Introduction
Health workforces around the world face longstanding geographic imbalances and shortfalls in rural and remote areas to meet current and future population health needs1-4. Pecuniary incentives are frequently raised as a public policy option to bolster recruitment of health practitioners to rural communities in public sector occupations5. However, there is limited nationally representative research on remuneration and other factors influencing recruitment and retention of healthcare providers in rural and remote areas, and much of the available literature focuses on the physician and nursing workforces1,6-11. In Canada and elsewhere, comprehensive evidence on the distribution and incentivation of allied health professionals (AHPs) is remarkably deficient, especially in relation to understanding spatiality issues across the rural–urban continuum.
Allied health workers represent diverse professions, providing a wide range of preventive, diagnostic, rehabilitative, and therapeutic services in a variety of settings. Even in countries with single-payer universal healthcare coverage such as Canada and Australia, AHPs operate in both the public and private systems, which may lead to perceptions of fewer opportunities for career enhancement and adequate remuneration under smaller practices in rural areas12-15. In Canada, previous research using administrative data from professional regulatory bodies has demonstrated a strong relationship between the degree of urbanization and highest concentrations of practicing AHPs within selected jurisdictions14,16. Studies elsewhere have relied on surveys to profile the rural AHP workforce in terms of demographic and practice characteristics not often captured in administrative sources17-19. A key challenge to informing policy initiatives to improve the geographical distribution of AHPs is the lack of a universal definition of rurality and, in turn, appropriate recognition that rural and remote communities are highly heterogeneous and entail marked differences in the experiences of healthcare practitioners3,20,21.
Allied health professionals are estimated to be a predominantly female workforce. Women represent 67% of the global health workforce, although the gender ratio varies across occupations and much of the supporting data on gender health labor market disparities refer to physicians and nurses22. The persistence of shortages of women practitioners in rural areas is a vital, albeit often overlooked, topic for policy dialogue and action23. There is a specific dearth of research evidence to inform planning and management of the rural AHP workforce from a gender perspective. For instance, a number of recent reviews of the literature on recruitment and retention of health workers in rural and underserved areas1,2,6 remained gender-blind – ie they failed to make any recognition of the role of sex and gender in rural health workforce outcomes. Yet, women health professionals are known to encounter many gender-related inequalities, such as wage gaps in relation to men22.
This national observational study examines the geographic distribution and earnings of AHPs in Canada across the rural–urban continuum. The AHP workforce is broadly considered to include five groups of university-trained health professions distinct from medicine and nursing: (1) dentists, (2) pharmacists, (3) other allied health diagnosing and treating professionals (eg optometrists, chiropractors), (4) physiotherapists and occupational therapists, and (5) other health occupations in therapy and assessment (eg audiologists, kinesiologists). The study leverages population census data linked to geocoded indices of community remoteness and accessibility, to examine factors predicting trends in the composition and compensation of the AHP workforce. Two key research hypotheses are tested: first, that the remuneration levels of AHPs would be inversely associated with relative remoteness; and, second, that these earnings imbalances would be exacerbated by disparities in female-to-male representation within and across allied health occupations. Special interest is paid to occupations that have been historically characterized as dominated by men, such as dentists and pharmacists24,25, to ascertain potential changes in the spatiality of AHPs associated with shifts in gender compositions.
Methods
For this study, two rounds of nationally representative data from the 2006 and 2016 Canadian population censuses26,27 were pooled and then linked with the geocoded Index of Remoteness (IR) for all inhabited communities28. In the census, detailed information on labor market activities and sociodemographic characteristics is collected by Statistics Canada using the mandatory long-form questionnaire, which was distributed to 20% of households in 2006 and 25% of households in 2016. The 2016 long-form collection response rate was 97.8% nationally, although slightly lower in the three northern, sparsely populated territories (94.7–96.5%)29.
Drawing on research approaches developed elsewhere to investigate imbalances in the physician and nursing workforces30, the census data were linked by respondents’ place of residence to an index computed by Statistics Canada scoring the relative remoteness and accessibility of all of the country’s 5125 communities (census subdivisions) reporting some resident population or connected to a population center through the national road and ferry network28. Rather than conventional geographic classifications of rurality and urbanity based on proximity to census metropolitan areas and agglomerations, the IR was measured on a continuous scale, using a spatial gravity model for capturing different elements of connectivity and service provision31. The index ranges from 0 to 1, with the lowest values representing the most urbanized and accessible areas (eg the most urbanized regions of southern Ontario and southern Quebec) and the highest values reflecting the most rural or remote areas (eg some northern settlements not connected year-round to a population center through the main road network)28,31.
Health professionals were mapped from the census data according to the National Occupational Classification, a taxonomy for systematically classifying occupations according to skills requirements, job duties, and working conditions32. The present analysis retained five groups of full-time allied healthcare providers, all highly educated professionals in the prime working ages of 25–54 years, with a bachelor’s degree or higher educational attainment, and reporting earnings through employment or professional practice (Table 1). Those whose main work duties were in teaching or in facility administration were excluded (classified elsewhere). Some occupations were grouped to respect federal statistical rules for minimum cell sizes and concentrations, especially for sensitive earnings data disaggregated by place of residence and by gender. As the main outcome of interest, earnings were captured at the individual level as all income received as wages, salaries, and commission from paid employment and net income from self-employment or professional practice in the calendar year before the census33.
Table 1: Selected allied health professional groups, 2006 and 2016 Canadian population censuses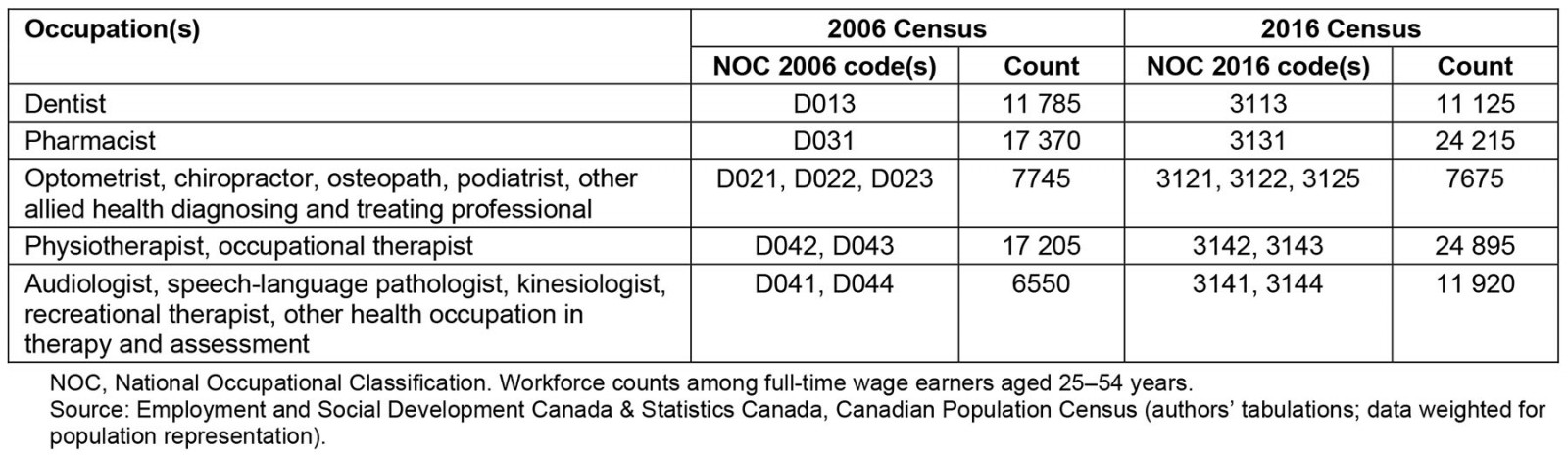
Statistics analysis
Descriptive, bivariate (correlation), and multivariate (regression) analyses were used to better understand the geographic distribution and other characteristics of the AHP workforce as well as predictors of differentials in remuneration by relative remoteness. Specifically, multiple linear regression was used to estimate the associations between IR values and individuals’ professional income (logged to address skewness), adjusting for gender and other personal and professional characteristics. The level of statistical significance for the regression coefficients was set at α=0.05. For ease of interpretation, the continuous remoteness values were classified into 10 equal intervals (deciles) to aggregate communities with similar IR values to form meaningful discrete categories34. Person-level census weights were applied to ensure population representation of the results and 95% confidence intervals (CIs). Counts were rounded and some variable categories were aggregated in respect of Statistics Canada privacy and confidentiality protocols. Regarding the 2006 census data, earnings are presented in inflation-adjusted Canadian dollars (ie constant dollars against the 2016 census income reference year). All analyses were conducted using the Stata statistical software package (StataCorp LLC; www.stata.com).
Ethics approval
The de-identified census microdata used in the analyses were accessed at the New Brunswick Research Data Centre (NB-RDC), located at the University of New Brunswick (UNB). The study complied with ethics protocols of the UNB Research Ethics Board, which does not require an additional institutional ethical review for research using national statistical sources accessed in the NB-RDC.
Results
The AHP workforce counted 79 820 full-time professionals aged 25–54 years according to the 2016 census data, up by 32% from 10 years earlier (Table 1). The rate of increase was faster than that of the general household population, such that the provider-to-population ratio grew from 19.6 per 10 000 population in 2006 to 23.2 per 10 000 population in 2016 (Fig1). The AHP densities remained highest in the most urbanized areas of the country in 2016: 23.6-25.6 per 10 000 population across the 30% most urban and accessible communities (ie Remoteness Deciles 1–3). The densities generally declined with increasing rurality and remoteness, falling steeply to a low of 1.6 AHPs per 10 000 population in the 10% most remote communities (ie Remoteness Decile 10). The latter was up only slightly from a decade earlier (1.3 per 10 000 in 2006).
The dentist workforce was characterized as predominantly male, but rapidly feminizing over time (31% women in 2006, increasing to 43% in 2016). Other AHPs in diagnosing and treating were similarly male-dominated but feminizing (from 38% up to 46% women over the 10-year period). The pharmacist workforce counted more women than men, with a somewhat slower pace of feminization (from 59% up to 62% over the same period). Physiotherapists, occupational therapists, and other AHPs in therapy and assessment remained strongly female-dominated (approximately 80% women). A strong positive correlation was seen among women AHPs in terms of the degree of feminization of their profession (ie share of women) and the geographic distribution by relative remoteness (ie mean IR value) (Fig2). While the correlation among men AHPs was weaker, the most male-dominated dentist workforce had the highest concentration in the most urbanized parts of the country (ie lowest mean IR value) among both men and women. Conversely, the most female-dominated therapy and assessment professionals were the most geographically dispersed in terms of relative remoteness (ie highest mean IR values), among both men and women. The most rapidly feminizing dentist workforce also experienced the most rapid geographic spread in terms of increased mean IR value between the two census periods.
The highly urbanized dentist workforce had the highest mean annual earnings of the AHP groups under observation, although the returns were found to decline somewhat against inflation over the decade among women and especially men (Fig3). Men AHPs earned more than women in both time periods and across all groups - except for other (non-physical or occupational) therapy and assessment professionals, among whom women’s average earnings surpassed those of men by 15% in 2016. A discernible but weak negative correlation was seen among women AHPs (negligible among men) in terms of professional earnings and relative remoteness.
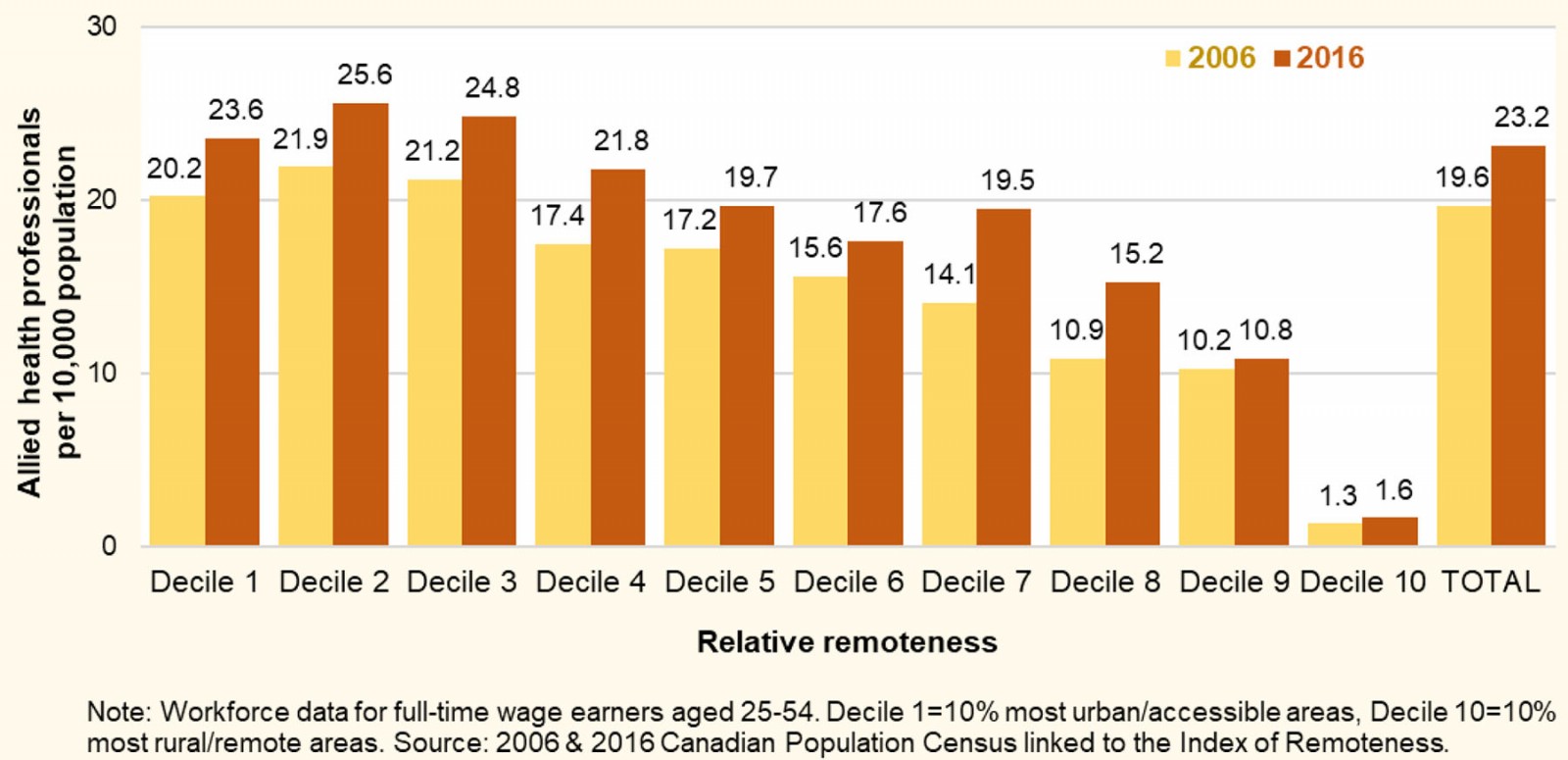 Figure 1: Allied health provider-to-population ratios by relative remoteness of communities, Canada, 2006 and 2016.
Figure 1: Allied health provider-to-population ratios by relative remoteness of communities, Canada, 2006 and 2016.
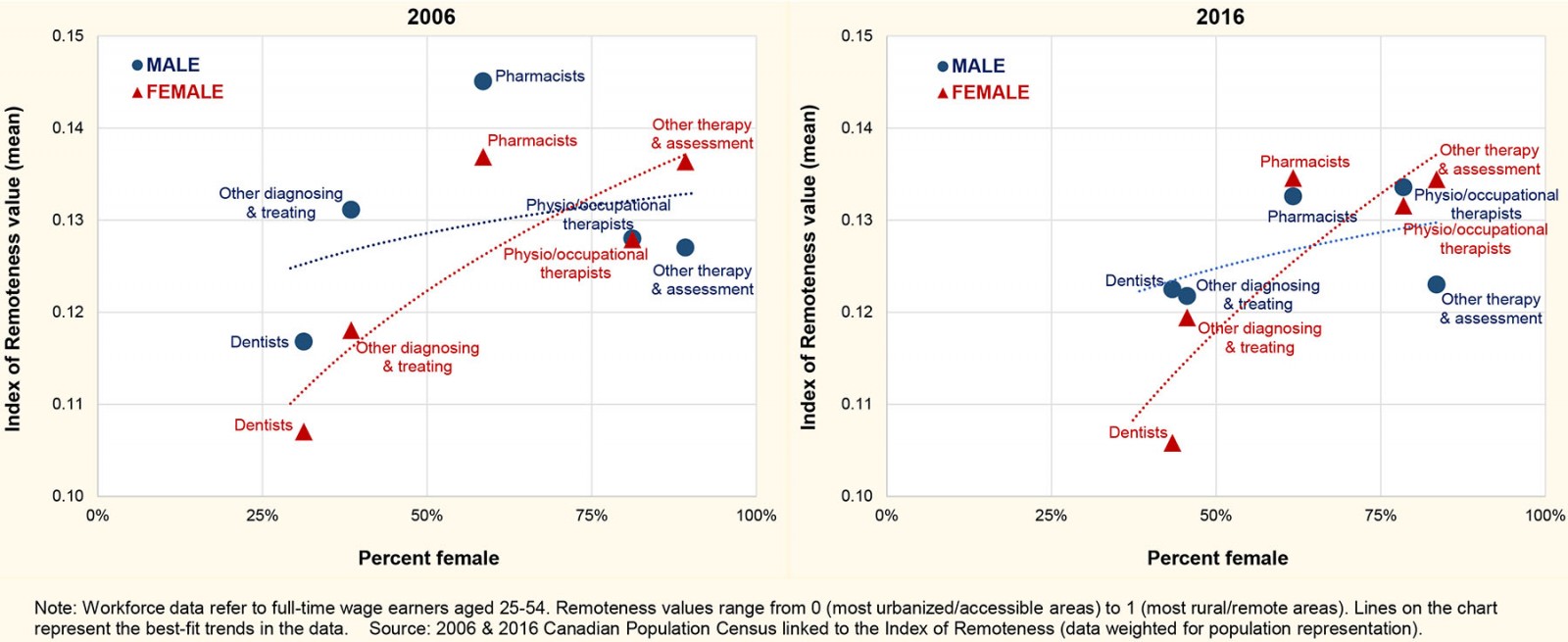 Figure 2: Mean relative remoteness score by percentage female among the Canadian allied health professional workforce, according to occupation.
Figure 2: Mean relative remoteness score by percentage female among the Canadian allied health professional workforce, according to occupation.
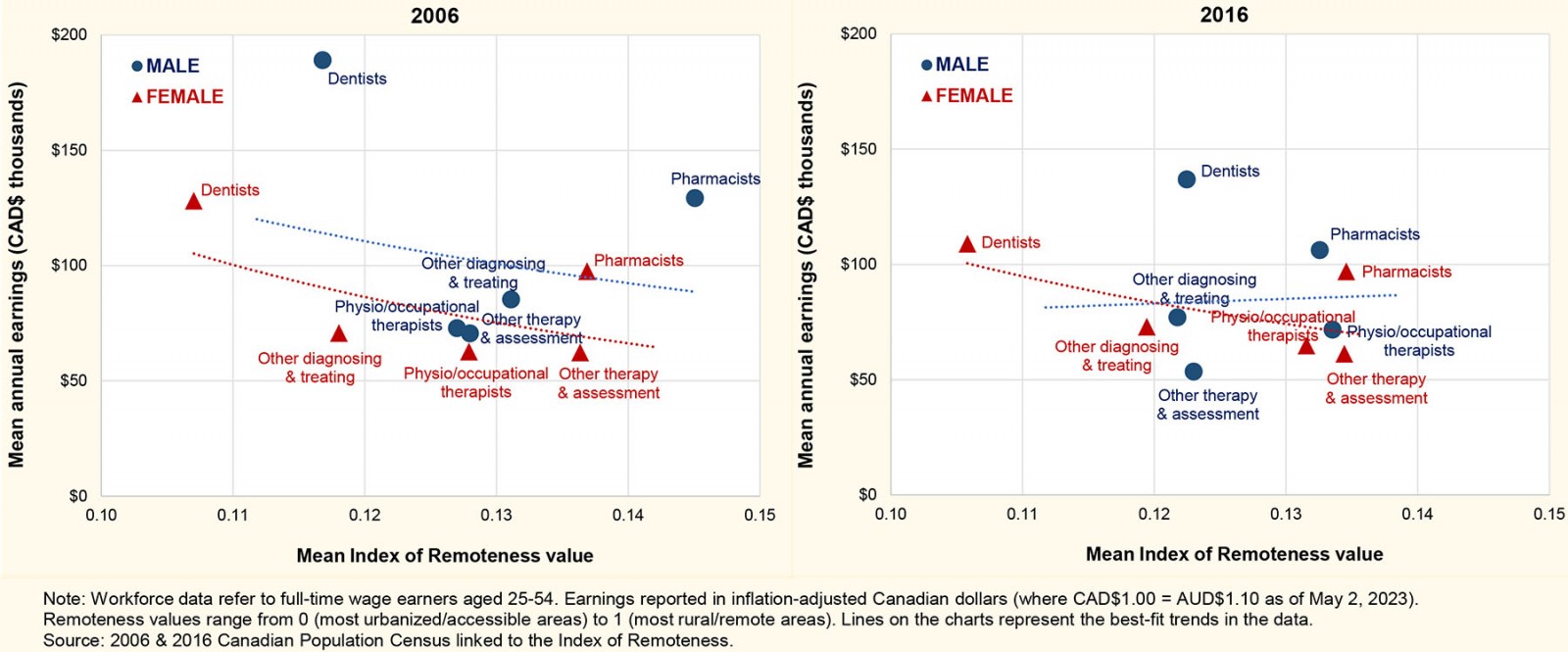 Figure 3: Annual professional earnings by mean relative remoteness score among the Canadian allied health professional workforce, according to occupation.
Figure 3: Annual professional earnings by mean relative remoteness score among the Canadian allied health professional workforce, according to occupation.
Results of multiple regression analysis of earnings differentials
The linear regression models indicated that relative remoteness generally contributed little to wage differentials within the five allied health occupations, upon adjusting for other professional and personal factors (Table 2). However, two statistically significant patterns emerged. Pharmacists residing in more rural and remote areas of the country (IR deciles 5+) were found to earn 9% (95%CI 4–15%) more annually than those in core urban centers (IR decile 1), all else being equal. On the other hand, among other (non-physical or occupational) health-diagnosing and treating occupations, a 16% (95%CI 6–28%) wage premium was found for those living in highly urbanized non-core areas (IR decile 2) compared to those in the core urban centers.
Gendered wage differentials were observed, with women earning significantly less than men in the professions of dentistry, pharmacy, and physical or occupational therapy. Conversely, women in other (non-physical or occupational) diagnosing and treating occupations earned 9% (95%CI 1–17%) more than men.
These patterns were observed during a period of relative wage stagnation among allied health professionals, with annual earnings tending to remain the same or lose ground to inflation across the two census periods. In terms of educational attainment of AHPs, having graduate-level studies was often found to positively impact earnings compared to having at-most undergraduate studies, particularly among dentists (40% higher earnings). Significantly lower earnings were seen among dentists and pharmacists who were visible minorities, after controlling for relative remoteness, education, and other factors. No discernible wage disparities were seen among AHPs who self-identified as Indigenous (First Nations, Métis, and/or Inuit ancestry), although the numbers of university-educated Indigenous professionals were considerably lower than their share in the total Canadian population (1.3% v 4.9% based on the 2016 census)27.
Table 2: Descriptive analysis (percentage distribution) and results of the multiple regression analysis (coefficients and 95% confidence intervals) for predictors of earnings differentials among the allied health professional workforce 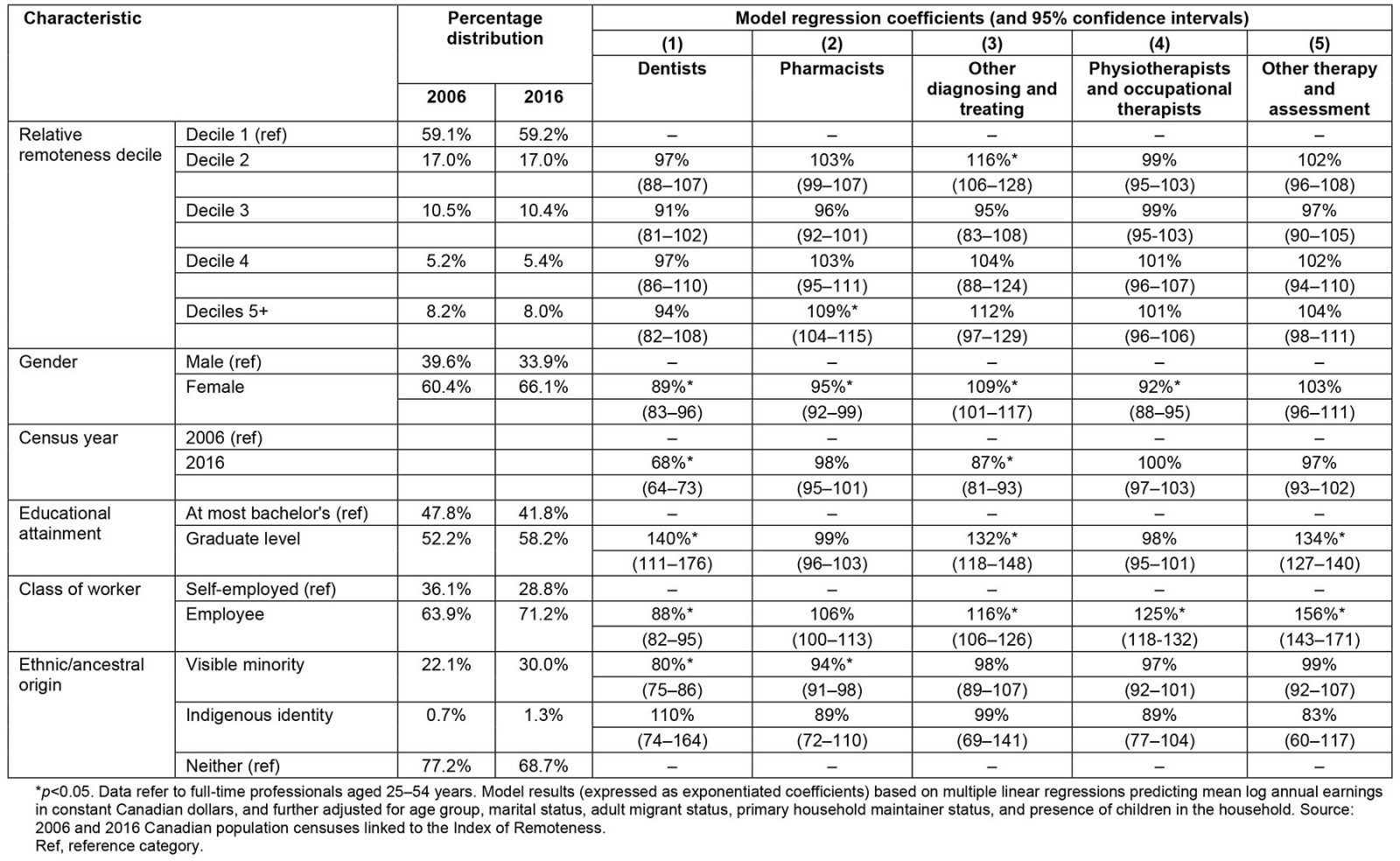
Discussion
Many health workforce studies to inform initiatives for recruitment and retention to rural and remote locations focus on physicians and nurses, classify rural and remote communities as a homogenous group, or rely on study designs lacking urban comparators. This Canadian study drew on nationally representative data to investigate trends in the geographic distributions and role of relative remoteness on professional earnings among a range of allied health occupations. Unequal distributions of AHPs were found, with provider-to-population ratios averaging around 15 times higher in more urbanized and accessible parts of the country compared to the most rural and remote areas, a pattern that had changed little over the 10 years of observation. Significantly higher annual earnings were found among pharmacists in rural and remote areas compared to those in core urban areas after adjusting for other professional and personal characteristics; however, similar wage variances were not seen for other AHPs in diagnosing, treating, and therapy services. The geographic distribution of the pharmacist workforce was more dispersed in terms of relative remoteness than dentists, and by 2016 was similar to that of some therapy and assessment occupations.
While the census-based income data used in the analysis did not enable the disentanglement of earnings from financial incentives as a recruitment technique (incentives that vary by province and territory under Canada’s decentralized healthcare system), the evidence base to support additional payments to AHPs to reduce perceived opportunity costs associated with working and living in rural and remote areas remains limited. Some findings from other contexts have pointed to financial incentives as a tool for recruitment and short-term retention, but not necessarily longer term retention in the same area6. A qualitative assessment in the Canadian province of British Columbia found few AHPs cited monetary incentives as important in decisions to practice in rural or northern areas; non-pecuniary factors such as personal values, rural background, and family and community influence often had greater salience35. Thus redressing geographic maldistribution in the health professional workforce may entail shifting the narrative from the need for incentivizing working in remote locations as a compensation for ‘hardship’ to the attractiveness of cultivating their practice while building a meaningful sense of place and belonging35,36. Different opportunities for services provision may be worth emphasizing for different ranges of remoteness31, such as enhanced virtual care.
Identifying the barriers and facilitators to AHP recruitment and retention in rural and remote areas is complex yet understudied, with gender issues particularly so. This study found, among the selected allied health professions, a direct association between the degree of occupational feminization and geographic dispersion in terms of relative remoteness. The pattern was consistent with research elsewhere among medical and nursing professions in Canada30. This suggests that, beyond formal incentives for rural practice, policy initiatives should target remedying gender-related pay inequities and enhancing professional opportunities for women with children25. Professional earnings were found in this study to average significantly less among women in dentistry, pharmacy, and physical or occupational therapy, consistent with widespread studies on gender wage gaps among physicians and nurses. However, women in other diagnosing and treating professions (other than dentists and pharmacists) earned more than men on average, after adjusting for remoteness and other characteristics. Limited earlier research from the US suggested that women may fare relatively better than males in some allied health occupations37. More timely and comprehensive research is needed on wage disparities and other gender-related questions among AHPs in different national and rurality contexts.
Study limitations
As with all observational research, some limitations to this study are noted. For ease of comparison, the target population of AHPs was restricted to full-time wage earners at the time of each census. It is possible that selection biases may have arisen due to the exclusion of part-time workers, who may be more predominantly women and/or rural practitioners. Also, the data did not distinguish between dual healthcare employment across the public and private sectors, the latter possibly being more constrained in rural and remote areas. In Canada, health professional licensing, scopes of practice, and funding models are governed within a complex web of government and non-governmental stakeholders, yielding highly varied work settings and arrangements38. For example, most dentists are in solo private practice, whereas physiotherapists are being increasingly embedded within family health teams, and other AHPs such as audiology practitioners have seen escalating shifts from the public to the private sector in many provinces38. The census data upon which this study relied lacked the granularity to demarcate different practice models or sources of remuneration. The present analysis did not measure length of stay in the residential location, hampering the consideration of turnover, which may be notably problematic in the most remote communities. Lastly, the study did not account for effects of regulatory measures for service in rural and remote areas, for which more robust evidence of effectiveness compared to financial incentives has been found elsewhere6.
Conclusion
In Canada and around the world, people in rural and remote areas often have poorer health outcomes than their urban counterparts, attributed at least in part to unequal access to healthcare service providers4,39. Financial incentives for rural practice are commonly described as a policy option to address health workforce maldistribution. The present study using nationally representative data did not find convincing evidence of wage disparities by relative remoteness as characterizing allied health professionals in Canada. More attention is needed to gender and other social characteristics of health professionals that are underexplored and underexplained in research and policy dialogues on factors for rural health workforce recruitment and retention.
Acknowledgements
Financial support for this work was received from the Social Sciences and Humanities Research Council of Canada (SSHRC) (award #435-2020-0706). The data analysis was conducted in the secure computing environment of NB-RDC, which is part of the Canadian Research Data Centre Network. The services and activities provided by the NB-RDC are made possible by the financial or in-kind support of the SSHRC, Canadian Institutes of Health Research, Canadian Foundation for Innovation, Statistics Canada, and University of New Brunswick. The project funder and partners had no role in study design, data analysis and interpretation, preparation of the manuscript, or decision to submit for publication.
References
You might also be interested in:
2015 - Indonesian medical students' preferences associated with the intention toward rural practice
2011 - Tribute to Dr John Irwin
2011 - Health promoting community radio in rural Bali: an impact evaluation

