Context and issues
Transgender refers to an experience of assigned sex that does not match gender identity. Throughout this report, transgender will be used as an umbrella term to refer to people who fall outside binary gender expressions and people who have gender identity that does not match assigned sex.
Transgender patients experience barriers to accessing health care and receiving quality, non-discriminatory care1-4. Lack of access to culturally competent healthcare services contributes to health disparities that disproportionately impact the transgender community, leading to poorer health outcomes1,5-7.
One setting in which barriers for transgender people exist is the rural-serving, primary care environment. Research indicates healthcare experiences of transgender individuals in rural-serving primary care settings in South Central Appalachia are characterized by occurrences of stigma and marginalization8. Lack of cultural competency training related to transgender health needs may maintain care barriers. This project developed training for rural-serving medical residents that amplified transgender community members’ experiences with health care in the region to mitigate health disparities.
Training deficits in transgender health care
Literature on barriers to competent care for transgender patients indicates that providers experience discomfort regarding their ability to provide competent care2. Providers report a median of 5 hours of transgender healthcare training across their entire medical school curriculum9 with a national minimum of 45 minutes per year10. A 2018 national survey of US medical schools indicated 76% of medical students rated their transgender health education as fair or poor, while 83% of students reported minimal to no transgender health education in their entire residency training experience11. This gap in training is apparent in medical providers’ lack of knowledge regarding best practices for transgender health care and in their discomfort with treating transgender patients11. Primary care physicians have expressed a lack of preparation and appropriate training for working with transgender patients12, reporting feeling worried that their lack of training could inadvertently harm transgender patients they treat. This concern often leads to avoidance of treating transgender patients at all13. Literature suggests that many barriers to competent care may be addressed by improvements in provider education14.
Rural-serving primary care clinics
Provider trainings for transgender health competency have been piloted in clinics across the USA15-21. Many of these piloted interventions for healthcare providers have improved provider knowledge regarding trans patient care needs and overall clinical competency15-21. While literature supports the notion that trainings in residency focusing on transgender health are useful, many of these studies have been piloted in metropolitan areas and, to the authors’ knowledge, none have been piloted in rural-serving clinics in the southern region of the USA. This type of medical training is imperative to improve the health of transgender patients. Appalachian culture is predominantly steeped in Christian ideology8. Literature highlights that cultural belief systems that reinforce biblically informed gender norms discourage and minimize identities outside of this rigid system22. Therefore, developing a customized training model for this region was critical for understanding how to best address deficits in provider education and cultural barriers that exist in the region.
An intersectional approach, or one that considers the range of identities a person holds, is suggested22 when conducting research with participants who have marginalized identities. Transgender patients in South Central Appalachia experience intersectionality that exponentially multiplies barriers to receiving competent health care8. In addition to barriers to care in rural areas, such as lack of economic resources8 and lack of transportation/proximal distance barriers to affirming healthcare clinics, transgender patients with lower income experience higher rates of care refusal due to having fewer resources to research more inclusive providers and/or travel further for care8,9,23. Medical education for residents within this region can assist in reducing negative bias toward transgender patients and remove some barriers that exist in seeking competent health care.
Appalachian culture itself functions as an identity that impacts medical care. There is reportedly a perception that medical providers lack cultural competency regarding Appalachian values broadly8. Cisgender patients in this region cite this incompetence as a barrier to utilizing healthcare services and are more likely to report poorer health outcomes than people who are not from Appalachia8,24. Transgender patients in Southern Appalachia specifically report having to educate providers about ways to respect them and being afraid of care refusal if they practice self-advocacy25,26. Further, patients must work diligently to obtain health insurance that might cover some of their transition care26 and search for a provider close to their geographic location who is willing to treat them26. Transgender patients in South Central Appalachia are at greater risk of experiencing healthcare disparities compared to other transgender patients in the country, and yet there have not been medical education interventions for primary care providers in this region that have included community needs assessment data.
The current project
The present project utilized a mixed-methods design to engage rural-serving medical residents in primary care in South Central Appalachia in the development of a cultural competency training specific to the needs of transgender patients in this region. This training was developed utilizing the Kern Model27, a medical curriculum development approach. This model includes six phases: (1) problem identification and general needs assessment, (2) targeted needs assessment, (3) outlining goals and objectives, (4) identifying educational strategies, (5) implementation of the educational intervention, and (6) evaluating the intervention. This article’s focus is steps 1 through 4.
Ethics approval
This project was approved by the East Tennessee State University Campus Institutional Review Board (# c0221.15e) on 2 March 2021.
Lessons learned
Phase 1: Problem identification and general needs assessment
First, a scoping literature review28 was conducted. Structured searches of three databases using relevant keywords were utilized. Literature was sorted into a matrix based on type of methodology, year of publication, and predetermined, qualitatively assigned categories.
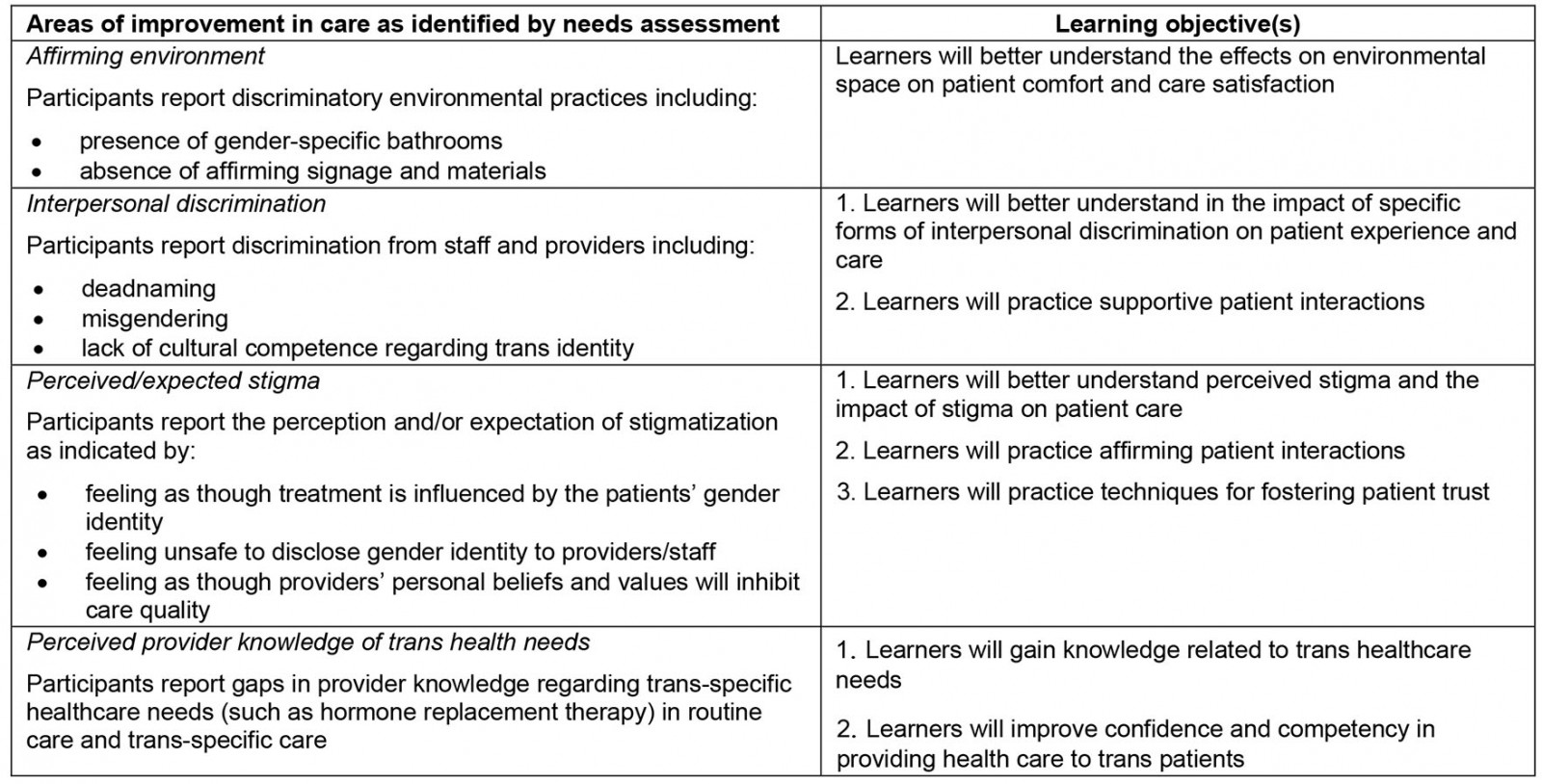
The scoping literature review yielded approximately 50 relevant peer-reviewed works that encompassed about seven qualitatively determined themes within transgender health care (barriers to care, provider education, minority stress, intersectionality, pedagogical considerations for medical education, trans health in the southern USA, Appalachian health care). These themes and the community-based data described below informed the development of the learning objectives as the intention of this project was to elevate the voices of community members and stakeholders. Learning objectives are described in Appendix I.
Phase 2: Targeted needs assessment
Targeted needs assessment involved community-based data gathering from two relevant groups. First, needs assessment data collected from the East Tennessee State University’s TransACCESS survey detailed transgender patients’ experiences with health care in South Central Appalachia. These data were utilized in phases of development to provide feedback to residents related to patients’ healthcare experiences. The second group consisted of medical residents at a medical college in South Central Appalachia across three regional clinics.
Two major themes arose from planning with these key stakeholders: accessibility/reusability of the material and usefulness of the material to the resident. Stakeholder participation in the program development was used to create a sustainable training that could be left with the residency program after the conclusion of the project. Stakeholder participation was also utilized to fit the training to social distancing guidelines during COVID-19. Stakeholders included training facilitators within the medical school faculty, clinic behavioral health providers, and resident liaisons. Resident liaisons assisted in the development of the training by indicating what the most useful topics within transgender health would be to learners.
COVID-19 presented an opportunity to address accessibility concerns in rural areas broadly by having to design material to be hybrid-delivered while also being engaging, useful, and meaningful. Ultimately, this was achieved by creating material that was site specific and by reimagining the participatory elements of the training for fully virtual training sessions. This was also achieved by curating a resident-informed resource guide that could allow quick access to primary care resources residents may need on site.
Phase 3: Outlining goals and objectives
Learning objectives for the planned medical education intervention were largely derived from the TransACCESS data and following input from stakeholders including resident liaisons, educational consultants to the training program, and behavioral health didactic facilitators within the residency training program. Stakeholders were asked to identify areas of competency that would be beneficial for their practices and what baseline information would be necessary for all participants to know.
Phase 4: Identifying educational strategies
Educational strategizing occurred in three steps: contextual considerations, goal setting, and training design. First, due to the current study taking place during the COVID-19 pandemic, the training had to be customized to the needs of busy family medicine practices while also following social distancing guidelines. Trainings were a hybrid of virtual and live delivery to pivot in response to space allocations at each clinic and to allow residents who were on hospital rotations to attend. The full virtual version of the modules allowed for maximum engagement and interaction from virtual attendees through polling activities, chat function-based discussions, and more interactive material such as videos. Second, pedagogical goals for this study were set and included accessibility, sustainability, and usefulness to the residents’ practice, as these aspects have been identified in literature as being barriers to transgender healthcare training implementation11. Third, an educational consultant was utilized to inform the best style of training design to meet the stated pedagogical goals. Accessibility was addressed through the hybrid delivery format as well as through the ‘living’ resource guide provided to residents following the conclusion of the study. Sustainability was addressed by including behavioral health providers and training facilitators in the training module design and implementation for the training to be continued in future residency cohorts. Usefulness was addressed through interactive case presentations and interdisciplinary work on clinical vignettes that may present in a family medicine practice. Including stakeholder residents in the development of the modules also contributed to usefulness, as it allowed topics to be included that residents were specifically seeking information about, such as cancer screening protocols, information about hormone replacement therapy, and documentation challenges with pediatric patients.
Discussion
A national deficit in transgender health-related educational content during medical training9-13 contributes to health disparities and discrimination in health care. Much of this programming implemented to address this concern15-21,29 has been implemented prior to students working directly with patients or in more urban areas. Thus, there is an ongoing need to address intersectionality concerns in rural-serving areas.
Previous studies have indicated that, on average, medical providers do not receive adequate training on transgender health needs. Research has demonstrated that more training opportunities for providers leads to increased provider knowledge and comfort treating transgender patients in primary care. Ultimately, enhanced training leads to higher care quality and fewer discriminatory experiences for transgender patients.
The summary of the systematic literature review conducted at the beginning of this project indicated a national deficit in competency trainings. Literature also suggests differences in general medical education due to resource competition30. If resources are part of the cause of the national deficit of transgender healthcare education, precious resource utilization needs to culminate in sustainable, accessible, and useful content. Developing sustainable, accessible, and useful medical education is challenging in optimal circumstances but development during a global pandemic presented unique barriers. It was imperative to this project to include resident and community member feedback in the content creation of this project as it allowed the modules to be customized to the community’s and residents’ unique needs. This will allow for the future implementation of these modules beyond the timeline of this project, and for residents to have their practice needs met through the living resource guide and the training content.
Stakeholder input on the pedagogy of this project was critical due to physical space constraints with social distancing guidelines as well as the setting of a very under-resourced region with health risks that outnumber the national averages and a unique sociopolitical culture. This training needed to meet the needs of the transgender community, the needs of medical residents, and adhere to social distancing guidelines to mitigate the impact of COVID-19 as much as possible. Without stakeholder input on how to meet these seemingly conflicting goals, the development of this training would not have been successful. While it emerged largely as a response to COVID-19, virtual medical education will not become obsolete post-pandemic. This training highlights the value in engaging virtual curricula, as it allows optimal accessibility for rural clinics and for residents who may be out on other rotations. Virtual curricula can also allow for longevity of content, as highlighted by the resource guide, an outcome that is important to consider for under-resourced clinics.
Integrated care is the new frontier of both medicine and health sciences. Conducting psychological research that leverages community participation allows for translation of integrated clinical practices to integrated pedagogical and psychological research. This project was a collaborative effort and stimulated interdisciplinary conversations at all time points of the project and with all roles that were involved. This was a critical, yet unintentional, outcome of this project. During the time of this project, multiple anti-transgender political actions were underway, including Bill SB-1646 in Texas, which upholds providing transgender youth health care as reportable child abuse, and Tennessee’s bill that passed in May 2021 prohibiting medical providers from prescribing hormone replacement therapy (including puberty blockers) to transgender youth. Having interdisciplinary discussions rooted in scientific evidence while these laws were being discussed and highly politicized allowed for real-time problem solving and differing ideas to be shared. Medical education that includes voices from other disciplines furthers the future of integrated care and provides comprehensive training that benefits patient communities.
This project developed a training specific for South Central Appalachian providers that was informed by transgender people in the region and tailored specifically for regional providers based on stakeholder input. The resulting training, coupled with the resource guide provided to residents, may be an invaluable tool for the future medical providers in this rural-serving region that is medically and educationally under-resourced and experiences inflated intersectional discrimination at systemic and interpersonal levels8. As previously noted, residency program directors in the Southeastern USA predominantly hold negative attitudes regarding the importance of transgender health education11, which exacerbates existing social disparities in Southern Appalachia8. Continuing to implement trainings nationally to advance transgender healthcare competency is an improvement to the larger healthcare system. Care avoidance due to fear can be a costly public health issue, which can be assuaged by more provider trainings; in Appalachia, this is multiplied as Appalachia is historically burdened by poorer health outcomes compared to other regions in the USA8,24,26. With a recent rise in the call to action for psychological and medical communities to be more inclusivity focused, efforts in developing trainings to promote inclusion and improve provider competency could improve the wellness of transgender Appalachians. When research and program development can focus on the serving communities in which we live, tangible and experiential change can occur, even if improving patient care for just one person or improving competency for one provider.
References
You might also be interested in:
2022 - Medical students’ experiences of compulsory rural service in Guatemala: a qualitative study
2016 - Solutions to physician undersupply in rural areas: from the experience of rural Fukushima