Introduction
Adolescent pregnancies are a major public health problem in low- and middle-income countries, causing many poor health outcomes such as maternal mortality and health issues for infants1,2. According to WHO data, approximately 21 million women between the ages of 15 and 19 years, and an estimated 1.5 per 1000 girls between 10 and 14 years, are known to conceive in developing countries every year2,3. Eleven percent of all births worldwide are births between the ages of 15 and 19 years3,4. In Turkey, due to the country’s cultural structure, social norms and a number of traditions, marriage of children, and adolescent pregnancies, continue to be widely seen in some regions5. For example, the rate of those starting to have children in their adolescence is 2% in western Turkey, whereas it is 7% in southern Turkey6.
Adolescent pregnancy can lead to many physical problems such as premature birth, cephalopelvic mismatch, fetal distress, bleeding, pre-eclampsia, urinary tract infection, fetal anomaly and presentation anomaly7. Adolescent pregnancy can also lead to substance abuse, and cause mental health problems such as anxiety, depression and post-traumatic stress disorder8. The pregnancy period is associated with various changes such as biological and physical appearance changes, and psychological disorders, and it is known that such changes have a particular effect on the behavior, attitude and decision-making processes of adolescents9. Insufficient social support causes anxiety in pregnant women10. Hartman et al (2020) pointed out that stress, anxiety and depression are highly correlated with pregnancy in adolescents11.
It has been noted that adolescent mothers experience significantly higher rates of depression both before and after birth than adult mothers and their non-pregnant peers8,11. Among adolescent mothers, the prevalence of depression is estimated to be between 16% and 44%. In contrast, the lifetime prevalence of major depression among non-pregnant adolescents is between 5% and 20%, while estimates of the lifetime risk of depression among adult pregnant women range from 6% to 17%8. In their study with adolescents, Osok et al (2018) reported that 32.5% of the adolescents clinically reported symptoms of depression, and 15.9% of the sample also had severe depressive characteristics12. As a result of many studies evaluating psychosocial risk factors for perinatal depression, it has been shown that lack of social support in both pregnancy and postpartum periods often causes perinatal depression12,13.
Social support has the potential to play a protective role by buffering the effects of stress in life on a woman's emotional wellbeing during pregnancy14. Studies investigating the relationship between the psychological state of pregnant women and perceived social support have shown that anxiety, depression and stress factors decrease as pregnant women's perceptions of social support increase10,15.
Early and effective interventions with psychosocial support are thought to provide better biopsychosocial results for the mother and the baby to empower pregnant adolescents against psychosocial risk factors and minimize the risk of developing anxiety, depression and many other mental disorders16. Peter at al (2017) found that social support seems to be a protective factor against anxiety disorders in pregnant adolescents, with a positive effect on mental health10. Abazarnejad et al (2019) reported a significant decrease in anxiety levels after therapeutic intervention sessions in the psychoeducation group17. Dysthe et al (2021) found that psychoeducation reduced symptoms of depression in adolescents18. Laurenzi et al (2020) carried out a meta-analysis study in which they synthesized randomized controlled trials on psychosocial interventions to prevent and improve mental health for pregnant adolescents and adolescent parents. They concluded that psychosocial interventions for pregnant adolescents and adolescent parents result in beneficial effects on adolescents' mental health19. Psychosocial treatment interventions are successful treatments for depressive symptoms in the pregnancy and postpartum period in pregnant adolescents.
The literature review conducted for this study revealed that the adolescent pregnancy rates in Turkey are still high, especially in some regions. The pregnancies are associated with marriage at an early age, socioeconomic status and education6,20,21. According to the Turkey Demographic and Health Survey (2019) data, approximately 4% of women and girls in the age group of 15–19 years in Turkey had their first birth in the previous 5 years, 3% had already had a live birth, and 1% were pregnant with their first child at the time when the survey was conducted. Among these individuals aged 15–19 years, 1% had been married before the age of 15 years, and 0.2% had given birth to a child before the age of 15 years. Although having children before the age of 17 years was generally rarely encountered, 10% of women aged 19 years either had become mothers or were pregnant with their first child6. According to the Turkey Demographic and Health Survey (2019) data, the rate of adolescents starting to have children decreased from 5% to 4% in the period since 2013. While these numbers suggest that the number of adolescent pregnancies is decreasing in Turkey, adolescents with children continue to experience significant problems. This is because adolescent mothers’ exposure to negative pregnancy outcomes or maternal mortality is more prevalent than for adult mothers6,20,21.
Although there are many studies on the rates, causes and obstetric outcomes of adolescent pregnancies in Turkey, only a limited number of studies have been found on mental problems associated with adolescent pregnancies. Knowing about problems affecting the mental health of pregnant adolescents and developing treatment plans are among the duties of the profession of psychiatric nursing.
The aim of this study was to determine the effects of psychosocial support-based (PSSB) psychoeducation given to Turkish pregnant adolescents in relation to their anxiety, depression and perceived social support levels. Accordingly, a PSSB psychoeducation program was provided for improving the mental health of pregnant adolescents and providing them with ways to make behavioral changes in a positive direction. It was thought that this program would make a positive contribution to the lives of pregnant adolescents, and contribute to the Turkish and international literature on psychiatric nursing.
Methods
This study was conducted using a pre-test–post-test with a randomized-controlled design.
Location and period of the study
This study was carried out in the obstetrics and gynecology outpatient clinic of a research and training hospital in Van province, Turkey, between January 2020 and December 2020. In determining the hospital where the study was conducted, the number of pregnant adolescents in the city was among the top 10 in the ranking throughout Turkey21. In the city of Van, where the study was conducted, there are only two hospitals. The fact that the number of pregnant adolescents in the hospital was higher than other hospitals and the ease of transportation to the city where the researcher lived played a role in the determination of this hospital.
Inclusion and exclusion criteria
Inclusion criteria for the study were:
- being an adolescent woman of age 15–19 years
- being in the third trimester of gestation (Anxiety and depression levels are higher in the third trimester.)22,23
- being open to communication and cooperation
- being able to read and write.
Exclusion criteria of the study were:
- having previously or already participated in any psychoeducational program
- being unwilling to participate in this study
- filling in the data collection tools incompletely.
Population and sample
The population of the study consisted of 750 pregnant adolescents presenting to the obstetrics and gynecology outpatient clinic of a state hospital in eastern Turkey. The study initially excluded 130 pregnant adolescents, including 75 pregnant adolescents who did not meet the inclusion criteria, and 55 whose contact information was missing or incorrect. Power analysis was conducted to determine the necessary sample size based on the remaining 620 pregnant adolescents as the population, with an error margin of 0.05, in a confidence interval of 0.95, at an effect size of 0.8 and population representation power of 0.80. The required sample size was determined as 100 pregnant adolescents (50 in the experimental group and 50 in the control group).
A total of 124 pregnant adolescents (experimental group n=62, control group n=62) were initially included in the study, considering that there might be losses during the study. Nine pregnant adolescents from the experimental group were excluded because they could not participate in the psychoeducation practice at different times, and three pregnant adolescents in the same group were excluded because they could not be reached during the post-test data collection process. Seven pregnant adolescents from the control group were excluded because they could not be reached during the post-test data collection process. The study was completed with a total of 105 pregnant adolescents (experimental group n=50, control group n=55).
According to the total number of participants required for the study, 124 envelopes were prepared, and one of the codes A or B was placed on each one based on a list of random blocks of two (sequential sampling method). A trained nurse who was not a researcher in this study was responsible for registering participants and assigning them to the two groups (single blind method). After each patient was admitted to the obstetrics and gynecology outpatient clinic, the participants were randomly assigned to group A (experimental) or B (control) according to the blocks of two prepared at the first stage. Recruitment of participants by randomization continued. CONSORT (Consolidated Standards of The sample selection process based on the Reporting Trials) criteria are given (Fig1).
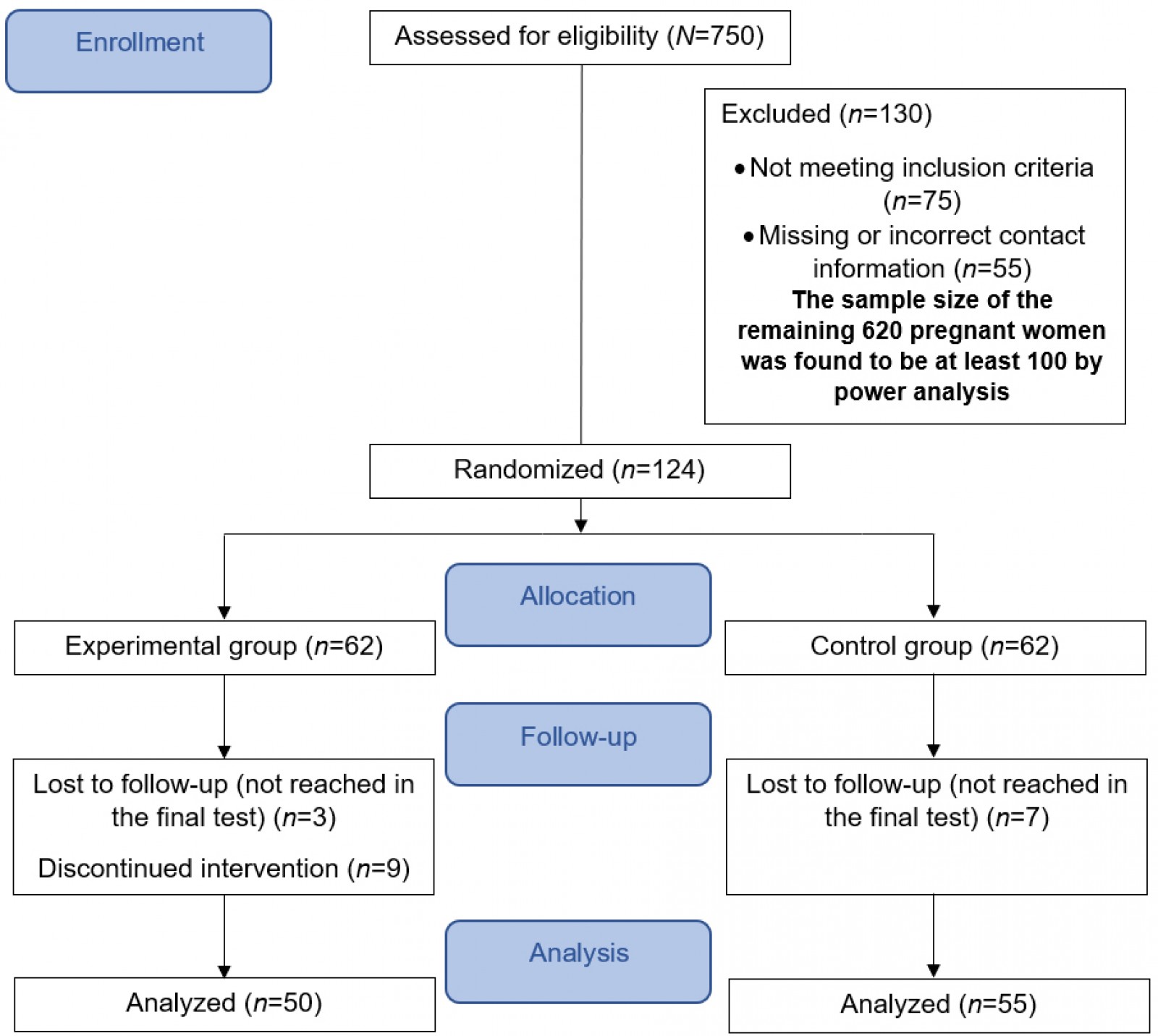 Figure 1: The CONSORT flow diagram for data collection.
Figure 1: The CONSORT flow diagram for data collection.
Data collection tools
The data were obtained using an introductory characteristics form, the Beck Anxiety Inventory (BAI), the Edinburgh Postpartum Depression Scale (EPDS) and the Revised Form of the Multidimensional Scale of Perceived Social Support (MSPSS).
Introductory characteristics form: This form, prepared by the researcher by reviewing the literature, consisted of 11 questions, relating to age, spouse’s age, education status, spouse’s education status, employment status, income level, family type, marital status, number of pregnancies, pregnancy planning and gestational week10,12.
Beck Anxiety Inventory: The BAI, developed by Beck et al (1988), evaluates an anxiety-provoking situation in the life of an individual, provides a scale of measurement for this situation and allows scoring24. The validity and reliability of the Turkish form of the inventory was tested by Ulusoy et al (1998)25. In the inventory, consisting of 21 items, each item contains four options scored from 0 to 3. The total possible score in the inventory ranges from 0 to 63. The Cronbach's alpha internal consistency coefficient of the scale was reported as 0.93. In this study, the Cronbach's alpha internal consistency coefficient of the scale was determined to be 0.92. Higher scores in the inventory indicate higher levels of anxiety symptoms. Scores in the inventory were previously classified as follows: <10 points as normal, 10–18 points as mild anxiety, 19–29 points as moderate anxiety, and 30–63 points as severe anxiety25.
Edinburgh Postpartum Depression Scale: This scale is used to determine risks in terms of depression in the pregnancy and postpartum periods, as well as measuring changes in levels and severity. The EPDS was developed by Cox et al (1987)26. The scale, which was shown to be valid and reliable in Turkish by Engindeniz et al (1997)27, determines the risk of depression in the postpartum period. It is a four-point, Likert-type self-assessment tool, and there are 10 items in the scale, scored between zero and three points. The scoring of each item is different; items 3, 5, 6, 7, 8, 9 and 10 show decreasing severity, and the scoring is in the form 3, 2, 1, 0. Items 1, 2 and 4 are scored in the form 0, 1, 2, 3. The total score of the scale is calculated by adding the scores of these items, and the lowest and highest possible scores in the scale are 0 and 30. The cut-off score of the scale was determined to be 12/13, and its Cronbach's alpha internal consistency coefficient was reported as 0.79. In this study, the Cronbach's alpha internal consistency coefficient of the scale was found to be 0.89. Those with a scale score of 13 or higher are considered to be at risk of depression27.
Revised Form of the Multidimensional Scale of Perceived Social Support: The MSPSS is a brief and easy-to-use scale used to subjectively measure the sufficiency of social support received from three different sources (family, friends and significant others). The scale, developed by Zimet et al (1988)28, was first adapted to Turkish by Eker and Arkar (1995)29. The second adaptation to Turkish was the validity and reliability study of MSPSS conducted by Çakir and Palabiyikoglu (1997) for young people between the ages of 12 and 22 years30. The factor structure, validity and reliability of the Revised Form of the MSPSS were reviewed by Eker et al (2001)31 and the internal consistency coefficients of MSPSS and its subscales were at an acceptable level (Cronbach’s alpha coefficients 0.80–0.95). In this study, the Cronbach's alpha internal consistency coefficient was found to be 0.90 in total, 0.82 for the ‘family’ dimension, 0.89 for the ‘friend’ dimension and 0.90 for the ‘significant other’ dimension. The scale consists of 12 items with three categories of social support from a significant other (items 1, 2, 5 and 10), family (items 3, 4, 8 and 11) and a friend (items 6, 7, 9 and 12). It is a seven-point Likert-type scale, and the total score of the scale is calculated by adding the scores of the four items in each subscale, then adding all subscale scores. The lowest and highest possible scores in each subscale are 4 and 28, respectively. For the entire scale, the lowest possible score is 12, and the highest is 84. A high score indicates a high level of perceived social support31.
Data collection process
The data were collected by the researcher using the face-to-face interview method in a room where private meetings could be held 2 days a week, on Mondays and Fridays, in the obstetrics and gynecology outpatient clinic of the Health Sciences University Research and Training Hospital in Van between January 2020 and June 2020. The introductory characteristics form, BAI, EPDS and MSPSS were applied in the control and experimental groups for the pre-test, and BAI, EPDS and MSPSS were applied for the post-test. The implementation of the data collection tools took approximately 15–20 minutes for each participant.
Nursing intervention
Psychosocial support covers the dynamic relationship between the psychological and social life aspects of the individual, the individual’s possession of a meaningful social role by these aspects affecting each other, and the components of feeling happy and hopeful, living in compliance with basic values defined by oneself in the environment to which one belongs, being in positive social relationships and in a supportive environment, overcoming difficulties and living by trusting and being protected32. The purpose of psychosocial support practices is to provide patients with the knowledge and skills necessary for them to cope with their disease, to help them achieve a state of wellbeing and functional adaptation and to increase their quality of life33.
The training applied by the researcher for the experimental group was carried out in the form of interactive training supported by the Psychosocial Support Based Psychoeducation booklet. In the first session, the pregnant adolescents in the experimental group were informed about the PSSB Psychoeducation program and the training days were determined. For pregnant adolescents who could come to the hospital, training was held on Mondays and Fridays in the training hall of the University of Health Sciences, Van Training and Research Hospital, Obstetrics and Gynecology Hospital. Home visits were made to the pregnant adolescents who could not come to the hospital, on the days and times suitable for the pregnant adolescents, and the research was given by the researcher as one-on-one training, twice a week for 4 weeks. Each session lasted approximately 45 minutes. The content for the eight sessions of the PSSB Psychoeducation program were prepared by the researcher in line with the literature32-34.
The pregnant adolescents were given a training booklet after the first session. No intervention was applied on the pregnant adolescents in the control group. During the psychoeducation program, the pregnant adolescents continued their routine treatments and follow-ups.
Session 1: The main purpose of this session was to inform the participants about the psychoeducation program and to get to know the participants. For this purpose, the educator and the participants introduced themselves. The content of PSSB psychoeducation and the importance of regular participation in the education program were mentioned. The training days, hours and group rules were determined with the participants who wanted to participate. The participants' experiences and expectations were shared. The research made a preliminary assessment to identify participants’ needs and problems.
Session 2 – Psychological support: The dynamics between the psychological and social life aspects of pregnant adolescents were emphasized, and psychosocial problems and social support sources were determined. It was aimed to fill these gaps in the form of brainstorming by having participants express their emotional needs and focusing on relevant problems. It was aimed to increase their level of knowledge about psychosocial problems and minimize psychosocial stress by providing them with information about methods to increase social support from spouses, family and friends.
Session 3 – Social and emotional learning: This topic is an important component of psychosocial support, and in this session information was given on emotions, thoughts and behaviors, and methods of recognizing and managing emotions, developing and maintaining positive relationships, making responsible decisions and strengthening interpersonal relations. Methods involving behavioral approaches for change or the elimination of psychosocial risk factors were described. At the end of this session, it was aimed to increase the participants’ levels of emotional wellbeing by improving their self-awareness, emotional awareness and management, cognitive flexibility, empathy, social skills and relationship-building skills through social and emotional learning.
Session 4 – Endurance and coping: This session aimed to help participants use appropriate coping methods, as well as enabling them to develop new coping methods. The participants were encouraged to reinforce existing positive coping methods and use new methods that are specific and appropriate to the individual, the situation and the culture. Coping mechanisms such as problem-solving, support-seeking, motivation, optimism, belief, decision-making and implementation, conflict management and other life skills were explained to the participants. The provision of these skills was done using culturally appropriate contexts.
Session 5 – Psychosocial stressors: The main purpose of this session was to introduce the concepts of stress, anxiety and depression to the participants and teach them coping skills. The aim of increasing their levels of knowledge on how to deal with psychosocial stressors was achieved. The pregnant adolescents were informed about appropriate psychosocial interventions for anxiety, depression and behavioral risk factors. In this session, the participants were informed about the effects and meanings of symptoms, ways of coping with daily activities, changing behavioral risk factors (such as smoking, alcohol, exercise, weight-related problems), improving relationships and communication with other individuals, reducing arousal and stress responses, and planning better for the future.
Session 6 – Positive perceptions of parenting: The main goal in this session was to create a positive perception of parenting. The aim was to determine each participant's perception of parenting and have them share their concerns about future parenting skills. It was aimed to address these concerns with the experiences of the group members. Parenting roles and coping skills were discussed.
Session 7 – Family member participation: In line with pregnant adolescents’ needs in relation to psychosocial support, the necessary focus training was given and the importance of social support and cooperation was explained to the spouses, families and friends of the pregnant adolescents identified as sources of social support in the program.
Session 8 – Process evaluation and closing remarks: In this final session, the aim was to evaluate the effectiveness of the program and to reinforce what was learned. The participants were asked to evaluate themselves and the psychoeducation program. Criticisms and recommendations about the process were listened to by the researcher.
Data analysis
SPSS v24.0 (IBM; https://ibm-spss-statistics.software.informer.com/24.0) was used to analyze the data, and p-values of less than 0.05 were accepted as statistically significant. The conformity of the data to normal distribution was examined with histograms, P–P plots, Q–Q plots, as well as Shapiro–Wilk and Kolmogorov–Smirnov tests. Percentage distribution, arithmetic mean, standard deviation and the χ2 test were used to analyze the introductory characteristics for the data that showed normal distribution as a result of the analyses. The independent-samples t-test was used for the comparison of the mean scale scores in the experimental and control groups, whereas the paired-samples t-test was used for the intragroup comparisons of the pre-test and post-test total scale scores in the experimental and control groups.
Ethics approval
In order to conduct the study, approval from the Scientific Research and Publication Ethics Board of Inonu University (approval number 2019/136) and legal permissions from the Van Health Sciences Institute were obtained (approval number:36866945-514.10). The principles of the Declaration of Helsinki, including the right to participate in the research process freely, no harm or loss to participants, maintaining the right to withdraw from the study, and confidentiality of information, were observed in this study. Before starting the study, the objective of the research process was explained to the pregnant adolescents who were included, and their relatives, and the questions of the participants were answered. It was stated to the pregnant adolescents that the information they provided would be kept confidential, it would not be used anywhere else, and they had the right to leave the study at any time. The verbal and written consent of the participants was obtained. After the post-test data collection process was completed, the PSSB Psychoeducation program was provided to those in the control group who wanted to participate, and the training booklet was distributed to them.
Results
Descriptive statistics
According to the data collected on the introductory characteristics of the pregnant adolescents in the control and experimental groups, 42% of the pregnant adolescents in the experimental group were primary school graduates, and 40% of their spouses were secondary school graduates. All pregnant adolescents (100%) in the experimental group were home-makers, 88% had less income than their expenses, 76% lived in an extended family, 96% had a civil marriage, 74% were having their first pregnancy and 60% were having a planned pregnancy.
The mean age of the pregnant adolescents in the experimental group was 18.36±0.77 years, the mean age of their spouses was 25.14±3.20 years, and the mean week of their pregnancy was week 32.54±2.37.
It was determined that 34.5% of the pregnant adolescents in the control group had graduated from primary school, and 50.09% of their spouses had graduated from secondary school. A total of 96.4% of the pregnant adolescents in the control group were home-makers, 81.8% had less income than expenses, 83.6% lived in an extended family, 89.1% had a civil marriage, 80% had their first pregnancy and 61.8% had a planned pregnancy. The mean age of the pregnant adolescents in the control group was 18.18±0.94 years, the mean age of their spouses was 25.21±2.86 years, and the mean week of their pregnancy was week 32.38±2.13. There was no statistically significant difference between the two groups in terms of the control variables, and the groups were homogeneous (p>0.05, Table 1).
Table 1: Descriptive statistics of experimental and control groups (n=105)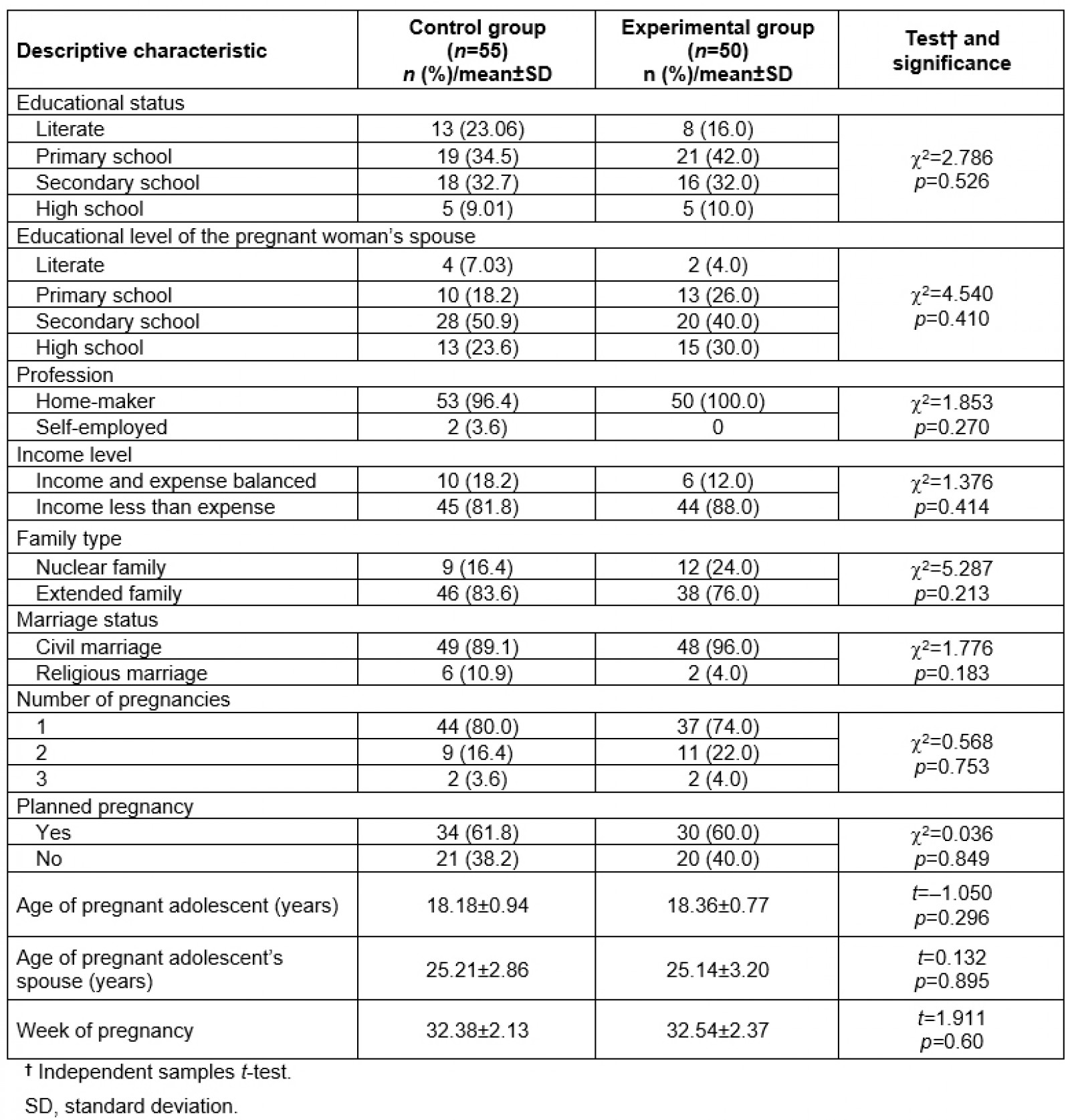
Comparison of pre-test BAI, EPDS and MSPSS
According to the analysis results on the pre-test scale scores of the pregnant adolescents in the experimental and control groups, the mean BAI score was 47.30±12.44 (severe anxiety) in the experimental group and 46.18±8.76 (severe anxiety) in the control group, the mean EPDS score was 15.01±3.63 (risk of depression) in the experimental group and 15.92±3.06 (risk of depression) in the control group, and the mean MSPSS score was 50.70±15.78 in the experimental group and 48.41±14.42 in the control group. The differences between the pre-test mean total BAI, EPDS and MSPSS scores of the two groups were not statistically significant (p>0.05, Table 2). The pre-test BAI, EPDS and MSPSS scores of the experimental and control groups were similar.
Table 2: Comparison of pre-test BAI, EPDS and MSPSS dimension and total mean scores for pregnant adolescents in experimental and control groups (n=105)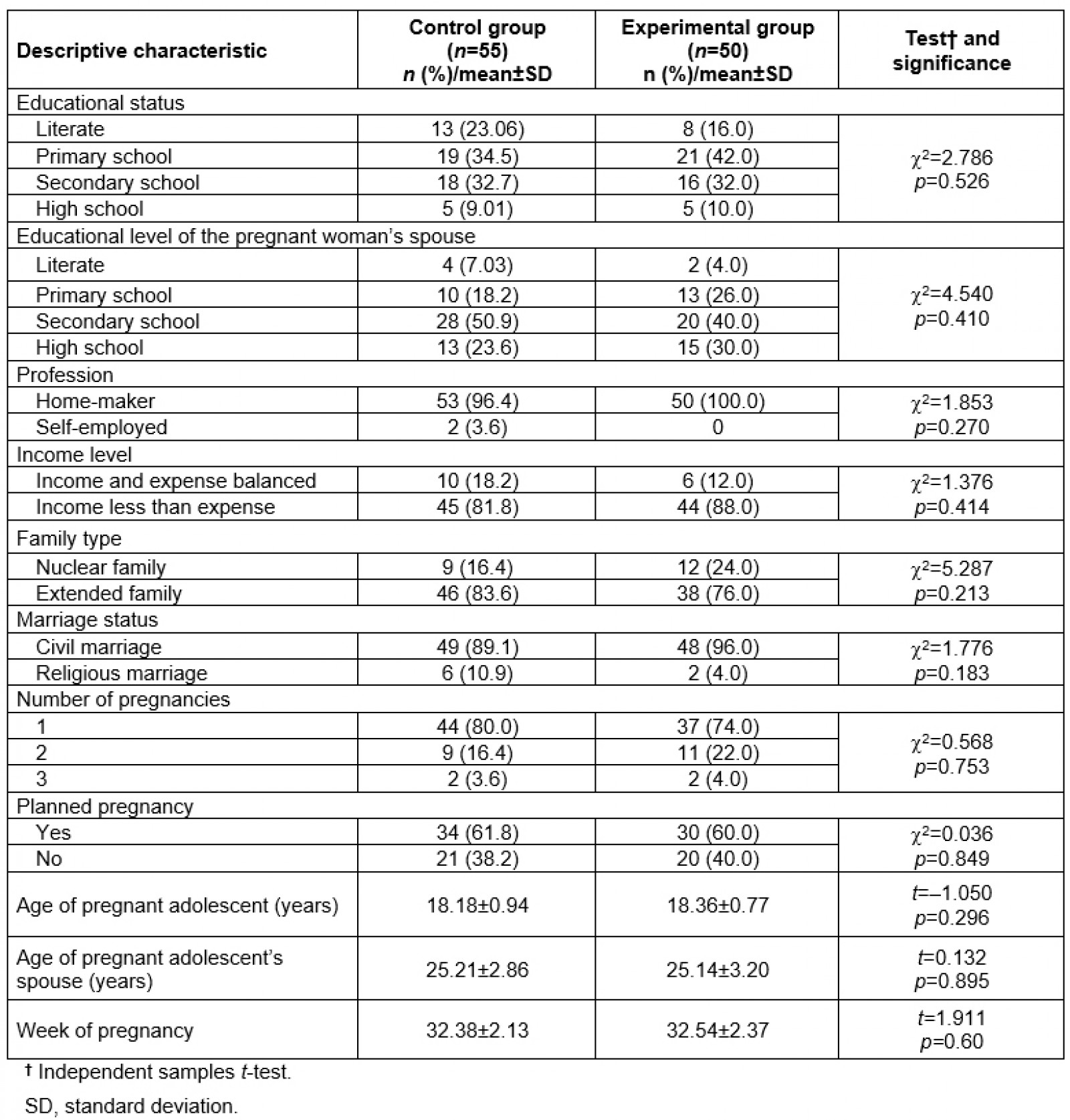
Comparison of the post-test BAI, EPDS and MSPSS
According to the analysis results on the post-test scale scores of the pregnant adolescents in the experimental and control groups, the mean BAI score was 30.52±6.46 in the experimental group and 48.13±14.16 in the control group, the mean EPDS score was 13.01±3.84 in the experimental group and 16.34±2.73 in the control group, and the mean MSPSS score was 59±16.06 in the experimental group and 50.41±11.86 in the control group. The differences between the post-test total BAI, EPDS and MSPSS scores of the two groups were statistically significant (p<0.05, Table 3). The mean post-test BAI and EPDS scores of the pregnant adolescents in the experimental group were significantly lower in comparison to those in the control group, while the mean post-test MSPSS score of the experimental group was significantly higher in comparison to that in the control group.
Table 3: Comparison of post-test BAI, EPDS and MSPSS dimension and total mean scores for pregnant adolescents in experimental and control groups (n=105)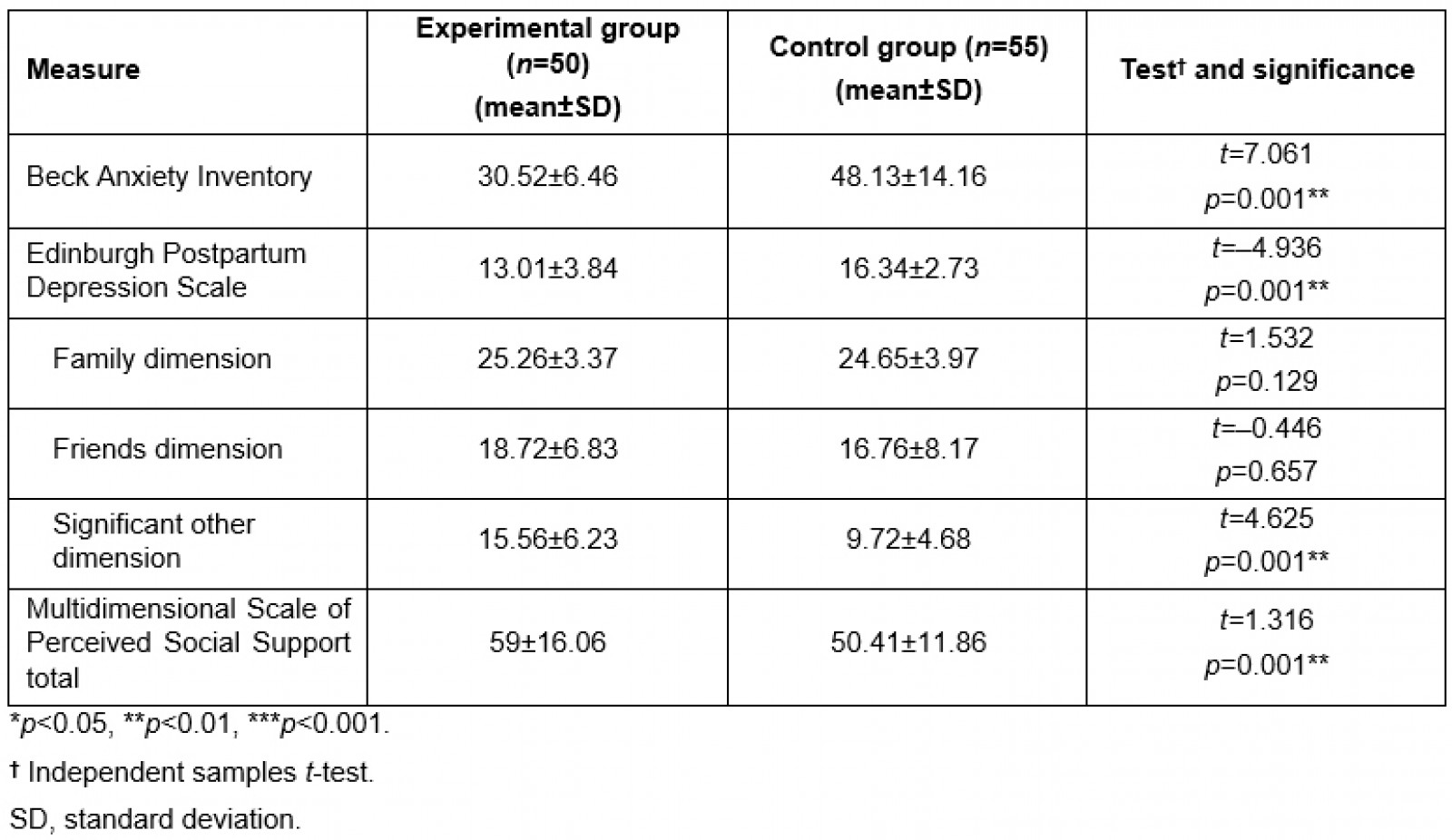
Intragroup comparisons of pre-test and post-test BAI, EPDS and MSPSS
In the intragroup comparisons of the pre-test and post-test scores of the pregnant adolescents in the experimental and control groups, the respective mean pre-test and post-test BAI scores of the experimental group were 47.30±12.44 and 30.52±6.46, and the respective mean pre-test and post-test BAI scores of the control group were 46.18±8.76 and 48.13±14.16. Moreover, the respective mean pre-test and post-test EPDS scores of the experimental group were 15.01±3.63 and 13.01±3.84, while the respective mean pre-test and post-test EPDS scores of the control group were 15.92±3.06 and 16.34±2.73. Accordingly, it was determined that there was a significant difference between the pre-test and post-test BAI and EPDS scores of the experimental group (p<0.05, Table 4), whereas there was no significant difference between the pre-test and post-test BAI or EPDS scores of the control group (p>0.05, Table 4). The mean total post-test BAI and EPDS scores of the pregnant adolescents in the experimental group were significantly lower than their pre-test scores. The respective mean total pre-test and post-test MSPSS scores of the experimental group were 50.70±15.78 and 59.00±16.06, while the respective mean total pre-test and post-test MSPSS scores of the control group were 48.41±14.42 and 50.41±11.86. The differences between the pre-test and post-test scores of both groups were determined to be statistically significant (p<0.05, Table 4). There was a sharp increase in the mean total post-test MSPSS score of the pregnant adolescents in the experimental group compared to the pre-test score.
Table 4: Intragroup comparisons of pre-test and post-test BAI, EPDS and MSPSS dimension and total mean scores for pregnant adolescents in experimental and control groups (n=105)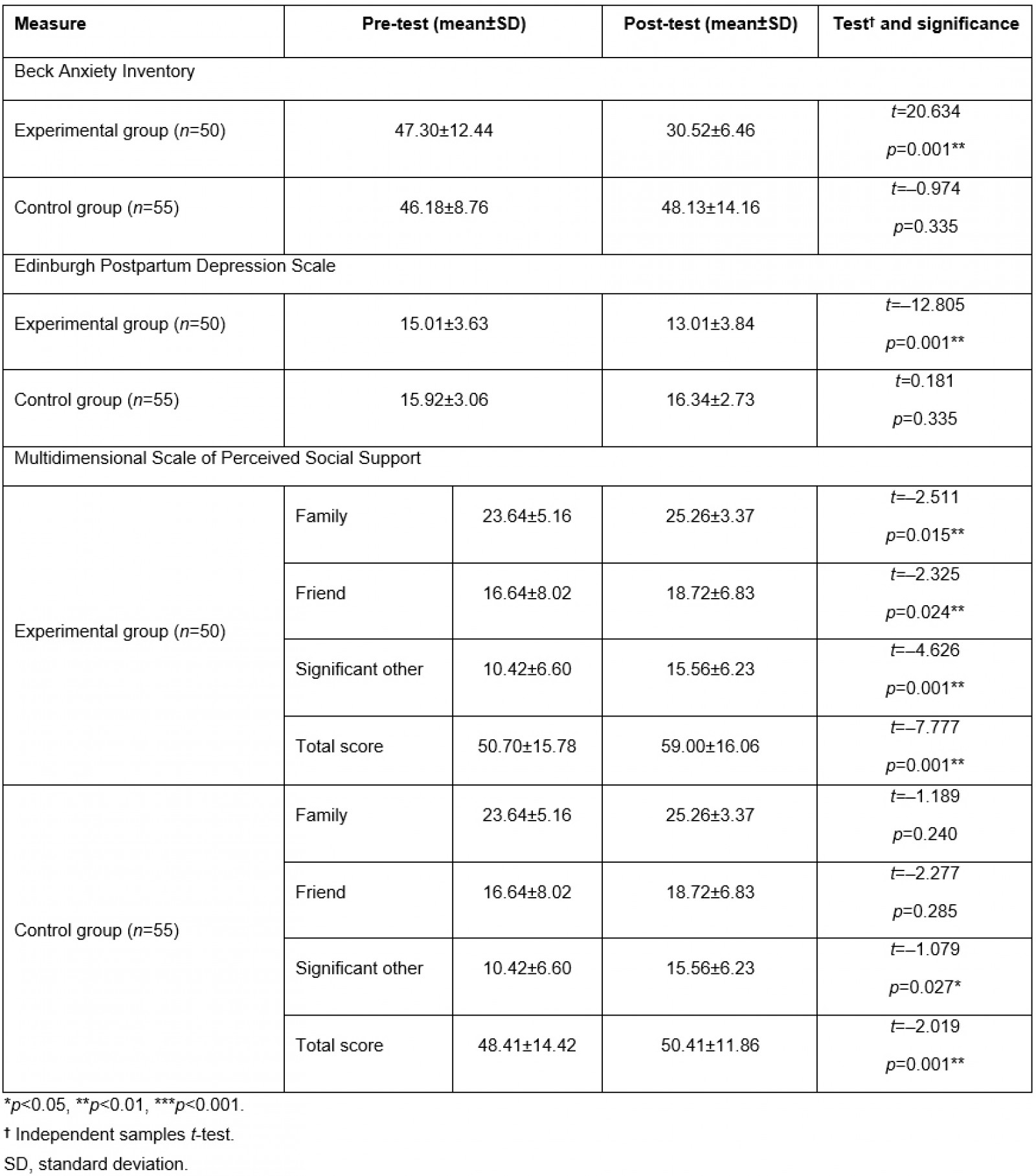
Discussion
In this study, the effect of PSSB psychoeducation on anxiety, depression and perceived social support in pregnant adolescents was examined, and the results are discussed in this section with the relevant literature.
Findings related to anxiety
After the psychoeducation program, the anxiety level of the pregnant adolescents in the experimental group was significantly lower than that in the control group (p<0.05). This decrease in the anxiety level in the experimental group after PSSB psychoeducation confirmed the hypothesis that PSSB psychoeducation given to pregnant adolescents reduces their level of anxiety.
It was observed that the mean post-test total anxiety score of the pregnant adolescents in the control group increased slightly in comparison to their mean pre-test total score. This situation may have been caused by the fact that the pregnant adolescents who were included in this study were in the third trimester of their pregnancy, and their anxiety levels may have increased as they approached labor.
In a study they conducted with pregnant women, Abazarnejad et al (2019) reported a significant decrease in anxiety levels after therapeutic intervention sessions in the psychoeducation group17. Fenwick et al (2015) conducted a study with pregnant women and stated that, after a midwife-led prenatal psychoeducation intervention for prenatal fear, birth fears experienced by the women decreased significantly34. The results of these previous studies support the results of this study.
The psychoeducation program that was provided to the participants of this study may have been positively effective because it provided detailed information on topics such as ways of coping with daily activities, changing behavioral risk factors (eg smoking, alcohol consumption, exercise, weight-related problems), improving relationships and communication with other individuals, reducing arousal and stress responses, increasing one’s level of thinking about the future, planning and imagining.
Findings related to depression
After the psychoeducation program, the depression level of the pregnant adolescents in the experimental group was significantly lower than that of those in the control group (p<0.05). This decrease in the depression levels in the experimental group after PSSB psychoeducation confirmed the hypothesis that PSSB psychoeducation given to pregnant adolescents decreases their level of depression.
A slight increase was observed in the mean total post-test depression score of the pregnant adolescents in the control group in comparison to their pre-test score. The reason for this situation is considered to be the fact that the pregnant adolescents were in their third trimester, and their depression levels may have increased as they approached labor.
Thomas and Looney (2004) observed an improvement in pregnant adolescents and adolescent parents in terms of risk, depression, self-esteem and parenting attitudes/beliefs after a comprehensive psychoeducational intervention35. In studies investigating the relationship between the psychological state of pregnant women and their perceived social support, it has been found that, as the social support perception of pregnant women increased, their anxiety, depression and stress factors decreased10,15. Laurenzi et al (2020) carried out a meta-analysis study in which they synthesized randomized controlled trials on psychosocial interventions to prevent and improve mental health for pregnant adolescents and adolescent parents. The researchers found that psychosocial interventions for pregnant adolescents and adolescent parents result in beneficial effects on adolescents’ positive mental health and school attendance19.
In the content of the presented psychoeducation program, providing detailed information on topics such as self-awareness, emotional awareness and management, cognitive flexibility, empathy, increasing the level of emotional wellbeing by improving social skills and relationship skills may have enabled the intervention to be positively effective.
Findings related to perceived social support
After the psychoeducation program, the perceived social support level of the pregnant adolescents in the experimental group was significantly higher than that in the control group (p<0.05). This increase in the level of perceived social support in the experimental group after PSSB psychoeducation confirmed the hypothesis that PSSB psychoeducation given to pregnant adolescents increases their level of perceived social support.
Abazarnejad et al (2019) reported a significant decrease in anxiety levels after therapeutic intervention sessions in the psychoeducation group of pregnant women17. Fenwick et al (2015) reported that birth fears experienced by the women decreased significantly after a midwife-led prenatal psychoeducation intervention for prenatal fear34. Thomas and Looney (2004) observed an improvement in pregnant adolescents and adolescent parents in terms of risk, depression, self-esteem and parenting attitudes/beliefs after a comprehensive psychoeducational intervention35. Laurenzi et al (2020) carried out a meta-analysis study in which they synthesized randomized controlled trials on psychosocial interventions to prevent and improve mental health for pregnant adolescents and adolescent parents and concluded that psychosocial interventions for pregnant adolescents and adolescent parents result in beneficial effects on the adolescents' positive mental health and school attendance19. The results of previous studies support the results of this study.
In the content of the presented psychoeducation program, with the family member participation session, the positive effect of the intervention may have been promoted by ensuring the participation of the spouses, families and friends of the pregnant women who were identified as sources of social support. This session about issues where pregnant adolescents are deprived of psychosocial support may also have enabled the intervention to be positively effective by providing the necessary focus training and establishing social support and cooperation.
Study limitations
Due to the COVID-19 pandemic, which started during the data collection process, a curfew was initiated in Turkey to prevent the spread of the virus. During this period, the training implementation plan of the experimental group had to be suspended in April and May. With the start of the normalization process as of June 2020, training was given to the experimental group. The disruption of the continuity of the intervention due to the interruption of the research process during the pandemic period and the fact that the research was carried out in a single center constituted the limitations of the study. Additionally, the sociocultural factors of the region where this study was conducted and the fact that the pregnant adolescents were living in rural areas led to difficulties in these adolescents’ participation in the psychoeducation program. The strength of this research was giving training to pregnant adolescents, a group from which it is difficult to collect data. Another of the limitations was the low sample size.
Some practices of adolescent pregnant women such as working in harmony with the researcher, fulfilling their homework and regularly participating in trainings have increased the motivation of the researcher, and these have contributed to obtaining more reliable results from the analyses.
Conclusion
In the study, the anxiety and depression levels of the pregnant adolescents in the control and experimental groups before the PSSB psychoeducation program were high, and their perceived social support levels were average. The anxiety and depression levels in the experimental group decreased significantly in comparison to the control group after the PSSB psychoeducation program, whereas their level of perceived social support was significantly higher than that of the control group in the post-test. In the intragroup comparison after the psychoeducation program was provided, the anxiety and depression levels of the pregnant adolescents in the experimental group decreased in the post-test compared to the pre-test, and their perceived social support level increased in the post-test compared to the pre-test. In the intragroup comparison of the scores of the pregnant adolescents in the control group, there was a slight increase in their post-test anxiety and depression levels compared to the pre-test, whereas there was no change in their perceived social support level. Hence, the PSSB psychoeducation program was effective in reducing the anxiety and depression levels of the Turkish pregnant adolescents and increasing their perceived social support levels.
Based on the results, the following recommendations are made:
- Employ mental health screening programs in addition to routine follow-ups of pregnant adolescents in obstetrics clinics.
- Take an active role in planning and implementing psychosocial interventions for pregnant adolescents, developing culture-specific interventions.
- Conduct studies to shed light on the effectiveness of different types of interventions to contribute to the mental health of pregnant adolescents.
- Increase the awareness of the family and society towards changing the existing perspectives on adolescent marriages and pregnancies.
- Adopt culturally compatible psychosocial models, and take into account that adolescent pregnancies are generally due to sociocultural reasons.
Acknowledgements
We would like to thank all participants for their participation and the staff in the hospital for helping with the recruitment process for this study. All data in this study are based on a doctoral dissertation prepared by the first author.


