Introduction
Brazil is a country of continental dimensions and with marked social and health inequalities. The North and Northeast macro-regions represent the lowest income segments and the worst health indicators in the country1,2, and, in general, more disadvantaged scenarios are observed in populations living in rural areas2,3. Given this context, rural riverside populations in the Amazon are characterized by daily life related to the dynamics of the rivers, giving a peculiarity to their way of life, and whose economic activity is strictly linked to fishing and plant extraction4. Despite the marked socioeconomic and health vulnerability, as well as the difficulties in regular access to health services5, evidence regarding the lifestyle and health conditions of these populations is still limited.
In this context, non-communicable chronic diseases are the main global cause of death and represent one of the main public health problems in recent decades6, with impacts that permeate the occurrence of premature deaths, the appearance of disabilities, reduction in life expectancy and in the workforce, in addition to high costs for the health system and for society7. The percentage of premature deaths caused by these diseases is higher in low- and middle-income countries8, such as Brazil, demonstrating that the burden of these diseases falls, notably, on populations with greater social vulnerability.
Among chronic diseases, systemic arterial hypertension (SAH) and diabetes mellitus (DM) are highly prevalent in the adult population and are major threats to global health, and, according to WHO, are among the five main global risks factors for mortality in the world9. According to the most recent Brazilian National Health Survey (2019), the self-reported prevalences of SAH and DM were 23.9% and 7.7%, respectively10. These diseases share numerous risk factors and underlying pathophysiological mechanisms, the most important of which are insulin resistance and inappropriate activation of the renin–angiotensin–aldosterone system11. It is known that chronic diseases can occur in isolation or coexist in the same individual. Especially when associated, SAH and DM are relevant causes of morbidity and mortality, increasing the risk of cardiovascular diseases12.
Knowledge of the distribution of chronic diseases in vulnerable and neglected populations is essential for planning, organizing health services, and health policies. By considering the rapid demographic and epidemiological transition, the impact of isolated and coexisting chronic diseases on health, the high care costs, and the scarcity of data on the evaluation of one or more chronic diseases in rural populations along the riverside of the Amazon, Brazil, as well as public health policies focused on their specificities, this study aimed to estimate the prevalence of SAH or DM and their concomitant occurrence, and its association with sociodemographic characteristics, lifestyle habits, and access to health services.
Methods
Study design
The present study is part of a household-based cross-sectional survey conducted with a representative sample of residents from 38 rural riverside locations along the left bank of the Negro River, in the municipality of Manaus, Amazonas, Brazil.
Area and study population
The study was carried out on the river stretch from the left bank of the Negro River, municipality of Manaus (2 182 763 inhabitants) to the border with the municipality of Novo Airão (19 454 inhabitants)13. All 38 rural riverside locations studied are accessible only by river, and the boat trip from the urban area of Manaus to the last communities takes approximately 10 hours, depending on engine power and water level. Some dwellings are located far away (10–30 minutes by canoe) from the headquarters of the community to which they belong. The evaluated communities are in environmental protection areas, and a large part of this population essentially lives from activities related to fishing, agriculture, and plant extractivism, as well as social benefits. Regarding access to health services, the locations belong to the territory of a fluvial family health team of the Municipal Health Department of Manaus, which provides health care through monthly trips in a mobile fluvial health unit. The community health workers are the only team of professionals living in the territory. The organization of health care in the territory has been previously described5.
Sample size calculation
Of the communities in the study area, six were excluded because they were Indigenous communities and, consequently, considered under another healthcare model (the Brazilian Indigenous Health Subsystem). Thus, 38 rural riverside locations belonging to 21 communities were part of the study. Information on the population residing in the territory was obtained from the Rural Sanitary District of Manaus, which is responsible for the fluvial family health team in the area (excluding Indigenous lands). In June 2018, 2342 people lived in 765 households in the area covered by the study. Stratified random sampling was carried out proportional to the number of residents in each location, and the calculation of the sample size considered the probability of having an adult or elderly person in the selected households, as well as the estimated prevalence of 50% of the outcomes of interest and accuracy of 95%. The sample size was increased by 10% to compensate for possible losses or refusals.
For the selection of households, the community health agents prepared detailed maps with the location of the households. From the number of households selected in each location, estimated through the probability of finding the residents of interest, the sample fraction was calculated, dividing the total number of households in the location by the number of households sampled. The value obtained defined the sampling interval for the systematic random selection of households, following the natural order along the course of the river, or the analogous organization of blocks and faces in larger clusters. The first household to be evaluated in each area was drawn by using a table or a random number generator program. The same strategy was used in the selection of the resident from each interest group (adult man, adult woman, elderly man, elderly woman), when there was more than one individual in that group within the same household. Therefore, the random draw of an adult or elderly person of each gender in the selected households corresponded to the second stage of sample selection. In this way, randomness was ensured in the two stages of selection. Thus, 287 (37.5%) of the 765 households were visited and 495 adults and elderly people were interviewed in households with residents in the age range of interest in the research.
Data collection
Data collection was carried out from 19 March to 30 May 2019, by 19 previously trained researchers. The training included theoretical content and simulations of interviews between members of the collection team, followed by a pilot study carried out in two of the municipality’s rural areas not involved in the survey.
The questionnaire was structured in thematic notebooks, referring to socioeconomic and household characteristics, lifestyle habits and health conditions, as well as the use of and access to health services. It is noteworthy that the questionnaire contained some questions pertaining to the family, including household individuals not included in the sample. The questionnaire, developed in the Research Electronic Data Capture (REDCap) application (https://www.project-redcap.org), was applied directly to the selected resident in the home environment by smartphones and tablets. If any of the selected residents were absent, new attempts were made in different shifts and times to locate the resident in the household.
The occurrence of chronic diseases (SAH and DM) was verified by self-report of medical diagnosis through the question ‘Has any doctor ever told you that you have SAH/DM?' The self-reported criterion has also been used previously in Brazilian surveys, such as the National Health Survey14 and Vigitel Survey15. Two dependent variables were considered in the present study: occurrence of at least one chronic disease (yes/no) and concomitant occurrence of SAH and DM (yes/no), defined as at least one and two positive responses to both of these questions, respectively.
The independent variables considered for this study were: sex (male and female); age (years, age group: 18–39, young adult; 40–59, middle age; and ≥60, elderly); self-reported skin color (White, Black, Brown or Indigenous); education (never attended school, elementary school, and high school/college); household monthly income (reais: <1 × minimum wage and ≥1 × minimum wage); occupation (domestic activities/student/unemployed, employed/self-employed/public servant, and retired); social benefits received by a resident of the household (no and yes); housing characterization (predominant floor material (earthen floor/wood and cement/ceramic), wall (straw/rammed earth/clay/canvas/plastic/brick and wood) and roof (wood/straw/canvas/plastic and zinc/asbestos/clay tile)); origin of the drinking water (artesian well, river/lake/rain/shallow well, and protected source/local network); water tap that works indoors (no and yes); electricity at home (no, yes/discontinuous, and yes/regular); smoking (never smoked/ex-smoker and current smoker); monthly purchase of beverages for consumption at home (soft drinks (liters) and alcoholic beverages (liters)); fishing for consumption (frequent, infrequent, and never); vegetable garden (no and yes); hunting in the forest (no and yes); medical/dental health plan (no and yes); health services used (pharmacy/home care, public healthcare service, and private healthcare service); travel time to the nearest health service in minutes (average between periods of drought and flood of rivers); and health self-assessment (good/very good, fair, and poor/very poor).
The absolute and relative frequencies of the independent variables were calculated according to the presence of SAH or DM (yes/no) and SAH and DM concomitantly (yes/no). The Kolmogorov–Smirnov test was performed to assess the normality of continuous quantitative variables and statistical tests were conducted respecting the sample design. Bivariate analyses (χ2 test/Fisher’s exact test and Student's t-test/Mann–Whitney U-test) were performed to verify association between outcomes and independent variables. Variables with a p≤0.10 in the bivariate analysis were included in the multivariate Poisson regression analysis with robust variance to estimate the prevalence ratio (PR) and 95% confidence interval (CI). In the adjusted model, variables with p≤0.10 were kept in the models. The final significance level adopted was 5% for all analyses.
Ethics approval
Data collection respected the ethical precepts set out in Resolution 466/2012 of the National Health Council. Consent was obtained from the Manaus Municipal Health Department and the research project was submitted to the Research Ethics Committee of the Fundação de Medicina Tropical Doutor Heitor Vieira Dourado, having been approved under Certificate of Ethical Appreciation 57706316.9.0000.0005. Participants who agreed to participate in the study signed the free and informed consent form.
Results
In the present study, 495 residents were investigated (young adult (n=257; 51.9%), middle age (n=132; 26.7%), and elderly (n=106; 21.4%)), with 51.5% (n=255) being women. Mean age and monthly household income were 43.3±17.1 years and R$1100±902 (A$345±283), respectively. Regarding the housing characterization, earthen/wooden floors, wood, and tile (zinc/asbestos/clay) represented, respectively, the predominant floor, wall, and roof materials in most homes. Almost 10% of the households did not have electricity at home, about 60% of the families used drinking water from an artesian well, and 51.5% had at least one functioning water tap inside the residence. About 70% of the families used sodium hypochlorite to treat drinking water and almost 76% reported burning or burying waste produced in their homes in the community (data not shown in tables).
About 17% (n=86) and 6% (n=29) self-reported a medical diagnosis of SAH and DM, respectively. The occurrence of at least one chronic disease was observed in 18.8% (n=93), and concomitant SAH and DM in 4.4% (n=22) of the sample. Despite their knowledge about the medical diagnosis, it was observed that about 8% and 31% did not use antihypertensive and hypoglycemic medications, respectively. The occurrence of the chronic diseases according to sex and age group is presented in Table 1. A higher frequency of chronic diseases was observed in the elderly than in adults, and there was a lower percentage of women than men with reports of moderate/intense limitation of usual daily activities due to SAH.
In the bivariate analyses (Tables 2 and 3), sociodemographic data, lifestyle habits, and health self-assessment were associated with the occurrence of the assessed outcomes. The occurrence of at least one chronic disease, as well as the presence of concomitant SAH and DM, was observed in greater proportion among individuals with higher household monthly income and lower education, and among retirees, compared to individuals not affected by these diseases. In addition, monthly purchase of soft drinks at home, fishing habits, hunting in the forest (except for occurrence of concomitant SAH and DM), and health self-assessment were associated with the occurrence of chronic diseases.
After the Poisson regression analysis, it was identified that, in the adjusted model, higher average age (PR=1.1, 95%CI 1.0–1.1), lower average monthly household purchase of soft drinks for consumption at home (PR=0.9, 95%CI 0.8–0.9), and worse health self-assessment (fair: PR=2.0, 95%CI 1.3–3.2; poor/very poor: PR=2.3, 95%CI 1.3–3.7) significantly increased the likelihood of having at least one of the chronic diseases. Regarding occurrence of concomitant SAH and DM, in the adjusted model, an association was observed with higher average age (PR=1.1, 95%CI 1.0–1.1), lower average purchase of soft drinks for consumption at home (PR=0.7, 95%CI 0.5–0.9), and worse health self-assessment (fair: PR=3.6, 95%CI 1.1–12.0; poor/very poor: PR=3.7, 95%CI 1.0–14.6) (Table 4).
Table 1: Occurrence of chronic diseases according to sex and age group in a rural riverside population, Manaus, Amazonas, Brazil, 2019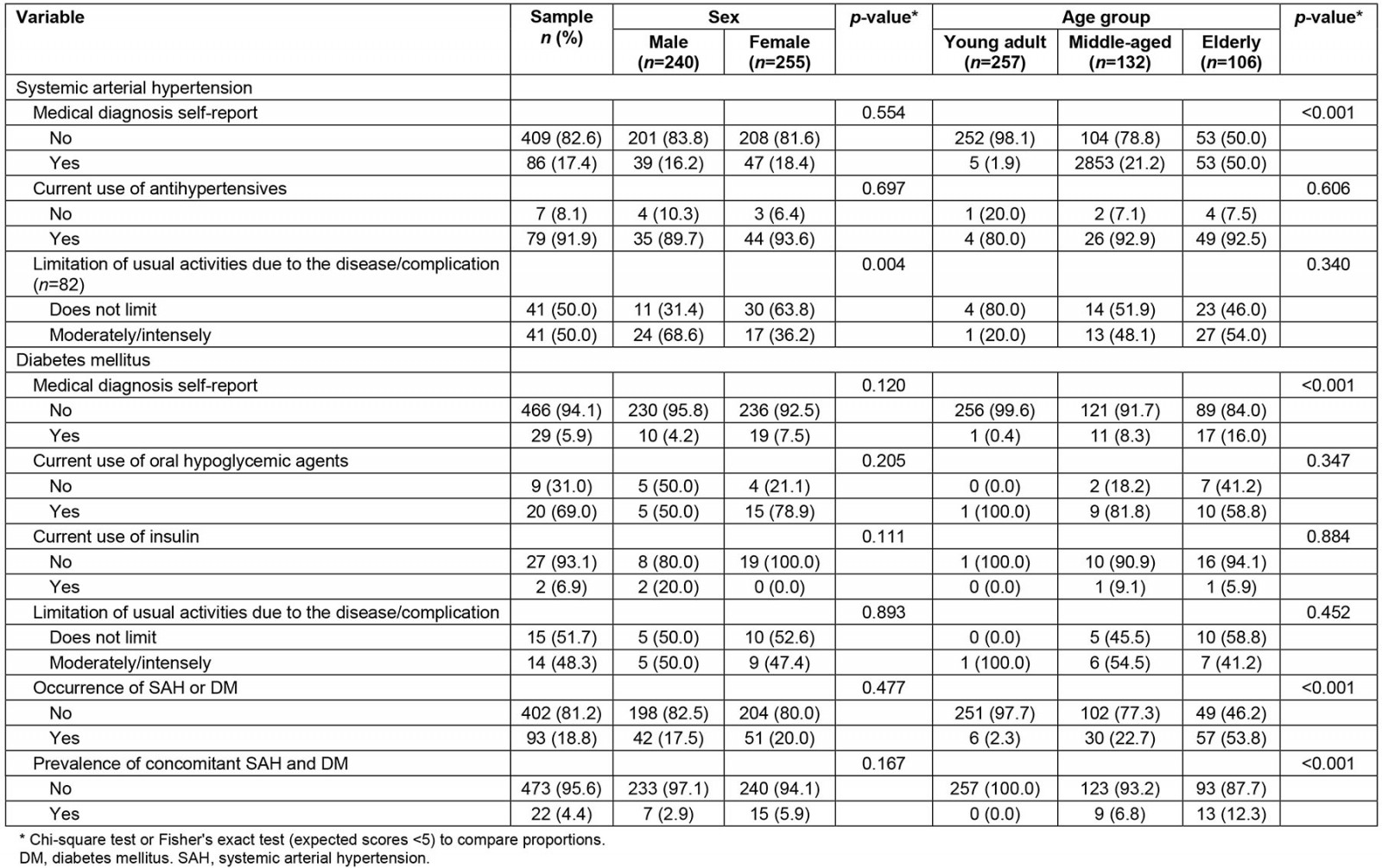
Table 2: Sociodemographic characteristics according to the occurrence of chronic diseases in a rural riverside population, Manaus, Amazonas, Brazil, 2019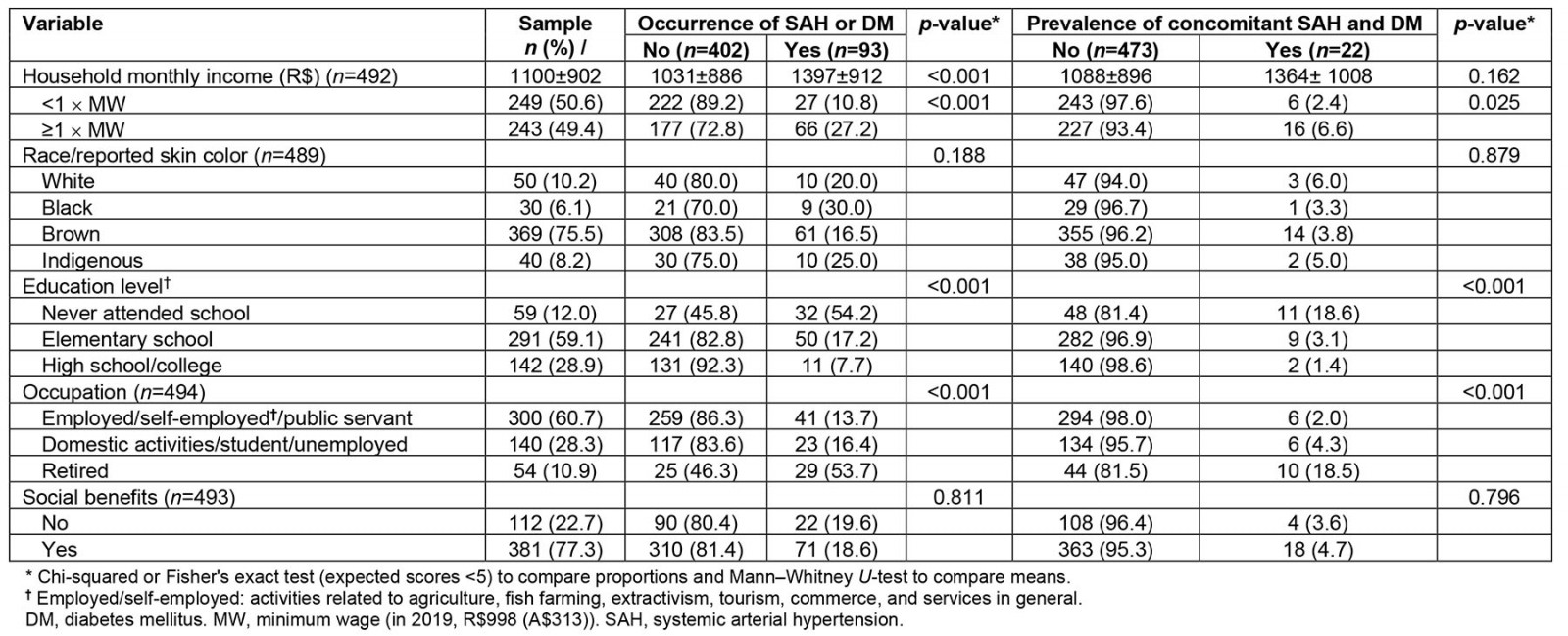
Table 3: Characterization of the sample according to lifestyle, food context, access to health services, and health self-assessment with respect to the occurrence of chronic diseases in a rural riverside population, Manaus, Amazonas, Brazil, 2019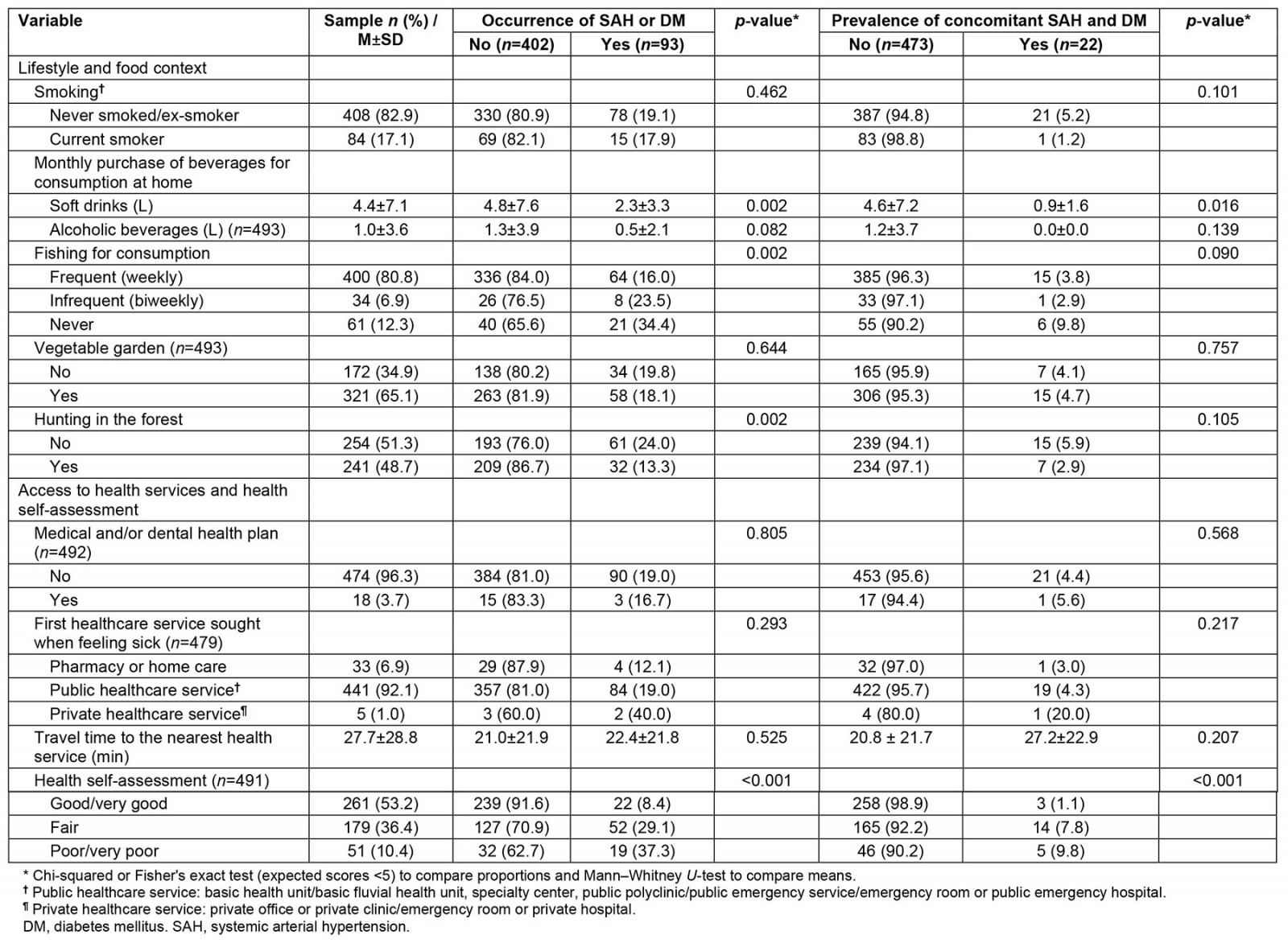
Table 4: Association† between the occurrence of chronic diseases and sociodemographic, behavioral variables and health self-assessment in a rural riverside population, Manaus, Amazonas, Brazil, 2019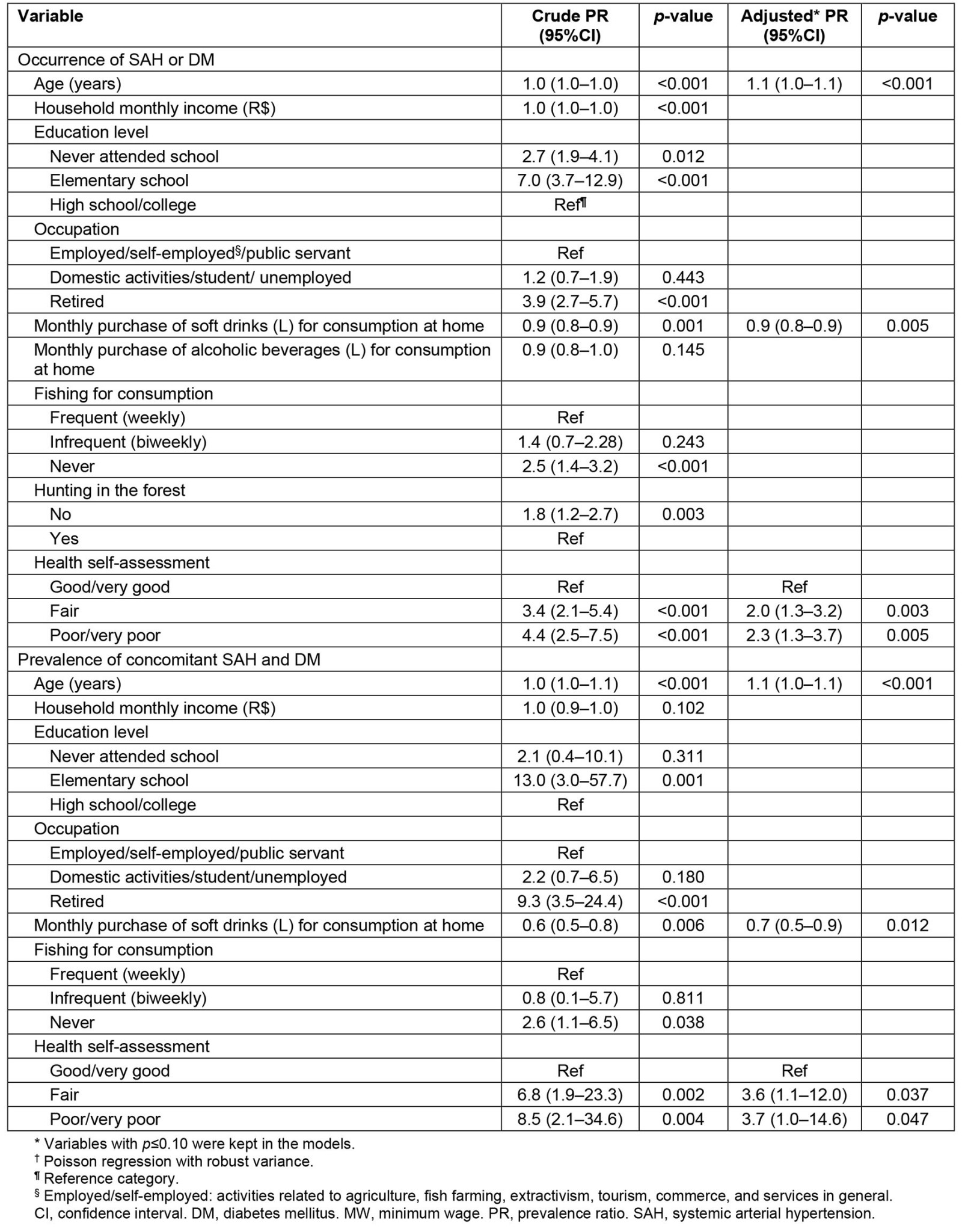
Discussion
The occurrence of at least one of the chronic diseases was found in 18.8% of the sample, with a high prevalence of self-reported medical diagnosis of SAH (17.4%). The occurrence of SAH or DM was associated with higher average age, lower average monthly household purchases of soft drinks for consumption at home, and worse health self-assessment. Regarding prevalence of concomitant SAH and DM, identified in 4.4% of the sample, the same associations were observed.
SAH was the most frequent (17.4%) of the two chronic diseases analyzed. The prevalence of medical diagnosis of this clinical condition for the adult Brazilian population according to the most recent National Health Survey10 was 23.9%, being lower in the North region (16.8%), corroborating the findings of the study. Other national epidemiological studies carried out with populations from the Southeast and South regions of the country also showed a higher occurrence of SAH among the evaluated chronic diseases, although with higher estimates16,17. An investigation carried out with individuals from Porto Velho (n=1410 individuals, 35–80 years), capital of the state of Rondônia, North region of Brazil, observed a prevalence of SAH (self-reported and/or blood pressure ≥140/90 mmHg and/or use of antihypertensive medication) in 53.19%, higher in urban areas (55.48%) than in rural riverside areas (48.87%)18. The highest mean age and the highest number of criteria for classifying this clinical condition seem to explain the highest estimate of SAH when compared to our study. In the present study, approximately 9% of the sample that was aware of their SAH did not use medication, with a higher percentage observed by Almeida et al18 when analyzing data from the rural riverside population of another municipality in the north of the country, demonstrating that public health actions are necessary to improve the prevention and treatment of SAH and, consequently, prevent comorbidities.
The prevalence of self-reported medical diagnosis of DM in this study was around 6%, slightly below the national average among Brazilian adults observed in the National Health Survey (7.7%), but close to the average evidenced for the North region of the country (5.5%), probably because it has a younger population than the other regions10. A cross-sectional study carried out in rural communities in municipalities in the state of Goiás (13 riverside communities, 51 quilombolas (Afro-Brazilian residents of rural communities formed by descendants of Afro-American slaves), and 63 agrarian reform settlements), Central-West region of Brazil, showed a general prevalence of self-reported diabetes of 9.8% (13.5% in riverside dwellers, 10.0% in quilombolas, and 9.3% in agrarian reform settlers)19. The higher mean age of the sample (51.6 years) may explain the higher prevalence of the disease than in the present study. A cross-sectional study with a sample of 191 adults from different ethnic groups (Sateré-Mawé Indigenous, Indigenous from the Negro River, Brown/Black and White) living in the city of Manaus, North region of Brazil, found a general prevalence of impaired glucose tolerance/DM in 15.2% (0% among the Sateré-Mawé Indigenous, 18.6% among the Indigenous from the Negro River, 20.2% among Brown/Black people and 12.5% among white people)20. It is important to emphasize that the high percentages may be due to the diagnostic criteria that considered impaired glucose tolerance and DM and, in addition, more than 52% of the sample was aged more than 40 years. According to National Health Survey data (2013), about 74% of adults with DM in the North region reported taking oral hypoglycemic agents or insulin in the last 2 weeks21, similar to our findings. This scenario is worrisome, as DM has increased in developing countries over the last few decades and is often underdiagnosed22. In addition, patients with DM living in remote rural areas have barriers to continuous access to medication. In Mexico, inadequately controlled diabetes is a leading cause of premature death in adults23. Therefore, it is essential that people with DM are aware of the benefits of regular use of medication, along with other non-pharmacological behaviors, to improve quality of life and prevent more severe outcomes.
The concomitant prevalence of SAH and DM in the sample was 4.4%, lower than that observed by Francisco et al (2018) in Brazilian elderly participants from the Surveillance System for Risk and Protective Factors for Chronic Diseases by Telephone Survey (Vigitel) (Brazil: 16.2%; Manaus: about 9%)15. These diseases are among the most prevalent chronic conditions worldwide, and often occur together, which not only complexifies the treatment strategies and increases healthcare costs, but also significantly increases the risk of cardiovascular outcomes24. Health promotion actions that enable improving patients’ adherence to healthy lifestyles, expanding the provision of care by the family health teams, and encouraging body weight control should be incorporated into routine health planning for the prevention of cardiovascular diseases.
It is important to highlight that the Amazonian rural riverside populations have daily activities such as fishing and hunting in the forest in their routines4 and, in addition, the extractive characteristic of the diet is still present in the communities more isolated from urban centers where there is a predominance of consumption of cassava flour, fish, and milk25, lifestyle habits that can be considered beneficial to health. However, there is also evidence that the ease of access to urban areas through river vessels can help change lifestyle habits, such as increased consumption of processed foods26,27, constituting an unhealthy lifestyle habit.
The prevalence of at least one chronic disease and the concomitant occurrence of SAH and DM were associated with age. The recognized occurrence of chronic diseases with advancing age is explained by greater exposure to risk factors throughout life, impairment of the physiological balance and senescence in multiple organs, leading to onset of diseases28. Results of a systematic review and meta-analysis about SAH in the population of Ecuador showed a linear increase in the prevalence of this disease according to age (<30 years 9.4%; ≥30–≤50 years 22.0%; >50–≤60 years 26.1%; and >60 years 48.7%)29. Nunes et al30, analyzing baseline data from the Brazilian Longitudinal Study of Aging (ELSI-Brazil), conducted with a nationally representative sample of the non-institutionalized population aged 50 years or older (n=9412 individuals), identified increasing prevalence of two or more chronic diseases according to increasing age (50–59 years 58.8%; 60–69 years 73.4%; 70–79 years 79.0%; and ≥80 years 82.4%).
No association was observed between the prevalence of chronic diseases and other sociodemographic variables, such as income and education. However, international evidence31,32 indicates consistency in the association between lower socioeconomic income levels and higher occurrence of chronic diseases, pointing to the social determination of the health–disease process among populations in high-income countries. However, the opposite has been observed for populations in low- and middle-income countries. In Brazil, studies have shown high percentages of chronic diseases and multimorbidity in rural and urban populations in the Southeast and South regions16,17. Population-based studies reinforce these findings33,34, suggesting heterogeneity related to socioeconomic development. Although we did not find an association between the occurrence of diseases and education, the association between low education and a greater chance of the occurrence of chronic diseases has already been observed in several studies31-33. Higher schooling seems to be a good socioeconomic predictor related to better life habits35, which can be explained by the awareness of prevention and control of risk factors for chronic diseases among individuals with more years of education36.
It is already well established in the literature that the main behavioral risk factors for illness from chronic diseases are smoking, physical inactivity, high alcohol consumption, and unhealthy eating37. Thus, eating habits are one of the main factors that can be modified for these diseases38,39. Results of a systematic review and meta-analysis of 43 observational studies showed that the consumption of ultra-processed foods, such as soft drinks, was associated with several cardiometabolic diseases and all-cause mortality40. A study carried out with data from the Family Budget Surveys conducted in 2002–2003 and 2008–2009 showed that more than a quarter (28.6%) of the increase in the prevalence of obesity among Brazilians was attributed to the increased consumption of ultra-processed foods in the period evaluated41. On the other hand, it was shown that the lower average purchase of soft drinks consumed at home was associated with a higher frequency of chronic diseases. This association can be explained by the reverse causality bias, given the cross-sectional evaluation of the present study. It is possible that after the diagnosis of a chronic disease, the family changed their behavior by reducing the purchase of these beverages on medical advice, given the harmful effect of regular consumption on cardiometabolic health evidenced in longitudinal studies42,43. In addition, it should also be noted that purchases for the home may not necessarily reflect individual exposure, which may resemble an ecological bias.
Another factor associated with a higher prevalence of at least one chronic disease and concomitant prevalence of SAH and DM was self-assessment of general health. Among those individuals with fair and poor/very poor health self-assessment, higher percentages of chronic disease were observed. National17,34 and international44,45 observational studies also observed an association between chronic diseases and a higher probability of fair or poor health perception. Health self-assessment jointly considers objective and subjective aspects of global health from the individual’s perspective and, due to its ability to predict morbidity and mortality, is an important indicator of the health status of populations46.
This study has limitations and strengths. There are limitations typical of cross-sectional studies, which restrict causal inferences and the interpretation of the directionality of some associations. The chronic diseases were assessed by self-report of medical diagnosis, which may be subject to recall bias. In addition, in general, the evaluated population has lower access to health services and, consequently, less possibility of diagnosing diseases. Therefore, it is likely that the evaluated outcomes are underestimated. However, it is noteworthy that the self-reported diagnosis is the most used strategy in epidemiological studies on this topic. We emphasize that a small number of chronic diseases were evaluated, since the main objective of the larger investigation from which this study derives was to evaluate the most prevalent diseases and access to health services. Despite the limitations, to the best of our knowledge, this is the first evidence of the prevalence of concomitant SAH and DM in an Amazon rural riverside population using data from a survey with probabilistic sampling. It is a difficult-to-access population, since they live dispersed in the territory and the main means of transportation are by rivers, which makes this group generally neglected in scientific research. Therefore, these findings can contribute to the planning of actions related to the management of multiple chronic health conditions, foster discussion on the subject and, at the same time, point to the need for future investigations that investigate a greater number of outcomes in the long term in these populations.
Conclusion
The prevalence of self-report of SAH or DM and of concomitant SAH and DM were observed in 18.8% and 4.4% of the sample, respectively. Sociodemographic characteristics, lifestyle habits, and health self-assessment were associated with a higher occurrence of the chronic diseases. In a scenario of socioeconomic vulnerability, lack of basic sanitation, intricate geographic barriers, and limited access to health care, the rural riverside populations are facing a great challenge through demographic, epidemiological, and nutritional transition processes. The available health services still have difficulties in offering continued care and in planning health policies and strategies aimed at the specificities of these populations. Comorbidities arising from chronic diseases will require an increase in displacement to urban areas in order to reach specialized care, which will not always be feasible to these populations. Recognizing the specificities of the Amazonian territories in the organization of health services is essential in the context of chronic diseases, and to guarantee the right to health of these populations. Finally, the study findings reinforce the need to strengthen health promotion and chronic diseases prevention strategies in the context of primary care.
Funding
The study was funded by the Foundation for Research Support of the State of Amazonas (FAPEAM) PPSUS-01/2017 – EFP_00014168, and PROEP-LABS/ILMD Fiocruz Amazônia, call for projects 001/2020. Jordana H. Siqueira received a scholarship (Scientific and Technological Development) from FAPEAM. Fernando J. Herkrath received a research productivity scholarship from FAPEAM.
Conflicts of interest
The authors declare that they have no conflicts of interest.



