Introduction
Compared to their urban counterparts, residents of rural areas present more often with multiple vulnerability factors, such as lower income and less formal education, and are less likely to exhibit healthy lifestyle behaviors. They also have higher rates of overall mortality, injury and poisoning, and chronic diseases such as cardiovascular disease and diabetes1. Rural populations also experience more challenges in accessing primary health care (PHC) services than urban populations, partly because of travel distances but also because there are fewer health care professionals (including family physicians) in rural areas than in urban areas1. They also face low retention rates of healthcare professionals and a lack of onsite specialists and other resources2.
PHC increasingly depends on the contributions of multiple professionals3. However, health providers in PHC face enormous ideological, organizational, structural and relational challenges4, and the presence of different types of professionals in PHC teams alone is not sufficient to improve access5. The fact that different health professionals work together in a PHC setting does not automatically mean that interprofessional collaboration (IPC) exists. It is therefore essential to create supportive environments for IPC and to encourage IPC behaviors in different environments6.
IPC is a process that occurs when at least two professionals with different areas of expertise share common goals that reflect the values of individuals and families, use effective and regular communication mechanisms, actively participate in the delivery of quality care and encourage shared decision-making to maximize healthcare delivery and individual outcomes7. IPC is an essential element of healthcare organization to enhance access to health care and to improve the health status of a population8, especially for those with complex and chronic conditions9. IPC and effective interprofessional teamwork are critical components of safe healthcare provision, as they can contribute to improved clinical performance and patient outcomes10-12. Fostering IPC among health professionals working in rural and remote health centers can help overcome some of the unique challenges of PHC in these settings, thereby enhancing access to PHC and improving the health status of the populations living there.
Several scholars have undertaken reviews of interventions or initiatives to improve IPC among health professionals in different settings, including PHC facilities13-15, but no reviews have been conducted on interventions or initiatives in rural or remote PHC facilities. Considering the importance of optimal IPC in rural and remote PHC services16, there is a need to identify initiatives to improve IPC in these healthcare facilities and the factors that either enhance or limit the implementation of these initiatives.
The main objective of this project was to map initiatives described in the scientific literature that were implemented to promote IPC in PHC facilities located in rural and remote areas. The secondary objective was to identify barriers and facilitators to the implementation of these initiatives. Two types of initiatives were researched: interprofessional education (IPE) and interprofessional practice (IPP) initiatives, as these have been identified in health care as playing an important role in improving healthcare services and patient outcomes17. As defined by Reeves et al, IPE initiatives occur when two or more professions learn interactively, whereas IPP initiatives are activities or procedures incorporated into regular practice18. Both are designed to improve IPC and the quality of care provided18.
Methods
A scoping review is a method of uncovering key concepts, types of evidence and gaps in the research of a specific field through the lens of an exploratory research question, and the subsequent systematic process of searching the literature, selecting relevant results and synthesizing existing evidence19. The framework developed by Arksey and O’Malley was used to organize this scoping review20. Five of the six steps proposed by these authors were carried out: identification of research questions, identification of relevant articles, selection of articles, data extraction and analysis, and presentation of results20.
A concept map and search strategy were developed, as detailed in Table 1, employing terms for each of the following three concepts: interprofessional collaboration, primary care, and rural or remote areas. The search strategy was validated by a health sciences librarian. The literature review was conducted in 2019 and updated in 2021 and 2022. Only articles published between 1999 and 2021 were considered. The databases consulted included Abstracts in Social Gerontology, Academic Search Complete, AMED, CINAHL, MEDLINE, SocINDEX and PsychINFO, and the search yielded 3085 articles after the removal of duplicates.
As detailed in Figure 1, these articles were screened using the following inclusion criteria: (1) the study explored characteristics, facilitators and/or barriers of collaborative practice or an initiative; (2) the initiative took place in a rural or remote area; and (3) PHC facilities were involved. In terms of exclusion criteria, literature reviews, commentaries, and theoretical or reflection articles were excluded. After the screening of titles and abstracts by two reviewers (KP and DAB), the full text of the 94 retained articles was subsequently screened using the same criteria, resulting in 23 articles, which were then analyzed using a directed content analysis approach21. NVivo v12 (QSR International; http://www), a qualitative data analysis software, was used in the data extraction process to ensure greater rigor22. Co-coding was performed by three reviewers (DP, KP and DAB) and discussed as a group. The coding process followed the interprofessional framework developed by Reeves et al18, which defines the three main categories of interprofessional interventions (IPE, IPP and interprofessional organization) and specifies the types of interventions, objectives and outcomes for each category18.
Table 1: Concepts and related keywords for document search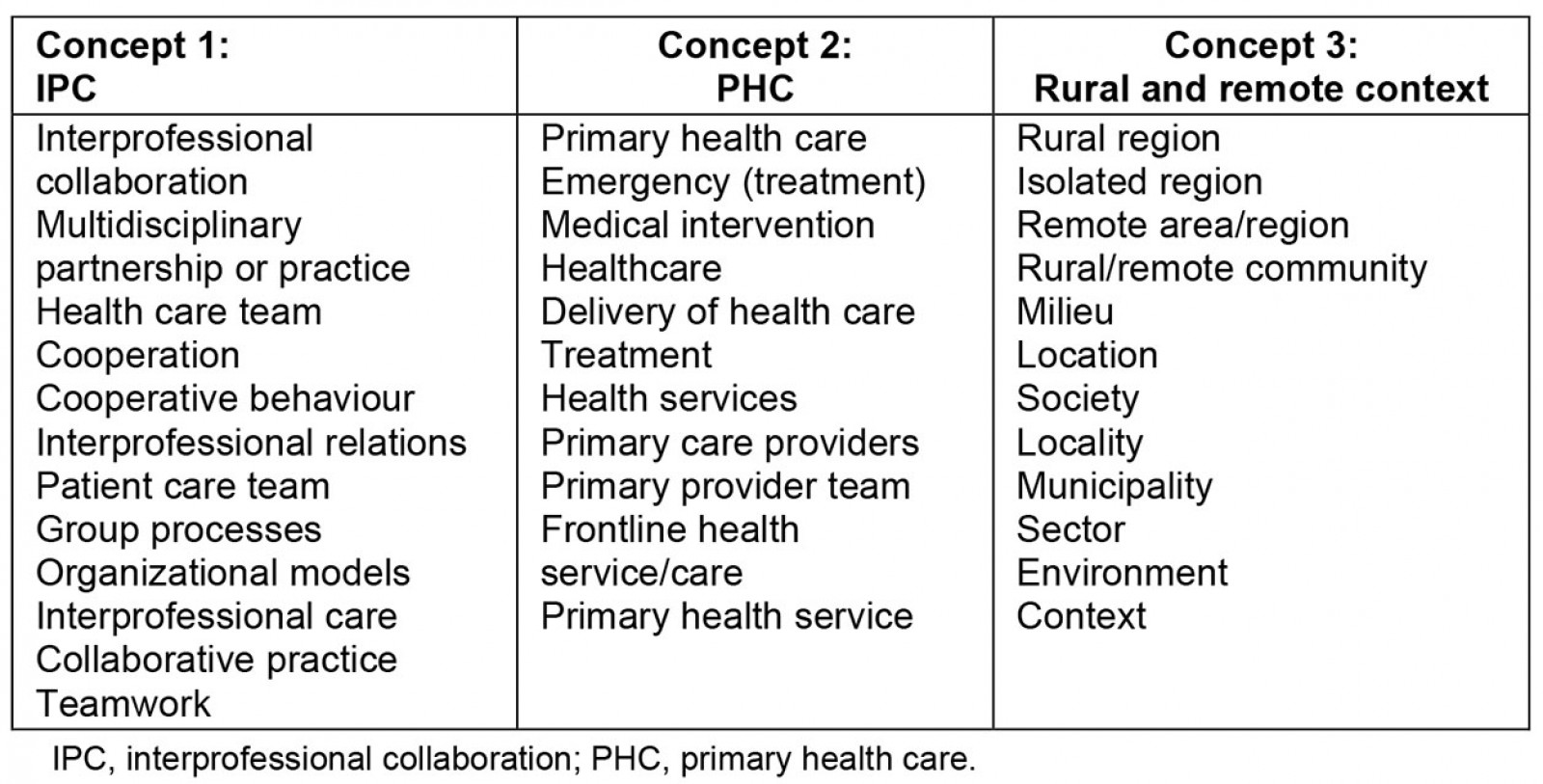
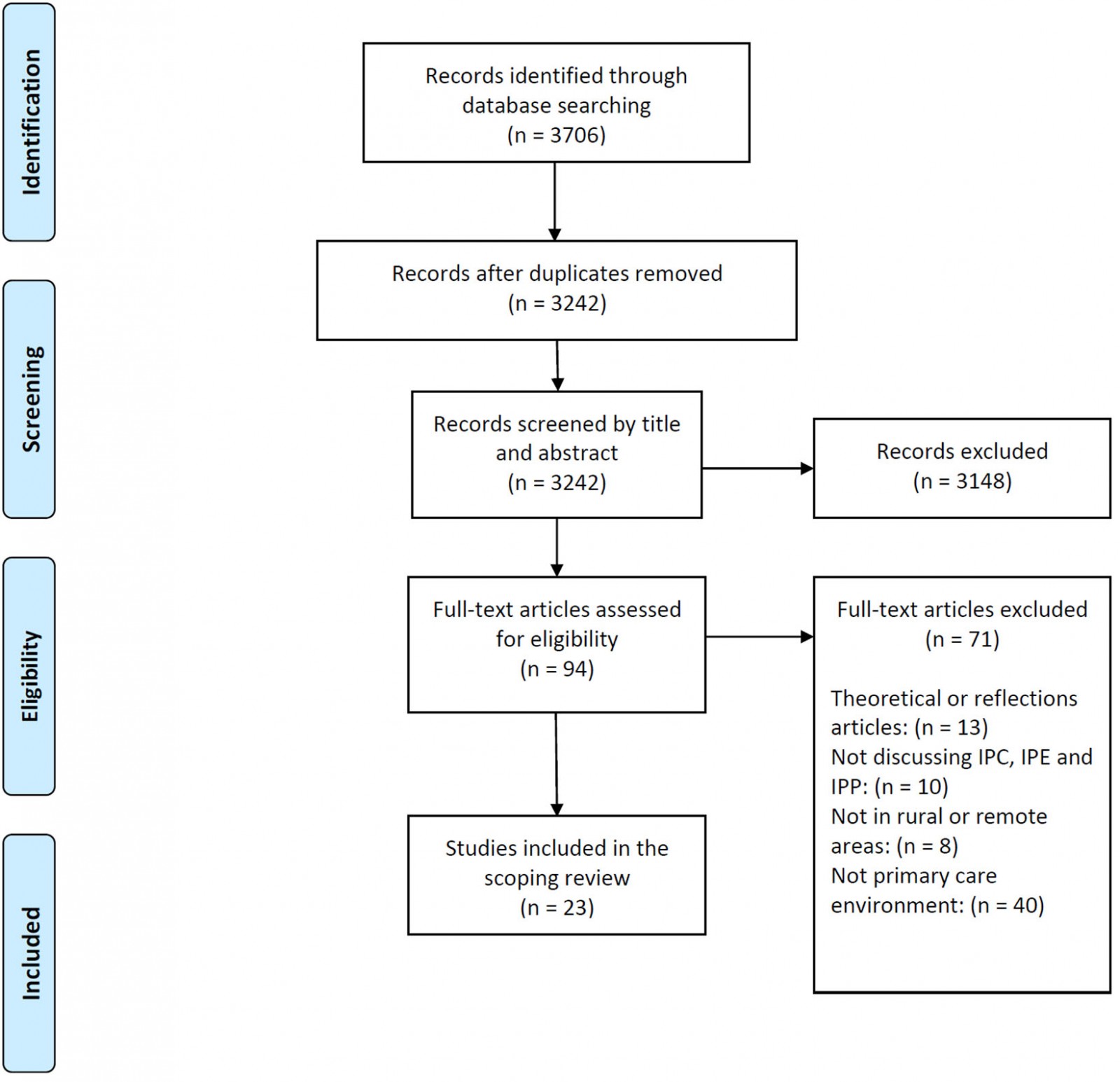 Figure 1: PRISMA flow diagram.
Figure 1: PRISMA flow diagram.
Results
Of the 23 selected articles, only 10 focused on the implementation of IPE and IPP initiatives to improve IPC in PHC facilities located in rural and remote areas, whereas 13 articles reported barriers and facilitators to the implementation of initiatives to improve IPC in existing contexts. IPE was discussed in five articles23-27, IPP was discussed in three articles28-30, and two studies discussed both IPE and IPP31,32. Only one of the 10 initiatives identified was implemented in a remote PHC facility28, whereas the others were implemented in rural PHC facilities.
Interprofessional education and interprofessional practice initiatives
Details of the IPE and IPP initiatives identified in rural and remote PHC facilities are shown in Table 2. The most common IPE initiatives were workshops, courses (in-person or video-conference), discussion groups and simulations, while IPP initiatives fell into two main categories: clinical (manual, inventory, protocol, care model) or technological tools (video-conferencing system). For two initiatives24,32, IPE activities were inspired by Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), a validated training curriculum for teaching interprofessional communication to healthcare professionals33. Initiatives were implemented in a variety of practice locations (PHC services, emergency, mental health, palliative care and home care), and the vast majority of professionals involved were physicians and nurses. The key IPC-related outcomes of IPE and IPP initiatives were clarification of professional roles, improved teamwork and improved IPC.
Table 2: Summary of articles describing interprofessional education and interprofessional practice initiatives implemented to improve interprofessional collaboration23-32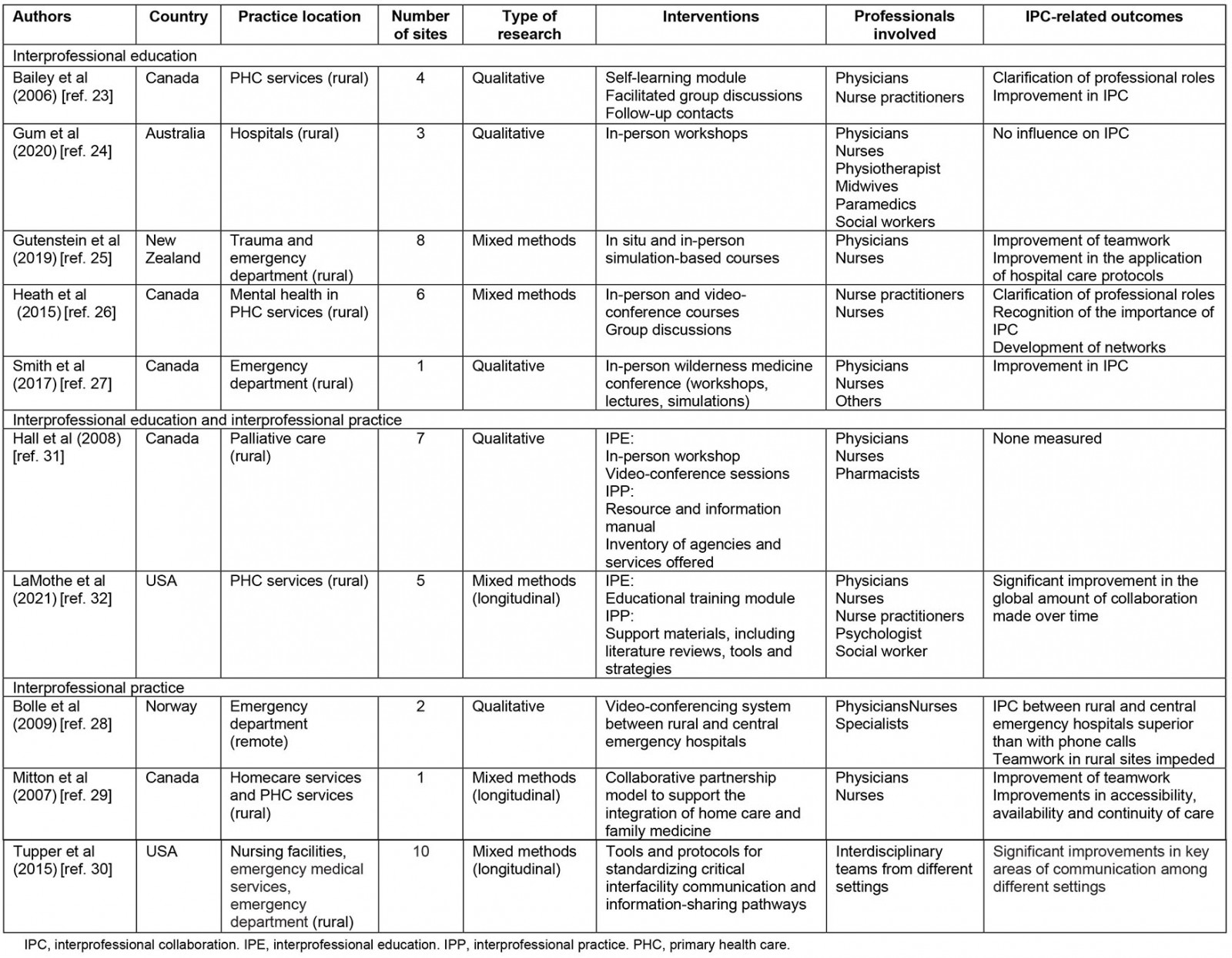
Barriers and facilitators to the implementation of initiatives to improve interprofessional collaboration in rural and remote areas
Common themes that emerged from the articles were grouped as either barriers or facilitators to the implementation of initiatives to improve IPC.
Barriers: Four barriers related to initiatives to improve IPC specifically in rural and remote areas were identified.
Human resources Insufficient human resources emerged as a major barrier to the implementation of initiatives to improve IPC in rural and remote areas32,34-39. Some authors spoke in particular of the availability of too few professionals to cover vast geographical areas, resulting in less collaboration simply because there were fewer professionals to share information with34,35,38. Others spoke of work overload for rural health professionals, which hindered their engagement in initiatives to improve IPC34,35,37,40. Because teams in rural PHC facilities are usually small, losing one team member can greatly impact the performance of other team members32. Other barriers related to human resources included recruitment34 and retention of health professionals in rural and remote areas34,38 as well as the presence of transient teams24, which prevented the building of solid relationships necessary for IPC24,38.
Understanding of roles Family physicians frequently lacked an understanding of the basic knowledge and skills of nurse practitioners23 and midwives41, leading to confusion and concerns surrounding who was responsible for which aspects of patient care. In rural areas where surgical or specialist services were not locally available, insufficient understanding of the scope of practice and competencies of each professional meant physicians tended to demonstrate a lack of trust toward other professions and, therefore, were less open to sharing responsibilities35,41. Siloed practice among health professionals working in some rural clinical facilities also contributed to the lack of understanding of the roles of other health professionals24. Non-resident medical professionals who gave orders to those who were familiar with the local community were seen as acting inappropriately, and relationship building was hindered when individuals felt that their professional contribution was criticized and not fully acknowledged42.
Knowledge of context A theme specific to remote areas was the level of engagement of health professionals in becoming familiar with the particularities of this context36,39,42. Virtual medical support teams who were not familiar with the realities of providing care in remote areas lacked an understanding of the roles and needs of the professionals they were trying to help36,42. Physicians arriving from urban centers were not always aware that some medications and equipment are not available in remote areas39. Implementing a model of care that has not been adapted to the particularities of rural clinical facilities can also inhibit the implementation of initiatives to improve IPC40.
Traditional roles The attitudes of some professionals leaning more toward acting independently and/or according to traditional social norms were reported as a barrier to the implementation of initiatives to improve IPC. In some rural PHC facilities, patterns of working independently rather than collaboratively were ingrained in team members, resulting in a lack of teamwork32. Physicians tended to be viewed as competent in their role simply because of their academic qualifications, whereas nurse practitioners found themselves having to repeatedly demonstrate their competence23. In some rural settings, there were deep-rooted hierarchical relationships between health professionals that negatively impacted IPC32,35. Midwives also felt the need to prove themselves and demonstrate the importance of their role due to the negative perceptions held by professionals with more traditional roles, which may be the result of a lack of recent training among health professionals working in rural facilities41.
Facilitators: Five facilitators related to initiatives to improve IPC specifically in rural and remote areas were identified.
Team size Teams in rural or remote areas were typically smaller, which promoted proximity23,26,35 and interactions (formal and informal) among team members2,27,38,43 and may have also flattened hierarchical relationships2,43. Smaller team sizes also promoted shared responsibility31 and leadership among team members2,27,31,34,35,43. In some facilities, the presence of a ‘champion’ within teams was reported to enhance the implementation of initiatives to improve IPC30,37.
Past experiences and relationships Past experiences and relationships were important facilitators of IPC in rural or remote communities2,23,29,35,43,44 because professionals working in these settings frequently had a history of shared experiences with other health professionals27,35,41 that fostered the development of trust2,41. These past experiences and relationships in the same setting also fostered the development of a network of communication with various health professionals2.
Connection to community Connection to the community was another element that fostered IPC in rural or remote facilities35,42. Health professionals working in these facilities for some time became familiar with the unique challenges of patients and other health professionals2,35,39 and developed a sense of social responsibility and accountability2,35,42. They also developed a common understanding of the context2,35 and goals, and a shared team vision to better meet the needs of the community42. When initiatives to improve IPC aligned with organizational values and healthcare professionals were able to see positive impacts on the care of patients they knew, they were much more open to pursuing that initiative32.
Flexibility and openness The reality of rural or remote practices called for flexibility to adapt to different ways of doing things according to the specific environment2,31,34,39,41 and promote IPC-related behaviors. Working in small teams meant having the openness and flexibility to adjust to each other’s personalities and capabilities2,31,41 and even to blur professional roles34.
Financial support The presence of financial support was cited by several authors as an essential element when initiatives to improve IPC were implemented in rural PHC facilities30,31,35,45. Because teams in rural areas are smaller and workloads are high, financial support was particularly important to protect paid time to coordinate an initiative31,35. This financial support was also important to compensate clinical facilities, which generally have rather small operating budgets and cannot afford to implement IPC initiatives without financial compensation30. However, in the presence of a mobilized team, a lack of resources (including financial resources) could also result in creative solutions to improve IPC27.
Discussion
This scoping review found that few IPE and IPP initiatives to implement IPC in rural or remote PHC settings have been reported in the literature. The most common IPE initiatives were workshops, courses, discussion groups and simulations, while IPP initiatives fell into two main categories: clinical or technological tools. More studies have focused on the barriers and facilitators to the implementation of initiatives to improve IPC in rural and remote PHC settings, allowing the authors to identify several barriers and facilitators that appear to be unique to rural and remote settings.
The scarcity of research on IPE and IPP initiatives implemented in rural or remote PHC settings may be due to a number of factors. First, it should be noted that in the scientific literature most IPE initiatives are conducted with initial training learners rather than health professionals46,47. Second, it is likely that many initiatives in rural and remote PHC settings have not been published because health professionals working in these clinical settings might be less involved in research initiatives given their distance from most universities and researchers. Although the authors were able to consult some grey literature, it is possible that the number of IPE and IPP initiatives presented in this scoping review is an underestimation. Finally, the development and implementation of IPE and IPP initiatives is relatively complex15, and health organizations working in rural or remote areas may not have the full range of resources required to develop and implement these types of initiatives.
For IPP, the number of initiatives identified in the scoping review was even smaller; however, the number of IPP initiatives in different types of clinical settings identified in a systematic review by Reeves et al in 2017 was also small relative to that of IPE initiatives12. The lack of literature on IPP could be explained by a lack of consistency in the use and understanding of the term IPP, and further conceptualization work is needed to clarify IPP12.
With the COVID-19 pandemic in 2020, IPE initiatives in health science training programs have almost all moved online in the past year48. This shift in approach from face-to-face to online will likely carry over to IPE initiatives in clinical settings as well. Online IPE initiatives, particularly asynchronous training, are more flexible49, which may make this type of initiative more accessible to health professionals working in rural or remote PHC settings. However, to deploy this type of IPE initiative, reliable internet access is required49, which is generally very limited in rural or remote settings50. Therefore, the lack of high-speed internet access in rural and remote settings50 may limit the deployment of online IPE initiatives in these clinical settings and may also explain why few were identified in this scoping review.
Some of the barriers and facilitators identified may appear contradictory, indicating a high degree of variability of lived experiences and significant differences in group culture among rural and remote PHC facilities. These findings reaffirm that a one-size-fits-all model is not appropriate for IPC and that solutions should be developed locally in relation to the specificities of clinical settings. Implementers, policymakers and managers must, therefore, be flexible and carefully analyze social processes when developing and implementing initiatives to improve IPC51 in rural and remote PHC settings. Considering the importance of informal relationships in rural and remote areas, health organizations must facilitate relationship-building to foster the development of a common identity, particularly in transient teams, in order to promote collaborative practice24.
The presence of a local champion has been highlighted by some authors as a facilitator of IPC deployment in rural and remote PHC facilities30,37,52,53, but IPC implementation goes beyond the responsibility of a single individual and even beyond the responsibility of the team51. As highlighted, financial support from health organizations is an important element in supporting IPC implementation in rural and remote clinical settings, but strong actions and leadership from policymakers and health organizations are also needed to optimize IPC deployment51.
To be successful, IPE initiatives require leadership at all levels, both in academic and practice settings, so that the development of IPC skills and the increase in interdisciplinary practice are aligned with teaching modules13. The establishment of intersectoral groups or actions involving both health organizations and health professional educational institutions is a possible approach to ensure the sustainability of future IPE initiatives for health professionals working in rural or remote areas52. In Quebec, Canada, the delocalization of medical training in eastern Quebec led two universities and several regional health organizations to come together to identify IPC successes in PHC facilities to guide the development of IPE initiatives for health science students and health professionals working in rural and remote areas of eastern Quebec54.
Strengths and limitations
The strengths of this scoping review lie in the rigorous process of article identification and selection. First, a search statement was developed in close collaboration with a health sciences librarian to include all relevant articles. Subsequently, the articles were screened by three co-investigators until satisfactory inter-judge agreement was reached, thereby ensuring the credibility of the research.
Unfortunately, as recommended by some authors19,55, we were not able to carry out a consultation with stakeholders involved in PHC facilities in rural and remote areas in order ‘to offer additional sources of information, perspectives, meaning, and applicability’55. Consultations with stakeholders involved in these clinical settings will be the objective of an ongoing funded research project54. Given the limited literature on IPE and IPP initiatives to improve IPC in rural and remote PHC facilities, further research is needed. In particular, more longitudinal research might be relevant to better understand the medium-term impact of these initiatives on IPC deployment56 in rural and remote clinical settings. In addition, the use of theory-driven evaluative approaches such as a realist evaluation would also be very useful in guiding the development of future initiatives aiming to enhance IPC in rural and remote PHC facilities. These approaches are relevant for evaluating complex interventions such as IPE and IPP because they are process-oriented57, allow for the description of how an intervention is expected to produce its outcomes as well as the conditions under which it is expected to work58.
Conclusion
The results of this scoping review indicate that few initiatives to improve IPC in rural and remote primary care facilities have been published in recent years, although the deployment of IPC in these facilities is critical given the different challenges faced by those in these clinical settings. The facilitators specific to rural and remote clinical settings identified in this literature review, as well as the recommendations gathered, provide hope that new initiatives more tailored to rural and remote settings will be implemented and evaluated in the coming years to improve IPC and care delivery.
Acknowledgements
We thank Lisa Starr for her linguistic revision. This work was supported by the Faculty of Health Sciences of Université de Sherbrooke, the Collectif de recherche sur la santé en région (CoRSeR) of Université du Québec à Rimouski, and the Centre de recherche du CISSS de Chaudière-Appalaches.

