Introduction
The COVID-19 pandemic has demonstrated the catastrophic impact a communicable disease can have on a country’s health, society and economic sustainability. It has also revealed how rapidly a novel viral respiratory pathogen can affect healthcare systems in countries globally, leaving little opportunity to broaden existing response mechanisms. This is particularly important in low- and middle-income countries where existing health infrastructure is inadequate and where the rate of existing communicable and non-communicable diseases is already high.
Papua New Guinea (PNG) has a population of approximately 8.8 million and more than 70% of the population live in rural areas1. Low health literacy, hygiene practices, and access to healthcare services in rural and remote locations contribute to poor health outcomes. PNG is challenged by diseases commonly seen in low-income countries, such as HIV/AIDS, malaria, tuberculosis, leprosy and cholera, as well as illnesses more common in high-income countries, such as cancer, stroke, heart disease, obesity, diabetes and hypertension2.
PNG is therefore facing many challenges in managing an already overburdened healthcare system as it responds to COVID-19. Reports from non-governmental organisations have suggested that PNG’s health systems are on the brink of collapse as COVID-19 cases increase and multiple healthcare workers test positive and are required to isolate3. Pre-COVID-19, PNG was already affected by several escalating rates of communicable diseases. Tuberculosis, including the drug-resistant strain XDR-TB, has one of the highest incidences in the world, with 30 000 new cases reported each year4. Malaria, a constant threat to PNG and the surrounding islands, makes up 94% of cases in the Western Pacific region5. Similarly, because of low immunisation rates, PNG has reported recent outbreaks of polio and measles6,7. However, in PNG, resources normally focused on immunisation programs have been diverted to COVID-19 initiatives. In addition, normal vaccination outreach patrols drastically reduced, if not ceased, in some areas due to travel restrictions at the time. Effectively, COVID-19 has affected not only the community but also a healthcare system that was already struggling to support a vulnerable population.
This research was undertaken in September 2021, when transmission of COVID-19 was reported by the government as ‘rampant’; however, mass testing was not possible, and infections were presumed to be vastly underestimated. A national roll-out of the AstraZeneca vaccine, donated by Australia, commenced in May 2021. These doses were targeted at the healthcare workforce; however, uptake was slow, with less than half the doses administered. Sinopharm BIBP, donated by China, was rolled out to Chinese citizens in June 2021, and in July 2021 a nationwide vaccination program for those aged more than 18 years commenced. This occurred as the country faced considerable vaccine hesitancy, with fewer than 55 000 having received a vaccination, and approximately 70 000 donated doses discarded8. Provincial District Health Services and non-governmental organisations turned their efforts to correcting misinformation spread on social media and other forms of communication and began providing vaccine awareness campaigns to healthcare workers, community leaders and church leaders9.
On 17 June 2021, the Papua New Guinea Council of Churches (PNGCC) declared its support for COVID-19 vaccination, following a conference in Port Moresby. In a statement, church leaders pledged their complete support to assist the government of PNG and local communities to ‘address community concerns, to work with all partners to ensure that all people are reached and vaccinated consistently’10. Church leaders also joined the Sleeves Up campaign to dispel misinformation and promote vaccination as a safe way to control COVID-19 and protect individuals from serious illness or death.
The experience of COVID-19 in PNG illustrates the critical need for continued distribution and delivery of life-saving vaccines. This project aimed to understand the accessibility of vaccines for the general community in provincial PNG, the level of and reason for community vaccine hesitancy, and ways to strengthen vaccine acceptance among target groups within the community.
Methods
Study design and collection
A concurrent mixed-method design was used, whereby both qualitative and quantitative data were collected to address the research aims. Data collection was carried out in-country by an experienced Australian healthcare researcher and a local healthcare worker and researcher fluent in English and Tok Pisin (interpreter as required), both official languages of PNG. Both researchers were present at the time of data collection with the local healthcare worker taking the lead to provide local context and ensure the questions were understood. Participant information and consent were provided in both languages; however, due to most participants being fluent in English, the survey itself and interviews were conducted in English with translation when required.
A self-administered survey, employing both Likert and short-answer responses, was used to address vaccine hesitancy and intent to vaccinate within the community. The survey was disseminated to a convenience sample of willing participants at local community events where vaccine awareness campaigns were being undertaken. The questions included were adapted from two pre-existing validated survey instruments, the Oxford COVID-19 Hesitancy Scale and the Oxford COVID-19 Vaccine Confidence and Complacency Scale11. To address specific PNG beliefs about COVID-19 and the COVID-19 vaccine currently circulating at a community level, in the media and on social media, additional questions were included to identify cultural and religious beliefs, myths and misinformation. These additions were developed with and piloted by a small cohort of six public health nurses working in the province. For a more in-depth perspective, purposive sampling was undertaken with known community leaders and healthcare workers/managers employed within the local health district. For those who consented to be interviewed face to face, semistructured interviews were undertaken to ascertain their perspective on vaccine hesitancy in their community. The survey was used as a point of discussion during the interviews to explore their perspective in greater detail.
Setting
The study was set in New Ireland Province, PNG. Participants were recruited from both urban and remote locations within the province. New Ireland is divided into two districts, Kavieng and Namatanai, with New Hanover (also known as Lavongai) located in a remote region 40 km west of Kavieng. Its diverse geography includes beaches, islands, coastal lowlands, mountains and inland plateaus. New Ireland province is spread over 9600 km2 of land and 230 000 km2 of sea12. The population is approximately 243 035; 32% are in paid employment and 68% live a subsistence lifestyle, selling local produce at local markets12. Most rural communities lack power and running water, although sanitation and clean piped water are available in main towns. Immunisation programs are usually provided through hospital outpatients, rural health centres, scheduled outreach community site visits, and urban clinics.
Data analysis
Paper-based surveys were distributed to participants to complete. Survey responses were then scanned and digitised, and the data were manually entered into Statistical Package for Social Sciences (SPSS) v27.0 (IBM Corp; https://www.ibm.com/products/spss-statistics). Survey responses were analysed using SPSS. Summary descriptive statistics are presented as frequency distributions and percentages in table form. Both parametric and non-parametric methods were considered to analyse these data. Interviews were transcribed by the researchers manually and thematically analysed using the six phases of qualitative analysis recommended by Braun and Clarke13. Participants were given the opportunity to review the notes taken at the interview stage (member checking), to enable them to add or delete information. However, they were unable to review the transcript itself as this could only be achieved at a later date due to the remoteness of the location and lack of IT resources available. Themes were coded by the research team and checked independently by a team member who was not present for the interview, to ensure accuracy.
Ethics approval
This research was approved by the Acting Chief Executive Officer of the Kavieng Hospital; ethics approval was granted by the HML IRB Research and Ethics (HML IRB Review 449PNGO21), and PNG government approval to conduct research was granted by the PNG Institute of Medical Research (MRAC 21.18).
Results
Survey
The sample included 181 participants; to gain responses from both urban and remote areas, participants were located in Kavieng (133) and New Hanover (48). The largest proportion of participants (41.2%) identified as community member (CM), 21.0% as community leader (CL), 8.3% as healthcare worker (HCW) and 7.2% as community health volunteer (CHV); 22.3% did not nominate an answer.
Figure 1 provides a descriptive summary of responses to the adapted vaccine hesitancy scale. All participants surveyed were over the age of 18 years; 37% were female and 63% were male. The age of each participant was not used in the analysis because some participants were unable to state their exact age.
Overall, the cohort had a high level of awareness of the COVID-19 vaccine, with 86.7% of participants indicating they had heard of the vaccine. The most common sources of vaccine information were identified as health workers (33.7%) and social media (14.4%), and 13.8% of participants cited multiple sources. Despite the high level of vaccine awareness and availability in the province, only 7.2% of participants indicated they had received a dose of a COVID-19 vaccine. When asked if they would get the vaccine should it be available to them, just 27.6% of participants answered ‘yes’. Study participants were also unlikely to encourage friends and family to get the vaccine, with only 35.9% indicating they would be happy to do so.
There was a reasonable degree of uncertainty about the authenticity of the COVID-19 virus, with 36.5% of participants saying they were uncertain whether the virus was a hoax. In addition to the uncertainty, 27.6% of participants agreed to some extent that the virus was a hoax. Moreover, 37.6% of participants agreed to some extent that the virus was manmade, and a further 33.1% of participants were unsure. Only 21.0% of participants disagreed outright that the virus was manmade.
There were also concerns about the origins of the virus and its spread, with 48.1% of participants agreeing to some extent that the spread of the virus was deliberate. CLs were more likely than CMs to think the virus was spread deliberately (52.6% CL v 37.0% CM). There was a similar pattern of response to the statement ‘companies have created the virus to make money’, with 32.0% of participants indicating some agreement. Again, agreement with this statement was more frequent among CLs than CMs (42.1% CL v 33.0% CM). Further to this, only 35.9% of participants disagreed that COVID-19 was created to ‘force vaccination’. Mistrust of government advice was another key theme identified, with 42.5% of participants agreeing to some extent that they do not trust the government’s vaccine advice. This mistrust was also higher in the CL cohort (55.3% CL v 42.5% CM).
The study unearthed concerns about the safety of the vaccine, with 26.5% of participants agreeing to some extent that PNG people were being deceived about vaccine safety. In addition to this, 33.7% of participants agreed to some extent that the vaccine may cause health problems in the future, and only 26.5% of participants disagreed with the statement that ‘The vaccine will make me sick’. CLs were more likely than CMs to agree that the COVID-19 vaccination would make them sick (42.2% CL v 30.4% CM).
The results of the survey also revealed a heavy belief that religion and faith will provide protection from COVID-19. Of all respondents, 69.1% agreed to some extent that faith would protect them from the virus. There were also similar responses to the level of protection the environment provides against COVID-19, with 47% of participants agreeing that the temperature in PNG would protect them from the virus.
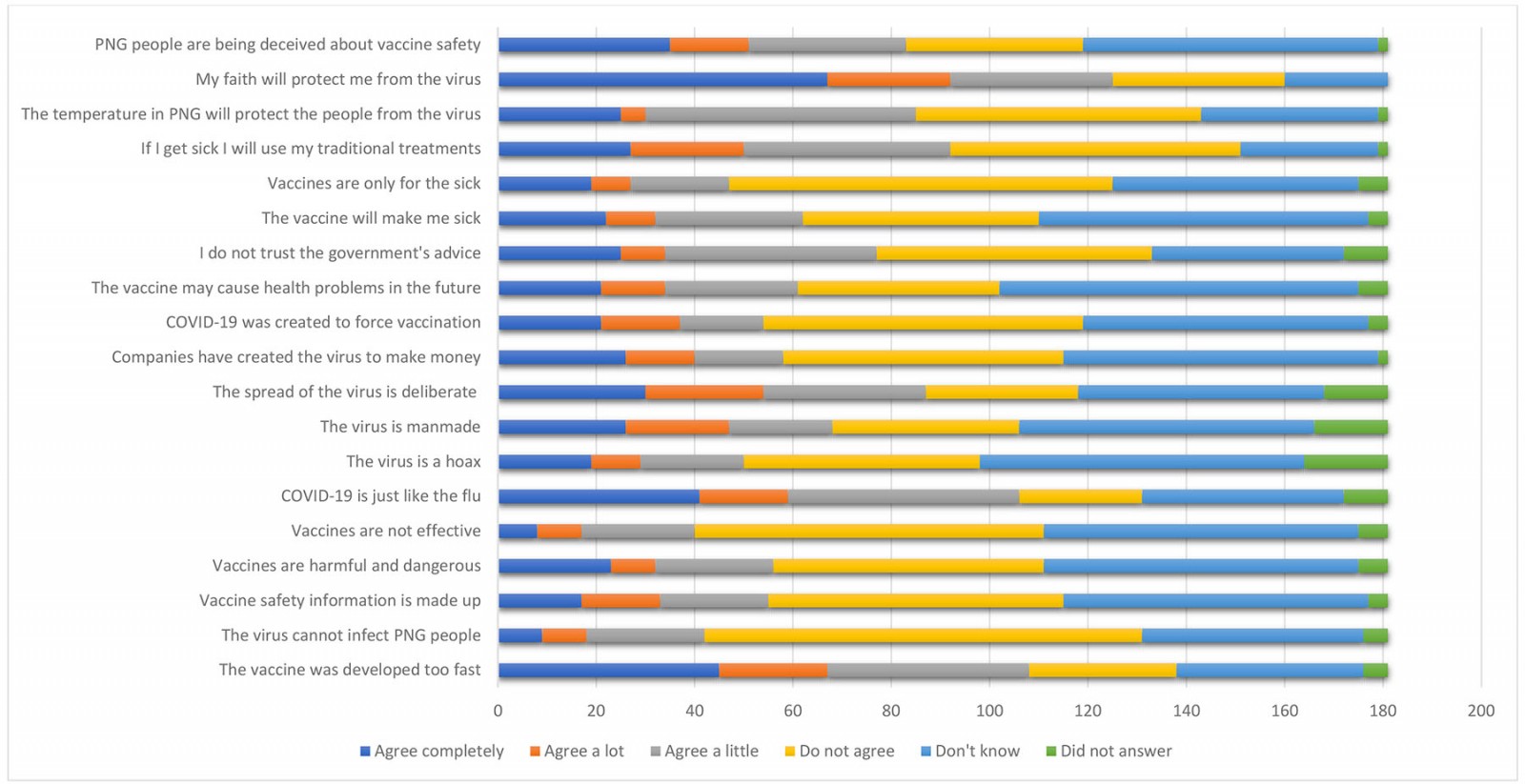 Figure 1: Overview of vaccine hesitancy survey responses.
Figure 1: Overview of vaccine hesitancy survey responses.
Structured interviews
To explore the perspective of CLs and HCWs within the community, 19 participants agreed to be interviewed. The participant role in the community was either a healthcare manager (2), HCW (7) or CL (10). CLs comprised religious leaders and local business managers. Saturation of themes was achieved after 19 interviews. The following themes were identified.
Religious beliefs
Many healthcare facilities are run by the Church; therefore, they are a source of trusted information because they are considered a fundamental part of the local community. The survey results revealed that 14.3% of participants received COVID-19 vaccine information from their religious leader.
While some participants agreed that representation from the church leaders was a positive step to promote vaccination rates, others doubted the motives of the PNGCC, stating that ‘It is a shame that the man himself [Cardinal Sir John Ribat] also believes in this’ (CL2). Others questioned the Church’s agenda for promoting vaccinations, stating that church leaders have ‘lost their faith’ and that ‘there are no more true church leaders, only businessmen’ (CL3) with a financial or political agenda.
Community representatives and HCWs agreed that the messages from provincial church clergy were often not consistent with messages from the leaders of the church. Participants indicated that many provincial clergy were not actively advocating for the vaccine to parishioners, nor were they attempting to dispel misinformation about the relationship between COVID-19 and the Bible. An example of this was the expressed belief that COVID-19 is a punishment from God, or that people of the Christian faith are immune to COVID-19. A local pastor (CL6) defended this by stating, ‘The vaccine education has not been given to the local ministers … they can’t answer questions’. However, participants agreed that the misinformation was effectively promoted by many provincial clergy. A participant (CL9) stated after participating in a community vaccine advocacy session, ‘They [pointing at the church] tell us wrong things, they say COVID is not real, and vaccines make us sick’. Healthcare staff administering the community vaccine advocacy sessions concurred, stating that even during their presentations to the community, which included video statements from the PNGCC, they had been challenged by local clergy in front of community members about vaccine safety and the relationship between COVID-19 and the Bible’s prophecies.
Misinformation concerning the relationship between religion and the COVID-19 vaccine according to participants is also spread by social media and word of mouth in more rural areas. While partaking in vaccine advocacy campaigns, participants recalled comments from patients, such as, ‘COVID vaccines implant a chip with 666’ (HCW1). When asked to explain the meaning of this statement, the participant indicated that this was a reference to Satan, further stating that members of her community believe that ‘If you receive the vaccine, other community members will know whether you are on Satan's or Jesus’ side’.
Other participants commented that within their communities there is a belief that God will offer protection from the disease. A CL stated that for some there is a belief that ‘God will protect PNG people; it is a white man’s disease’ (CL1). They stated that this is driven by online comments that suggest ‘God is the creator, and he is the one to protect our country … not vaccination’ (CL1).
Political messages
Participants stated that the divide between the central PNG government and provincial governments in communication and messaging increases the challenge of managing COVID-19. Participants referred to social media posts from government officials that provided conflicting information, causing them to underestimate the impact COVID-19 would have on the community and doubt the need for vaccination. It was observed by the researchers that during community vaccine advocacy campaigns, speeches from government officials were played over loudspeaker to counter the vaccine advocacy message. Participants agreed that these messages did not encourage trust in the vaccine. They stated that comments such as PNG people are being offered up as ‘lab rats or guinea pigs for testing of the vaccine’ and that ‘there may be underlying reasons for the apparent natural resistance to Corona virus so far by Papua New Guineans’ were not helpful. According to CLs and healthcare managers, it is this type of misinformation that fuels vaccine hesitancy. The rhetoric of being ‘offered up as guinea pigs’ for the vaccine was a strong sentiment observed during community vaccine advocacy presentations.
Social media influence
Participants agreed that although social media is not widely available in the provincial rural and remote communities, it still contributed to misinformation surrounding COVID-19 vaccines. In the provinces, mobile phones come loaded with Facebook as part of affordable prepaid data plans. Facebook is a well-known platform for antivaccination comments. Often the misinformation stems from user comments to a primary post providing health advice. However, most people cannot afford to pay for internet browsing and information literacy is poor; therefore, fact-checking information provided on social media is almost non-existent.
Participants indicated that even though social media may not be prevalent in small communities, antivaccination information was widely available via WhatsApp, with the sending of video links that discouraged vaccination in large community platforms. The participants stated that ‘conspiracy theories on these platforms are spreading faster than COVID-19 itself’ (CL8). Participants recalled comments that they had read on social media, such as ‘COVID-19 is an invention of the West to control population’, that ‘Papua New Guineans are guinea pigs for vaccines’ and that ‘God is protecting Melanesians from catching the disease’.
Community/family beliefs
When discussing the vaccine itself, participants expressed anxiety over three specific areas:
- the short timeframe for the vaccine’s development and approval by PNG-based regulatory groups
- vaccine safety, specifically a belief that it may cause infertility or death
- the actual ingredients of the vaccine and how it interacted with the body, such as its ability to change a person’s DNA, or that it contained parts of the virus that would make a well person sick.
In addition, a fear of being excluded from the family or their community for getting the vaccine was a concern expressed by some participants. A participant (HCW4) stated that ‘she would be forced by relatives to leave the family home if she received the vaccine’. Similarly, another participant (HCW6) stated that his wife told him he would have to ‘leave the family home if he was vaccinated’; he stated his wife was also concerned about how she would ‘pay for my funeral’, given the belief that the vaccine would cause a person to die.
Some female HCWs and CMs stated their inability to receive the vaccine due to pressure from their husbands. This is directly related to the belief that the vaccine caused infertility. One participant (HCW4) explained that in her community if a woman was unable to bear children, it would be a poor reflection on the husband’s masculinity, therefore increasing gender-based violence in the home. The participants stated that the belief that vaccines cause infertility also resulted in young female members of the community resisting vaccination as they feared it would affect their ability to conceive in the future.
Fear of death from the vaccine in many developed countries is directly related to fear around adverse reactions to the vaccine or the specific rare clotting issues, thrombosis with thrombocytopenia syndrome, reported in mainly young AstraZeneca recipients14. In New Ireland Province, the concern of thrombosis with thrombocytopenia syndrome was not widely discussed. Only one participant commented that members of the community had discussed the clotting threat of AstraZeneca from Australian media sites. In New Ireland Province, participants stated that there was a fear in the community of the vaccine causing death but few reasons as to why death may occur. A participant (HCW5) stated ‘the patients believe that if you have the vaccine you will die at 2 years’. This belief was quite common among community members but with little explanation as to why or how death would occur. Four participants commented that it is because ‘people think that the vaccine will change their DNA, then they will not be able to fight other diseases’ (CL4).
Misunderstanding new terminology
The adult literacy rate in PNG is reported to be 63.4%15; poor literacy skills and the inability to fact-check information may be contributing to a lack of understanding and the misinformation circulating in the community. Participants expressed some confusion over new terminology that is being used when discussing various aspects of COVID-19 and the vaccine. A participant (HCW5) recounted how a patient had attended the hospital concerned over the number of new viruses being discussed in the media. The nurse stated that the patient believed that ‘Corona virus’, ‘COVID-19’ and ‘isolation’ were new and separate diseases.
The provision of consent to receive the vaccine was also a source of confusion. Adult vaccination is new to many PNG people; therefore, discussing vaccine risk to provide informed consent and signing a consent form to receive the vaccine was generating hesitancy. A participant (CL9) stated ‘if they sign consent, are they giving up their ability to take action if they have a reaction?’.
The term ‘isolation’ was also a source of concern for some community members. HCWs stated that not understanding ‘isolation’ and ‘self-isolation’ meant that symptomatic community members would often not present for testing for fear of being required to isolate. Furthermore, those positive patients who were isolating at home with mild symptoms carried on with life as normal due to a lack of understanding about how the virus is spread. A participant (HCW7) stated that ‘The word 'isolation' is being confused with being locked up, therefore sick people won’t present for testing in case they test positive’. Many people in PNG live in multi-generational households, with grandparents, children, grandchildren and other relatives living together under one roof. The ability to isolate is nearly impossible for many patients.
Disregard for virus
HCWs and CLs agreed that many community members had a disregard for COVID-19 and were quite dismissive of the urgency surrounding new, more transmissible variants. Although healthcare staff expressed concern over the community’s complacency, they stated that in many ways COVID-19 was seen as ‘just another sickness’ (HCW6). This fatalistic acceptance was also observed during vaccine advocacy campaigns as community members expressed anger over the urgency surrounding COVID-19 when illnesses such as malaria, HIV and tuberculosis had caused suffering for many years. The dismissive nature expressed by the public indicated either a convergence with the belief that this was ‘God’s plan, he will take me when its time, no matter if its tuberculosis or some other disease’ (CL7), or anger expressed over the number of resources being directed at COVID-19 when other illnesses are yet to receive the same attention. Participants stated there had been contempt expressed from the community for Western countries introducing COVID-19 into an already under-resourced PNG. Leaders stated that this followed a long history of a lack of investment in provincial healthcare services, mistrust in leadership and many years of resentment over the divide in wealth equality, governance and transparency.
Discussion
On 9 March 2021, the government of PNG granted approval for 588 000 doses of AstraZeneca from Australia to be distributed across PNG. In addition to the doses already donated by Australia, the Chinese government pledged 200 000 doses of the Sinopharm vaccine to PNG. According to the World Health Organization16, the target was to have 20% of the population vaccinated by 2021 and 30% by 2022. Although the COVID-19 vaccine has been available since May 2021, only 3.5% of the population in PNG are fully vaccinated16,17. This project aimed to highlight the reasons behind vaccine hesitancy in New Ireland, PNG.
The responses indicate that participants have been influenced by misinformation, and they are also somewhat sceptical of the information received. Many survey participants were split on the legitimacy of the virus, with many outright agreeing that it was a hoax. In addition to this, an even greater number were unsure, meaning that just over a quarter of participants thought the virus was real. Factors contributing to this are probably multifaceted; however, it is well documented that social media can be a significant source of extensive misinformation on all topics, including COVID-1918. This type of misinformation can be harmful to population health, as people may not take appropriate precautions for the virus or may even utilise inappropriate and potentially harmful interventions. Misinformation may also dissuade people from taking a risk-averse approach, where public health recommendations such as social distancing and mask-wearing may not be adhered to, potentially resulting in increased virus spread19. A lack of acceptance of COVID-19 as being both real and a significant public health concern is likely to be a significant barrier to increasing vaccination uptake.
Across many items, a reasonable number of participants chose to provide a ‘Don’t know’ response. This may reflect the limited number of vaccine advocacy activities to educate community members, but more positively suggests the ability to influence people’s perception of vaccines with future campaigns. Additionally, participants frequently chose an ‘Agree a little’ response, particularly to questions that reflected the general misinformation that is circulating on social media. This could suggest that although participants were aware of misinformation such as ‘the temperature in PNG will protect people from the virus’, they remained cautious about whether they completely believed it.
Across all provinces, the acceleration of community engagement activities that coincide with mobile vaccination clinics in neighbouring provinces has resulted in an increase in vaccine uptake; however, this has come at a cost to staff safety. West New Britain Province, for example, reported an increase in vaccine uptake but also an increase in violence towards healthcare staff undertaking vaccine advocacy campaigns20. This aggressive response to vaccine advocacy was also witnessed by researchers in New Ireland Province. As New Ireland Province continues to ramp up COVID-19 vaccine advocacy campaigns despite the risk to staff safety, other provinces such as West New Britain are finding that minimising the approach and treating COVID-19 just like any other public health campaign may work best for their community. This decision has also been made due to a concern over other public health campaigns being neglected as well as community criticism over COVID-19 resourcing.
In New Ireland, the delivery of vaccine advocacy is hampered by certain barriers. Staff report that although the vaccine advocacy campaigns are planned to increase, staff availability, financial resourcing, and appropriate planning and leadership have limited the number of community advocacy presentations. According to staff, there is also resistance to mobilising the vaccine clinic in addition to the fixed site at the hospital due to a lack of appropriately trained staff and concern for cold chain maintenance.
Limitations
The research team’s ability to conduct additional face-to-face semistructured interviews was limited by travel restrictions in certain geographical areas due to the COVID-19 pandemic. The in-field research team followed World Health Organization public health guidance, including using face masks and hand sanitiser and practising social distancing, while undertaking qualitative interviews in the field. During the data collection phase, various sites were quarantined due to COVID-19 outbreaks among healthcare staff; this limited the availability of data. In addition, some geographic locations were not accessible due to violence and community unrest. These areas were avoided to maintain staff safety; however, this limited the geographical reach of the study.
The authors acknowledge that undertaking research in communities that rely on international aid to maintain health programs may be conflicted by positionality, reflexivity and power relations in research. An example of this may include participants answering questions to maintain services or attract additional resources. Participants were informed that they would not receive any direct benefits for participating; however, their contributions to the conversation/discussion would inform future improvements for health programs being conducted within their community. As a research team, we were fully cognisant of one’s epistemology, appropriate research boundaries, participant marginalisation, and research relationships and their power differentials21. This was managed by the utilisation of local public health nurses known to the community who assisted in recruitment.
Conclusion
In New Ireland Province, as in many other rural provinces, the lack of preparedness for a rise in COVID-19-positive cases and a lack of community engagement with vaccine initiatives at this stage in the pandemic is concerning. Although the provincial health authorities are raising awareness about COVID-19 and offering vaccines, the messages to address vaccine hesitancy concerns have affected early vaccine uptake and have become ingrained in the community. Misinformation can be harmful to public health initiatives such as vaccination campaigns. Social media plays a significant part in the distribution of misinformation, which contributes to lower levels of vaccine uptake. The PNG government, provincial health authorities, and non-government organisations are endeavouring to correct misinformation disseminated on social media and other forms of communication. However, the government admits that they have previously been complacent about the impact COVID-19 would have on the country. Misinformation from all sources needs to be addressed to contribute to the increase of vaccination levels in PNG.
Acknowledgements
We would like to acknowledge the New Ireland Provincial Health Authority and the management and staff of the Kavieng Hospital for their support and involvement in this project.
Funding details
This article represents independent research funded by UNICEF. This work was supported by HPD ADI 29.06.21-JB.
Conflict of interest
The authors declare no conflict of interest.
Data availability
The data that support the findings of this study are available on request from the corresponding author (BF). The data are not publicly available because they contain information that could compromise the privacy of research participants.
References
You might also be interested in:
2020 - The 'Snake song': a pilot study of musical intervention in Eswatini
2012 - Rural older adults' mental health: status and challenges in care delivery



