Introduction
In contrast to other developed nations, the US does not have universal health care. The nation’s healthcare system is complex, including multiple payers, and combining public and private funding. Without universal care, access to health care varies considerably. Notably, financially disadvantaged, rural, and minoritized populations face barriers to accessing health care. The US is also experiencing a shortage of healthcare workforce due to an aging population, aging workforce, and limited infrastructure for training new physicians1.
Complexities of health care in the US can be seen particularly in maternal health. In recent decades, the maternal morbidity and mortality rate has tripled2-4, leaving the US far behind other high-income countries5. Additionally, infant mortality of 5.8 deaths per 1000 live births in the US is considerably higher than the 3.8 average of other developed nations6.
Moreover, the crisis is worse in rural America. Maternal morbidity and mortality and infant mortality rates are highest in the most remote and least populous areas3,7. One analysis of a nationwide sample controlling for sociodemographic factors and clinic conditions revealed that rural patients were 9% more likely to experience severe maternal morbidity than urban patients8. Several factors contribute to the current crisis and poor outcomes in rural areas. The scope of the current protocol and the project it evaluates is limited to physician shortages and limited access to maternal care.
The shortage of physicians in the US is projected to get worse, and limited access to maternal care services, especially in rural areas, contributes to the maternal health crisis9,10. For example, nearly half of US counties lack obstetrics and gynecology physicians11, and more than a third of counties are considered maternity-care deserts (with no hospital or birth center offering obstetric care). Most maternity-care desert counties are in rural areas12. Further, the number of maternity-care deserts is increasing13. By 2030, the Health Resources and Services Administration (HRSA) projects a shortage of 5170 obstetrics and gynecology physicians. HRSA projects increased participation of advanced practice providers, particularly certified nurse midwives, in providing maternity care. Although increased involvement of advanced practice providers will improve access, especially in rural areas, physicians are essential in maternity care, especially for managing complex and high-risk cases, surgical procedures, and emergencies14.
Recent political developments further complicate the maternal health crisis in the US. The Supreme Court in the decision relating to Dobbs v Jackson Women’s Health Organization (2022) opened the way for states to ban abortions. The resulting confusion and uncertainty in legal implications of providing some obstetric and women’s health services are predicted to result in limited access and increased inequity in women’s health services. The decision is also expected to have detrimental impacts on the training physicians receive in reproductive health care15. The chilling effects of the Dobbs decision may exacerbate maternity care shortages further.
Due to the lack of obstetrics specialists, many women, especially in rural areas, rely on family medicine physicians for maternity care. Unfortunately, fewer family medicine physicians are providing maternity care services16,17. Whether family medicine will or even should continue to provide maternal care is in question18-20. The current crisis will not be resolved without addressing service shortages and defining the role of family medicine in maternal care in rural areas.
Calls have been made to build capacity for high-quality maternity care in rural areas and maternity-care deserts21,22. However, limited access to maternity care is a complex problem stemming from multiple factors. Efforts to build capacity must, likewise, be multifaceted in order to succeed23. This article describes the evaluation of a project aiming to build maternal care capacity in rural and underserved areas.
Methods
Project
This project takes place at the University of Utah Health, Salt Lake City, Utah and is supported by the HRSA of the US Department of Health and Human Services as part of an award totaling US$2,797,464.00 (A$4,349,455.10). Contents of this protocol are the authors’ and do not necessarily represent the views of nor an endorsement by HRSA, the Department of Health and Human Services, or the US Government. The project’s purpose is to increase the number of highly qualified family medicine physicians providing maternity care services in rural and underserved areas of Utah. As shown in Figure 1, the project uses a multifaceted approach to addressing maternal care shortages in rural Utah, including:
- strengthening partnerships between educators, providers, and community-based organizations
- enhancing maternal care training of family medicine residents and obstetric fellows
- improving the transition from training to rural practice.
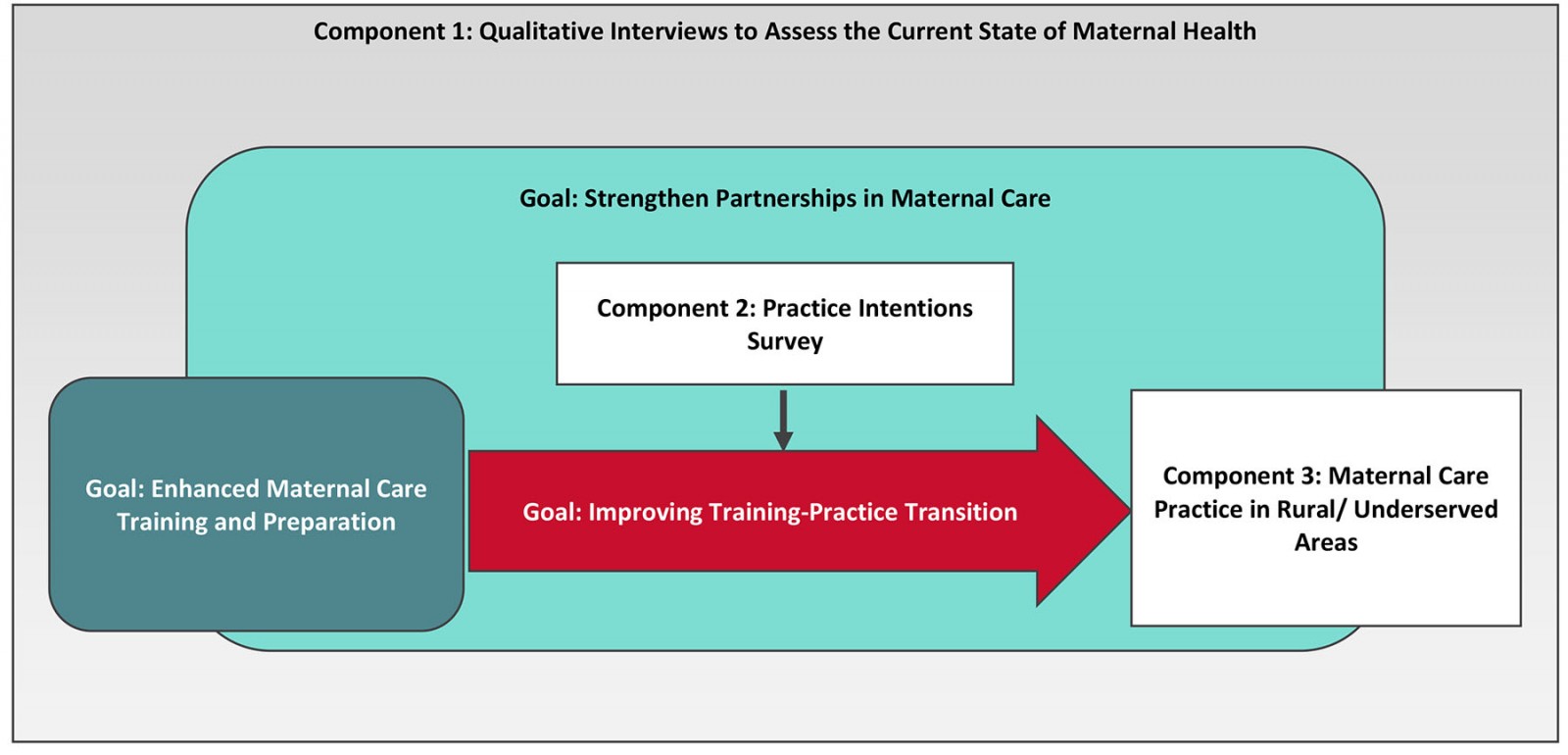 Figure 1: Project evaluation framework
Figure 1: Project evaluation framework
Evaluation design
The aim of the evaluation is to better understand the state of maternal health in rural and underserved Utah and identify effective ways to increase the number of physicians providing high-quality maternity care in those areas. To reach this aim, the evaluation employs a mixed-methods approach. The sample includes patients, providers, administrators, educators, residents, fellows, and other stakeholders.
As shown in Figure 1, the evaluation includes three components. Component 1 consists of qualitative interviews that serve as a contextual evaluation of the state of maternal health in rural and underserved areas. Component 2 is a practice intentions survey to gauge the interest of residents and fellows in practicing in rural or underserved areas and in including maternity care services in their practice. Component 3 assesses outcomes of graduates, including practice in rural and underserved areas and provision of maternity care services.
Component 1: Contextual evaluation
The first component is a contextual evaluation and consists of qualitative interviews with various stakeholders. The specific aim of these interviews is to increase understanding of the current state of maternal health in rural and underserved areas of Utah. Discussions focus on identifying needs of and barriers to maternal health and high-quality maternity care. Interview findings will inform grant activities and training of family medicine residents and obstetric fellows.
Participants: Interview participants include individuals with knowledge and experience in maternal health in rural areas. Participants' involvement in maternal health falls into one of seven roles (Table 1). About 5–10 participants from each group will complete interviews. Participants are selected based on experience with maternal health and involvement and connection to the Maternal Health Capacity Building project. During interviews, participants are asked for referrals of other individuals with knowledge and experience regarding maternal health in rural and underserved areas to include in the interview sample. Physicians and home visitors are asked to refer new and expectant mothers to participate in interviews. All interviews are conducted in English.
Table 1: Interview participant descriptions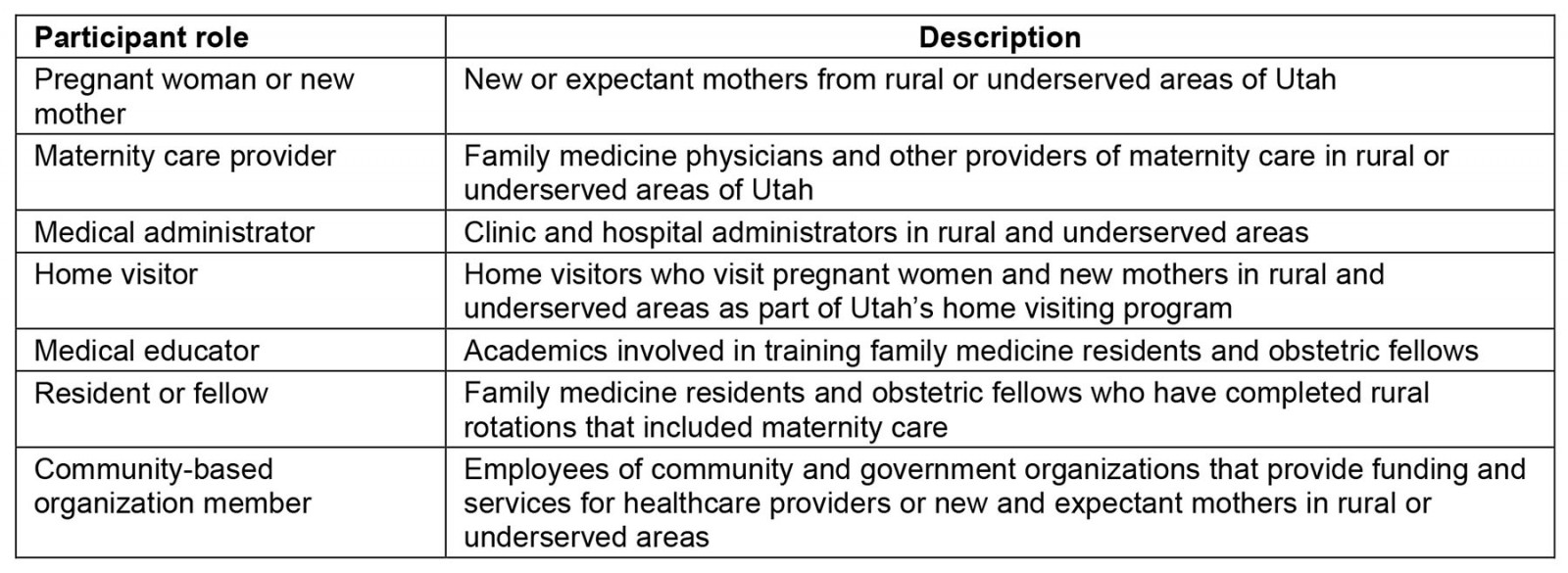
Interview question development: Interview questions were developed based on a targeted literature review on maternal health in rural areas of the US and a review of the project’s goals. First, a set of questions for home visitors were developed. Semi-structured interview guides focus on four areas: background information about the participant, maternity care information regarding the area in which the participant works or receives care, substance-use disorder resources for pregnant women and new mothers in the area, and the use of telehealth services for maternity care provision. Interview guidelines include general questions with optional prompts that the interviewer could use to elicit more specific information. After an initial draft of the home visitor interview guide, members of the project steering committee and community advisory board provided feedback, revised questions, and added additional questions. The home visitor guide provided the basis for interview guides for all other participant groups. All interview guides included the four areas of focus described above and the same basic questions. Wording and prompts were adjusted to be appropriate to each participant group.
Interview procedure: Semi-structured interviews are conducted virtually by Zoom, in person, or by phone. All participants receive an email invitation to participate. Invitations include study information and inform participants that, by completing the interview, they are providing their consent to participate in the study and for the information they provide to be included in analyses. Interviews last about 30 minutes to an hour.
Interview analysis: Conventional content analyses24 is used to summarize interview findings. The analysis involves:
- development of codes: Multiple researchers independently review interviews, and sort and combine keywords and phrases into groups and subgroups based on similarity and relatedness. After each researcher independently develops a system of categories, researchers meet and review and discuss the categories they independently generated and develop a final comprehensive coding system.
- coding and reporting: Multiple researchers employ the final coding system to code each interview transcription. Multiple researchers code a minimum of 25% of interviews to calculate inter-rater reliability. Researchers identify themes and create summaries based on the prevalence and salience of specific codes.
Component 2: Practice intentions survey
The second component of the evaluation is a survey of practice intentions of family medicine residents and obstetrics fellows. The survey aims to determine how many residents and fellows intend to provide maternity care in rural or underserved areas in their professional practice, and to understand the factors and considerations related to practice intentions.
Survey participants: The survey is administered to family medicine residents and obstetric fellows for 4 years. The obstetric fellowship is a 1-year program; in order to get longitudinal data for fellows, the survey is administered to them twice per academic year, once at the beginning and once at the end. In total, the survey will be completed up to 120 times by 60 residents, with residents completing the survey up to three times; and 30 times by 15 fellows, each fellow completing the survey twice.
Survey development: The intentions survey was developed based on a targeted literature review of family medicine physicians’ intention and decision to provide maternity care and intention and decision to practice in rural or underserved areas. The review identified specific factors related to practice decisions that were included in the survey. The survey consists of five sections:
- Asks questions about intentions to practice in a rural or medically underserved area and relevant considerations for determining where to practice.
- Asks questions about intentions to provide maternity care services and relevant considerations for determining whether to include maternity care services in practice.
- Asks questions about additional practice intentions that may be related to rural or underserved practice.
- Asks questions related to the residency or fellowship program, including questions about rotations completed.
- Asks questions about demographic and background information of residents and fellows, including medical degree, age, gender, and race and ethnicity.
Content experts, including family medicine physicians and educators, reviewed, piloted, and revised the survey
Survey procedure: The residency director and fellowship director send an email invitation, including a survey link to residents and fellows. Reminder emails are sent to residents and fellows every 2 weeks until a sufficient number have completed the survey or until no additional residents and fellows complete the survey after receiving reminders.
Data analysis: Analyses will include descriptive statistics such as frequencies, cross-tabulations, means, and standard deviations or standard errors to summarize demographic and other survey responses and compare descriptive statistics across the years of implementation to monitor changes in response patterns across years of the project. In addition, item responses will be combined into scales, and alpha or other appropriate scale statistics will be calculated. Scale scores will be used for statistical tests. Data analysis will include comparing means across groups or categories using student t-tests or ANOVA and comparing frequencies across groups or categories using χ2 testing. Regression models may also be employed to test for relationships between variables of interest. Power calculations indicate that statistical tests or regression analyses will only be feasible given a sufficient sample size and will only be used to analyze results after a few years of implementation and given sufficient participation (n=75 approximately by year 5, for a medium effect size, the desired power level of 80%, given an alpha level of 0.05). Before statistical tests, data will be analyzed for normality and other pertinent assumptions.
Component 3: Outcomes
The evaluation’s final component includes measuring the professional practice of graduated residents and fellows through a fellowship alumni survey and by tracking National Provider Identifier (NPI) numbers. This component aims to determine how many graduates go on to practice in rural areas, and to track information about their professional practice.
Participants: All 34 fellowship alumni who have graduated since the start of the obstetrics fellowship will be invited to complete the alumni survey. In addition, 50 graduates of the residency and 15 graduates of the fellowship will be tracked using NPI numbers.
Survey development: The fellowship alumni survey consists of six sections. The first section collects information about demographics, fellowship completion, and training. The second section asks about current practice location and general characteristics. The remaining four survey sections include practice-related items, such as care provided, conditions managed, maternal care-related procedures performed, and obstetric surgical procedures performed. The last four sections of the survey are presented in random order to counteract any effects of survey fatigue. Content experts, including family medicine physicians and educators, reviewed, piloted, and revised the survey.
Data collection: Information will be collected from NPI profiles of program graduates including practice status, specialty, and location. Beginning with residents and fellows who completed the program in the academic year 2020–2021, the year before the start of the HRSA-funded project, practice status, specialty, and location are reported from NPI profiles. This information is tracked for graduates of both programs for the subsequent years of the project, concluding in 2026. Rural practice is reported for graduates based on practice location listed in the NPI registry. Internet searches of graduated residents will be used to ensure information from the NPI registry is up to date. To administer the survey, invitations are sent via email to alumni. Survey completion is tracked, and follow-up emails are sent to alumni who have not completed the survey.
Data analysis: Counts of graduates who continue to practice and specialize in family medicine, and practice in rural and underserved communities, are reported and compared year-to-year. Changes in practice location are tracked, with particular interest in the number of graduates who practice in rural or underserved areas compared year-to-year.
Overall, analyses determine whether and how demographic, program, and training information are related to the outcomes of care provided, managed conditions, and procedures performed. Specifically, analyses address whether care and services provided vary depending on training received during or since fellowship completion or timing of fellowship completion. Power calculations indicate that statistical tests and regression analyses are not feasible given our sample size of 34 (n=45 approximately, for a one-sample medium effect size, the desired power level of 80%, given an alpha level of 0.05).
Ethics approval
The University of Utah Internal Review Board approved the interview procedures (IRB_001581199) and gave exemption status to survey procedures (IRB_00159399) described in this protocol.
Results
This study protocol describes the evaluation of a HRSA-funded project to build capacity for maternal care in rural and underserved Utah. The evaluation collects important contextual information regarding the current state of maternal health in rural and underserved areas and indicators of short- and long-term outcomes. Results serve three important purposes: to fill gaps in the current literature regarding outcomes of capacity-building efforts, provide practical guidance for this and other projects seeking to build rural capacity for maternal care, and to help define the role of family medicine in addressing the maternal health crisis.
The US maternal health crisis, the shortage of maternity care in rural areas, and the dwindling participation of family medicine in maternal care are well documented. However, research on outcomes of efforts to address maternal care shortages in rural areas of the US remains scarce. Despite the calls for action and recommended practices for improving maternal health, there is little published on efforts to increase and develop the rural maternity care workforce in the US. Results of this evaluation will help to fill this gap.
In addition, results of this evaluation will provide specific implications for overcoming the maternal health crisis in the US. Evaluation outcomes will help to identify successful elements of the project that can be scaled up and adopted to build maternal care capacity and improve maternal health outcomes in other rural areas.
For now, family medicine’s role in maternity care is an open question18-20. One path forward involves training all residents to perform basic maternity care and providing advanced training to residents with greater interest in maternal health. Such a path is aligned with recently updated family medicine residency requirements from the Accreditation Council for Graduate Medical Education. This path seeks to increase the number of family medicine physicians providing maternal care. Evaluation results will test the viability of advanced training for a subset of family medicine residents as a means of increasing the number of family medicine physicians providing maternal care.
Conclusion
The contributions of this evaluation are important, but additional research is necessary. There is a need for articles, research protocols, and demonstration projects including both methodology and outcomes to identify effective practices for building maternal care capacity, and exploring and defining how family medicine can best collaborate with other specialties and advanced practice providers to address the maternal health crisis in rural areas of the US.
Funding
The University of Utah received funding from the HRSA for this study.
Conflicts of interest
The author and co-authors declare no conflicts of interest.
References
You might also be interested in:
2008 - Labouring to nurse: the work of rural nurses who provide maternity care


