Context
Statistics Canada defines an urban area (or population center) as having a population of at least 1000 and a density of 400 or more people per square kilometer. Any territory not meeting this definition is considered a rural area1. In 2017, Statistics Canada developed a remoteness index (RI) for almost all Canadian census subdivisions2. The RI is assigned on a normalized scale of 0 to 1 where 0 is the most accessible (urban) and 1 is the least accessible (remote) area2. According to these definitions, approximately 20% of Canadians reside in rural or remote communities and the majority of Northern Ontario can be classified as rural or remote. In Canada, most otolaryngologists practice in urban centers and the number of practicing otolaryngologists in rural and/or remote areas of Canada is decreasing3. The main cities in rural Northern Ontario with populations of 7500–160 000 people have either ‘permanent’ otolaryngology physicians (Greater Sudbury, Thunder Bay, Sault Ste. Marie, North Bay and Timmins), ‘visiting’ otolaryngology providers (Kenora, Elliot Lake and Dryden) or no regular access to otolaryngology services. Less populated communities, such as Kapuskasing, Kirkland Lake, Fort Frances and communities in the Sioux Lookout area, also have access to ‘visiting’ otolaryngology providers.
The Meno Ya Win Health Centre is a 60-bed hospital in Sioux Lookout, Ontario. The hospital provides healthcare services to 30 000 people across 31 remote communities (Fig1) including all residents of Sioux Lookout and the surrounding area, including Hudson, Pickle Lake, Savant Lake and the First Nation communities in the region. The center has a broad range of general and specialized resources including acute care, admitting, general anesthesia and surgical resources. The Meno Ya Win Health Centre is a centre of excellence for Aboriginal care. Sioux Lookout has a population of 5272 encompassing an area of 536 km2, and a population density of 9.8 people per square kilometer. Sioux Lookout is therefore considered a rural and remote area.
 Figure 1: Map of service area of Meno Ya Win Health Centre, Northern Ontario, Canada.
Figure 1: Map of service area of Meno Ya Win Health Centre, Northern Ontario, Canada.
Issue
There is a discordance between the prevalence of otolaryngologic disease and the availability of otolaryngology services in remote and rural communities in Canada and other countries3,4. Crowson and Lin (2017) described the urbanization of otolaryngology – head and neck surgery (OHNS) providers, in which the number of rural OHNS providers is decreasing annually (–0.38 providers/year) and the number of urban OHNS providers is increasing annually (11.4 providers/year)3. Diminished access to otolaryngology services in rural areas will undoubtedly delay timely diagnosis and treatment. Underserved and vulnerable populations are less frequently diagnosed with common otolaryngologic disorders and come to clinical attention with advanced forms of disease5. Diminished accessibility to otolaryngology care in rural and remote areas is prevalent across other developed countries including the US and Australia6-8. Timely access to medical specialties such as OHNS in Northern Ontario is further challenged by long wait times and long distances to services9-12. It is evident that new models of care delivery are required that are efficient, cost effective and tailored to the needs of the population by minimizing disruption caused by travel and financial burden.
The visiting otolaryngology team
The authors proposed the implementation of a visiting otolaryngology team consisting of three surgeons with expertise in multiple subspecialty areas, including otology, neurotology, rhinology, head and neck surgical oncology and pediatric otolaryngology, as well as one otolaryngology trainee. Patients were not assigned a priori to a specific otolaryngologist based on patient age or presenting problem. Rather, patients were seen in the order of their appointment time by the first available otolaryngologist. Subsequent consultation with a second otolaryngologist with the relevant expertise was frequently done to ensure the most appropriate and timely investigative and treatment recommendations were provided to patients. This practice provided reassurance to the otolaryngology team members from a quality perspective and eliminated the need for referral to another subspecialist.
The team treated patients in the otolaryngology clinic at Meno Ya Win Health Centre over two 1-week periods in March 2020 and March 2021. Patients were referred to the clinic from primary care providers and nurse practitioners located in the northern communities. The COVID-19 pandemic did not influence the number of referrals to the clinic, or the level of care provided during the two seasonal visits. It should be noted that the annual team visit replaced an occasional single visiting otolaryngologist. As such, the annual visit has augmented the visiting outreach and represents a net gain in otolaryngology service.
Demographic and clinical data were collected from patients during clinical visits. The following information was recorded: gender, age, chief complaint, past medical history, past surgical history, tobacco use and alcohol use. The patients’ access to a GP, wait time to see a GP, wait time to see a specialist and distance traveled for the current visit were also recorded. Chief otolaryngology complaints were categorized as maxillofacial traumas; sleep-related breathing disorders; head and neck cancers/mass; general ear, nose and throat conditions; laryngology; rhinology; nasal obstructions and sinusitis; otology and neurotology; or other.
Ethics approval
The study was reviewed and approved by the Institutional Research Ethics Board at Meno Ya Win Health Centre (REB #03-21, 23 April 2021).
Demographics
Demographic and clinical data were retrieved from 276 consecutive patients presenting to the Meno Ya Win Health Centre otolaryngology clinic during the March 2020 (n=154 patients) and March 2021 (n=122) clinics. The median age was 47 years (range: newborn to 85 years). Seventy-one patients (26%) were children (age <18 years) and 78 patients (28%) were older than 60 years. A prominent cohort (n=110, 40%) was adults aged 31–60 or more years (Table 1).
Table 1: Patient characteristics, alcohol and tobacco use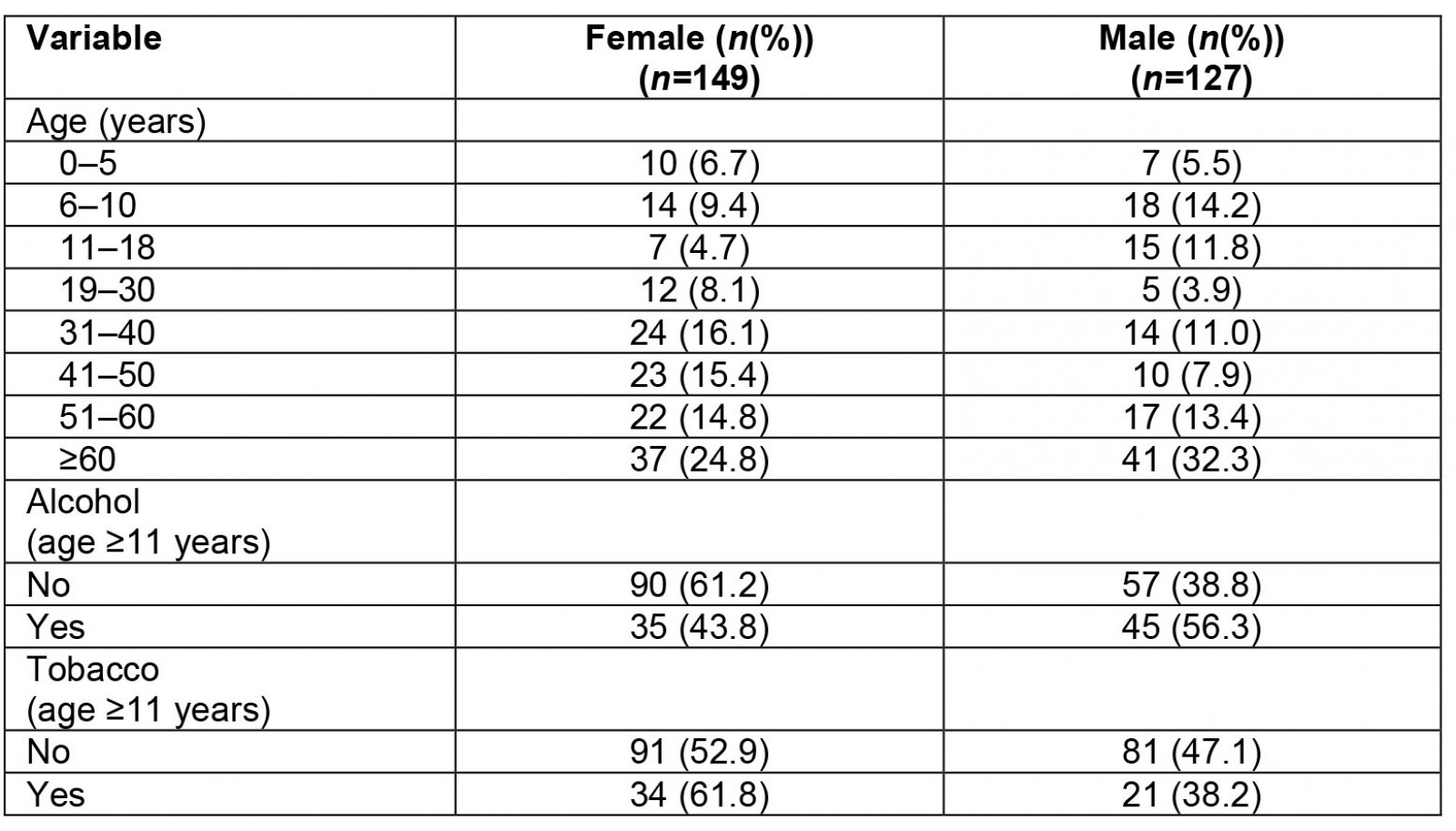
Clinical presentations
In all patients, the most common otolaryngology-related clinical complaints were hearing loss (n=62, 23%), nasal obstruction (n=34, 12%), vertigo (n=16, 6%), tinnitus (n=15, 5%) and adenotonsillar disease (n=14, 5%). It should be noted that some patients presented with more than one complaint in the clinic and the total number of clinical complaints was greater than the number of patients (n=279). Clinical presentations were categorized and summarized for pediatric and adult patients in Figure 2. Pediatric patients most commonly presented with otitis media (n=12, 17%) and hearing loss (n=10, 14%). Patients older than 18 years most commonly presented with hearing loss (n=52, 25%), nasal obstruction (n=29, 14%), vertigo (n=15, 7%) and tinnitus (n=14, 7%). Surgical interventions were limited to adenotonsillectomy, myringotomy and tube insertion, functional endoscopic sinus surgery, tympanoplasty, septoplasty, rhinoplasty, and needle and open biopsy procedures in patients without serious comorbidities. Patients requiring similar procedures and who had comorbidities were referred to regional centres. Very complex surgeries or patients with significant comorbidities were referred to academic tertiary centres for treatment.
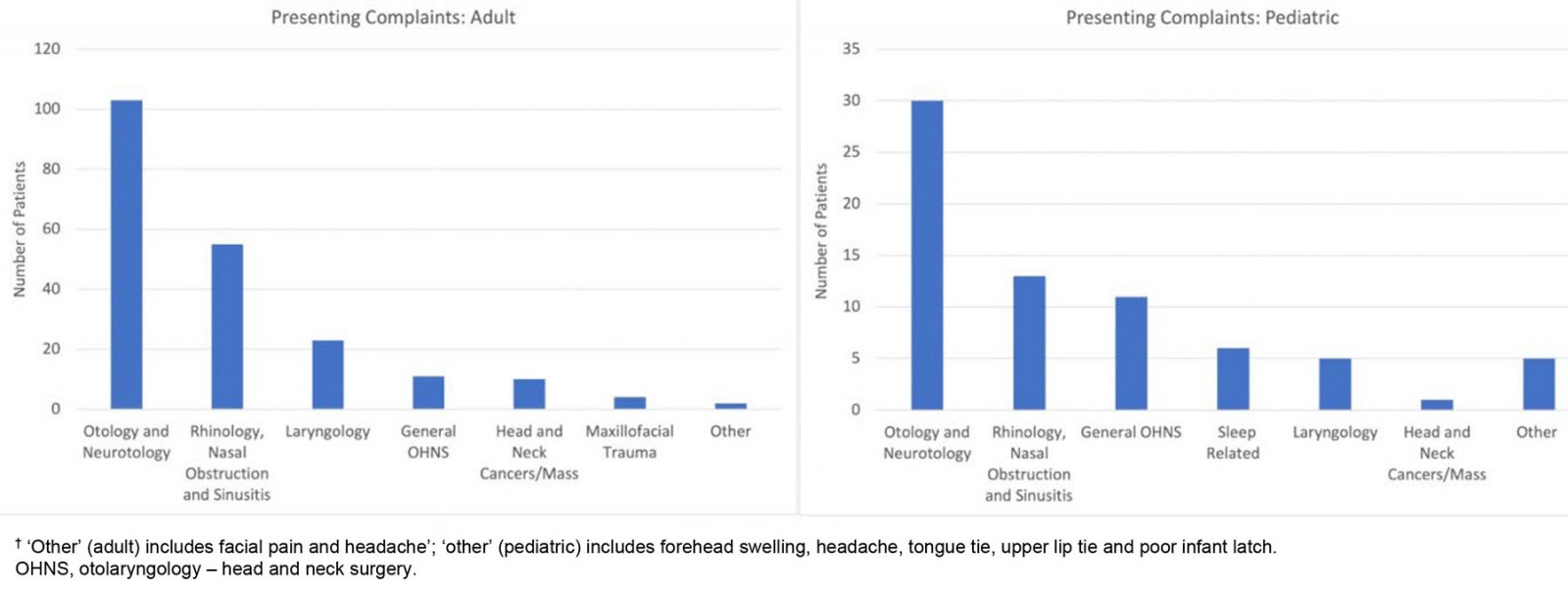 Figure 2: Presenting complaints (adults and pediatric)† at Meno Ya Win Health Centre otolaryngology clinic, March 2020 (n=154) and March 2021 (n=122).
Figure 2: Presenting complaints (adults and pediatric)† at Meno Ya Win Health Centre otolaryngology clinic, March 2020 (n=154) and March 2021 (n=122).
Comorbidities
Comorbidities were reported in 32% (n=23) of the pediatric patients and included diagnoses such as metabolic disorders (obesity and type 2 diabetes mellitus), inflammatory disorders (eczema), mental health disorders (attention deficit hyperactivity disorder, drug abuse), and congenital disorders (fetal alcohol syndrome, 22q11.2 deletion syndrome and cerebral palsy).
In contrast, comorbidities were reported in 66% (n=135) of the adult patients. The most commonly reported comorbidities were hypertension (n=34), type 2 diabetes mellitus (n=24), respiratory disease (chronic obstructive pulmonary disease, asthma; n=17), cancer (melanoma, non-Hodgkin lymphoma, osteosarcoma, breast carcinoma, gastric carcinoma; n=12), mental health disorders (anxiety, depression and substance use disorders; n=12), and musculoskeletal disorders (n=10). Gall bladder disease requiring cholecystectomy was identified in 10 adult patients.
Access to care
Nearly 30% (n=81) of patients traveled further than 150 km to access otolaryngology services at the Meno Ya Win Health Centre, and 5% (n=13) of patients traveled further than 250 km. The majority of the patients (n=172, 62.3%) reported a 3–6-month wait time to be assessed in the Meno Ya Win Health Centre otolaryngology clinic. However, due to time constraints, not all patients referred to the clinic were able to meet with an OHNS care provider as the consultation waitlist ranged between 300 and 500 patients. Wait times experienced by these patients were not considered. A summary of distances traveled and access metrics for general medical and otolaryngology services is presented in Table 2.
Table 2: Access to care for patients attending Meno Ya Win Health Centre otolaryngology clinic, March 2020 (n=154) and March 2021 (n=122)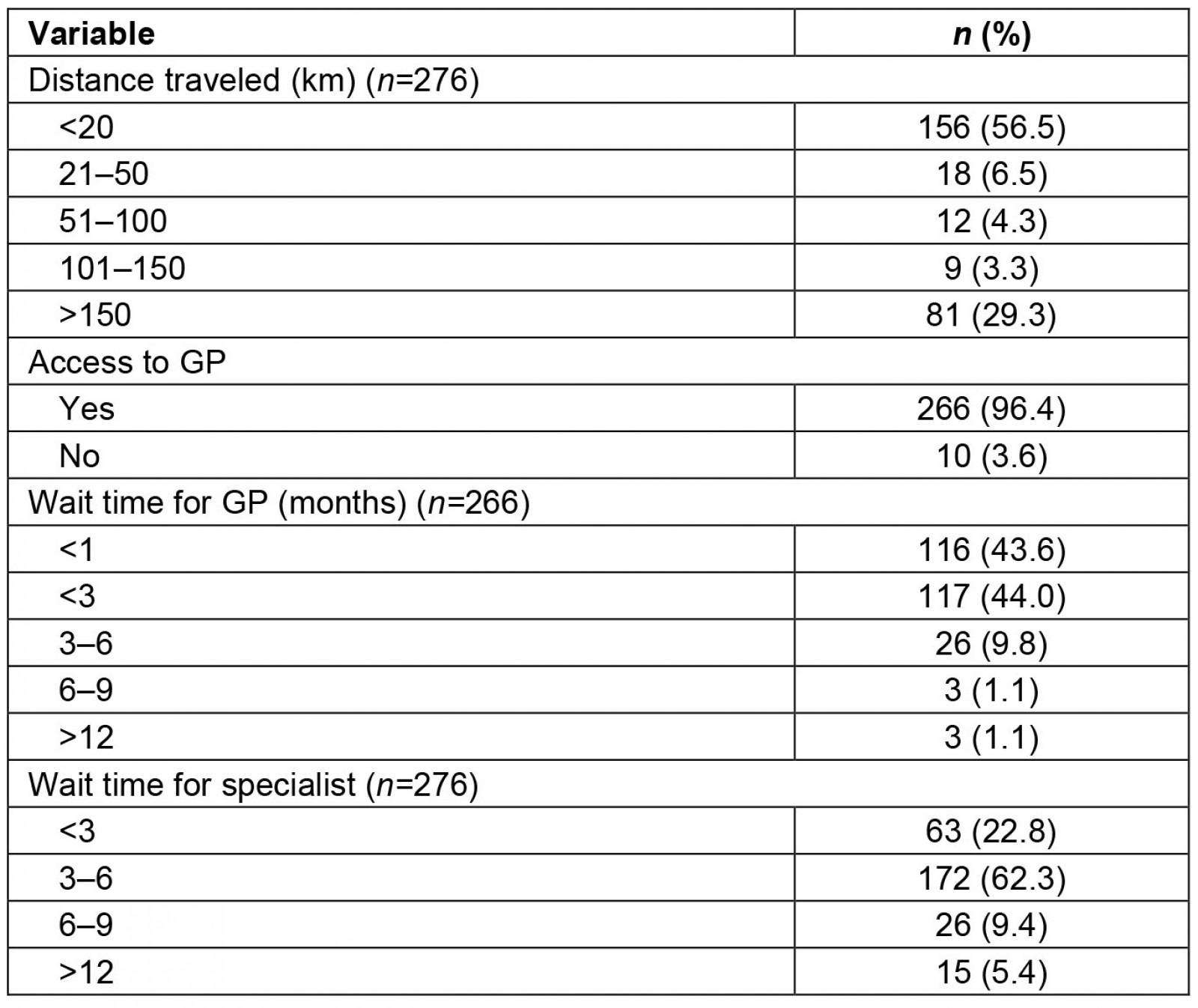
Lessons learned
The authors have expanded the concept of the ‘visiting’ otolaryngology provider to a visiting otolaryngology team with expertise in multiple subspecialty areas. This approach has facilitated the management of a wider variety of clinical presentations locally rather than reliance on the costly, multiple referrals to subspecialists at academic centers. The approach has also been instrumental in the building of professional relationships with local primary care providers, streamlining communication, and facilitating diagnostic and treatment planning. Key features of this project are relevant to the rural and remote context and may be used to inform similar programs for providing care in other specialties or other rural and remote areas.
First, the authors were able to identify common clinical complaints specific to rural and remote Northern Ontario and include subspecialty care providers as part of the visiting otolaryngology team to address these conditions. The findings of the current study and a previous Canadian study by Crowson and Lin3 suggest that otolaryngology expertise is needed in the areas of hearing loss and nasal obstruction in order to address common clinical complaints in rural/remote populations in Northern Ontario. Similarly, studies conducted in the US identified hearing loss, chronic ear disease and non-malignant sinonasal disease as the most commonly encountered otolaryngological conditions in rural and remote settings13,14, whereas studies in Australia noted a high prevalence of otitis media among rural children8,15. There are considerable differences between common otolaryngological complaints encountered in an urban setting compared to a rural/remote setting. The presence of a visiting otolaryngology team with subexpertise can be utilized to optimize patient outcomes.
Second, the implementation of a visiting otolaryngology team offers an effective solution to overcome geographical barriers to otolaryngology services. Although there is no permanent otolaryngologist, the Meno Ya Win Health Centre now has access to a visiting otolaryngology team comprising otolaryngologists with subspeciality training in otology, neurotology, rhinology, head and neck surgical oncology, and pediatric otolaryngology. For patients, travel from remote communities to urban centers for medical care is difficult and expensive, especially during the winter months. Coordination of air travel and accommodation is time consuming, requires considerable human resources for planning, and is costly for provincial government agencies. By having the OHNS team travel to the local community, the costs associated with patients traveling to urban centers to receive care are reduced.
The visiting otolaryngology team-based approach can similarly be implemented in other rural and remote communities without access to a permanent otolaryngologist. In a study that observed patient access to otolaryngology providers in Iowa, 59% of patients were located within a 30-minute driving distance of an otolaryngologist’s primary practice location, compared to 92% of patients living within a 30-minute driving distance of a visiting consultant clinic16. Significant geographical distances to health services may lead to reduced healthcare utilization, treatment effectiveness and overall health outcomes10,11,17,18. It has been reported in studies from Canada, the US and Australia that there is a significant trend of increasing otolaryngology providers located in urban centers and decreasing providers in rural or remote communities3,8,14,19. In an Australian study by Gunasekera et al, 33.3% of rural and remote practitioners reported no OHNS services available in their town, compared to 3.9% of urban practitioners8. There is a clear discordance between the prevalence of otolaryngologic disease and the availability of local otolaryngology services in remote and rural communities. The visiting otolaryngology team is able to address this challenge by traveling to the community to provide subspecialty care.
Third, the visiting otolaryngology team is able to provide timely subspecialty otolaryngology care to the local community. Physician shortages and limited access to specialists can result in longer wait times for appointments12,17,20,21. Rural and remote otolaryngology providers in Australia noted 14% of patients waited longer than 6 months for appointments compared to 11% for urban otolaryngologists8. Underserved and vulnerable populations are less frequently diagnosed with common otolaryngologic disorders and come to clinical attention with advanced forms of disease5. Delays in diagnosis and treatment for patients living in rural communities can lead to reduced survival rates for patients with head and neck22, and oral cancer23. In a study conducted among children living in Torres Strait and the Cape York region in Australia, the waitlist for OHNS surgery ranged from 11 months to 3.7 years, far exceeding the local health recommendations24. In a scoping review by Urban et al it was stated that ‘Many studies cited rural access to care as the reason for advanced disease progression and poorer outcomes’14. Timely and accessible otolaryngology services are needed in rural and remote communities to address population health needs.
The visiting team has engaged the community by contributing to continuing medical education activities, teaching medical students from the Northern Ontario School of Medicine, and collaborating with healthcare administrators to enhance clinic and operating theatre resources. This has also provided a learning opportunity to an otolaryngology resident to experience exposure to rural patient populations. Establishing a consistent presence at the Meno Ya Win Health Centre will provide an opportunity for outreach and collaboration with regional Indigenous communities that respects values and is culturally competent. Further studies such as satisfaction surveys of patients and local providers, wait-time quality assessments, and formal cost-effective analyses are required to fully quantify the benefit of the visiting team approach and to guide refinements in the model. The visiting otolaryngology team concept has also been regarded as an important strategy to address the increase in wait times for assessment and treatment caused by the COVID-19 pandemic. The increase in local wait times has been aggravated by backlogs currently facing the secondary and tertiary referral centres in Ontario and the moratorium on interprovincial otolaryngology services provided by Manitoba.
The key lessons learned from this study and care delivery model include that:
- it identified a significant need for otolaryngology specialty care in Northern Ontario
- directed investment in the visiting otolaryngology model should be informed by data that identifies common clinical complains, resource utilization trends and clinical outcomes
- the ‘visiting’ model provides important educational opportunities for local trainees and faculty. Moreover, it provides visiting trainees exposure to potential careers in rural and remote communities
- the psychosocial and economic impacts to the patient and family, such as delayed access to specialty care, and disruption due to travel and time away from home, were mitigated by the visiting model
- the visiting model has the potential to reduce the considerable financial burden on the healthcare system by reducing the costs associated with travel and lodging to urban centers.
Research gaps and future directions
There is a paucity of data regarding the demand for and availability of otolaryngology services in remote and rural areas of Canada. The data are required to inform healthcare providers and health resource administrators to address barriers to access, reduce wait times for care and improve health outcomes. The findings of this study can be used to identify specific otolaryngology needs and barriers to access to care. Furthermore, the data may guide healthcare providers and administrators on resource allocation and optimization of the delivery of otolaryngology services. A similar approach may be applied to different medical specialties in order to design a visiting team of medical providers who can provide subspecialty care that caters to the needs of rural and remote communities in Canada and other countries.
Conclusion
This project report describes a visiting otolaryngology team that provides OHNS services to a Northern Ontario community with the aim of providing accessible specialty care catering to treatment common clinical complaints. The study findings highlight the need for otology and rhinology services and the need to develop efficient and cost-effective otolaryngology delivery models to serve remote and rural communities in Canada and other countries. The data can be used to guide healthcare providers and administrators on resource allocation to optimize the delivery of otolaryngology services. Further studies are needed to define the benefit of a team approach for patients, local providers and healthcare delivery.
Acknowledgements
Sioux Lookout Meno Ya Win Health Centre acknowledges that it was built on the sacred land and traditional territory of the Lac Seul Ojibwe Nation. The authors acknowledge the contributions of our clinic nurses Kim Suprovich and Kim Coughlin for their commitment and invaluable contributions to the success of the otolaryngology clinic. The authors also thank Dr John Rutka for establishing the visiting otolaryngology clinic at the Meno Ya Win Health Centre, for numerous years of service to the community, and for supporting the team clinic approach.
Funding
The authors received no funding for this research.
Conflicts of interest
The authors declare no conflicts of interest for this study.

