Introduction
Severe mental disorders (SMDs) affect 4% of the adult population globally and account for 26.1% of the reported cases of mental disorders in South Africa1,2. These disorders include major depressive disorder, bipolar mood disorder, schizophrenia, and other psychotic disorders3. Although no official statistics exist on SMDs in rural South Africa, a profile of common causes of mental illnesses in Mpumalanga, a rural province, revealed that most patients were diagnosed with bipolar mood disorder, schizophrenia, major depressive disorder, and substance induced psychosis4. People with SMDs experience a decline in function, and their ability to live independently is compromised. This dependency on others results in enormous social and economic burdens on themselves, their informal caregivers, and their communities5.
Caregiver burden is described as the strain encountered by a person providing care to someone who is chronically ill6, and can be categorised into objective and subjective burdens7. Objective burden relates to the tangible negative effects of caregiving that arise from the demands of the tasks required to care for a person with a mental disorder8. This burden is characterised by disruption in family routines, restrictions on families’ social and leisure activities, and additional financial costs incurred due to caregiving6. Subjective burden relates to the perceived feeling of getting overwhelmed as a result of providing care to a person with a mental disorder8. This burden is characterised by negative appraisal of the caregiving circumstances, which results in feelings of loss, guilt, shame, and anger7.
Studies conducted in Sub-Saharan countries found that the extent of caregiver burden among informal caregivers of people with mental disorders ranges between 60% and 90%9-11. Studies conducted in Ethiopia found that 63% of informal caregivers of people with schizophrenia and bipolar mood disorder experience moderate-to-severe caregiver burden10. Similarly, a study conducted in Nigeria found that 45% of caregivers of people with major depressive disorder experience a moderate-to-severe subjective burden12. In South Africa, 43.4% of caregivers of people with schizophrenia were reported to experience severe caregiver burden13.
In rural and remote areas where general access to mental health services is limited, the sustained care and management of those with SMDs often becomes the responsibility of informal caregivers. The role of informal caregiving is often filled by family and at times by friends, neighbours, or any compassionate person, who are often unpaid while providing ongoing care to a person with an SMD14. Informal caregivers assume responsibility for the day-to-day needs of people with SMDs, manage their behaviour, monitor their mental state, and identify the early signs of illness relapse and deterioration15. Additionally, they are expected to supervise compliance with medication, provide emotional support, and help the people with SMDs access mental health services16-18. Most informal caregivers within rural and remote areas struggle to access mental health services to support them in providing adequate care to people with SMDs19-22. It is important to understand the extent of caregiver burden among informal caregivers because this forms the basis for the development of strategies to support caregivers in their role.
In rural South Africa, there is limited published evidence on the extent of subjective and objective caregiver burden among informal caregivers of people with SMDs. This study therefore aimed to establish the extent of subjective and objective burden experienced by informal caregivers. This forms part of a PhD project aimed at developing strategies for alleviating caregiver burden among informal caregivers of people with SMDs in rural South Africa.
Methods
Context and setting
The study took place in an acute mental health unit situated in Bushbuckridge municipality in the Mpumalanga province of South Africa. Mpumalanga province is a rural province in the north-east of South Africa. The population size of Bushbuckridge municipality is 546 215, and the municipality has an estimated average annual household income of US$850 (~A$1280)23. The acute mental health unit is considered the largest in the province, with a bed capacity of 50, and caters for a variety of patients, ranging from acute to chronic and forensic cases. Therefore, all patients with SMDs requiring long-term care are referred to this unit for further management. After discharge, patients with their caregivers attend follow-up visits at the outpatient clinic, which take place once per week at the mental health unit. Depending on the severity of their conditions, patients are required to attend their follow-up visit 1 month after discharge or every 6 months for review. If the patient is deemed stable after the first follow-up visit, they are referred to their local clinic for further management. Due to the limited mental health services in the province, the unit caters for a large catchment area, which was further expanded by the introduction of forensic services in 2014. As a result, there is a shortage of staff to cater for the needs of the patients and their caregivers. Currently, the unit has a multidisciplinary team consisting of a part-time psychiatrist and a medical officer who work 3 days per week. Nursing staff consist of a psychiatrically trained sister in charge of the unit, a professional nurse, and an auxiliary nurse per 7-day shift. One social worker, a registered counsellor, and two occupational therapists facilitate the rehabilitation programs for both in- and outpatients in the unit. At the local clinics there are nursing staff, and a medical officer who visits the clinic once a month to offer mental health services.
Study design
This study used a quantitative, descriptive cross-sectional design. The data were generated through structured interviews with the participants.
Measures: The demographic and caregiving characteristics were gathered using a questionnaire developed by the first author from existing literature. The burden measure developed by Montgomery, et al24 was used to measure objective and subjective burdens. This scale was considered appropriate as it is multidimensional, and therefore provides aggregate scores for objective and subjective burdens. This instrument comprises the following 22 items: 9 items on objective burden with a Cronbach alpha of 0.85, and 13 items on subjective burden with a Cronbach’s alpha of 0.86. Each subscale item is rated using a five-point Likert scale (Table 1). For objective burden, the global scores range from 9 to 45, with higher scores indicating a higher burden, and the subjective burden global scores range from 13 to 65, with the higher scores indicating a higher burden. Table 2 outlines the five categories representing the levels of severity for both objective and subjective burdens24.
Permission was received from the instrument developers to use and modify the instrument for the study context. A pilot study was conducted to establish the validity and reliability of the burden measure. Face validity, a subset of content validity, was conducted by inviting six participants who were considered knowledgeable in mental health to give their subjective opinions on whether the instrument measured the objective and subjective burdens as intended25. The identified participants rated each subscale item using four categories: relevance, clarity, simplicity, and ambiguity25. Items requiring revision were modified for clarity based on the recommendations of the participants. Prior to data collection, the revised scale was sent back to the pilot participants for the finalisation of the items on the instrument. In addition, the inter-rater reliability was conducted to determine the reproducibility of the results when using the burden measure. The researcher and two trained research assistants were required to independently administer the burden measure, with 10 informal caregivers recruited from the research site. These informal caregivers were excluded from the overall sample of the study. A standardised instruction sheet was used to ensure homogeneity in the process followed by the three raters. A weighted kappa was calculated using the Statistical Package for the Social Sciences v27 (IBM; https://www.ibm.com/products/spss-statistics) to determine the level of agreement between the raters. Landis and Koch’s classification was used to determine the acceptable kappa value, where 0 was regarded as poor agreement, 0.00–0.20 as slight agreement, 0.21–0.40 as fair agreement, 0.41–0.60 as moderate agreement, 0.61–0.80 as substantial agreement, and 0.81–1.00 as almost perfect26. The weighted kappa value of 0.69–0.86 was established as indicating a substantial to almost-perfect agreement between the three raters, proving the reproducibility of the results when using the Montgomery, Gonyea, and Hooyman burden measure26.
Table 1: Objective and subjective burdens subscale score descriptors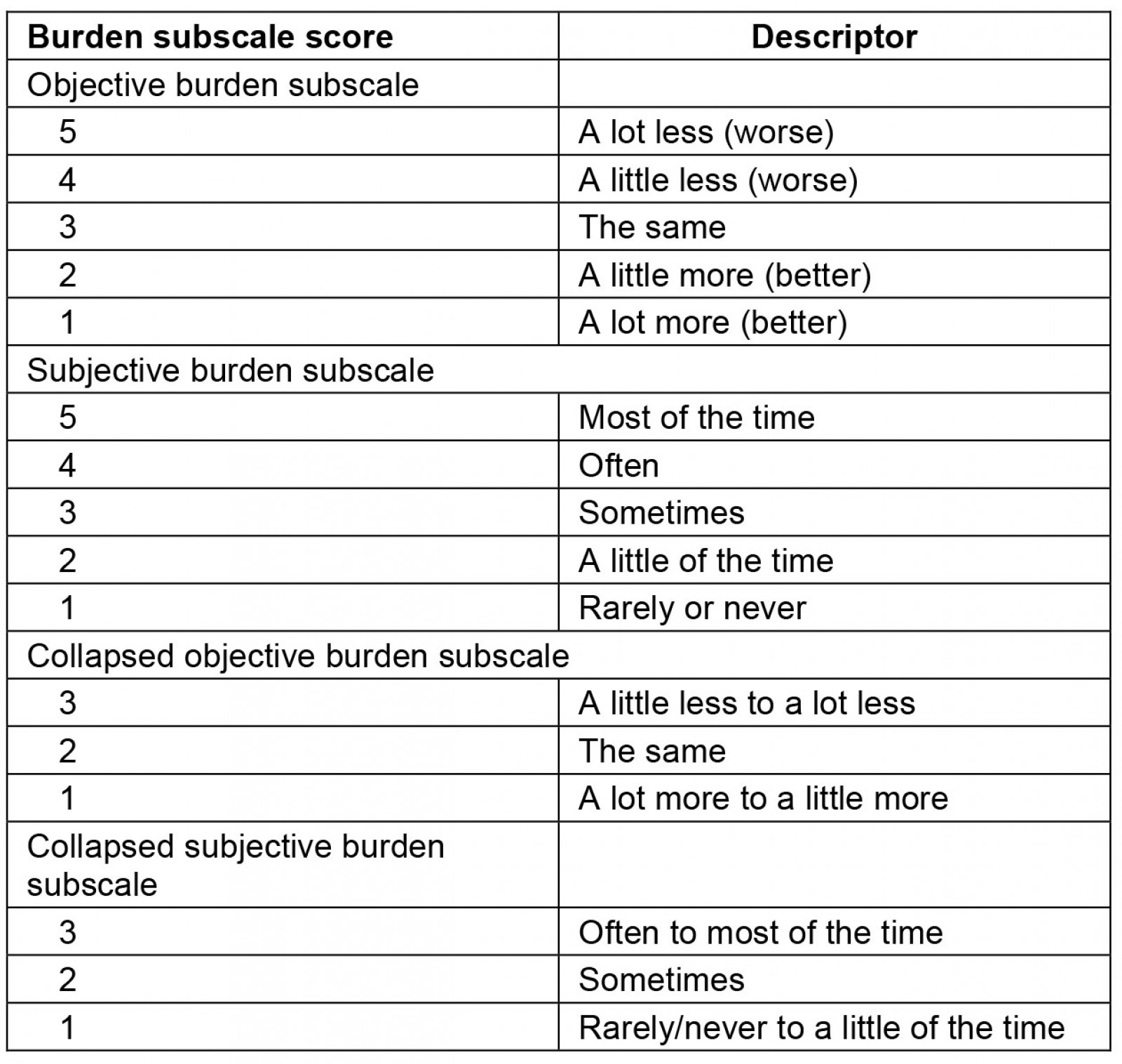
Table 2: Objective and subjective burdens severity categories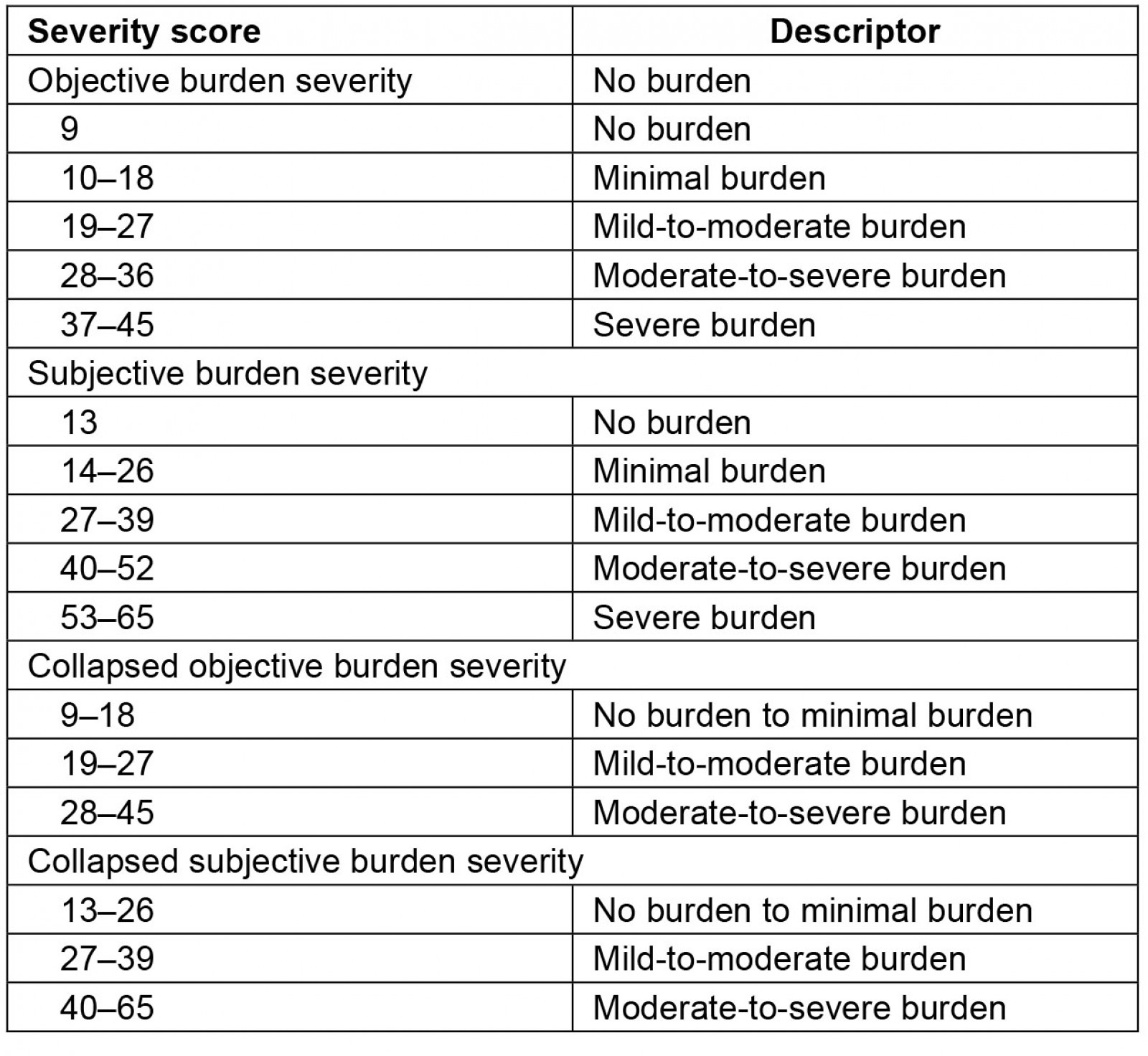
Data collection: Data were collected using structured interviews conducted by the first author along with two trained research assistants. This process took place over a period of 6 months, starting from March 2021.
Sampling size and method: To estimate the sample size of the informal caregivers, sample size calculations were based on the number of patients attending the outpatient clinic at the research site with an assumption that each patient has one informal caregiver. An estimated number of 353 mental healthcare users were identified as attending the outpatient clinic at the research site per month. Therefore, a sample size of 185 informal caregivers was required when the margins of the error were set at 5% with a confidence interval of 95% on Cochrane’s formula27. A non-probability convenience sampling method was used to recruit informal caregivers of people with SMDs who accompanied their care recipients to follow-up visits at the outpatient clinic. Participants were approached in the queues as they waited to be seen by the doctor. The purpose of the study was explained to the group of informal caregivers, and those willing to participate were interviewed in a separate room before or after being seen by the doctor, depending on their preference.
Inclusion criteria: A set of inclusion criteria was used to identify suitable participants for the study. The inclusion criteria were (1) informal caregivers included a family member, a relative, a friend, or any person who provided unpaid care to a person with an SMD; (2) the informal caregiver had provided continuous care for the person with an SMD for more than 6 months; (3) the age of the informal caregiver was more than 18 years; and (4) the informal caregiver performed activities associated with caregiving at least once a week (administering medication, assisting with and structuring daily activities). Informal caregivers with physical conditions or chronic illnesses (including mental conditions) were excluded to avoid confounding factors that could arise from difficulty in dissociating the burden resulting from caregiving and the burden caused by their own disability or illness.
Statistical analysis: Stata v15 software was used for the data analysis. Descriptive statistics were used to summarise the demographic and caregiving characteristics of the informal caregivers, the severity of the objective and subjective burdens, and the level of burden projected by each item on the two subscales. To determine the level and severity of objective and subjective burdens, the data were collapsed into three categories and the ratings of each subscale were grouped together. Categories were collapsed to produce summary statistics and enable better data management (Tables 1, 2). In addition, for the purpose of this study, the severity of the burden was identified based on the three revised categories for both objective and subjective burdens (Tables 1, 2). The Pearson χ2 was computed to test the association between the objective and subjective burdens with demographic and caregiving characteristics.
Ethics approval
Ethics clearance (M200957) was obtained from the University of the Witwatersrand Human Research Ethics Committee. Permission to conduct the study was obtained from the CEO of the research site, and the Mpumalanga Department of Health Research Committee granted final approval (MP_202010_010). All participants were required to sign an informed consent form declaring their willingness to engage in the study. Each participant was allocated a unique participant code to ensure the anonymity of the data.
Results
Demographic characteristics of informal caregivers
The results of the study as outlined in Tables 3 and 4 reveal that most of the informal caregivers were female (83.5%) in middle-to-late adulthood, with the majority (45.3%) in the age range of 45–64 years, followed by those in early-to-middle adulthood with the age range of 34 years and younger (34%). Many informal caregivers reported being single (57.1%) with a high school level of education (53.0%). Participants who were unemployed and dependent on a social grant formed the majority of the sample (39.4%).
Table 3: Associations between the demographic characteristics and levels of objective caregiver burden (n=170)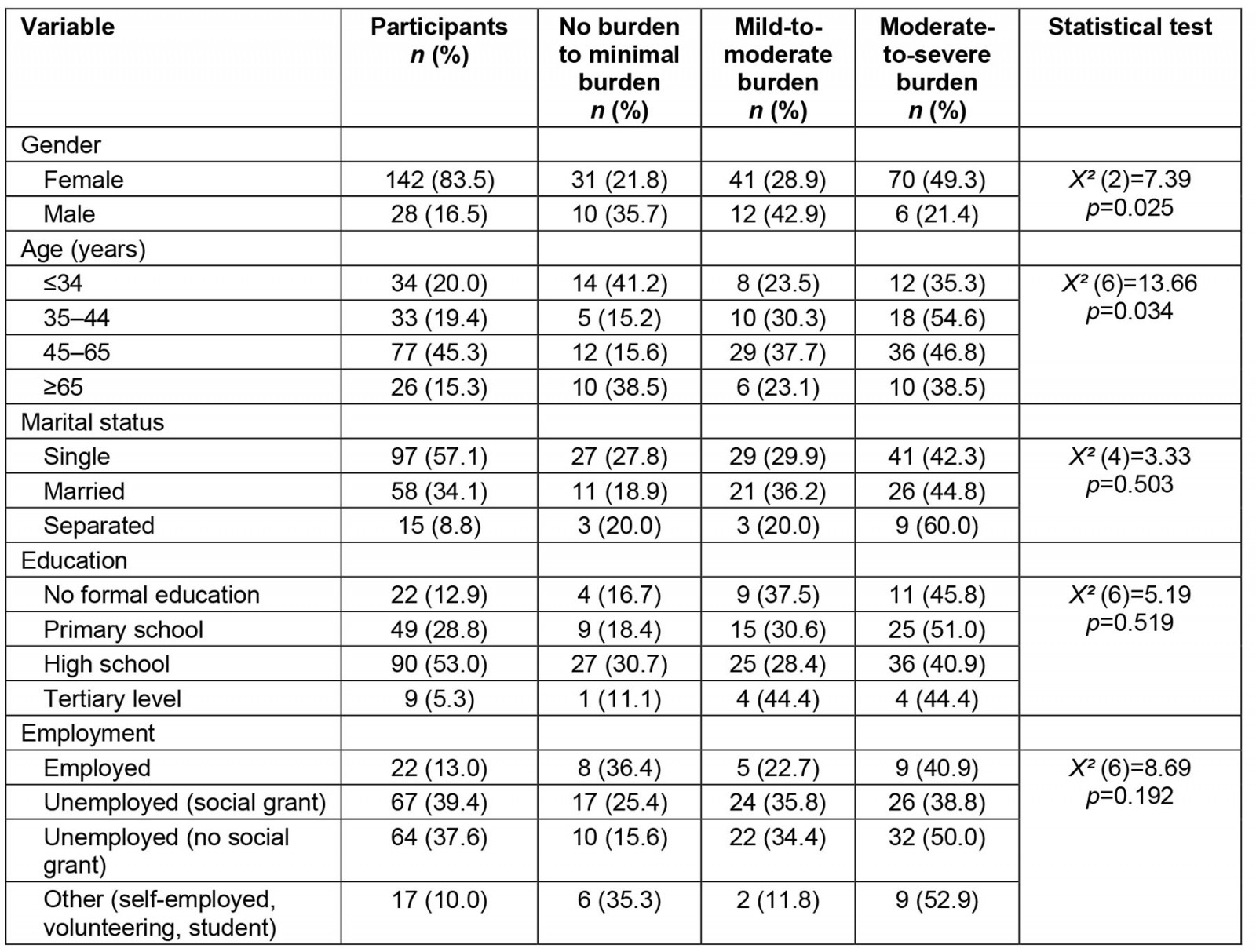
Table 4: Associations between the demographic characteristics and levels of subjective caregiver burden (n=170)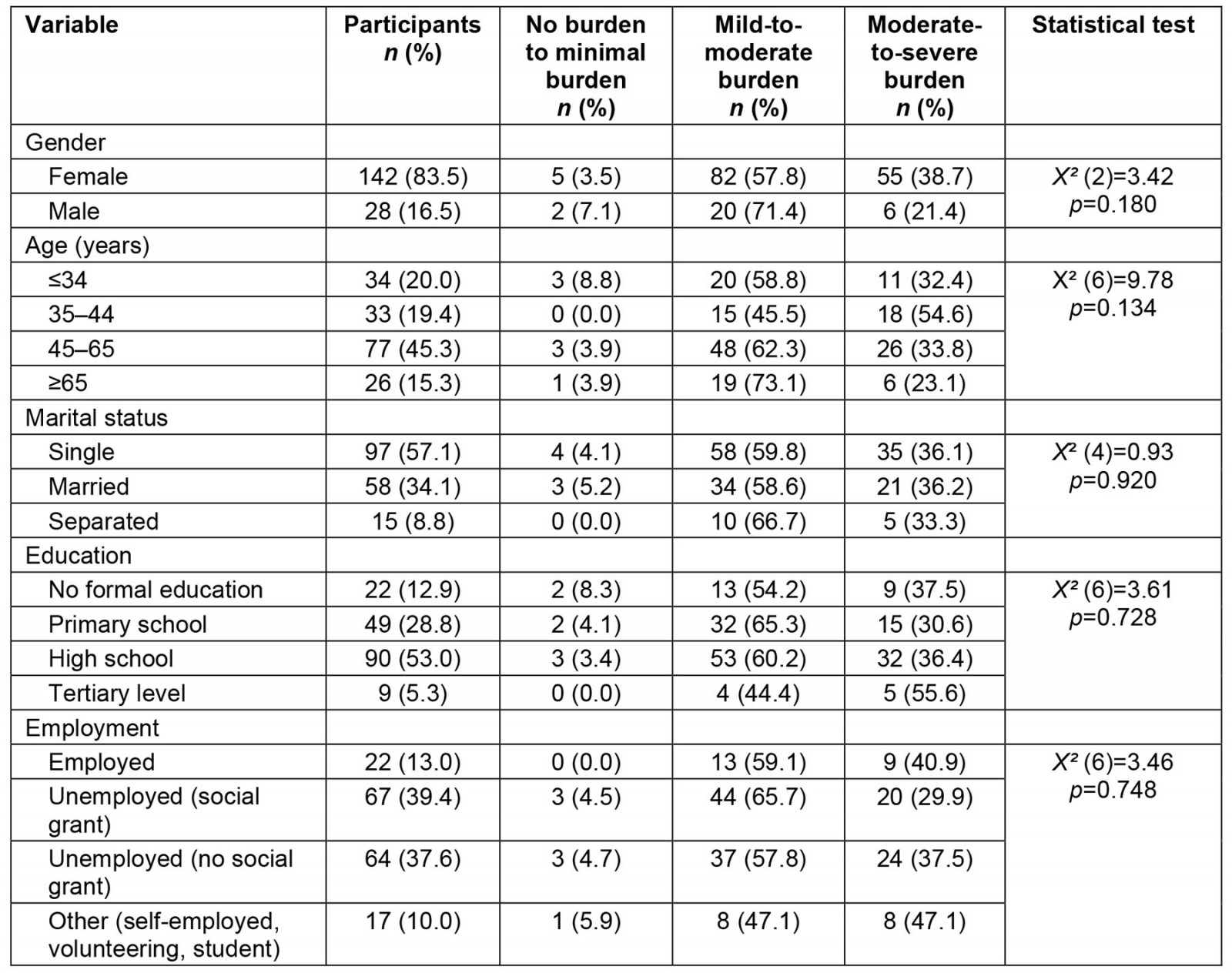
Caregiving characteristics of informal caregivers
Most informal caregivers were parents of the care recipient (45.3%), followed by siblings (24.7%), and the majority of caregivers resided at the same residence as their care recipient (81.2%). The majority of the sample (47.0%) had been providing care for the individual for 5 years or less. The hours spent in daily caregiving varied between one and 24 hours, and most of the informal caregivers spent 8 hours or less daily (53.5%), followed by those who spent 19–24 hours daily (28.8%). The care recipients were diagnosed mainly with schizophrenia (52.8%), and those with a psychotic disorder not otherwise specified accounted for 27.1% of those receiving care from informal caregivers. Care recipients with bipolar mood disorder, substance-induced psychosis, and major depressive disorder accounted for 10.6%, 7.1% and 2.4% of care recipients, respectively. Most of the participants (61.8%) spent less than 100 South African rand (~A$8) per month, with some (34.1%) spending up to 500 South African rand (~A$40) per month for the medical costs of the care recipients (Tables 5, 6).
Table 5: Associations between the caregiving characteristics and levels of objective caregiver burden (n=170)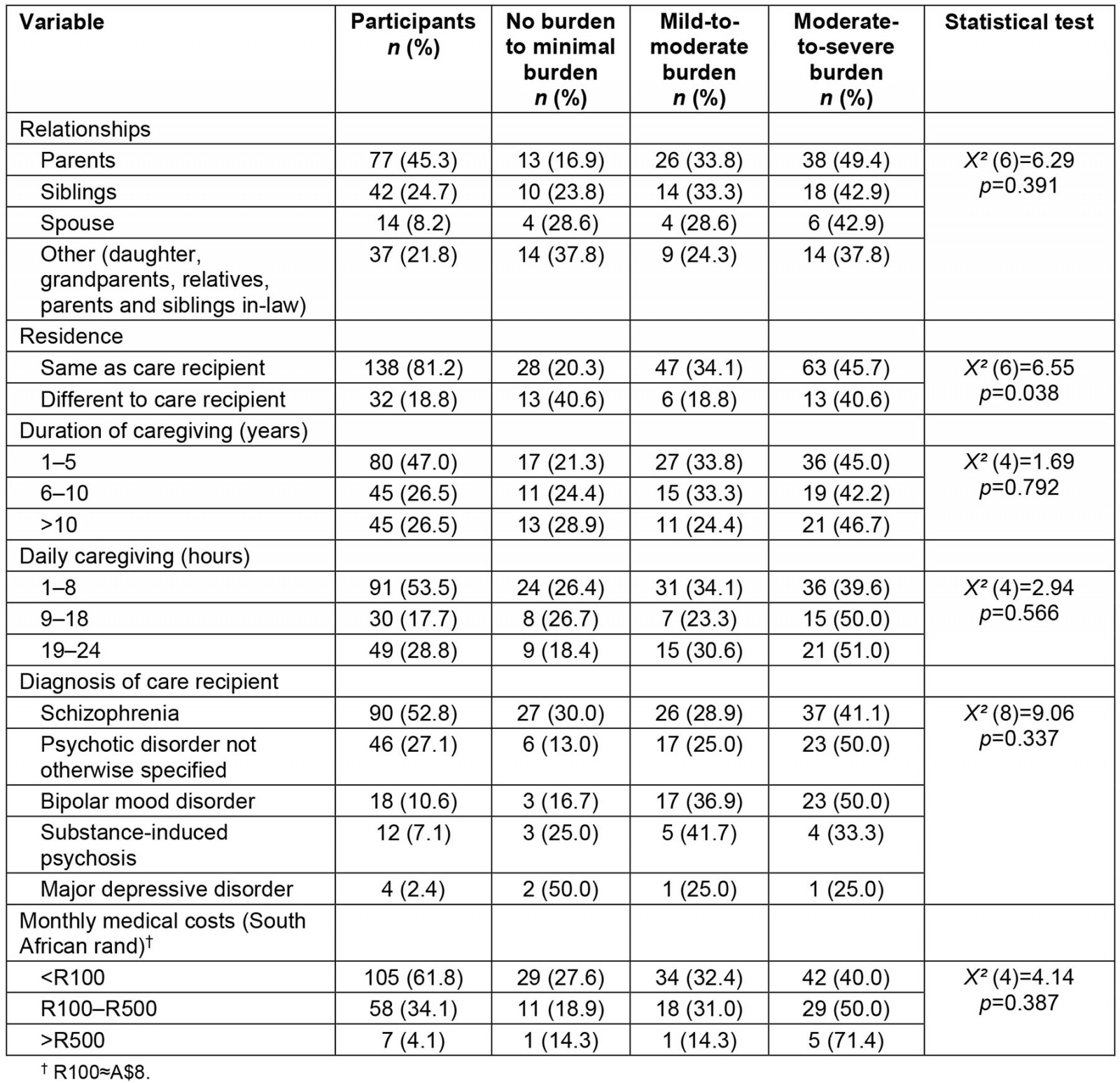
Table 6: Associations between the caregiving characteristics and levels of subjective caregiver burden (n=170)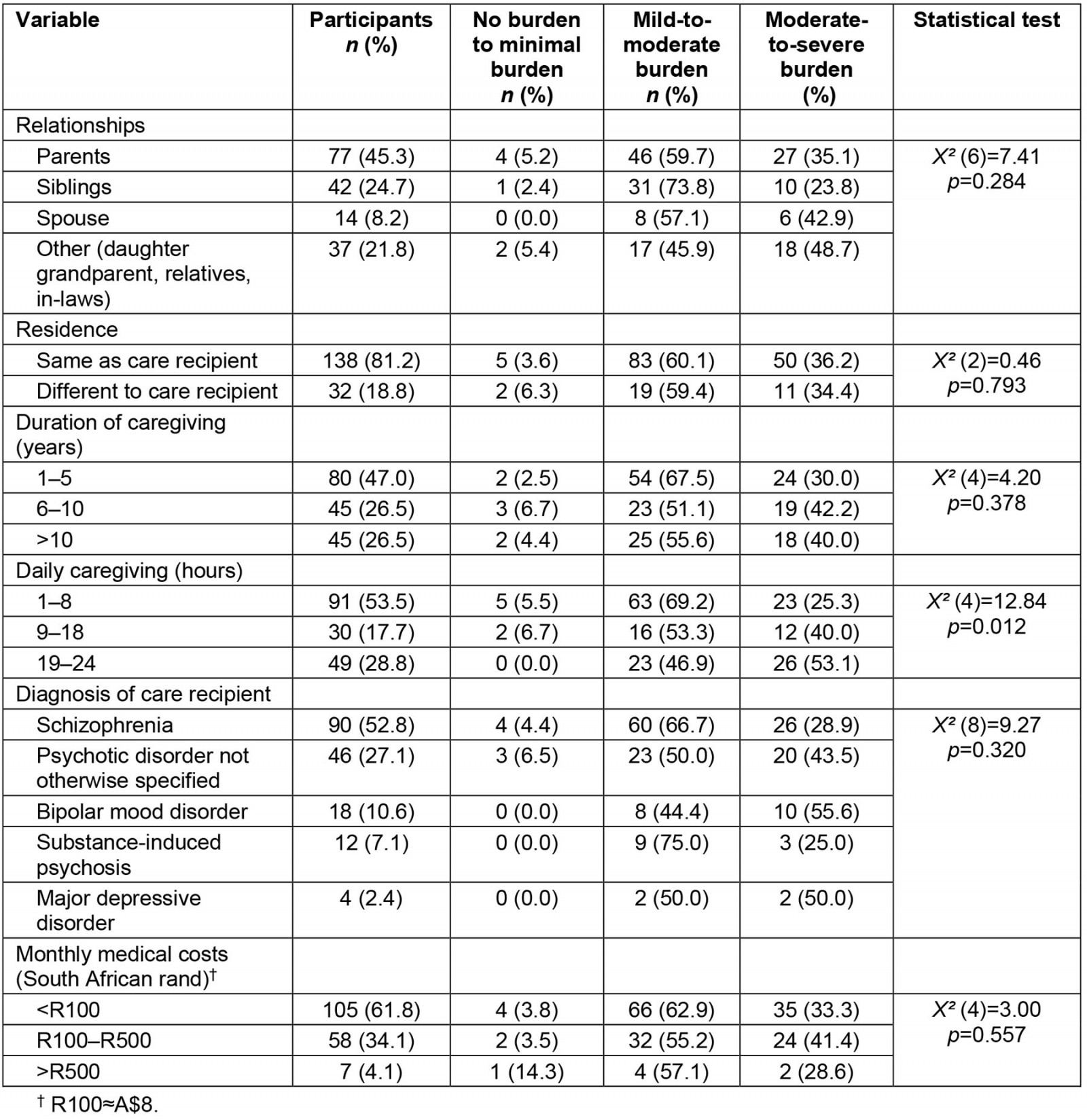
Associations between caregiver burden and demographic characteristics
The results revealed a significant association between gender and objective burden. Female participants reported a significantly higher burden than males, with most (49.3%) reporting moderate-to-severe objective burden (X² (2)=7.39; p=0.025). Similarly, the associations between age and objective burden yielded significant results, with many informal caregivers aged between 45 and 65 years (46.8%) reporting moderate-to-severe burden (X² (6)=13.66; p=0.034). Thus, older caregivers reported a higher burden of care. While most participants were unemployed and dependent on a social grant, the findings revealed that the associations between employment status and objective burden were statistically insignificant. The associations between the demographic characteristics and subjective burden were not statistically significant (p>0.05; Tables 3, 4).
Associations between caregiver burden and caregiving characteristics
The informal caregivers who resided with care recipients reported significantly higher objective burden, with most participants (45.7%) reporting moderate-to-severe burden (X² (6)=6.55; p=0.038). The associations between objective burden and other caregiving characteristics were not significant (p>0.05). The associations between daily caregiving and subjective burden yielded significant results, with most informal caregivers (53.1%) who provided care for 19–24 hours reporting a moderate-to-severe burden (X² (4)=12.84; p=0.012). No associations were established between subjective burden and other caregiving characteristics (p>0.05; Tables 5, 6). While there were no significant associations between care recipients’ diagnoses and objective and subjective burdens, it is important to note the levels of these burdens (Tables 5, 6).
Objective and subjective burdens global scores
The global burden scores revealed considerable burden among the informal caregivers. Most informal caregivers (44.7%) reported moderate-to-severe objective burden, followed by those who reported mild-to-moderate burden (31.2%). Those with no burden to minimal objective burden accounted for 24.1% of the sample (Fig1). Similarly, most informal caregivers (60%) reported mild-to-moderate subjective burden, while 35.9% reported moderate-to-severe subjective burden, and the least number of participants (4.1%) reported no burden to minimal subjective burden (Fig2).
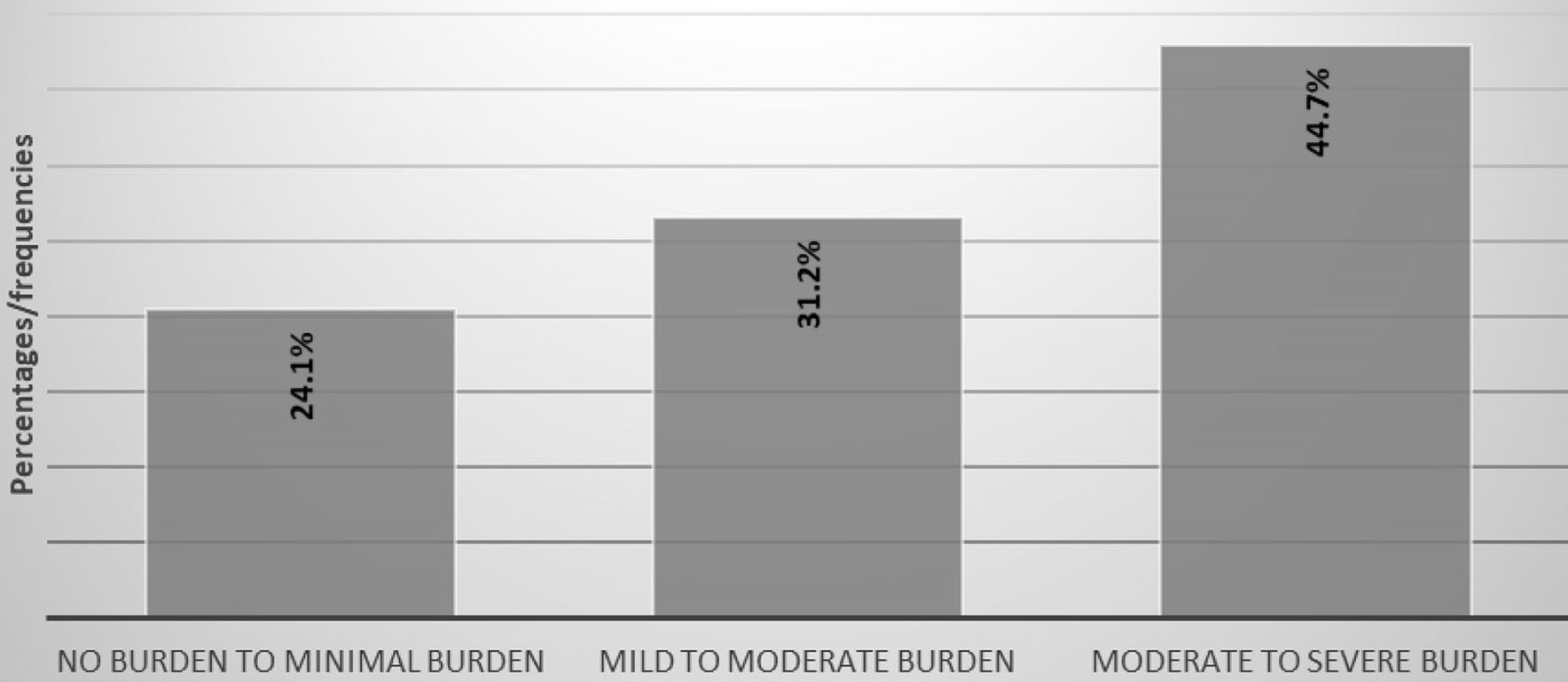 Figure 1: Informal caregiver objective burden global scores (n=170)
Figure 1: Informal caregiver objective burden global scores (n=170)
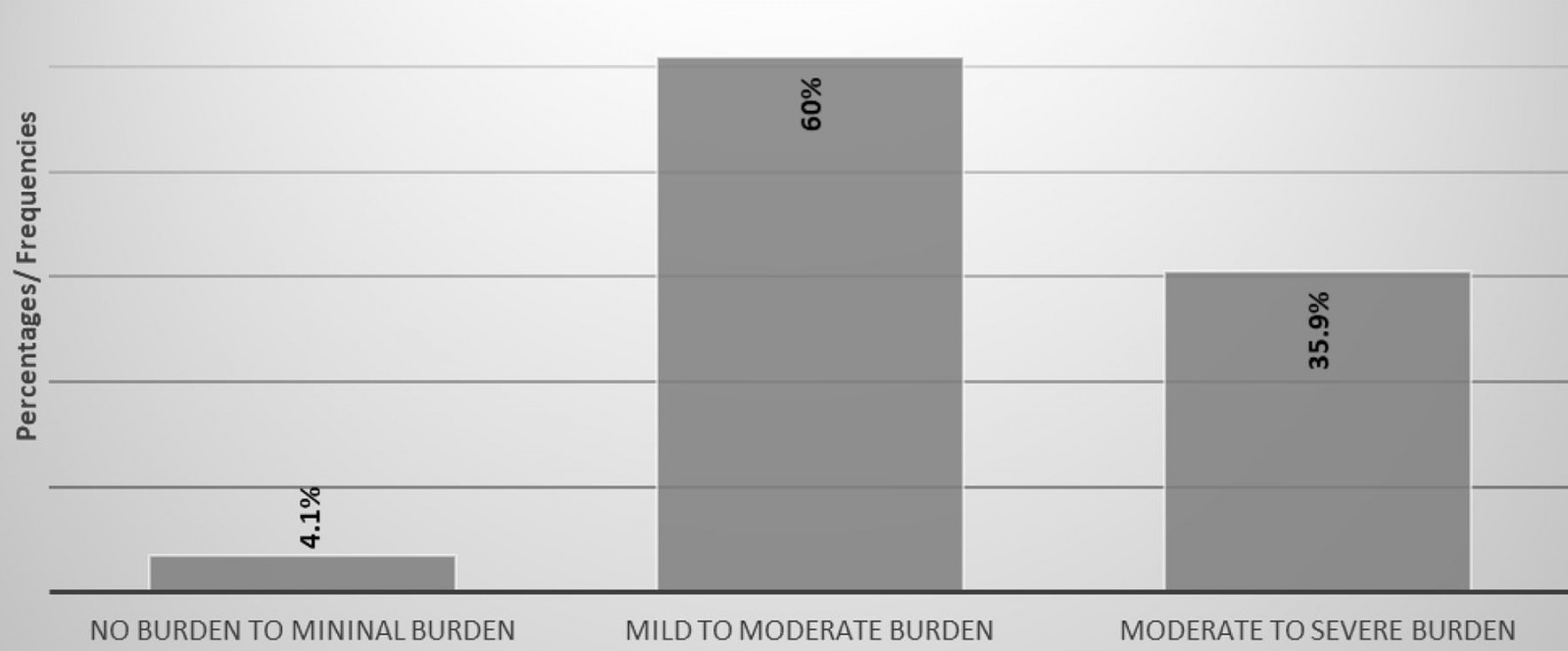 Figure 2: Informal caregiver subjective burden global scores (n=170)
Figure 2: Informal caregiver subjective burden global scores (n=170)
Discussion
The global burden scores for both objective and subjective burdens revealed a higher burden among the informal caregivers in rural South Africa. A majority of the informal caregivers (44.7%) reported moderate-to-severe objective burden, and 35.8% reported moderate-to-severe subjective burden. This indicates that the severity of objective burden was higher than that of subjective burden. The results of this study differ from previous studies conducted in Sweden and Nigeria that reported higher subjective burden among informal caregivers of people with schizophrenia8,28,29. Additionally, a study conducted in Nigeria indicated that 45% of informal caregivers of people with major depressive disorder reported moderate-to-severe subjective burden12.
The higher levels of objective burden can be attributed to various factors, including the gender and age of the informal caregiver. In the present study, most of the informal caregivers were women (83.5%), with significant associations established between gender and the objective burden reported by informal caregivers (p=0.025). This is consistent with previous studies conducted in other developing countries, including South Africa, that identified that most informal caregivers tend to be women11,13,30-33. These findings are not surprising as caregiving is considered a traditional role that best fits women in the home and community13,33.
Female informal caregivers occupy many roles that predispose them to higher burdens than their male counterparts. The roles include being a mother, worker, house maintainer and key emotional supporter11. A study conducted in India among informal caregivers of people with bipolar mood disorder highlighted that cultural issues such as restriction of females to household duties, the inability to spend time on leisure activities, and the financial dependency were associated with high burden among informal caregivers33. In rural South Africa, women are responsible for overseeing the day-to-day running of households and, as a result, when a responsibility for caregiving arises, their routines are disrupted, resulting in less time for self and socialisation, leading to objective burden34. Therefore, the findings in this study highlight that gender can be considered a predictor for objective burden among informal caregivers of those with SMDs35,36.
The results revealed non-significant associations between objective burden and employment status; however, it is important to note that both employed and unemployed informal caregivers reported higher levels of objective burden. It could be that the informal caregivers struggled to meet the expenses of the household and provide for the needs of the care recipients in spite of their employment status. The results in this study are similar to a study conducted in rural Ethiopia that revealed that caregivers reported higher levels of burden related to financial problems, often due to the cost of treatment37. The informal caregivers in this study were expected to meet basic household expenses, and they were required to deal with the additional cost of providing care, which includes covering the transport costs to the hospital for follow-ups. Marimbe et al highlighted that the increased financial burden may be related to the fact that some informal caregivers frequently forego economic opportunities to fulfil their caregiving responsibilities33. It is therefore necessary to plan and implement community-based programs that enable caregivers to take up income-generating roles to increase household income38.
Although no significant associations were established between subjective burden and the demographic characteristics of the informal caregivers, most males (71.4%) and females (57.8%) reported mild-to-moderate subjective burden. This highlights that male caregivers in this study reported the same level of subjective burden as females. These findings differ from previous studies conducted in Sweden and Nigeria that reported that females experienced higher subjective burden than men29,38. The findings of the present study are worth noting as they emphasise that research aimed at developing strategies for alleviating subjective burden should focus on the needs of both male and female caregivers.
The majority of the informal caregivers in this study were older adults in middle-to-late adulthood, and many were aged between 45 and 65 years (45.3%), with some aged 65 years or more (15.3%). These findings are consistent with a study conducted in South Africa that revealed that most caregivers are above the age of 55 years and that 15.8% are above the age of 65 years13. The increased age of the informal caregivers in this study yielded a significant association with established levels of objective burden (p=0.034). These results are concerning as old age is associated with poor quality of life and a decline in health caused by comorbidities13. Additionally, older caregivers often have decreased energy levels to perform daily activities, reducing their ability to cope with the demands of caregiving6,36,38,39. The age of the informal caregivers and the schizophrenia diagnosis of most of the care recipients in this study are concerning facts given the recovery patterns of this mental disorder. Schizophrenia is associated with serious functional and social impairments as well as unpredictable and risky or even hostile behaviours, which demand more time and structure from informal caregivers40-45. Considering declining health and energy levels among elderly people, this means that the burden of care becomes the responsibility of those who may be struggling to care for themselves, and this may have serious consequences for continuity of care for the care recipients. In a resource-constrained context like rural South Africa, there is limited access to mental health services, and thus informal caregivers are the backbone of recovery for mental healthcare users. The combination of a resource-constrained healthcare system and the advanced age of caregivers poses a serious threat to the quality of caregiving, which can aggravate relapses in people with SMDs46. Therefore, this is likely to perpetuate a cycle of the ‘revolving door’ phenomenon that is constantly crippling the mental health system in South Africa47.
Most informal caregivers in early-to-middle adulthood (35–44 years) reported a moderate-to-severe subjective burden (54.6%). Most caregivers at this age are in their productive stage and actively participating in working life27. In this study, 22 (13%) informal caregivers reported being in full-time employment. According to Flyckt, et al, employed informal caregivers experience reduced productivity and often struggle to cope with a full-time working week40. This is attributed to the fact that the demands of caregiving and work often compete for the same limited resources, such as time, financial, and psychological resources48. Consequently, most informal caregivers are likely to experience high levels of stress, which results in reduced mental health and wellbeing, precipitating limited productivity48. Some studies conducted in Europe revealed that employed informal caregivers reported high rates of absenteeism compared to non-caregiving employees49,50. Additionally, the caregivers were more likely to exit the open labour market prematurely compared to those who did not have caregiving responsibilities47. Therefore, it is important that strategies be implemented to support working informal caregivers, to prevent them from losing their incomes.
In the present study, a significantly higher subjective burden was established among informal caregivers who spent prolonged hours in daily caregiving (p=0.012). Those who spent 1–8 hours (69.2%) in daily caregiving reported mild-to-moderate subjective burden, but those spending 19–24 hours (53.1%) reported more severe subjective burden. It is not surprising that increased time spent on daily caregiving leads to an increase in the severity of subjective burden reported by the informal caregivers, considering that most (81.2%) stay in the same residence as the care recipient. Ayalew et al9 also identified that informal caregivers who spent long hours in daily caregiving expressed feelings of higher burden. With increased time spent on caregiving, the informal caregivers had less time for themselves, which predisposed them to increased burden51-53 and burnout, manifesting as physical, emotional, and mental exhaustion54. Informal caregivers who experience caregiver burnout are likely to express high levels of emotion, including critical comments and emotional hostility toward care recipients55. Experiencing criticisms and hostility acts as a stressor, which may be a causative factor leading to a person with SMDs experiencing relapse56.
Limitations
The limitations of this study include the cross-sectional design and convenience sampling of participants at a single research site, which means these findings may not be able to be generalised to other populations. The omission of care recipient characteristics, such as their age, gender and duration of illness, in this study prevented a comprehensive understanding of the factors associated with caregiver burden. Future studies should therefore investigate the impact of care recipients’ characteristics on the burden of care reported by informal caregivers in rural areas. Incorporating a qualitative component could add value in the in-depth exploration of caregiver burden, and this is an area that can be explored in future research.
Conclusion
Caring for individuals with SMDs is associated with considerable levels of objective and subjective burdens for the informal caregivers. The impact of these burdens on the health and wellbeing of the informal caregivers and the spill-over effect of this to the quality of care received by care recipients have been clearly defined in previous studies. The findings in this study highlight the need to integrate the assessment of burdens among informal caregivers of people with SMDs in routine clinical practice. This can be done by ensuring that regular assessments are conducted to determine who is providing care and to determine the mental and physical status of the informal caregiver. It is important that gender stereotypes, such as labelling caregiving as a female-oriented activity, be addressed to ensure that both males and females are equally involved in the role of caregiving. Support strategies such as respite care may be implemented by involving other family members in caregiving activities to ensure the distribution of the caregiving demands. This can be achieved by strengthening community-based mental health services such as setting up day centres where people with SMDs can participate in activities to provide some respite to informal caregivers. To alleviate the financial burden of informal caregivers, it is recommended that governments implement a caregiver grant as an incentive, particularly in low-resource settings where employment opportunities are limited.
Acknowledgements
The authors acknowledge the informal caregivers of people with SMDs in the Bushbuckridge municipality for participating in the study, Dr Denise Franzsen and Dr Eniola Bamgboye for their assistance with the statistical analysis, and the Consortium for Advanced Research Training in Africa for funding the study and for their exceptional training program, which has enhanced the first author’s academic writing skills.
Statement of funding
This research was supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No. G-19-57145), Sida (Grant No:54100113), Uppsala Monitoring Center, Norwegian Agency for Development Cooperation (Norad), and by the Wellcome Trust [reference no. 107768/Z/15/Z] and the UK Foreign, Commonwealth & Development Office, with support from the Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa) programme. The statements made and views expressed are solely the responsibility of the Fellow.
References
You might also be interested in:
2018 - Oral Health Disparities among Adolescents from Urban and Rural Communities of Central Chile
2016 - Towards understanding the availability of physiotherapy services in rural Australia
2008 - They really do go



