Introduction
Stroke is the second leading cause of mortality and disability, following ischaemic heart disease, in Australia and contributes to significant health expenditure1,2. Atrial fibrillation (AF) is a strong risk factor for ischaemic stroke and increases risk of stroke by five times3,4. Antithrombotic therapy is the cornerstone of stroke prevention in AF, and reduces AF-related risk of stroke by two-thirds5.
The CHADS2 (congestive heart failure, hypertension, age≥75 years, diabetes and stroke) score is a relatively simple and well-validated risk stratification scoring system used for stroke prediction in patients with AF in relation to the decision of whether to anticoagulate3,6. A score of 0 is low risk, 1 point is moderate risk and >2 is high risk7. However, there are limitations in the CHADS2 score in relation to low risk score, as anticoagulation is not recommended for low-risk patients, and for score 1 either antiplatelet or anticoagulation therapy can be considered8. The European Society of Cardiology and Asia Pacific Heart Rhythm Society proposed CHA2DS2-VASc in 2010 to better identify patients at a truly low risk7. The CHA2DS2-VASc score can be considered an extension of the CHADS2 assessment by considering additional stroke risk factors – vascular disease, age 65–75 years and sex – that may influence a decision whether or not to anticoagulate9. The HAS-BLED (hypertension (ie uncontrolled blood pressure), abnormal renal/liver function, stroke, bleeding history or predisposition, labile INR (if on warfarin), elderly (e.g. age >65, frail condition), drugs (e.g. aspirin, NSAIDs /alcohol concomitantly)) scores are used to assess risk of bleeding in AF patients10.
Stroke prevention is receiving more attention, with a recent South Australian publication reporting increasing numbers of patients having experienced embolic strokes11. Few studies have examined stroke risk factors in South Australia 11,12 and it is unclear from this incidence study how many of these strokes could be prevented by appropriate anticoagulation. The primary aim of this study was to examine current stroke prevention management practices for patients with diagnosed AF and to identify gaps in current practice in a rural town of South Australia. The secondary aims were to identify whether patients with AF are receiving anticoagulation in accordance with stroke risk and also whether the decision not to anticoagulate is in accordance with the HAS-BLED score.
Ceduna is a remote rural town on the west coast of South Australia, with a population of 4000 people. Ceduna is located over 750 km from Adelaide, and 400 km from other regional centres. A significant proportion of the population (20–30%) are Indigenous people. Ceduna encompasses a diverse range of small communities and large farming properties, with agriculture and fishing representing the largest proportion of the local workforce. There are two medical practices in Ceduna, and a 15-bed general practice hospital. There are no onsite laboratory or radiological services. The catchment of the Ceduna District Health Services includes communities approximately 500 km to the north and west.
Methods
This retrospective cohort study included all patients with AF or atrial flutter (AFL) who were admitted at Ceduna District Health Services from 1 June 1 2008 to 30 July 2013. Patients with valvular or non-valvular AF or AFL were identified by the presence of primary or secondary diagnosis with an ICD-10-CM code at the time of discharge. Patients diagnosed with AF as their primary (presenting) or secondary (AF was included in discharge summary or current illnesses) complaint were included. The hospital records of all these patients were identified and reviewed.
There was no direct contact with the patient, and confidentiality and privacy were maintained. The date of the first qualifying AF diagnosis, either primary or secondary, during the study period was designated as the index date and then followed up on further admissions. These further admissions were not included in the total number of patients during the study period. Data about patients’ demographics, medication on admission, antithrombotic medication at the time of discharge and comorbidities were recorded in a spreadsheet. Outcomes were recorded as numbers and simple percentages. The CHA2DS2-VASC scores were not available to practitioners during the data collection period. Although the CHADS2 score was mostly used by the general practitioners, the written CHADS2 score was not found in all the files. Therefore, CHADS2 and CHA2DS2-VASC were evaluated for stroke risk assessment and the HAS-BLED was evaluated for bleeding risk assessment. There was sufficient data available in case files to evaluate the scores. The clinical (secondary) outcomes such as stroke, systemic embolisation and bleeding complications were reviewed in all patients during the 5-year study period.
Ethics approval
This study was approved by the South Australian Health Human Research Committee (HREC/14/SAH/45).
Results
A total of 59 patients and 73 admissions were reported at Ceduna District Hospital with AF or AFL during the 5-year study period. Study population characteristics and risk scores are shown in Table 1. The AF patients could not be categorised into paroxysmal, persistent or permanent, as sufficient data was not available in the case files. The CHADS2 score classified 16.44% as low score (score=0), 30.14% as intermediate risk (score=1), and 53.42% as high risk (score ≥2). The CHA2DS2-VASC score classified 9.59% as low risk (score=0), 10.96% as intermediate risk (score=1) and 79.45% as high risk (score ≥2) (Fig1). According to the CHADS2 risk score, 83.56% patients were eligible for anticoagulation with CHADS2 risk score ≥1; 77% received anticoagulant. According to the CHA2DS2-VASC score, 90.4% patients were candidates for antithrombotic therapy, out of which 83% received anticoagulation.
During the study time period, warfarin and aspirin were the available options. Novel anticoagulants were not widely available until 2013 for the prevention of non-valvular AF and only two patients were taking novel anticoagulants. The remainder were taking either aspirin or warfarin. Five or six patients, as per the CHADS2 and CHA2DS2-VASC score respectively, did not receive antithrombotic therapy. Chart review identified justifiable causes of withholding anticoagulation; these included older age (75–90 years), dementia, palliative care, bleeding complication and poor compliance. The authors analysed another group of five patients with previous history of stroke, transient ischaemic attack or systolic embolic event. All of these patients experienced stroke before the study period and none had a stroke during the 5-year study duration. Five deaths occurred during the study period due to other causes, but no one died from bleeding complications or stroke and no patients were over-anticoagulated.
Before starting anticoagulation, a risk–benefit analysis has to be done based on stroke risk stratification and HAS-BLED score. A HAS-BLED score >3 is considered high risk; in this study, nine cases had a HAS BLED score of 3, three cases of HASBLED scored 4 and and three cases scored 5. The decision to use or ignore the HAS-BLED score is ultimately a clinical decision; however no bleeding complications were experienced with patients for which HAS BLED score was high.
Table 1: Study characteristics of patients with atrial fibrillation (N=59)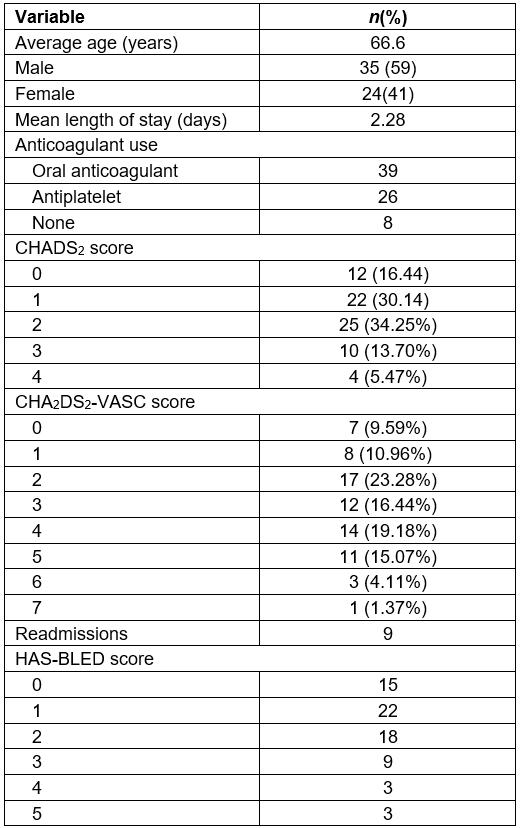
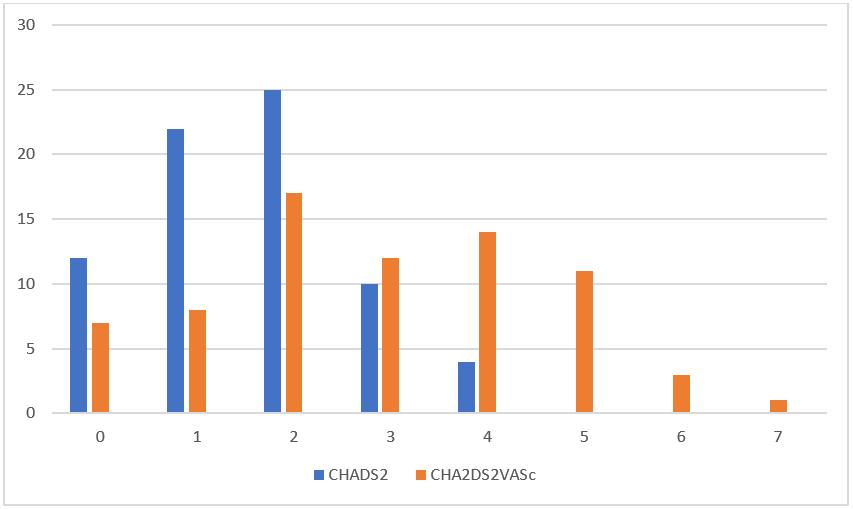 Figure 1: Risk stratification for study population.
Figure 1: Risk stratification for study population.
Discussion
In the study period, general practitioners mainly used the CHADS2 score for stroke risk assessment. A CHADS2 score >2 requires anticoagulation therapy, while CHADS2 of 1 indicates moderate risk, requiring either anticoagulation or antiplatelet therapy depending on the bleeding risk assessment f(eg HAS-BLED score). Current practice favoured warfarin therapy over anti-platelet therapy at CHADS2 and CHA2DS2-VASC scores of 113-15. Novel anticoagulants were not available on the Pharmaceutical Benefits Scheme until mid-2013 for the prevention of ischaemic stroke non-valvular AF. During the study period, warfarin and aspirin were available. Although there are well-known benefits for anticoagulant use in AF, several studies have shown suboptimal prescribing 11,16-19. Similarly, inconsistent use has also been observed with warfarin therapy20. This study demonstrated that, in a small rural hospital, 77% of patients (using CHADS2 score) and 83% (using CHA2DS2-VASC score) with newly diagnosed or pre-existing AF/AFL received appropriate anticoagulation therapy. The results of this retrospective audit are similar to the results observed in the Euro Heart Survey where increased prescription of oral anticoagulants was observed with increasing stroke risk scores21, and in a prospective survey in Geneva, where 88% of patients needing anticoagulants received therapy22.
The adherence to guidelines in this study presumably reflects the close relationship between the general practitioners, hospital, community services and patients. In a small community the patients are well known to all providers and there is only a small chance of patients becoming lost to follow-up. In this healthcare system, there was only one pharmacy and pathology service involved, so it was easy to track medication use and warfarin monitoring. Lastly, there was a staff culture of following guidelines in the hospital to encourage evidence-based treatment. In larger rural communities this single-system approach becomes more separated and the risk of errors increases. The onus of responsibility is on the practice prescribing, monitoring and recall systems, in tandem with ongoing education and clinical awareness. Further development of clinical prompts linked to guidelines when prescribing is one method of overcoming errors.
In this small study, two patients were given antithrombotic treatment inappropriately. The reasons for prescribing were unclear or missing, and this emphasises the importance of clear documentation, including the scoring system used. Any documentation should include patients who decline treatment despite adequate information to themselves and their carers. Fortunately, there were no adverse outcomes related to inappropriate prescribing. Several other ethical issues were apparent from the case records. These included a documented response to concerns of the risks of side effects of treatment, consideration of renal function, alcohol intake and likely adherence to treatment. A consent to treatment document that included a checklist would be a useful solution. Five patients had stroke before the study period (two Aboriginal and three non-Aboriginal). Four of them were appropriately anticoagulated; however, one had a transient ischaemic attack, with a CHADS2 score of 3, and was taking aspirin (without apparent reason). The authors could not find any adverse outcomes in patients who were not appropriately treated, nor whether they were on any anticoagulant when they had a stroke prior to the study period. No association was found with rheumatic heart disease with any adverse outcomes.
Limitations
The retrospective nature of this audit is a potential limitation. For the purpose of the audit, the authors estimated the CHADS2 score retrospectively based on the reported comorbidities. However, some of the physicians may have estimated patients’ CHADS2 score before prescribing anticoagulation; this information was unavailable in all patient files.
Conclusions
General practitioners in this remote practice in South Australia adhered to international guidelines regarding anticoagulation for patients with atrial fibrillation, contributing to safe practice. The change from CHADS2 to CHA2DS2-VASC scores has resulted in more patients requiring anticoagulation.


