Introduction
COVID-19 was declared a global pandemic on 11 March 20201. Many countries introduced safety measures to control the spread of the virus. Inevitably, medical schools across the world were affected by strict lockdown regulations and adapted teaching and training methods, some utilising alternative virtual platforms, which raised concerns regarding clinical clerkships and assessments2. The challenges faced by medical schools included shifting away from face-to-face teaching, virtual assessments, travel restrictions, student mental health and adequate university support services3. Studies on the impact of COVID-19 on medical students’ training have been conducted in various countries, including India, the UK, Singapore, China, Austria, Switzerland and the US2-9. A study conducted in the UK found that the majority of students felt that their preparedness for entering the health workforce had been impacted negatively but agreed that the curriculum changes were necessary and perceived that working in hospitals in need during the COVID-19 pandemic presented new learning opportunities4. In the US, universities attempted to overcome physical training restraints by converting to online teaching, some even using virtual reality-enhanced classrooms. Other universities allowed their students to aid in the front line by rotating through call centres and thereby developing telephone consultation skills9. In Singapore, classes were continued on online platforms, but students were also involved in frontline screening with measures in place to protect their health6. Most of these studies, however, were conducted in high-income countries, where the infrastructure to convert to alternative training platforms is more established than in low- and middle-income countries. Evaluating changes to the medical curriculum in low- and middle-income countries is essential to ensure continued high-quality training during unprecedented times.
South Africa introduced an alert-level risk-adjusted approach to the COVID-19 pandemic, entering Alert Level 5 on 26 March 2020, which brought tertiary education to a halt10. Due to lockdown regulations and the COVID-19 pandemic itself, the Stellenbosch University (SU) Faculty of Medicine and Health Sciences (from here on simply being referred to as ‘the faculty’) faced a particular challenge related to the structure of the 6-year Bachelor of Medicine and Bachelor of Surgery (MBChB) program. In this program, students commence their final clinical rotations (part of a 16-month student internship) in August of their fifth year. Because of this timing, a doubling in the number of students in Tygerberg Hospital (TBH), the academic medical centre where most of the rotations take place, normally occurs for 4 months at this time each year. Given that TBH was a designated COVID-19 facility, it became clear that the traditional training program would not be feasible in 2020, necessitating alternative arrangements for the fifth-year students. The faculty aimed to mitigate these challenges while still enabling learning through clinical experience instead of purely theoretical/virtual teaching by introducing the Integrated Distributed Engagement to Advance Learning (IDEAL) rotation.
During the 12-week long IDEAL rotation, students in the MBChB year 5 class were distributed across a range of healthcare facilities throughout the Western Cape and Northern Cape provinces, the furthest site (De Aar Hospital) being 755 km from the faculty (see Fig1 for a visual representation of the distribution sites). Distributed sites were selected by the faculty in consultation with the respective provincial departments of health and included metropolitan (metro) and rural sites that the faculty had existing relationships with for clinical training purposes. Students were requested to select five of these sites (in order of preference), after which allocations were done by the faculty, which attempted to accommodate students’ preferences. During the IDEAL rotation, students were required to meet a set of integrated outcomes, which encompassed objectives from several disciplines, including outcomes from the pre-existing Primary Health Care module. All students received an online skills logbook in which they were required to record specific procedures as selected by the various SU medical faculty departments. In addition, students were required to record five patients in the SNAPPS format11 on a biweekly basis, using a mobile app, and to identify learning objectives that could be discussed with their clinical supervisor. In order to minimise the burden on the clinical platform, each site divided their students into two groups who worked alternating days.
The main objective of this study was to ascertain the perspectives of student interns at the SU medical faculty regarding the quality of their restructured training during the COVID-19 pandemic as part of the IDEAL rotation and compare the perspectives of rural-site students with metro-site students. Secondary objectives were to ascertain the medical student interns’ safety, wellbeing, and COVID-19 exposure at distributed clinical sites.
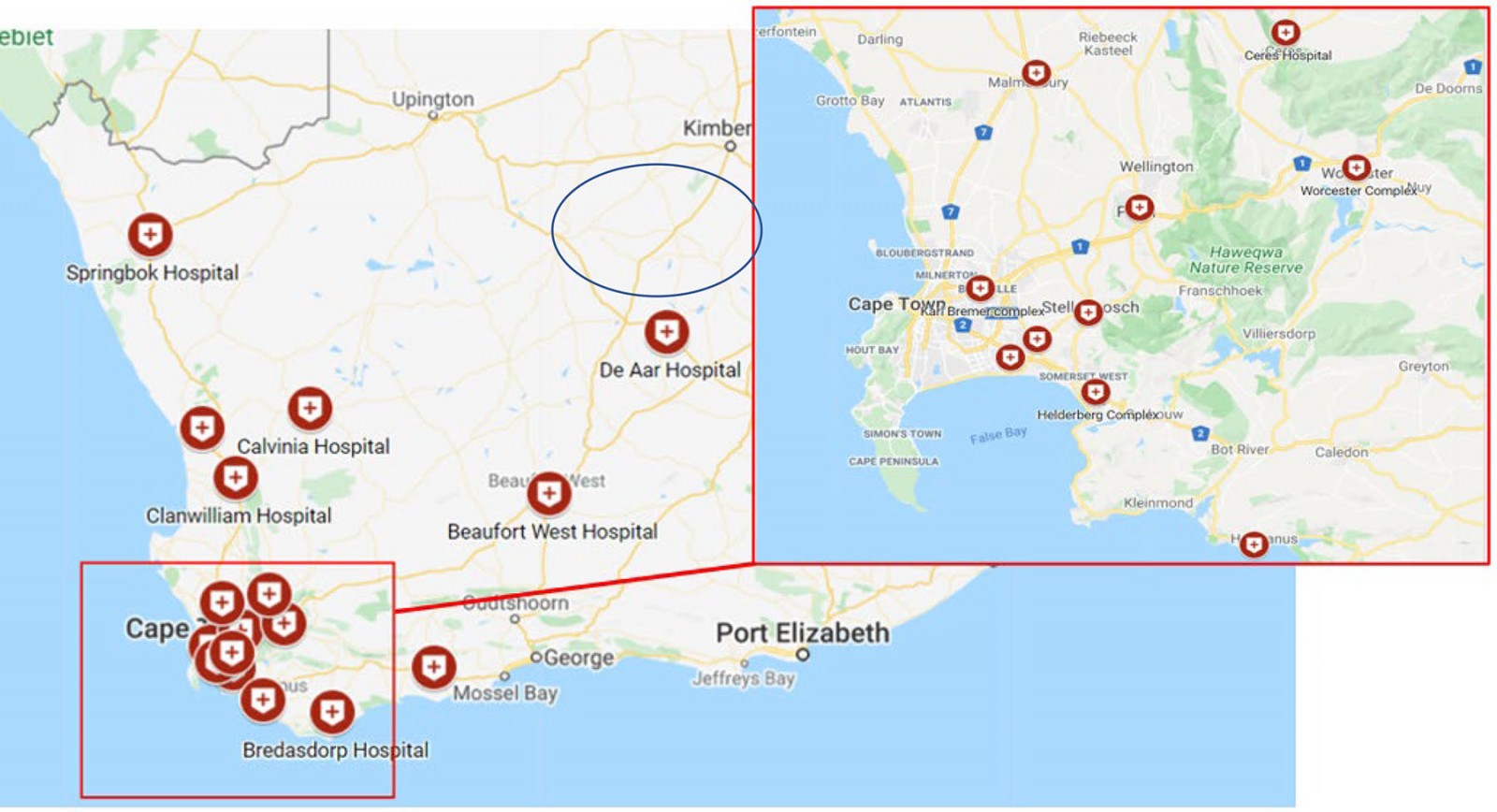 Figure 1: IDEAL rotation sites across South Africa.†
Figure 1: IDEAL rotation sites across South Africa.†
Methods
A cross-sectional study was conducted by online survey from 11 November to 17 December 2020. The study was conducted on SU MBChB year 5 students enrolled in the IDEAL rotation, including students distributed to both rural and metro sites. The survey was distributed to the students at all sites (Fig1) by email, Facebook and WhatsApp. The survey, consisting of 26 multiple-choice questions, 15 Likert-scale questions and 9 qualitative questions, was developed on Research Electronic Data Capture (REDCap) (https://www.project-redcap.org), a secure database12,13. The Framework for Distributed Health Professions Training14, that sets out essential components for training outside of tertiary sites, guided the survey questions. The survey included the following domains: clinical exposure and skills development (ie developing approaches to common undifferentiated health problems), theoretical teaching (ie formal and bedside teaching), student safety and support, COVID-19 exposure, and the overall training environment at the distributed site. The multiple-choice and Likert-scale questions were based on the domains described in the aforementioned framework, with the qualitative questions following some of these multiple-choice and Likert scale questions, asking participants to elaborate on their answers, in order to gain a better understanding of the quantitative data.
A total of 252 students were enrolled in the IDEAL rotation, with 68 distributed to rural health facility sites and 184 to metro sites. All students were invited to participate. Two students, although allocated to sites, subsequently interrupted their studies and did not complete the IDEAL rotation; there were thus 250 eligible participants.
Data analysis
Quantitative data were exported to SPSS Statistics v27 (IBM Corp, https://www.ibm.com/products/spss-statistics) for analysis. Multiple-choice questions were evaluated with descriptive statistics for frequencies and percentages, and cross-tabulated for inferential statistics for comparison of responses from rural and metro sites. To determine the statistical significance of associations, the Pearson’s χ2 test (significance threshold of 0.05) was done when 0–20% of cells had an expected count <5 and the two-sided Fisher’s exact test was done when more than 20% of cells had an expected count <5. Likert-scale questions were analysed as ordinal variables in order to determine distribution of the responses (strongly agree=1, agree=2, neutral=3, disagree=4, strongly disagree=5). The median, 25th percentile and 75th percentile were calculated for responses and the two groups were compared using non-parametric Mann–Whitney U-tests due to skewness of data and the ordinal scale of measurement (significant threshold of 0.05).
Qualitative responses were analysed thematically by identifying common themes in the data collected. Verbatim reading of the data was followed by inductive coding, with identification of themes and subthemes. All qualitative data were then categorised under the main themes identified. Initial coding was done by DSB, and then reviewed by RB and DB; there was consensus agreement on the main themes among all authors. Analysis of the qualitative data was performed separately for rural- and metro-site data, after which the two sets were compared. The themes that were raised most often are those reflected in this manuscript.
Ethics approval
The preface of the survey provided information on the study and explained that informed consent was implied if the student participant completed the survey. All responses were recorded anonymously. Three of the authors were students of the same class (all three were allocated to rural sites) and participated in the survey. Ethics approval was obtained from the SU Undergraduate Research Ethics Committee (reference U20/10/094; project ID 19043).
Results
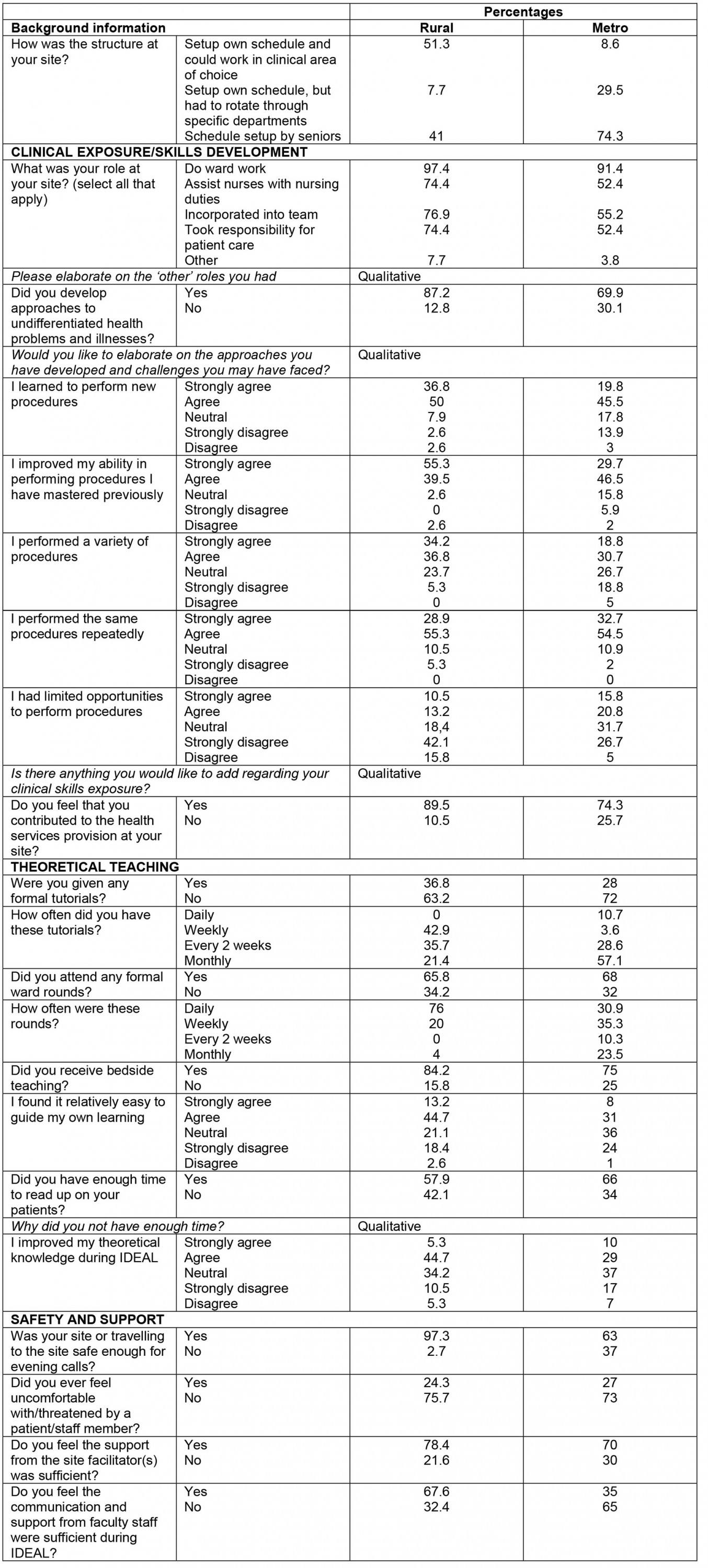
There were 155 respondents, a response rate of 62%. Of the 68 students distributed to rural sites, 39 (57%) responded to the survey; of the 184 students distributed to metro sites, 105 (57%) responded. Eleven of the respondents did not indicate in which site they were placed. There were 22 incomplete surveys, but the completed questions from these surveys were still included in statistical analyses. Refer to Appendix I for tabled results of all responses.
Clinical exposure and skills development
The structure of training at the sites varied from a flexible, self-constructed schedule to department-specific allocations (Table 1). Regarding the different roles assumed by students at distributed sites (Table 2), 109 students (78.4%) felt that they contributed to the health services provided at their site. A total of 106 participants (74.6%) indicated that they developed approaches to undifferentiated problems and illnesses, with rural-site students more likely to develop these approaches (34/39 (87.2%) v 72/103 (69.9%); p=0.035). In qualitative responses, some students from rural sites reported that the repetitive nature of common complaints helped them to develop practical approaches. However, other students from rural sites mentioned that there was a large number of common conditions they did not encounter and that the lack of feedback they received from healthcare staff decreased the productivity of patient encounters.
Rural-site students were more likely to report performing new procedures (p=0.006) and improving their perceived ability to perform procedures previously learnt (p=0.002) than metro-site students. Rural-site students were also more likely to report performing a variety of procedures (p=0.005) and less likely to report limited opportunities to perform procedures (p=0.01) than metro-site students. At rural sites, some students mentioned in their qualitative responses that they performed procedures above and beyond what had been on the list of requirements:
I was able to learn new procedures that were not on the skills list and thus learnt things above our requirements.
However, several rural students felt that there was a discrepancy between the way they had previously been taught to perform certain procedures and how the local staff were accustomed to performing them:
Sometimes the doctors or senior students taught a procedure, but not exactly in the way we have to know it. We also don’t have all the steps of the procedures, so we don’t know if we learnt the correct way of performing the procedure.
At metro sites, several students felt that exposure to clinical skills was insufficient and opportunities to undertake procedures were limited. This was exacerbated by alternating days on the clinical platform, frequent moves to different departments and elective students who had to share in the opportunities to perform clinical procedures:
Because we were rotating in different departments every week there was no time to get a good understanding of each discipline ... There’s a lot of the procedures in the log book that I didn’t even have an opportunity to see.
Table 1: Site structure for medical student interns during the IDEAL rotation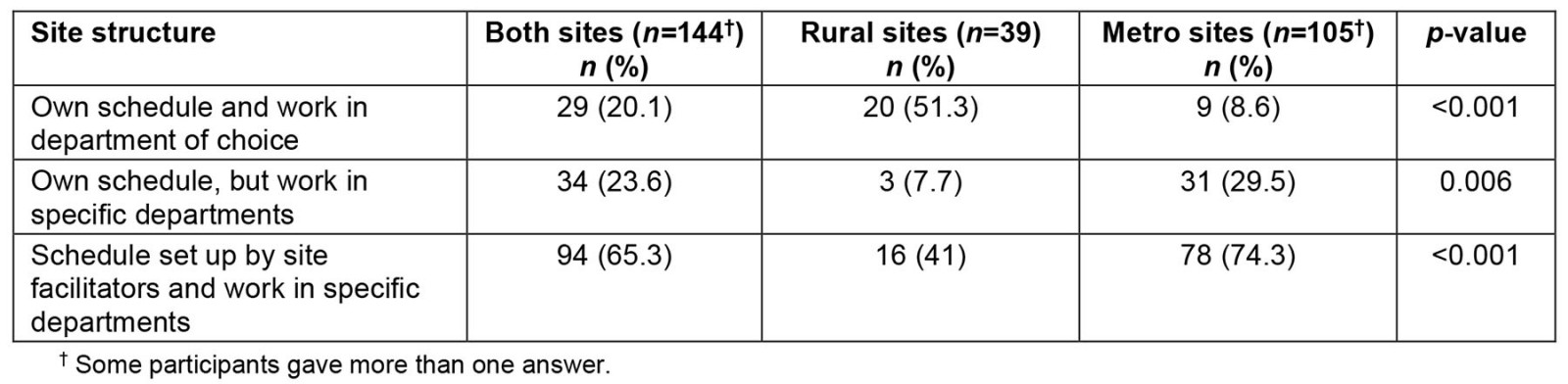
Table 2: Student role at the distributed site during the IDEAL rotation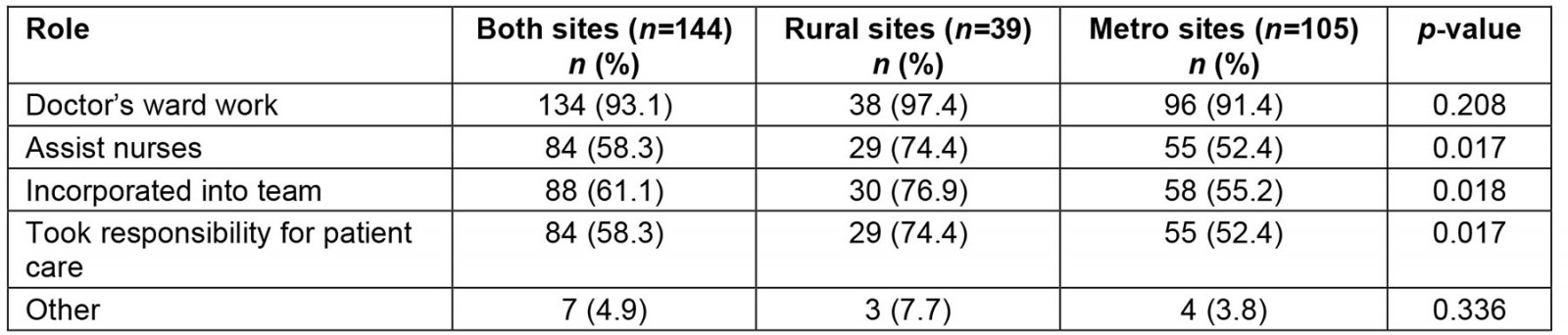
Theoretical learning
Only 42 students (27.1%) received formal tutorials at their distributed site, but 107 students (77.5%) received some type of bedside teaching and 93 students (60%) attended formal ward rounds. Rural-site students were more likely than metro-site students to attend daily ward rounds (19/25 (76%) v 21/68 (30.9%); p=0.001). Both metro and rural students found it easy to guide their own learning (median=2 (agree)), but only 88 students (63.8%) reported having had enough time to read up on the patients they saw in the wards or clinics and to consolidate their learning. Students were neutral (median=3) on whether they were able to improve their theoretical knowledge during the IDEAL rotation. Among both rural and metro sites, the foremost reason that students reported not having had sufficient time to read up on their patients was the large burden of assignments and projects:
There is too much tasks involved in IDEAL and these tasks limit one from actually learning new medical knowledge or revising old content.
Safety and support
Students in rural sites felt safer to travel to their site for evening shifts (p<0.001) than students in metro sites (some metro sites were located in informal settlements where crime rates are high). Although students at both rural and metro sites felt that their site-specific facilitators provided good support and guidance, rural-site students felt more supported by the overall SU medical faculty (p=0.001) (Table 3).
Table 3: Safety and support during the IDEAL rotation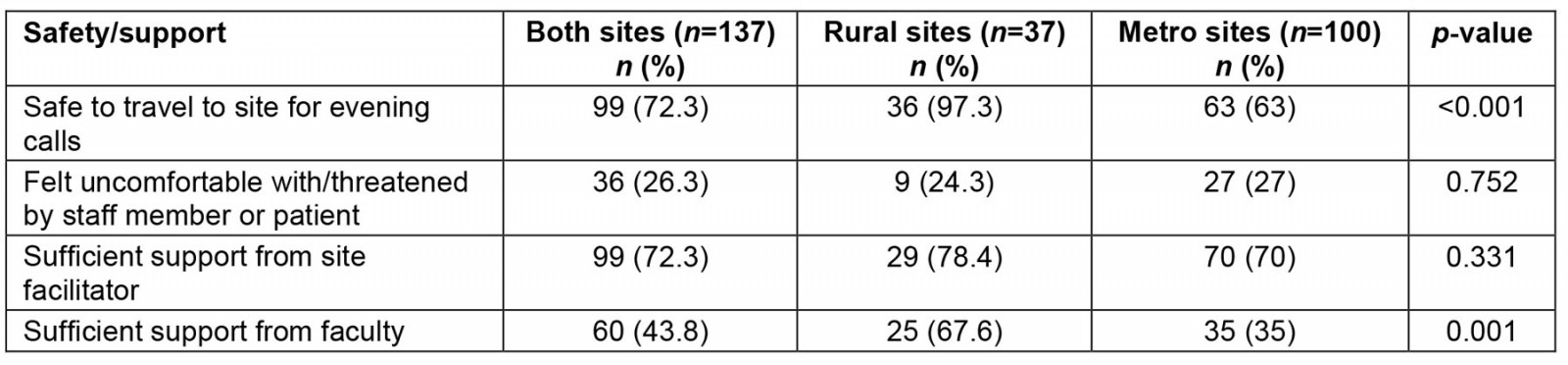
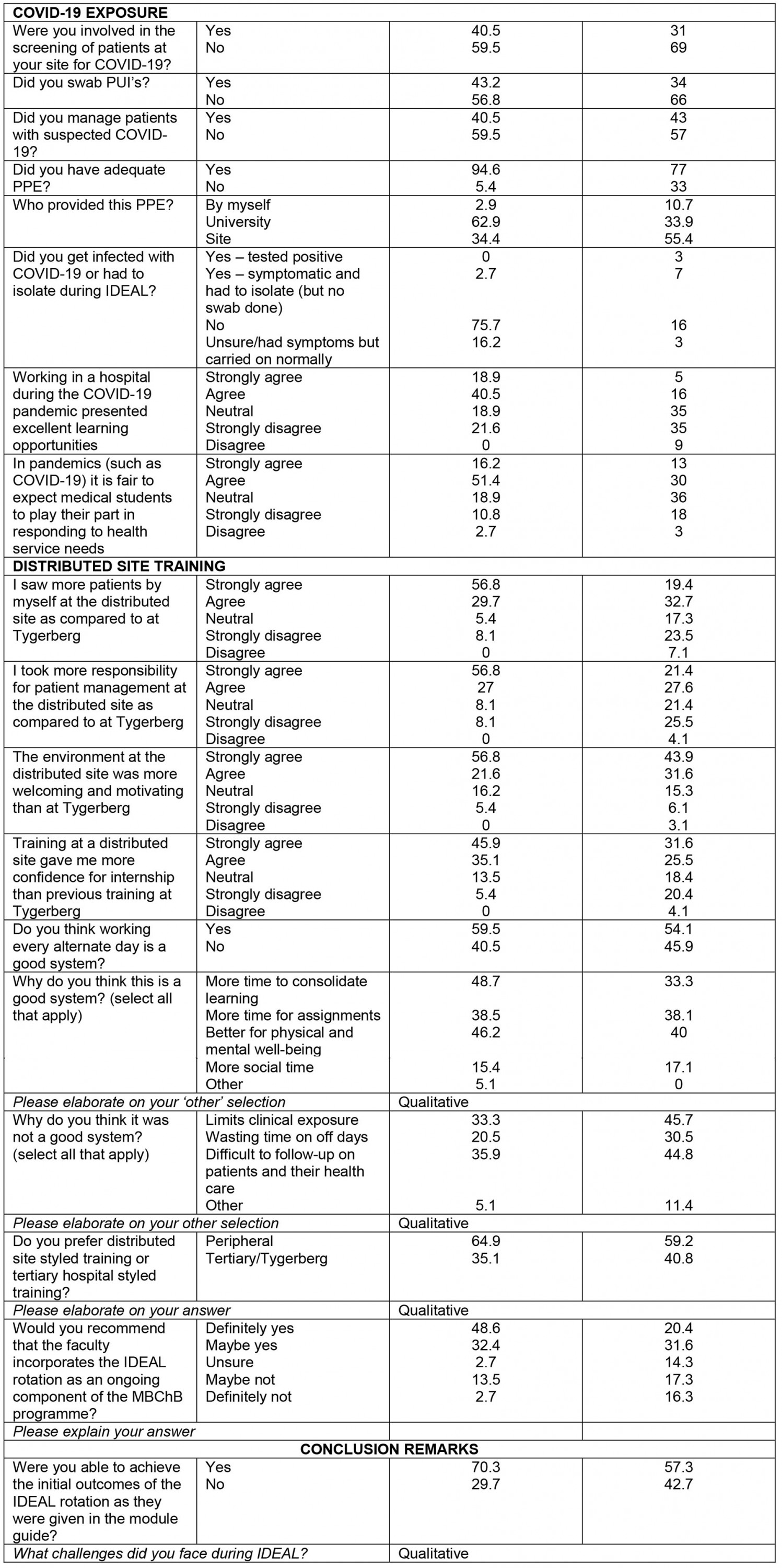
COVID-19 exposure
Students at both rural and metro sites performed pandemic-related clinical duties (screening, swabbing and managing COVID-19 patients) with similar availability of personal protective equipment and student infection rates (Table 4). Nonetheless, students at rural sites were more likely to agree that training during a pandemic provided good learning opportunities (p<0.001) and tended to agree that it is fair to expect medical students to play their part in a pandemic (median=2 (agree)), while metro-site students tended to be unsure (median=3 (unsure)).
Table 4: COVID-19 exposure during the IDEAL rotation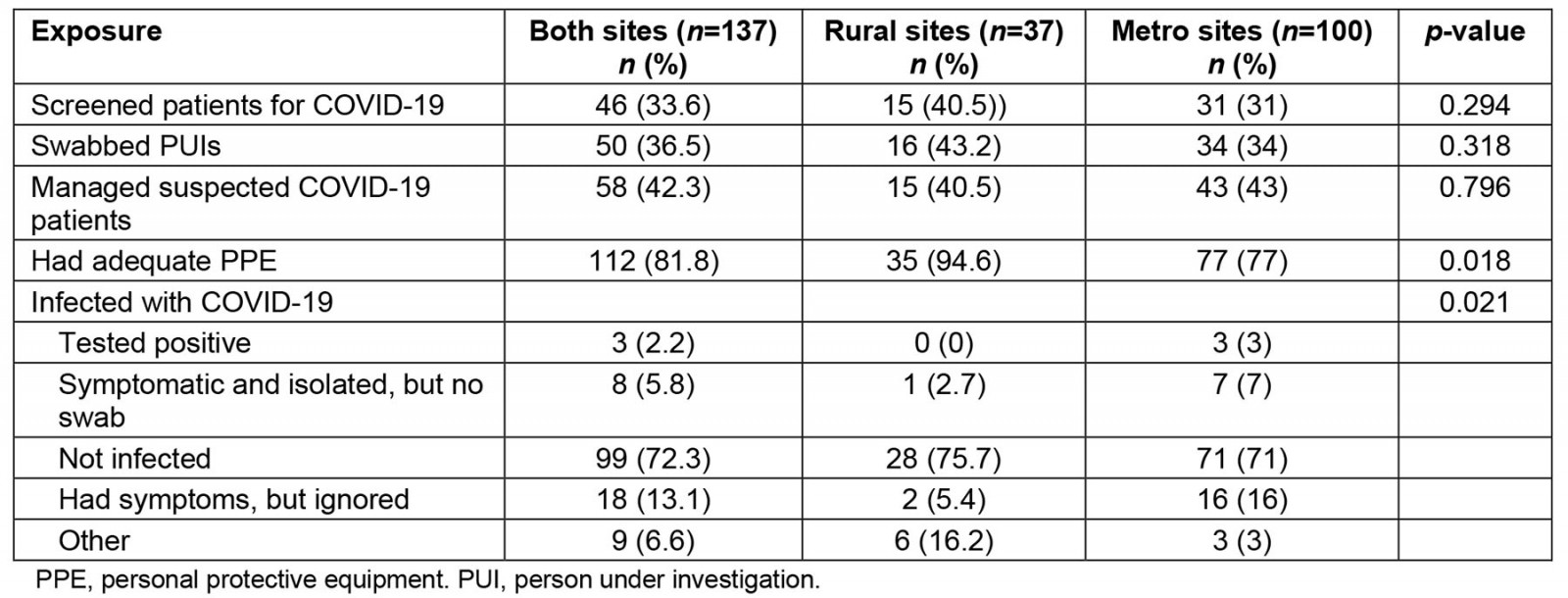
Comparison of distributed health facilities and tertiary hospital
Students at rural sites had different opinions from metro-site students about training in distributed sites compared to the tertiary hospital, TBH, where all students had previously trained. More rural-site students reported that they saw more patients independently (p<0.001) and took more responsibility for patient management (p<0.001) than during training at TBH. Students at both rural and metro sites reported that the environment at these health facilities was more welcoming and motivating than at the tertiary facility (rural median=1 (strongly agree), metro median=2 (agree)). Students felt that distributed training gave them more confidence for their future internship than previous training at TBH (median=2 (agree)). A total of 82 students (60.7%) indicated that they prefer training in the distributed site than at a tertiary hospital, with the likeliness of this preference being similar for both rural- and metro-site students (24/37 (64.9%) v 58/98 (59.2%); p=0.547). Several students at rural sites who preferred the distributed setting, despite some mentioning that they experienced theoretical training to be lacking, felt that the clinical training was suitable for their level of training and that the clinical environment was more supportive than they had previously experienced:
… the types of cases we saw were more in the level that we need to be at, and you get to see more patients that are undifferentiated which gives more opportunities for learning and using our own clinical reasoning.
In a similar manner to rural-site students, students at metro sites who preferred distributed sites also stated the lack of academic teaching to be a problem, but they based their overall preference on their positive experience at the distributed sites. This included exposure to common conditions that they felt was applicable for their level of training, smaller groups of students and a friendly environment that was beneficial for learning.
Students at rural sites who preferred the tertiary setting attributed their choice to the standard of teaching and staff engagement they receive at tertiary settings:
At TBH staff are used to having students present, and actively engage with students. In the periphery, it feels as though staff don’t know what to do with the students.
Students at metro sites who preferred the tertiary setting also attributed it to the negative experience they had at their rural sites, which included a lack of structure and standardisation, a lack of academic teaching and guidance, and a lack of communicated expectations.
The IDEAL rotation required students to work on the clinical service every alternate day. A total of 68 students (50.4%) felt that this was not a good system because it limited clinical exposure (n=61, 39.4%), led to a waste of time on off days (n=40, 25.8%) and made it more difficult to follow-up on patients and their care (n=61, 39.4%). However, 67 students (49.6%) supported the alternate-day system, reporting that they had more time to consolidate learning (n=54, 34.8%) and to complete their assignments (n=55, 35.5%). The latter also reported that alternating working days was better for their physical and mental wellbeing (n=60, 38.7%).
The majority of students at both rural and metro sites recommended that the faculty incorporate the IDEAL rotation into the MBChB program. Students reported that they based this on the confidence they gained from exposure to basic conditions they felt were applicable for their level of training.
Challenges faced by students
At rural sites, few difficulties were mentioned regarding clinical exposure, and most were related to having trouble accessing specific cases or types of patients that were required to carry out the projects stipulated by the curriculum. At metro sites, however, many students reported having too little clinical exposure and opportunities to perform certain procedures that were required of them. The reasons for the latter included the system of alternating days and changing departments as well as procedures not being available to all students.
The overwhelming majority of students from both metro and rural areas mentioned that they felt the project load had been excessive and distracted from their clinical focus and self-study goals.
Another common theme that arose from students at both rural and metro sites was the lack of academic teaching they received. At rural sites, students mentioned not only that there was limited teaching but also that the teaching they received often differed from what they had been taught previously.
Discussion
In response to the COVID-19 pandemic and resulting lockdown, the SU faculty introduced the IDEAL rotation, distributing students to rural and metro health facilities outside of the tertiary academic centre. Training at distributed sites appeared to have provided students with the opportunity to perform new procedures and to improve their skills, but also held unique challenges. Most students preferred distributed to tertiary-site training, due to a more welcoming and supportive environment and more opportunities to take responsibility for patient care.
Rose15 argued that, in response to COVID-19, it might be necessary for students to become part of the healthcare workforce and be embedded in the clinical platform to alleviate the pressure on healthcare systems. Our study shows that at distributed sites, especially rural sites, students were incorporated into the healthcare team and received excellent learning opportunities, while also feeling they supported the health system. These findings are similar to a UK study4, where the majority of students agreed that working on the clinical platform during a pandemic provided excellent learning opportunities. However, in contrast to the findings from our study, the students in the UK felt less prepared to start their Foundation year 1 (internship). Similarly, students in a Brazilian study16, also a low- and middle-income country, feared that they would not become good doctors following peripheral site training. This differs from our study, where the majority of students felt the restructured training during the pandemic gave them more confidence to start internship. This might be due to the fact that students at distributed sites were incorporated into the healthcare team, saw more patients independently and performed more procedures than at their tertiary training hospital. Various studies have emphasised the value of distributed-site training17-21, and our study supports its value. In addition, this study highlights the value of distributed-site training during the COVID-19 pandemic, not as a second best when the tertiary hospital could not cope, but as an equally good, or better, alternative.
The survey data suggest there may have been an advantage in training at rural sites during the pandemic. Students at rural sites reported being more likely to be incorporated into the healthcare team, take responsibility for patient management and improve their skills. Students at rural sites also reported being more likely to develop and consolidate approaches to common medical problems. This positive learning experience at rural sites is in keeping with the findings of a 2011 systematic review22.
A limitation of this study is that it was a single-institution study, and the uniqueness and context of the innovation described would make comparisons difficult. Another limitation is that it did not include the feedback of clinical trainers. A third limitation is that the survey did not include questions on how cultural diversity (or lack thereof) might have influenced students’ experiences at these various sites. A fourth limitation was confirmation bias, as all the student authors chose rural placements, and had to guard against interpreting the results in favour of rural sites.
To balance this, the strengths of this study are a response rate of 62%, with 57% of both rural- and metro-site students participating in this study, allowing for inferential statistical analysis. This study provides novel information on the training of medical students during the COVID-19 pandemic, as SU took a distributed training approach to mitigate the challenges of the pandemic, while the majority of medical schools converted to virtual training2,15. This study also provides information on medical training during the pandemic on the African continent. A further strength is that the study was conceptualised and led by medical students who participated in the IDEAL rotation (RS, DSB, DB), and who thus brought an important insider perspective to the research. To enhance reflexivity, the interpretation of the findings, in particular the qualitative data, was discussed with the faculty supervisor (IDC).
Conclusion
The COVID-19 pandemic provided challenges for the continuation of quality medical training. It also provided the opportunity for innovative changes. This study demonstrates the successful outcomes, even during the pandemic, of distributed-site training, where students are immersed in the healthcare team, take responsibility of patient management and report that they improve their skills. Students at rural sites tended to report a more positive perspective on their clinical training. Rather than seeing the end of the pandemic as a time to revert to the previous status quo, the students in this study suggest to us that the lessons learnt from this forced innovation in distributed learning can now inform a better approach to clinical education for the future.
Funding
No funding was obtained for the purpose of the study.
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2021 - Workplace locations of 2011–2017 Northern Territory Medical Program graduates