Introduction
After almost 4 years of being regarded as a global pandemic, COVID-19 is no longer a 'public health emergency of international concern'1. Marburg, monkeypox, ebola, chikungunya, zika, dengue and Rift Valley fever, among others, are threatening to replace the COVID-19 era2. During this era, the world witnessed the disruption of health systems3, more people were pushed into poverty4, and the lives of more than seven million people ended due to the virus5. To ensure that no one is left behind in the fight against future pandemics, WHO and other global partners have called for tailored and inclusive advocacy strategies to improve vaccine uptake6. One strategy includes ensuring unhindered access to vaccine information. However, operationalizing this call could be questionable, particularly where there are geographic challenges, such as in rural African settings.
In Africa, more than half of the population resides in rural areas7. The areas are usually characterized by poverty, limited access to public health information and essential medicines, and fragile healthcare systems 8,9. Unlike the urban population, less than a quarter of the rural population has access to internet connectivity in Africa10, and most rely on radio rather than television broadcasts for information11. Such characteristics place rural residents at a disadvantage as they are unable to enjoy the benefits of vaccines, which span from improved wellbeing to socioeconomic development. Moreover, tailoring vaccine advocacy strategies to the needs of rural residents is congruent with the International Covenant on Economic, Social and Cultural Rights, which reiterates ‘the right of everyone to the enjoyment of the highest attainable standard of physical and mental health’12. It also brings rural areas closer to achieving the third UN Sustainable Development Goal, which seeks to ‘ensure healthy lives and promote well-being for all at all ages’13.
As of 2024, approximately 62% of Sub-Saharan Africa's population resided in rural areas14, with Tanzania reporting 65% rural residency15. During the COVID-19 pandemic, Tanzania's complete vaccination rate reached only 54% (for both one and two doses of vaccines combined), compared to the global average of 67% as of December 202316. This disparity is particularly concerning given Tanzania's predominantly rural population and the continued emergence and re-emergence of infectious diseases and pandemics. Therefore, the study aimed to examine COVID-19 vaccination advocacy strategies in rural settings, specifically in Tanzania, that could be adapted to improve preparedness and response plans against future pandemics.
Methods
Study design
The study employed a case study design, integrating both qualitative and quantitative research approaches17. Combining these approaches mitigates the limitations of each and provides a comprehensive understanding of the studied phenomenon within its real-world context18. For this study, COVID-19 vaccination advocacy was the phenomenon of interest examined among rural communities in Tanzania.
Study area
Both the qualitative and quantitative phases were conducted in the Geita region in Tanzania due to the reported low vaccination uptake in 202119. The region is located in Lake Zone (north-western Tanzania) with a population density of 28/km², and 84% of its people reside in rural areas, most of whom are farmers20. The region is made up of five administrative districts (Bukombe, Chato, Geita, Mbogwe, and Nyang'hwale).
Study population
Participants of the qualitative phase were grouped as follows:
- supply side, responsible for delivery of COVID-19 vaccine information to the community, encompassing community health workers, local leaders, and healthcare workers
- demand side, comprising consumers or target beneficiaries of the COVID-19 vaccine information, here identified as influential people (included religious leaders and the elderly).
Participants of the quantitative phase (or respondents) were the heads of selected households.
Sample size
For the qualitative phase, the sample size was dictated by subsequent collection and analysis of the participant information. For the quantitative phase, the sample size was calculated before data collection using the formula developed by Daniel21. Assumptions were as follows: Z-score of 1.96 (two-tailed tests), 95% confidence level, unknown proportion of heads of household residing in rural villages with access to COVID-19 vaccine information, 5% margin of error and a design effect of 2 for multiple sampling designs was deployed in selecting heads of household. Therefore, the potential minimum sample size was 853 individuals after considering the assumed non-response rate of 10%.
Sampling procedures
Purposive sampling with maximum variation was used to select participants for the qualitative phase22. This ensured the experiences of multiple stakeholders with different responsibilities during COVID-19 vaccination advocacy (supply and demand side) were taken into account. Thus, the supply side was those responsible for delivering information about the COVID-19 vaccine, and the demand side was those receiving information. Geita district, which is rural, was purposively selected with the assistance of the regional and district COVID-19 response team leaders based on low vaccine uptake. The qualitative sample size was determined by thematic saturation, that is, when no new themes emerged from the analyzed data23.
For the quantitative phase, a multistage sampling technique was deployed. Sampling began at the district level within the Geita region. Stage 1 involved a simple random selection of two districts in Geita region (the selection excluded the Geita district involved in the qualitative phase). In stage 2, a simple random sampling was used to select three wards from each district. In stage 3, a simple random sampling was used to select three villages from each ward. This resulted in 18 villages selected as enumeration areas. In stage 4, each selected village was considered a cluster and each head of household was recruited depending on availability. The ratio of proportion to sample size was used to compute the total number of heads of household needed per village. Eligible respondents must have lived in the rural area for at least 3 years and be aged not less than 18 years. Those who perceived their health status as an impediment to participate in the study were excluded.
Data collection tools and procedure
In-depth interviews and questionnaires were used to collect qualitative and quantitative data respectively. In-depth interviews were accompanied by semi-structured interview guides tailored to participants of both the supply side and demand side. The interview guides were divided into two sections: the participants' demographic characteristics and then questions about approachability, acceptability and availability of COVID-19 vaccine information among rural communities, as indicated by Lévesque et al’s access framework24. The main questions were followed up with probing questions to elicit further or clarify participant responses. Interview guides were then shared with experienced qualitative researchers and a village leader for more input before data collection. In-depth interview participants were identified through their local leaders or the COVID-19 response team leaders at the village level. Participants were then invited for face-to-face in-depth interviews at a place of their choosing. All interviews were recorded using a digital audio-recorder and then stored on a password-protected digital file. A notebook was used to capture non-verbal cues during interviews or summarize the discussion. Some potential participants declined to be interviewed due to fear of political repercussions despite being assured of the confidentiality of all collected information. Interviews were conducted by the principal investigator and Hamis Bakari (research assistant) between 24 August and 3 September 2022. All interviews were conducted in Swahili language, which is widely spoken in the area.
For the questionnaire, closed-ended questions were developed from the analyzed qualitative data, with sections similar to those of the interview guide. Most questions had ‘yes’, ‘no’, ‘don't know’ or ‘no response' options and a few questions were structured based on a five-point Likert scale. The questionnaire was administered by trained research assistants (interviewer-administered) through the Kobo Toolbox. Kobo Toolbox is a web-based/application that assists in capturing and storage of data, advantageous for data collection in areas that have unstable internet connection25. For this phase, data was collected between 18 and 29 November 2024. The questionnaire was administered in Swahili.
Data analysis
This study is part of a large project on access to COVID-19 vaccine information among rural communities, conducted in both Kenya and Tanzania. This article reports on the analysis of the data collected from Tanzania. Thematic and descriptive analysis were deployed to analyze qualitative and quantitative data respectively.
Inductive and deductive methods were adapted for thematic analysis in developing themes. Inductive analysis involved using the participants' quotes to develop themes; for deductive analysis, codes and subthemes were developed by comparing the participants' quotes with existing literature or frameworks, including Levesque's access framework24. Thematic analysis began with verbatim transcription of audio recordings and then re-reading the transcripts to understand participants’ perspectives about access to COVID-19 vaccination strategies. This was followed by a deductive or inductive grouping of patterns of information based on their similarity to generate subthemes and themes. The coding process was aided by MAXQDA software v20.4.0 (MAXQDA; https://www.maxqda.com). Quantitative data were descriptively analyzed and presented using frequency tables, whereby categorical data is presented using frequency and proportions and continuous data using means and standard deviation. Descriptive analysis was conducted using Stata SE v18.0 (StataCorp; https://www.stata.com).
Ethics approval
The study sought ethics approval from the ethics committee of the Muhimbili University of Health and Allied Science (MUHAS-REC-06-2022-1207) and the National Health Research Ethics Committee (NIMR/HQ/R.8a/Vol.IX/4710). In addition, written consent was obtained from each participant. The consent form included information about the study, what would be expected from the participants, the study duration, benefits, risks and voluntariness. Audio information, transcripts and survey data were kept in a password-protected folder only accessible to the principal investigator.
Results
Presentation of results
Since the results originate from a mixed research approach, a weaving approach is used to present both qualitative and quantitative results. This approach allows the presentation of qualitative and quantitative data under a single concept or theme26.
Demographic characteristics of study participants and respondents
Table 1 and Table 2 present the demographic characteristics of individuals who participated in the qualitative and quantitative phases respectively. Briefly, the qualitative phase included 20 in-depth interview participants, most of whom were male, married, had primary education, were unemployed and had never been vaccinated against COVID-19. The quantitative phase included 901 survey respondents, most being female (63.6%), married (81.9%), had completed primary education (47.3%), were employed (93.8%), and had never been vaccinated against COVID-19 (77.3%).
Table 1: Demographic characteristics of qualitative phase participants
| Participant number | Characteristic | Variable |
Supply side (HCW, CHW, local leaders) (n(%)/mean±SD) n=13 |
Demand side (influential people) (n(%)/mean±SD) n=7 |
|---|---|---|---|---|
| 1 | Gender | Female | 5 (38) | 2 (29) |
| Male | 8 (62) | 5 (71) | ||
| 2 | Age (years) | 41.8±13.1 | 52.1±7.6 | |
| 3 | Marital status | Married | 7 (54) | 6 (86) |
| Not married | 6 (46) | 1 (14) | ||
| 4 | Education status | Primary | 6 (46) | 7 (100) |
| Secondary | 4 (31) | 0 | ||
| Certificate | 2 (15) | 0 | ||
| Diploma | 1 (8) | 0 | ||
| 5 | Employment status | Unemployed | 6 (46) | 4 (57) |
| Self-employed | 3 (23) | 3 (43) | ||
| Employed | 4 (31) | 0 | ||
| 6 | Vaccinated against COVID-19 | No | 5 (38) | 7 (100) |
| Yes | 8 (62) | 0 | ||
| 7 | Household possesses radio | No | 3 (23) | 2 (29) |
| Yes | 10 (77) | 5 (71) | ||
| 8 | Household possesses TV | No | 8 (62) | 5 (71) |
| Yes | 5 (38) | 2 (29) |
CHW, community health worker. HCW, healthcare worker. SD, standard deviation.
Table 2: Demographics and perceptions of quantitative phase participants
| Participant number | Characteristic | Variable | Frequency (%/mean±SD) n=901 |
|---|---|---|---|
| 1 | Gender | Female | 573 (63.6) |
| Male | 328 (36.4) | ||
| 2 | Age (years) | 36.5±12.7 | |
| 3 | Marital status | Married | 738 (81.9) |
| Not married | 163 (18.1) | ||
| 4 | Education status | Never went to school | 112 (12.4) |
| Did not complete primary school | 158 (17.5) | ||
| Primary | 426 (47.3) | ||
| Did not complete secondary school | 68 (7.6) | ||
| Secondary | 107 (11.9) | ||
| Above secondary | 30 (3.3) | ||
| 5 | Employment status | Unemployed | 10 (1.1) |
| Self-employed | 46 (5.1) | ||
| Employed | 844 (93.8) | ||
| 6 | Household size | 5.1±2.7 | |
| 7 | Household possesses radio | No | 419 (46.5) |
| Yes | 482 (53.5) | ||
| 8 | Household possesses TV | No | 647 (71.8) |
| Yes | 254 (28.2) | ||
| 9 | Ever been infected with COVID-19 | No | 895 (99.3) |
| Yes | 6 (0.7) | ||
| 10 | Had friends/family member who was infected with COVID-19 | No | 893 (99.1) |
| Yes | 8 (0.9) | ||
| 11 | Vaccinated against COVID-19 | No | 695 (77.3) |
| Yes | 204 (22.7) | ||
| 12 | Name of COVID-19 vaccine received | Johnson and Johnson | 32 (15.7) |
| Others | 36 (17.6) | ||
| Don’t know | 136 (66.7) | ||
| 13 | Considered themselves knowledgeable about the COVID-19 vaccine | No | 548 (61.8) |
| Yes | 339 (38.2) | ||
| 14 | Village information outreach points | Village gatherings | 371 (41.2) |
| Vijiwe | 176 (19.5) | ||
| Household visit | 30 (3.3) | ||
| Religious gathering | 46 (5.1) | ||
| Healthcare facility | 247 (27.4) | ||
| Other | 7 (0.8) | ||
| No response | 24 (2.7) | ||
| 15 | Type of COVID-19 vaccine information communicated | COVID-19 vaccine reduces the risk of acquiring COVID-19 | 521 (57.8) |
| COVID-19 vaccine reduces the risk of advanced infection of COVID-19 | 239 (26.5) | ||
| COVID-19 vaccine is safe | 97 (10.8) | ||
| Other (including no response) | 44 (4.9) | ||
| 16 | Thought the information about why they needed to be vaccinated was ... | Very difficult | 49 (5.4) |
| Difficult | 440 (48.8) | ||
| Easy | 311 (34.5) | ||
| Very easy | 89 (9.9) | ||
| No response | 12 (1.3) | ||
| 17 | Physically reached out to COVID-19 advocacy team for more information | Yes | 157 (17.4) |
| No | 735 (81.6) | ||
| No response | 9 (1.0) | ||
| 18 | How often the COVID-19 advocacy teams visited the village | Every day | 18 (2.0) |
| Once a week | 307 (34.1) | ||
| Not more than three times a week | 95 (10.5) | ||
| More than three times a week | 68 (7.6) | ||
| No response | 413 (45.8) | ||
| 19 | Preferred time of day for village households to be visited | Morning hours | 59 (6.6) |
| Afternoon hours | 521 (57.8) | ||
| Evening hours | 311 (34.5) | ||
| Others | 3 (0.3) | ||
| No response | 7 (0.8) | ||
| 20 | Preferred time of year for village households to be visited | Spring | 27 (3.0) |
| Summer | 815 (90.4) | ||
| Autumn | 41 (4.6) | ||
| Winter | 6 (0.7) | ||
| No response | 12 (1.3) |
SD, standard deviation.
Description of results (by weaving approach)
Individuals at risk for COVID-19 required information about the vaccine. The ease with which COVID-19 vaccine information could be approached was defined by the village information outreach points, the preferred timing for advocacy, and the information communicated. Thus, each of the three elements represents a key strategy to improve vaccination advocacy in rural settings (Fig1).
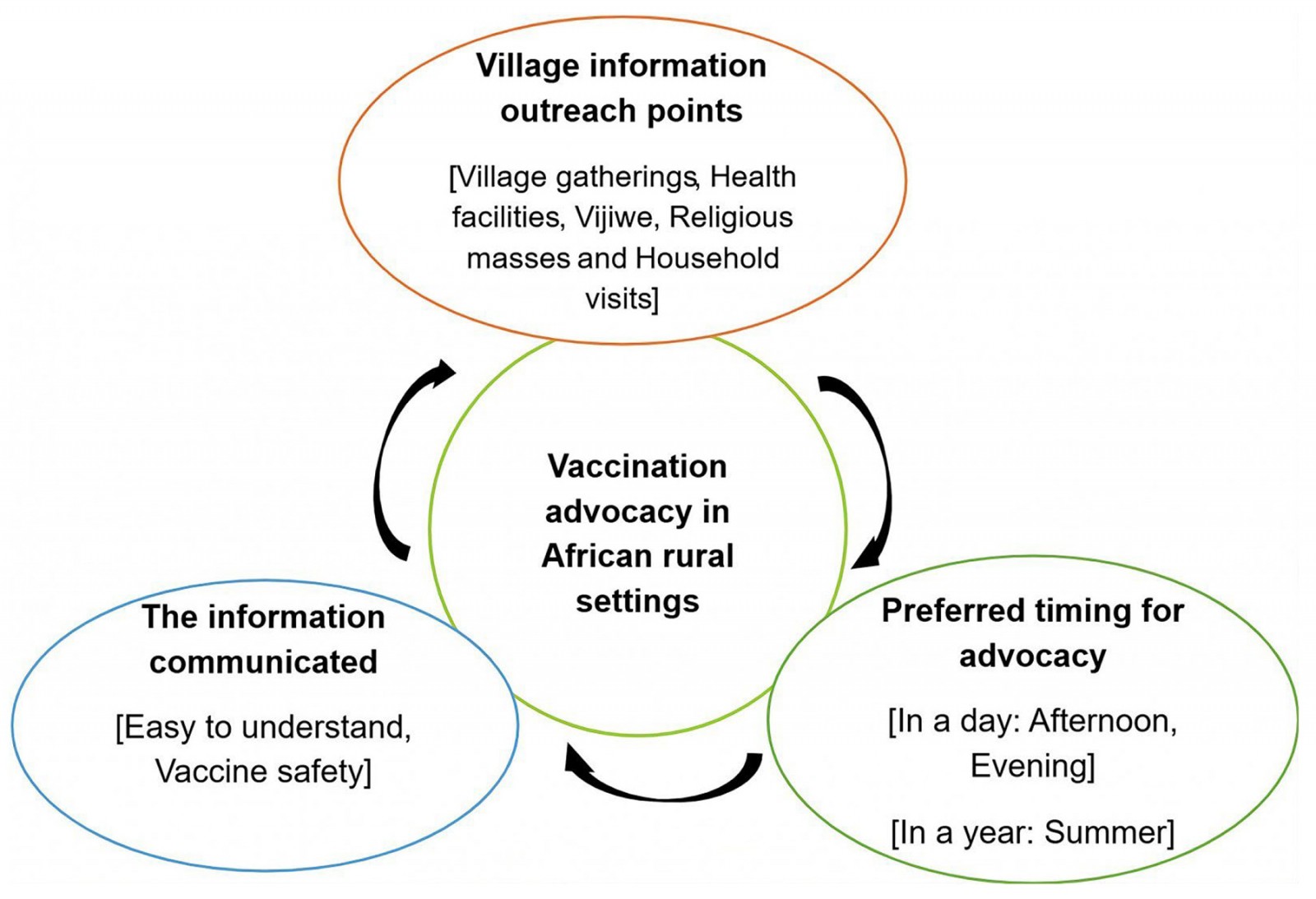 Figure 1: Vaccination advocacy strategies in African rural settings
Figure 1: Vaccination advocacy strategies in African rural settings
Village information outreach points
Regarding outreach activities, participants reported COVID-19 information was shared during village gatherings, small groups of people called vijiwe in Swahili, religious masses and household-to-household visits. Although village gatherings were organized with the sole intention of informing people about the COVID-19 pandemic and the vaccine, the intention was not made explicit during public announcements due to the concern that most of them would not attend. Most quantitative respondents (41.2%) reported having obtained COVID-19 vaccine information at village gatherings, followed by healthcare facilities (27.4%). COVID-19 vaccine information at the village level was also shared through vijiwe. Vijiwe helped reach out to young adults and elderly men in the village. For the quantitative phase, 19.5% of the respondents received COVID-19 vaccine information through vijiwe.
Other than village gatherings and vijiwe, religious gatherings were avenues used to inform people about the COVID-19 pandemic and vaccines. Participants noted that religious leaders encouraged people in hygiene practices such as handwashing and to avoid overcrowded places. However, after the introduction of the vaccine, religious leaders became divided on whether they should encourage their followers to also be vaccinated. Religious scriptures were used by religious leaders who decided to advocate for COVID-19 vaccination in their community. One religious leader said that:
Religion has a big role ... we return to scriptures that say the problem is my people lack knowledge. (Influential person 1)
For the quantitative phase, only 5.1% of surveyed respondents reported having obtained COVID-19 vaccine information through a religious gathering.
Some participants reported receiving COVID-19 vaccine information via household visits conducted by COVID-19 advocacy teams in the village. The vaccination team comprised a community health worker, a nurse, a records person, and the team was accompanied by a local leader. Upon arriving at the household, the vaccination team members would introduce themselves, explain the purpose of the visit and ask members of the household if they wished to be vaccinated. Participants noted that household visits were a confidential way of reaching out to people living with HIV who could not come to the clinic. They also reached out to people who could not attend village gatherings, as noted by one of the healthcare workers:
Calling people for village meetings was a challenge so, we went door to door, house to house. (Healthcare worker 2).
For the quantitative phase, 81.6% of the respondents never physically contacted the COVID-19 advocacy team for more information about COVID-19 vaccines. Only 3.3% of the respondents reported having been visited by COVID-19 advocacy teams in their homes.
Preferred timing for advocacy in village settings
Qualitative participants noted that it was important to consider the timing of COVID-19 vaccine advocacy campaigns. Early mornings or late evenings were deemed by participants as the appropriate time to carry out advocacy campaigns because it was the only time when the villagers were in their houses. Most farms were said to be at a far distance from the village, which made it difficult to find people in their homes during the daytime. This was partly corroborated by most quantitative phase respondents (57.8%) who preferred being visited in the afternoon hours, followed by evening hours (34.5%). One of the qualitative participants noted that:
... we are in a village and someone wakes up to go to the field [farming] at 6 am, others wake up at 5 am ... for example those who farm distant fields. (Influential person 7)
Apart from considering day hours, participants also indicated the need to consider agricultural or farming seasons. During the rainy season (March to May), most people would spend a lot of time preparing their agricultural fields and planting crops. During autumn, most of them would be harvesting their crops. Both seasons were regarded as not perfect for conducting COVID-19 advocacy campaigns. A similar perception was held by nearly all quantitative respondents (90.4%), who instead preferred advocacy campaigns to be held between June and August every year. To cement this, one of the participants in the qualitative phase said that:
… during the summer, people have long breaks and have no other work to do … in the fall, people go to work [farming]. (Local leader 1)
Information communicated
The type of information shared with the community was also considered to affect the approachability of COVID-19 vaccine information. Participants noted that the villagers could choose whether or not to get vaccinated based on what information was communicated. However, some participants reported refusing to be vaccinated because they felt they had not received enough information about COVID-19 and its vaccine. One of the local leaders noted that:
... I was not informed, but if I could have been informed, I would have been vaccinated [against COVID-19]. Because what you need is understanding and certainty. (Local leader 1)
For the quantitative phase, only 38.2% of respondents considered themselves well informed about COVID-19 vaccines. Just over 10% of the respondents reported having been informed about the vaccine’s safety during advocacy campaigns. The information communicated by advocacy teams about why someone needed to be vaccinated was considered difficult to understand by 48.8% of the respondents.
Discussion
The success of vaccination advocacy in rural communities hinges on three key factors: strategic outreach points, appropriate timing, and the clarity of information disseminated. Despite the implementation strategies used in the Geita region, only 8 out of 20 participants and 204 out of 901 respondents reported being vaccinated, which is an indication of the difficulty of COVID-19 vaccination advocacy in such settings.
Evidence about the low rates of COVID-19 vaccination among rural residents compared to their counterparts is accumulating27,28. Low vaccination rates in Africa have been exacerbated by widespread infodemics29. Partly, the aforementioned claim could be similar to findings of this study, whereby most respondents reported being unvaccinated against COVID-19 and uninformed about the vaccine. Village gatherings, vijiwe, household visits, religious gatherings, and healthcare facilities provide reasonable grounds to advocate for vaccination. However, the proposed outreach points are not to be assumed as one-size-fits-all. Disentangling which among these outreach points could ensure immediate access to vaccination information in rural settings demands a bottom-up approach to community engagement30,31. For example, in Sub-Saharan Africa, where the health system is characterized by the unequal distribution of health care, and lengthy travels (more than 3 hours) to access it, opting for healthcare facilities as outreach points could be problematic32. That is, the use of village healthcare facilities or posts as outreach points for advocacy may only be reasonable if the facilities are in proximity and physically accessible. Similarly, the use of village gatherings as a means to communicate vaccination information is dictated by how accountable political and local leaders are to their people, and the people’s trust in their leaders. It should be noted that some political and local leaders were labelled as perpetuators of mistrust and against COVID-19 vaccination during the pandemic, especially in Africa33,34. So, in the absence of trust between leaders and their community, the use of community gatherings would be unproductive.
Using vijiwe is an informal and less-demanding advocacy strategy that can be used among rural communities. Usually, a small group of people from the same community meet in an open space to discuss anything of interest while enjoying coffee, alcohol or playing scoring games among others. The discussion could be assumed to be a multi-directional communication where everyone is an active participant. Vijiwe are similar to other traditional means of communication used to pass on important information through storytelling35. However, vijiwe risks being the reservoir for an infodemic, especially during outbreaks. This could be lessened by devising means to synchronize the modernity of public announcements with Indigenous ways of communication that may influence vijiwe36,37. Correspondingly, exploratory studies are needed to corroborate the role of vijiwe in implementing community advocacy campaigns in rural and urban areas.
Apart from being cognizant of village outreach points, the timing of advocacy is equally important. Choosing either of the outreach points explained previously dovetails with the timing. Afternoon and evening hours were identified as the perfect time for reaching out to people regarding COVID-19 vaccine information. In the morning, most villagers would leave their houses to farm and return in the afternoon or evening hours. Visiting the households in the morning risks finding those who are sick, elderly or children at home – but not the household’s income-earners. In African culture, most heads of households are the income-earners and make final decisions about the health of people under their care. Part of such decisions could include whether or not a household member should be vaccinated38. Similar to challenges engrained in household visits, calling for a village gathering in the morning hours is unfeasible. In a year, the summer months between June and August were deemed the most appropriate periods for advocacy by both qualitative participants and quantitative respondents. From June to August, it is usually a dry season with minimal farming activities, so most people stay at home all day. This could be the perfect timing for household visits and reaching out to households that would otherwise be left out during the rainy seasons. Moreover, using vijiwe would be a more convenient advocacy strategy since most people could be spending more time outdoors. Literature about the influence of geographical seasons on vaccination advocacy is scarce or non-existent, but this study's findings provide a starting point for future research.
Planning for village outreach points and the timing for advocacy could be hampered by how the third key element is executed, the nature of information communicated. Based on the findings of this study, few people were informed about vaccine safety and nearly half found it difficult to understand the vaccination advocacy information. Similarly, other scholars have noted that concerns about vaccine safety and the unwillingness to be vaccinated are more prevalent among rural than urban residents39. Addressing these concerns necessitates implementing a bottom-up community engagement approach, whereby all vaccine safety concerns and myths are communicated and addressed with the involvement of the community: vaccination co-advocacy. This stance is equally stressed by the 2023–2025 WHO COVID-19 Strategic Preparedness and Response Plan40. Upholding vaccination co-advocacy could help to ensure easy understanding of the communicated vaccine information by targeted beneficiaries residing in a given rural setting.
Limitations
The findings presented by this article should be interpreted and discussed in light of the study's limitations. Social desirability by participants both in the quantitative and qualitative phases might have influenced some of the responses, especially on reporting whether or not they were vaccinated against COVID-19. Because the region where this study took place reported low vaccination uptake, some of the participants might have reported ‘not vaccinated’ to align with the general community. To mitigate the situation, researchers reiterated upholding confidentiality of shared information during the consenting process and emphasized honest responses. Recall bias during the quantitative phase is another limitation that should be considered when interpreting the study findings. We conducted the quantitative phase 3 years after the initiation of mass vaccination campaigns in Tanzania, that is, in September 2021. Thus remembering actual details might have been difficult for some of the participants.
Conclusion
Global initiatives to ensure that no one is left behind in the fight against pandemics could be hampered if narrow attention is paid to populations residing in rural areas. Focusing on information advocacy strategies responsive to rural settings, especially in Africa, is crucial. Village outreach points, timing and information communicated are key elements that should be considered during vaccination advocacy in rural settings. Undervaluing the three advocacy strategies could limit accessibility to vaccination information and subject rural communities to harm from vaccine-preventable diseases like COVID-19, ebola and Marburg, among others. These findings offer key lessons for designing future pandemic preparedness and response plans.
Acknowledgements
We sincerely thank all the participants and respondents who spared their valuable time and efforts to participate in this study. Moreover, we appreciate research regulatory bodies including the MUHAS-Research Ethics Committee and the National Health Research Ethics Committee for reviewing and approving this study. On the same note, we thank the President's Office for Regional Administration and Local Government and village gatekeepers for granting us permission to conduct the study. Lastly, we are grateful for all our research assistants who aided the data collection.
Funding
The study was funded by the East African Community Regional Center of Excellence for Vaccines, Immunization, and Health Supply Chain Management through the University of Rwanda (grant number: RCE-VIHSCM 009/2022) which aided the quantitative phase. The Amne-Salim COVID-19 research fund aided data collection during the qualitative phase. It should be noted that the funders had no influence in the study design, implementation and manuscript writing. Therefore, all the writings do not necessarily represent the position or opinion of the funders or the host institutions.
Conflicts of interest
There are no conflicts of interest to declare.


