to conduct the first set of interviews face to face to develop a good rapport with participants19. Then, participants were contacted once every 3 months to find out if there had been any changes regarding their job or circumstances such as transfers, promotion, salary and social life (marriage, children, parents, friends, bereavement), and whether such changes had influenced their perspectives on health workforce retention and their intention to leave or stay. Phone calls or social media such as WhatsApp® and Messenger® were used for the follow-up interviews. The repeat interviews took the same format as the initial interviews but were shorter and more focused. Participants were asked whether their perceptions of retention or intention to leave had changed based on the changes in their circumstances.
For the key informant interviews, the researcher visited the ministries of health premises in both countries, explained the research to relevant authorities and was given a list of officials to meet whom were met in person for the interviews. This was done only once at the beginning of the study.
Interviews were recorded on an Olympus WS 832® voice recorder. The researcher transcribed the interviews immediately and sought clarification by calling back the participants on the same day or a day after the interview. If the participant did not have enough time, the researcher brought the issues to the subsequent interview.
Table 1: Numbers of participants taking part in the interviews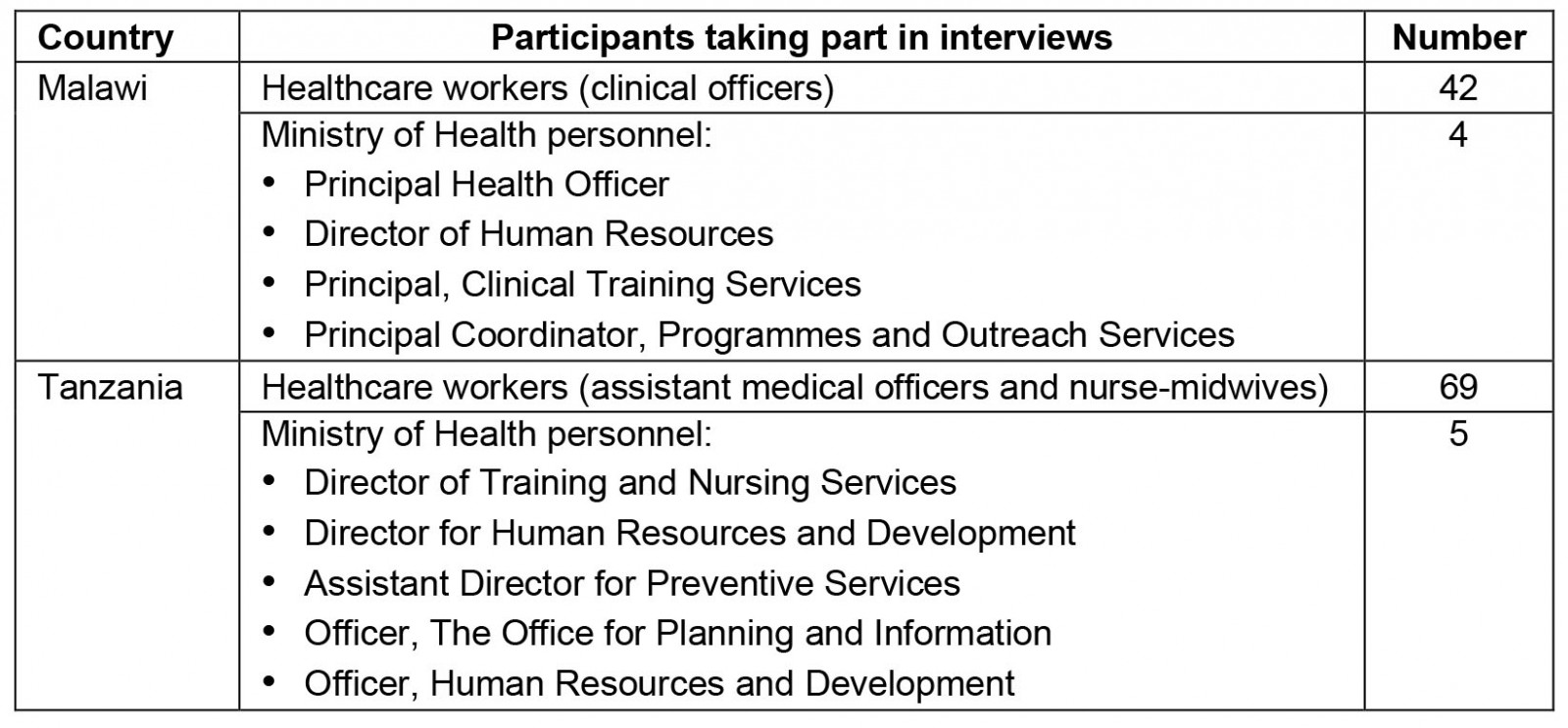
Data analysis
Framework analysis was used to analyse the data. The transcribed data were read and re-read to explore meanings and linkages across the main themes and to categorise the data according to the five SEM levels. Data analysis started after the first set of interviews. After each subsequent interview, the analysis was repeated and compared with the previous analysis. Similar themes were merged, and linkages from the emerging themes to those identified before were sought.
Ethics approval
This study was part of the ETATMBA program, with ethics approval from the University of Warwick, UK (REGO-2013-572), the University of Malawi (P.07/11/1102), and the Ifakara Health Institute, Tanzania (IHI/IRB/No:35).
Results
The study participants provided insights into health workforce retention and the perceived factors affecting retention and intention to leave. They shared personal experiences of transfers, promotion, changing jobs, changing roles, managing healthcare facilities, and carrying out administrative roles. These perspectives on retention and intention to leave are presented by using the five levels of SEM.
Individual (intrapersonal) factors
Common factors mentioned in this category included recognition, competency, confidence, promotion, and income.
A need for recognition: Recognition by colleagues, the health facility leadership, or community members was perceived to encourage retention. Quite often, participants linked recognition to a sense of belonging and personal achievement.
The people in the community recognise us. During outreach clinics, we diagnose conditions like hernias, lipomas, tropical ulcers and provide the necessary care. In addition, community health workers will call us directly if there is an emergency or send patients to our hospital with specific instructions to consult us. (CO, Malawi)
Feeling competent and confident at work: Health workers perceived competency to influence retention in that, with the skills acquired during training, they could provide a wider variety of services than before the training, which gave them a sense of more worth at the workplace.
I am a midwife, but I was trained to provide anaesthesia through this program [ETATMBA]. So you can see that the hospital needs my skills during every theatre procedure. (NMW, Tanzania)
Being competent and confident in the workplace was also linked to a sense of autonomy. For example, a health worker would decide to stay in a rural facility where they would have the autonomy to make decisions rather than transfer to an urban facility where that autonomy would be lost.
Promotion and salary increment: Promotion and salary increase was perceived to encourage retention. Apart from the extrinsic motivation that either of these brings, promotion and higher salary were associated with recognition.
The main issue is promotion. It does not matter if I get a salary increase or not. Even if I were transferred to another facility for a senior position, that would be okay for me. So, on promotion grounds – yes, I would comply with a transfer. (AMO, Tanzania)
A sense of belonging: Health workers perceived transfers across health facilities or departments within the health facility as annoying. However, they perceived that staying at a facility or a department longer was associated with a stronger sense of belonging, which was perceived to encourage retention.
It is better now that I am stationed at the maternity, not being rotated around like before the [ETATMBA] training into different departments. I like working with people I am used to. (CO, Malawi)
Other health workers had a different view on this. They perceived that a transfer to another facility or department would not affect retention. To some health workers, a sense of belonging resonated with the notion that COs and AMOs are cadres specifically trained to work in rural and remote areas. Therefore, they would not perceive a transfer to another rural facility as a deterrent to retention.
I trained to work in rural areas. Leave the central hospital for specialists. I think I would not be as helpful if I were transferred there. (AMO, Tanzania)
Source of income: Participants thought that the income from their job or sources such as private medical practice, farming activities, or spouses’ income influenced retention. Most participants thought that income was the most substantial factor influencing retention.
Salary is an automatic motivator. You pay people better first and sort out other things later. So how much money I get will determine how long I stay. Other benefits, eg medical insurance schemes, lease loans for buying a house or car, would encourage me to stay in the job. (CO, Malawi)
Career progression opportunities: Participants felt that the availability of career progression opportunities was a decisive factor for retention. In addition, participants highlighted their awareness that working in a remote place was a Ministry of Health eligibility criterion for allocating career progression opportunities. A Ministry of Health official in Tanzania echoed these perspectives.
I want to stay in government employment because there is an opportunity to upgrade. I am hoping that even after ETATMBA, there will come other opportunities to upgrade. (AMO, Tanzania)
We try to balance selection for scholarships for further studies. In addition, we give applicants from remote settings a higher priority for career progression. (Key informant interviewee (KII), Ministry of Health, Tanzania)
Notwithstanding, the perceived outcome of securing opportunities for further studies differed between health workers and the Ministry of Health officials. Ministry of Health officials thought opportunities for further studies would encourage health workers to stay in hard-to-reach areas, whereas health workers regarded such opportunities as a gateway out of hard-to-reach areas.
The reason for such favours is for those given the opportunity to return to remote places after their studies. However, this is not always the case. (KII, Ministry of Health, Tanzania)
… some abuse the system, their stay in remote areas is a means to get scholarships and would not return to the rural hospitals after training. That is not the aim of such a [retention] scheme. (KII, Ministry of Health, Malawi)
Some participants who held leadership responsibilities thought about what would happen to their posts if they went for further studies. As a result, they would only decide to pursue further studies if they retained their posts or were assured authorities would promote them to senior roles upon return.
When you go for further studies, someone else will act in your position, and you may not get to the same position after you return. (AMO, Tanzania)
This point illustrates the range of opinions among health workers interviewed. Some were seeking opportunities for further studies; others would only accept such opportunities if it would help them retain preferred roles or lead to a promotion.
The perspectives on retention and intention to leave based on individual health workers presented in this section show that perspectives vary between health workers according to personal preference and circumstances at hand. In addition, close family members (microsystem) and the surrounding community (mesosystem) – discussed below – appeared to influence these individual factors such as income source, faith, a need for recognition, and career progression plans.
Factors related to immediate family members (interpersonal/microsystem)
The welfare of close family members such as children, spouses, and extended family were considered essential when changing jobs or relocating. As a result, health workers were more likely to make decisions that would favour close family members rather than their individual needs.
Health workers believed they had the primary responsibility of meeting the financial needs of their family, attending family social events, taking care of sick relatives, etc. Their spouse’s job and children’s education were the most commonly mentioned factors, as illustrated by the quotes below.
If I were told to relocate, the only factor to consider would be my wife. She has made many customers in her business here, so [if we relocated] she will be one to lose. (CO, Malawi)
I do not mind being transferred to another facility within the town. However, the most significant consideration now is my kids. I would not want their education interrupted. As for myself, I would not worry too much. (NMW, Tanzania)
However, some health workers had a contrasting view on this. They felt that working with many family members around would affect their performance.
One challenge of working at a home district is that relatives and friends expect some favours. So naturally, this would affect my job performance. (CO, Malawi)
The major microsystem factor was the welfare of close family members. This factor directly links to individual factors and relates to how the health worker is related to the surrounding community.
Factors related to surrounding community (institutional/mesosystem)
Personal and professional networks: The presence of personal and professional networks with supportive friends and colleagues at the workplace was perceived to encourage retention. This factor links back to the sense of belonging presented in the individual factors. In addition, health workers thought the support received from colleagues would overshadow negative factors such as remoteness of location or a low salary.
We work as a team, and we enjoy team spirit; fellow staff members respect us, giving me a solid reason to stay. (NMW, Tanzania)
Despite the remoteness, four of us [ETATMBA trainees] support each other in work and ordinary daily life. That makes me forget about leaving this place. (CO, Malawi)
Professional support from managers at a health facility or district health authority was equally perceived to encourage retention. The fear of unfair treatment of staff by the leadership in the destination facility was considered a deterrent to relocating.
The district health management team listens to our ideas and is responsive to our suggestions and requests; this is not the case in other districts. (CO, Malawi)
Following the training and becoming part of the facility leadership meant that participants got involved in decision-making roles at the facility, which was perceived to encourage retention.
I used to complain a lot about many things. However, after taking up a leadership role, I realised that we are constantly working with a shortfall in resources. For example, last year, our hospital budget was 30 million [kwacha] [equivalent to A$45,000], but we only received 7 million [kwacha] [equivalent to A$11,000]; we need to understand the economic level of our country. So I am willing to stay in this facility and contribute ideas on improving our services with the resources available. (CO, Malawi)
Availability of resources: The lack of necessary equipment and consumables for patient care reduced staff motivation. Some health workers thought that the lack of resources would lead to misunderstandings between them and the facility leadership, adverse patient outcomes, and a negative impact on staff morale.
For example, caesarean section, which is a daily procedure, the theatre is not in good order, the [operating] table is not adjustable, and you have to do four to five caesarean sections in 24 hours using this kind of table. There is not enough medication for patients; it is frustrating. (CO, Malawi)
Participants also highlighted that the lack of health workers would result in excessive work and burnout and related this to poor retention.
Only one person gives anaesthesia in this facility. If she is not around, we struggle. Having adequate staffing would make work easy and encourage us to stay. (AMO, Tanzania)
Health workers thought that, as excessive workload led to low retention, a very low patient load would equally be demotivating, suggesting that a balanced workload would encourage retention.
Since I was transferred to this facility, I am not happy … I am a bit let down because I am not busy enough. I just perform a few cases of BTLs [bilateral tubal ligations]; I was busier at (district name). (CO, Malawi)
I would never go to a central hospital, … there I will be used like a hoe, at the district [hospital] I have time for rest. At [name of a hospital] or [name of a hospital], the specialists leave all the hard work for you to do. (CO, Malawi)
Some participants cited the lack of resources as a challenge but recognised that moving to another facility would probably not make any difference.
I believe that every place has its problems … at times, we tend to ask if this district has got this ... and that district has got that … all district hospitals have the same fundamental problem – lack of resources, which makes it difficult for one to discharge their duties effectively. (CO, Malawi)
Additional responsibilities: When the community members asked health workers to take on responsibilities other than their hospital jobs, they saw it as an expression of trust, respect, and honour. It made them feel recognised and that they belonged. As a result, some health workers considered the community responsibilities more critical than job-related factors in deciding whether to relocate or not.
I have been elected as chairperson of the local secondary school governing committee. I feel my contribution is still needed in this role. The school is doing very well academically, and I feel proud. Teachers and students would be very disappointed if I left now, so I would rather stay. (AMO, Tanzania)
Giving back to community: Health workers who had received support from the community during their studies thought they needed to remain at the health facility to pay back the loyalty.
Since the time I was a medical attendant, it was the health centre advisory committee that recommended me for further studies. So, I trained as a clinical officer and now the ETATMBA training. I have a strong desire to give back to the community. For this reason, I will remain in this facility even though it is a remote place. (CO, Malawi)
This section has presented the perspectives of health workers on factors related to the surrounding community that would affect retention. Broader societal factors (discussed below) influence these community factors.
Factors associated with society (exosystem)
The remoteness of a facility was perceived to reduce retention. Health workers thought that the further away a facility is from the urban area, the less likelihood of retention. The opinions from health workers sometimes indicated that the lack of amenities in rural areas was the problem and not the mere distance from the nearest major town.
When I came here first time more than 20 years ago, transport was a huge challenge. I was very concerned if we had an emergency that needed an immediate referral. We always experienced delays. Now we have a tarmac road, and you can get to town and back within a few hours; I do not see a problem working in this facility. (AMO, Tanzania)
Some participants mentioned climate as affecting retention. However, preferences for the desired kind of climate differed among respondents. For example, some preferred a warm climate, but others preferred a cold climate.
I will consider climate to relocate; I have been at Mzimba for some time. It is calm and pleasant here, and I would appreciate a change, but not to the lake [Lake Malawi]; for me, it is uncomfortably warmer there. (CO, Malawi)
Participants did not mention security, political or legal issues in either country when discussing societal factors. The reason could be because there are no precarious political or security issues in the two countries or that there is no notable difference in the political and security issues in the urban and rural areas in the two countries.
National and international guidelines (policy/macrosystem)
The Ministry of Health officials perceived that strategies for staff retention were in place. Specifically, they mentioned the hardship allowance policy, which grants additional payments to staff who work in remote locations.
The Ministry of Health officials in both countries thought that the existing policies on health workforce retention were comprehensive and adequate, and encompassed effective retention strategies. For example, the health policies in both countries mention that COs and AMOs have a higher retention rate, especially in rural settings, and were relied on for the bulk of health care in remote settings.
However, perceptions among health workers were different. Health workers raised claims of partiality, including nepotism, in allocating transfers, allowances, and opportunities for career progression and promotions.
The HRH policy is clear; we have developed strategies to improve motivation and retention of all health workers, we have special plans for those in remote areas, including a remote allowance. (KII, Ministry of Health, Tanzania)
I feel like, on deployment, we fell into the wrong hands, the authorities do not treat us in equal terms, there is apparent partiality. (CO, Malawi)
Overall, the retention strategies outlined by policy-makers did not concur with what health workers thought was important.
Partiality is very demotivating. After completing our studies, the Ministry of Health relocated most of us [COs in the ETATMBA program] to new facilities. Some of us complied with the transfer. Nevertheless, like me, my salary has not changed while others, just after reported to their facilities, their salary got increased, and they got a scholarship to go for further studies. It is unfair. (CO, Malawi)
Sometimes it is luck, but sometimes it is whom you know. For example, some of our colleagues are now working for the national [health] program. But I think they had someone to help them reach there. (CO, Malawi)
Health workers were aware of policies on retention but reported that the health authorities do not implement them. They also thought there was a lack of policies and systems to recognise exceptional achievement.
Sometimes you hear people talking about hardship allowance, but I have never received any allowance for working in this remote facility. I have been here for the past 18 years. (AMO, Tanzania)
We have a policy in place for hardship allowance … if they have not received it, it means they have not claimed it, but it is there. (KII, Ministry of Health, Tanzania)
On occasions, the participants received conflicting information from authorities, negatively affecting their motivation. In addition, the administrative line of authority was sometimes unclear to health workers. There were times when the Ministry of Health communicated HRH issues directly to the hospital leadership without informing the district level administration, causing confusion and dilemma for health workers.
To summarise these findings, the perspectives on retention and intention to leave by health workers tended to vary according to health workers’ factors, circumstances, and experiences. It is worth noting that each factor could pull in opposite directions – the same factors that will make some want to quit make others want to remain. A key observation was that perspectives on retention by health workers focused more on the first three levels of SEM – individual, close family, and the surrounding community – while key informants from the Ministry of Health focused more on the individual factors and the national HRH policies (macrosystem). In addition, there is a discrepancy between the policy – what is on paper against the HRH practice. Health workers highlighted issues of nepotism and favouritism, which may indicate people’s flaws and not necessarily faults with HRH policies.
Discussion
The application of SEM in health systems research, particularly in HRH, is limited. Some studies have applied a modified model without comprehensively addressing all five levels initially described by Bronfenbrenner14,20, which the authors attempt to apply in this study to provide a holistic view on health workforce retention and intention to leave.
Individual (intrapersonal) factors
Each individual is unique, and so are their job preferences and expectations. Despite the differences in job preferences, all health workers interviewed had opinions concerning factors that would make them leave or stay in the job. Some participants’ opinions changed over time, while others were maintained throughout the follow-up period.
The factors related to individual health workers, including the need for recognition, income, career progression, and a sense of belonging, are important and resonate with factors stated by health workers in previous studies21-24.
Participants in this study regarded a sense of belonging and income as crucial to retention, equally permeating through the first three SEM levels: intrapersonal, interpersonal, and mesosystem11,14,23-26. Likewise, non-monetary incentives such as formal recognition, career progression opportunities, and promotion were perceived to significantly encourage workforce retention21,27-29.
These findings support WHO’s strategies for improving retention15 and resonate with previous studies that show that factors that strongly influence retention strengthen health workers’ social and professional networks, improve monetary and non-monetary incentives, and avail career progression opportunities11,21,30. Therefore, health authorities need to recognise and support professional networks (eg through professional associations), allow flexibility in work–life balance, provide incentives, and avoid deploying lone staff to remote locations whenever possible.
Factors related to immediate family members (interpersonal/microsystem)
Most participants regarded the welfare of family members – parents, spouses, and children – highly, identifying family needs before outlining their own needs. They voiced concerns about good schools, suitable housing, and reliable health care as in previous studies3,4,11. On the contrary, policy-makers did not mention retention factors related to the family. However, two of the WHO strategies – incentives and personal support – can be regarded as focusing on the welfare of health workers’ families indirectly15. Therefore, health policies must state explicitly how health workers will be supported, especially those with young families, or how couples who are both health workers will be enabled to stay at the same facility.
Factors related to surrounding community (institutional factors/mesosystem)
In agreement with previous studies, participants in this study firmly indicated that stronger ties with the community, shown through taking responsibilities in community institutions, such as local schools, churches, or mosques, was a reason for retention14,23,26,31. Furthermore, this study and previous studies indicate that health workers who received support from rural communities during their studies show increased willingness to stay in remote settings to give back to the community. Although the exact mechanisms of how enhanced social ties occur between health workers and rural communities is not yet clear, invariably studies indicate a positive association between healthcare worker’s rural exposure and willingness to remain in rural locations longer32-41. Cosgrave et al (2019) suggest that place-based social processes that occur during rural exposure inculcate a positive attitude in healthcare workers regarding rural placement37. This finding attests to the contemporary relevance of the WHO recommendation of selecting students for healthcare training from rural backgrounds, establishing healthcare institutions in rural settings and developing training curriculums that ensure adequate and positive rural community health exposure15.
Another crucial aspect of how the community influences retention occurs at the healthcare facility. Friendly and supportive leadership and colleagues were perceived to strongly encourage retention. In addition, health workers who assumed leadership responsibilities following the ETATMBA program envisaged a more profound sense of belonging. These findings align with previous findings and resonate with WHO’s recommendation for personal and professional support3,4,9,15,25,29,31, as discussed earlier under personal factors.
Conversely, health workers perceived unfair HRH management practices such as partiality on promotion, salary increment, and in allocating career progression opportunities as demotivating and seriously reducing retention. For example, while some ETATMBA trainees had received salary increments, others had not. Health workers from previous studies in Malawi and Tanzania, and from other low-resource countries echo similar grievances3,6,42,43.
Health workers condemned unsupportive leadership as a deterrent to retention. However, improving health workers’ personal and professional support in rural and remote settings does not need substantial resource investments, and should be prioritised31. For example, the existing support given by the facility leadership, colleagues, or professional associations could be structured, formalised, strengthened, and scaled along with improvements in the management style.
Factors related to political, legal, and security issues (exosystem)
Although participants in this study did not discuss societal issues such as political stability, legal, economic, and security issues, these factors affect health workforce retention in other countries. For completeness, it should be mentioned that political instability and security concerns are the most significant factors for retention in other settings42,43, and should be taken into account when devising HRH policies. For example, during the economic crisis in Zimbabwe, the health sector implemented a flexible deployment policy by lifting bonding restrictions and prioritising deployment to areas most in need in order to improve access to the rural health workforce44, an approach highly recommended.
National and international guidelines (policies/macrosystem)
Failure to implement comprehensive HRH policies and strategies is a factor that health workers highlighted in this study (on mesosystem factors) and has been observed in other countries4-6,9-11,27,28. On occasions, health workers in this study received conflicting directives from district and national authorities, leaving them in a dilemma, which would discourage retention.
For example, health workers in both countries got transferred to facilities lacking the equipment and consumables that would allow them to apply the skills acquired during ETATMBA training, indicating deficiencies in the planning and coordination at the managerial level, which wouldn’t need expensive investments to improve.
Conclusion
The authors have outlined the perspectives on factors affecting retention, and intention to leave by mid-level health workers – a workforce less frequently included in HRH research – and those of policy-makers as appraised by SEM, and show that the factors are multi-layered and interlinked. Individual preferences and local context influence health workers’ views on retention and how they respond to these factors, such that the same factor could have a negative or a positive effect on retention. Health workers and policy-makers support intrapersonal factors in line with WHO’s recommendations for improving access to the health workforce in rural and remote settings. However, while health workers emphasise interpersonal and community factors, policy-makers focus on system factors, a discrepancy that is cause for concern. Therefore, health authorities need to align health policies to health workers’ expectations. Although some interventions, such as increasing the exposure of health workers to rural communities during training, could be costly, health authorities could prioritise low-cost interventions such as implementing policies that recognise and protect the needs of young families, strengthening personal and professional support and reorganising HRH management, eg flexibility in deployment. SEM could be applied locally or regionally to identify context-specific individual and community factors. Including such factors in HRH policies, regularly evaluating them, and adapting accordingly is likely to reduce health inequality and improve access to the health workforce in rural and remote populations.
Funding
The study was part of the ETATMBA program funded by the European Union.
Conflicts of interest
The authors received financial support from ETATMBA for travel and stipend expenses during data collection.
Acknowledgements
The authors thank Professor Nynke van den Broek for her contribution in conceptualising the study, Professor Tim Martineau and Professor Gerry Davies for their expert guidance, and Caroline Hercod at the Liverpool School of Tropical Medicine for proofreading the manuscript.


