Context
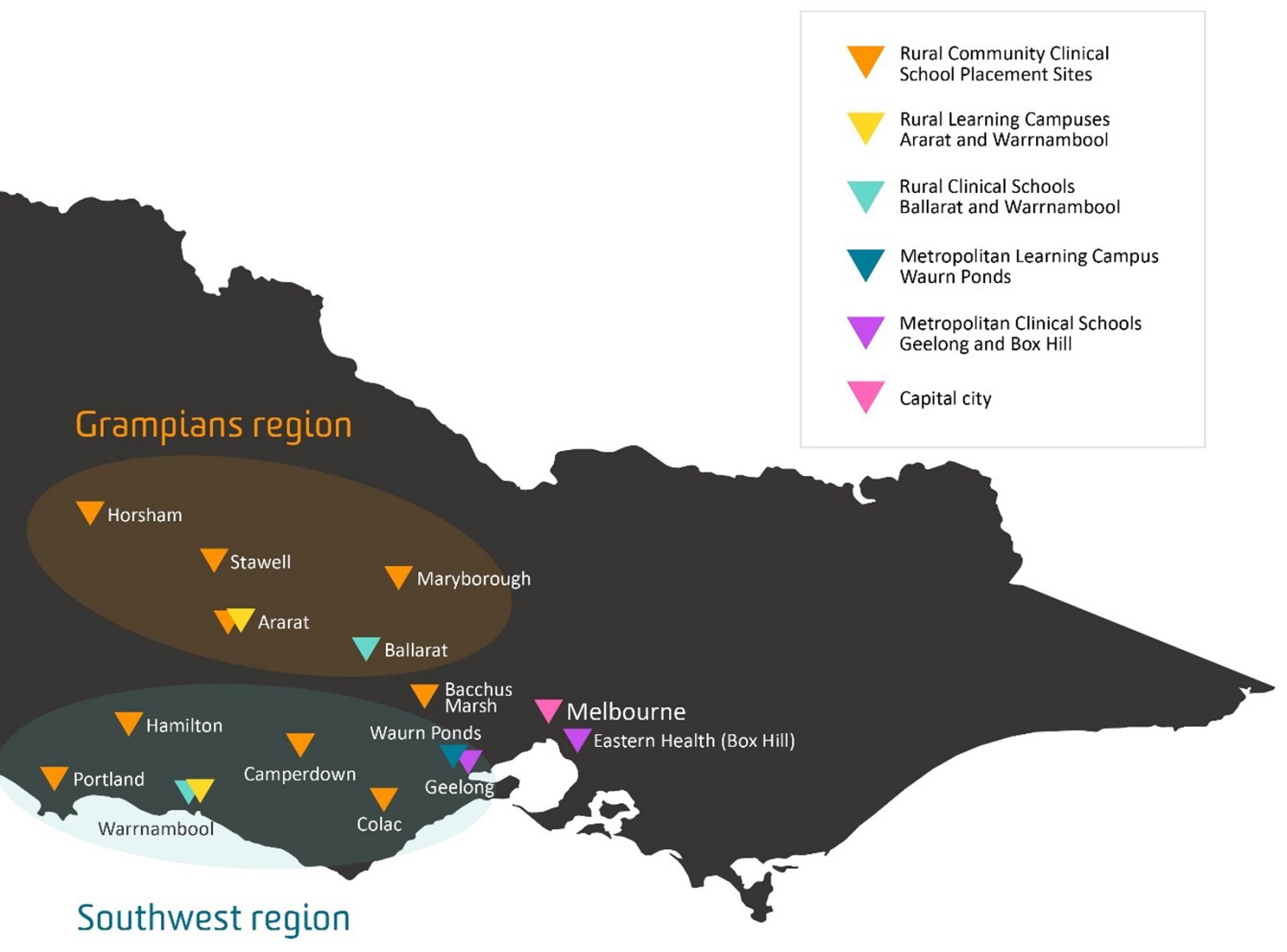
The Deakin University Medical School was established and designed to tackle rural workforce shortages in Western Victoria, Australia1. The school has three rural clinical schools (RCSs) based in this region, which is formally defined as the rural training footprint (Fig1)2. RCSs are an Australian Government initiative funded by the Rural Health Multidisciplinary Training program, providing clinical training for medical students in rural communities3. Our medical graduate tracking evidence, aligned with national data, demonstrates that RCS students are more likely to work rurally compared to medical students who have only undertaken metropolitan-based training4-6. Furthermore, emerging place-based education and return-to-region evidence demonstrate that medical students with a rural background who attend an RCS are more likely to work in rural areas, with training in or being from that region enhancing these outcomes4,7-9.
Our graduate tracking results provided valuable evidence supporting the need for a strategic change in our admission and training policies to enhance our rural workforce outcomes, especially in the rural training footprint. The culmination of this strategic direction was the implementation of a dedicated rural training stream (RTS) in 2022. Briefly, the RTS recruits 30 students with rural backgrounds annually, who commit to training within the rural footprint, with the explicit intention of becoming rural clinicians10. The RTS has a ‘grow your own’ philosophy that prioritises students from our rural training footprint and trains them in the same region2.
Deakin University’s 4-year Doctor of Medicine consists of 2 years of preclinical and 2 years of clinical training. Clinical school allocation is facilitated by a preferencing system. RTS students submit choices between the three RCSs. General Entry (GE) students can choose between all five clinical schools, with half of the RCS places available to these students. GE students come from a mixture of metropolitan and rural backgrounds.
Prior to the introduction of the RTS, students attended a clinical school information session held at their urban preclinical campus and had the opportunity to listen to presentations and meet representatives from each clinical school before submitting their preferences in their second year. Visits to RCSs were limited and arranged by prospective students themselves on an ad-hoc basis. One key missing decision-making element was an introduction to the surrounding rural community. Students take both clinical and non-clinical factors into consideration when contemplating clinical school preferences11,12.
To augment the introduction of the RTS, we created an innovative 3-day rural immersion program in year 1 (Fig2). The broad aim of the program was to provide students with practical experience and knowledge about the RCS environment, allowing them to make an informed clinical school preferencing decision that considers both their personal and learning needs. Despite delivering the same curriculum, each RCS has a unique clinical setting, community and program delivery. To showcase these individual aspects, each RCS designed a bespoke 3-day immersion program centred around three overarching themes:
- connecting students to the local Indigenous Country (of Wadawurrung, Eastern Maar and Gunditjmara Peoples)
- connecting students to the community
- connecting students to the clinical school.
The timing of clinical school preferencing was also moved to year 1 for the entire cohort. It was anticipated that this would provide students with certainty and facilitate the building of a connection with their allocated clinical school.
The immersion program has a capacity for 90 students and is conducted over 2 weeks (45 students per week). Students can attend only one RCS immersion, with the majority able to attend the RCS of their choice. Students who wish to visit more than one RCS are supported and encouraged to contact the clinical school and arrange a personal visit. To ensure that students who participate in the program do not miss learning opportunities, the required face-to-face tutorials for the week’s year 1 curriculum are facilitated locally by the RCS, which provides students with valuable experience of curriculum delivery at the clinical school.
All RTS students participate in the program, reflecting their commitment to undertake rural clinical training. Sixty places in the immersion are then available for interested GE students.
© Reproduced with permission.
Figure 1: Deakin University School of Medicine sites, Victoria, Australia.
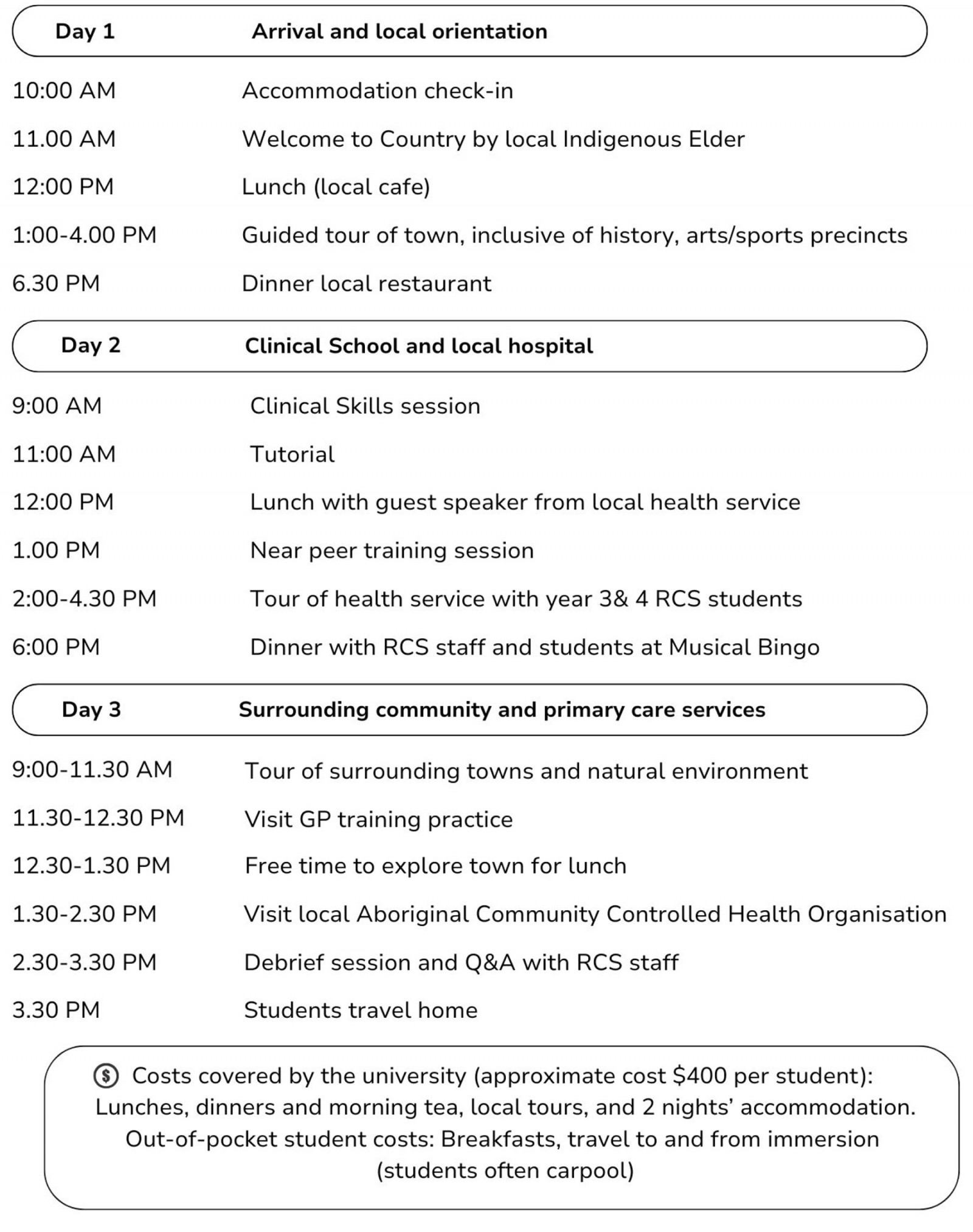 Figure 2: Indicative Deakin University Rural Clinical School immersion 3-day itinerary.
Figure 2: Indicative Deakin University Rural Clinical School immersion 3-day itinerary.
Issue
Given that RCSs were developed as a strategy to help mitigate the rural medical workforce maldistribution, effective management of this finite resource is required. As such, we are purposefully aiming to recruit students who wish to train and live in our rural footprint and, importantly, have the attributes to thrive in this environment professionally and personally.
Clinical school preferences have fluctuated annually, but the majority of students generally elect to remain at the larger years 1 and 2 urban training location (in Geelong). Students have often already relocated at the commencement of the Doctor of Medicine; therefore, they have embedded themselves in the community, established local networks, are familiar with the urban clinical school and may not wish to relocate or consider relocating again for clinical training. Arguably, students are preferencing what they know, urban clinical schools, without fully experiencing or considering the RCS option. As ‘you cannot be what you cannot see’ – we needed to provide an experience to engage students, ensuring a more informed clinical school preference.
There is limited information describing student RCS preferencing patterns. Previous studies have reported varied findings, with both under- and oversubscription to programs11-13. In one study, students who preferred metropolitan training primarily cited that their decision was based on perceived learning opportunities. In contrast, when asked about the major barriers to attending an RCS, common reasons were personal and practical, including family and partner commitments, transport and financial concerns12. An oversubscribed RCS identified students had three main reasons for wanting to attend the clinical school: belief in better learning opportunities in a rural area compared to metropolitan, being drawn to a rural area (often for personal reasons), and opportunities for personal development and life experience13.
Furthermore, our clinical schools have capacity constraints, so the highest preferences cannot always be accommodated, with the allocation of lower preferences not uncommon14. Therefore, providing students with the opportunity to gain a realistic understanding of the RCS environment was seen as a mechanism that may not only stimulate RCS preferences but also reduce any apprehension a student may have if they were allocated an RCS as a lower preference. Due to the requirement to meet minimum Australian Government rural training mandates, RCSs have conscripted students to fill quotas3,11,15. It has been suggested that students conscripted to an RCS may view the experience negatively, with one study finding that RCS students who did not preference it first felt that the placement contributed to lower levels of wellbeing, compared to students who had the RCS as their first preference15. Providing students with positive rural training experiences is important and fosters future rural work, with one RCS suggesting the voluntary nature of participation in their program is influential in achieving positive rural workforce outcomes9.
To contribute to the literature on medical students’ RCS preferencing decisions and to evaluate students’ perceptions of the immersion program, a survey was developed using Qualtrics (Qualtrics; https://www.qualtrics.com) and distributed on the final day of the program in 2022 and 2023. Of the 163 students who participated in the immersion (88 in 2022 and 75 in 2023), 115 students completed the survey (response rate 70.6%). Survey responses were submitted by 63 GE and 52 RTS students. Student survey responses were linked to their subsequent clinical school preferences and allocation.
Ethics approval
Ethics approval for this project was granted by the Deakin University Human Ethics Advisory Group (HEAG-H 101_2022).
Lessons learned
The program achieved its overarching aim of providing students with realistic exposure to the RCS environment, enabling students to make an informed decision about their clinical school preferences. Initially implemented as a pilot, this program has now become embedded within Deakin University’s Doctor of Medicine curriculum. Notably, the program was determined to be beneficial to both GE and RTS students alike, affirming RTS students’ decision to follow this dedicated rural training pathway and allaying GE students' fears and indecision about attending an RCS. This validated the decision to offer the program to all students regardless of their entry pathway, especially as 50% of the RCS cohort consists of GE students. The results demonstrate that the most significant changes in students' attitudes towards RCSs were associated with GE students.
Lesson 1: Students valued the program
Overwhelmingly, students responded positively towards the program, with no significant differences identified between GE and RTS responses. A total of 96.5% agreed the program was beneficial, 95.6% would recommend it to their peers, and 86.9% agreed that it helped them make an informed decision about their clinical school preferences.
Students were asked if the program allowed them to connect to the three overarching themes. Students overwhelmingly agreed this was achieved, with 96.5% agreeing the program helped them connect to the clinical school, 86% with the community and 77.4% with the Country.
Students were also encouraged to provide qualitative responses describing the most beneficial aspects of the program. Both RTS and GE students found the program beneficial:
The immersion experience was amazing! I enjoyed getting to meet the staff who I would be learning from and got a taste of life in the rural town I visited. This experience was an absolute privilege and has strongly affirmed my previous wishes to undertake my learning in a [RCS] location. (2023, RTS student)
Being able to see the hospital and get a taste of clinical years was fantastic, as was getting to see the facilities of the clinical school and hear about how the program is run. For me the most beneficial part was hearing the experiences of other students and getting a contrast of how [an individual RCS] compares to the other clinical schools. Ultimately, being able to hear what the program looks like from those who are going through it has helped me decide where will be right for me. (2023, GE student)
Lesson 2: The program changed students' perceptions of the Rural Clinical School
In the 2023 survey, we directly compared students' pre- and post-program RCS perceptions using a five-point Likert scale (Table 1). A significant positive shift was observed in students’ overall agreement regarding their intention to place the RCS they attended as their first preference, as well as their confidence that the RCS would be the right environment for them. There was a significant reduction in students' level of indecision about their clinical school preferences and hesitancy in the RCS environment. Perception changes were more apparent in GE students although, notably, RTS students also had a significant shift in their uncertainty about the RCS environment.
Table 1: Pre- and post-rural immersion program perceptions about rural clinical schools (2023 only)
| Perception (n=50)† | Pre-mean | Post-mean | Significance¶ |
|---|---|---|---|
| I am planning to preference the RCS I attended first. |
All 2.52 GE 3.20 RTS 1.80 |
All 1.96 GE 2.36 RTS 1.56 |
<0.001*** <0.001*** 0.18 |
| I am planning to preference another RCS first. |
All 3.74 GE 4.00 RTS 3.48 |
All 3.98 GE 4.08 RTS 3.70 |
0.116 0.723 0.083 |
| I am undecided about my clinical school preferences. |
All 2.86 GE 2.30 RTS 3.40 |
All 3.50 GE 3.20 RTS 3.80 |
<0.001*** 0.003* 0.067 |
| I am confident the RCS will be the best environment for me. |
All 2.28 GE 3.04 RTS 1.50 |
All 1.84 GE 2.2 RTS 1.44 |
0.001** 0.001** 0.491 |
| I am hesitant/ unsure about the RCS environment. |
All 3.30 GE 2.60 RTS 3.90 |
All 3.98 GE 3.64 RTS 4.36 |
<0.001*** <0.001*** 0.018* |
*p<0.05, **p<0.01, ***p<0.001
† Likert scale, agreement with statements: 1=strongly agree, 2=agree, 3=neutral, 4=disagree, 5=strongly disagree.
¶ Paired t-test.
GE, General Entry. RCS, Rural Clinical School. RTS, rural training stream.
Lesson 3: Balancing learning and personal needs
Another lesson learnt was the identification of factors students consider most important when deciding on their clinical school preferences. Answers were provided by free text and coded using content analysis to identify patterns of meaning in the data16. Student responses were inductively coded into two distinct categories: personal reasons and learning needs (Table 2). This aligns with previous research that found clinical school selection reasons primarily fell into two categories, which were labelled as ‘education’ and ‘social’12.
There was an even split between personal reasons (52.2%) and learning needs (47.8%). Interestingly, 65.5% of students who preferenced an RCS first nominated learning needs as their most important consideration. Another notable finding was that a higher percentage of RTS students (57.7%) nominated personal needs as their main consideration, compared to GE students (47.6%). This may reflect the RTS place-based learning philosophy, where students are recruited from the rural training footprint and therefore wish to be placed at an RCS close to their home community.
Table 2: Content analysis and examples of students' free-text answers about the most important considerations when selecting a clinical school
| Code |
All respondents (n=115) |
Preferenced an RCS first |
Examples of medical students’ free-text responses |
|---|---|---|---|
| Personal reasons |
60 (52.2) |
33 (55) |
|
| Learning needs |
55 (47.8) |
36 (65.5) |
|
RCS, Rural Clinical School.
Lesson 4: Positive impact of immersion on Rural Clinical School preferences but constrained by capacity
Student preferences are managed by a placement allocation software package, InPlace (Quantum IT; https://www.inplacesoftware.com). Preferences are submitted in order of most to least preferred. The aim is to match as many students as possible with their highest preference.
Of the medical school’s annual cohort of 140 students, approximately 60 attend an RCS in year 3 and 40 in year 4. As such, due to the capacity of each RCS, not all students received their first preference. All RTS students were allocated to an RCS, but only 57.7% (n=30) received their first preference. GE students were more successful in receiving their first preference (81%, n=51). Of these students 33% (n=17) placed an RCS first, with 14 gaining a place. This data prompted a review of the allocation procedure to develop processes aimed at increasing the percentage of RTS students allocated their first preference.
A promising finding was that, of the 66% (n=42) of GE students who initially felt hesitant about the RCS environment, 26.2% (n=11) placed an RCS as their first preference. Collectively, first and second preferences for RCSs increased compared to pre-immersion levels.
A limitation of this report is that preferencing outcomes are incomplete due to the absence of either students who did not attend the immersion program and may have preferenced an RCS first or of immersion participants who did not consent to participate in this research.
Translation of lessons learned
Deakin University Medical School’s 3-day rural immersion program in Victoria, Australia allowed students a unique glimpse into the Country, the community, and the clinical school, enabling them to make an informed choice regarding their clinical school preferences. This pilot program, now embedded in the year 1 curriculum, demonstrates the importance of genuine early exposure to RCS environments and the impact this can have on students’ perceptions and decisions regarding pursuing rural training. Earlier clinical school preferencing allowed students to extend on connections built during the immersion program, and this was noticed by RCS staff, who felt these students acted as ‘leaders’ and were ‘comfortable’ in the RCS environment when they returned in year 2 for the transition to clinical practice experience.
The lessons learned highlight that further work is warranted to review and develop clinical school selection policies and processes that mutually reflect both students’ and the university's needs. As our RTS grows and our strategically placed preclinical learning sites develop, we have a unique opportunity to monitor and further refine the preferencing and matching process. In line with our social accountability obligation and focus on place-based education, we are striving to provide students with the opportunity to remain in their rural community for the duration of the course. Therefore, where possible, RTS students should be matched to the RCS of their choice. The clear message from students is that training location is important, and an ongoing area of focus is building capacity in our rural training footprint to include opportunities for rural exposure for students at all year levels.
Acknowledgements
Rural clinical schools are an Australian Government initiative funded by the Rural Health Multidisciplinary Training program.
References
You might also be interested in:
2011 - Implications of increased student intake on rural rotations in Australian medical schools
2010 - Early childhood caries among Hutterite preschool children in Manitoba, Canada



