Introduction
Farmers, as an occupational group, have been found to have a lower risk of cancer overall than the general population1. However, an increased risk for some cancers has been reported, including non-Hodgkin lymphoma; myeloma; leukaemia; and cancers of the lip, skin, stomach, prostate and brain1-8.
Farming is a very diverse occupation with many tasks potentially resulting in exposure to carcinogenic agents, such as fuels, engine exhausts, organic solvents, crystalline silica, metals, wood dust and solar radiation2,9,10. Despite this, many studies of farmers concentrate only on pesticide exposure11-13 and little is known about the patterns of exposure to other occupational carcinogens among farmers.
Using an automated rule-based expert assessment method, OccIDEAS14, the present study aimed to investigate which carcinogens Australian farmers are exposed to, the prevalence of exposure, any difference in prevalence among demographic and farm type subgroups, the circumstances or tasks that led to the exposures, and protection measures used to reduce or eliminate exposure.
Methods
Study population
Data for this study comes from a larger study, the Australian Work Exposures Study (AWES) conducted in 2011–2012, and supplemented with data from the Australian Work Exposures Study-Western Australia (AWES-WA), conducted, using identical methods, in 2013. Full methods have been described in detail elsewhere15. Both studies were cross-sectional telephone surveys that investigated occupational exposure prevalence to 38 known or probable priority carcinogens in the Australian workplace15. The list of priority carcinogens was based on agents that the International Agency for Research on Cancer (IARC) had classified by 2012 as Group 1 (‘carcinogenic to humans’) or 2A (‘probably carcinogenic to humans’)16. The list was then refined to include only those that were used in Australian occupational settings16,17.
The AWES sample was randomly drawn from a list of about six million Australian households held by a commercial sampling firm. This list was compiled from various public domain data sources, including telephone directories, and included addresses and telephone numbers (both landline and mobile). The sample was stratified by state and territory to reflect the Australian workforce distribution in 201118. For each household, residents between the ages of 18 and 65 years who were currently employed, had sufficient English speaking ability, and who were not deaf or too ill, were eligible to participate.
The AWES-WA study used the same methods but was restricted to residents of the state of Western Australia.
Data collection
Trained interviewers carried out computer-assisted telephone interviews after obtaining oral informed consent. Participants were asked a series of questions to collect demographic information including age, sex, country of birth, language spoken at home and highest level of education. Socioeconomic status and remoteness were determined by applying the Australian Bureau of Statistics Socio-Economic Indexes for Areas Index of Relative Socio-economic Disadvantage (ABS SEIFA IRSD)19 and Australian Standard Geographical Classification Accessibility/Remoteness Index of Australia (ASGC ARIA+)20 to the participant’s postcode.
Participants were asked basic questions about their job and this information was used to assign one of 57 job-specific modules (JSMs), including a Farmer JSM, in the online application OccIDEAS14. Those participants who were in specific jobs that had been determined a priori to be non-exposed to carcinogens (eg office worker) were allocated no further questions. The JSMs in OccIDEAS were developed by occupational hygienists and epidemiologists and included questions on tasks that potentially result in exposure to carcinogens.
Each job was coded using Australian and New Zealand Standard Classification of Occupations (ANZSCO)21. Seven ANZSCO codes were determined as relating to farmers or farming: 1212 (crop farmers) and 8412 (crop farm workers), grouped as ‘crop’; 1213 (livestock farmers), 8415 (livestock farm workers) and 3612 (shearers), grouped as ‘livestock’; and 1214 (mixed crop and livestock farmers) and 8416 (mixed crop and livestock farm workers), grouped as ‘mixed’.
Participants were asked questions regarding the type of crop grown and/or livestock farmed, the amount of time spent outdoors, pesticide use, type of fuel used and other potential tasks undertaken by farmers such as painting, welding and degreasing. They were also asked questions about their use of protective measures such as sun protective measures (wearing sunscreen, working in the shade, wearing a hat, etc.) and respirator use. Based on the questions asked, farmers were assessed regarding their likelihood of exposure to 38 priority carcinogens16. Information on specific pesticides was not analysed for this article because it was not possible to investigate specific carcinogenic pesticides, and so a broad pesticide category was used. In addition, questions were asked about the number of hours per week (categorised into 0–<5 hours per week, 5–30 hours per week, >30 hours per week) that farmers undertook the task and the number of weeks per year it was carried out. Farmers were found to be probably exposed to 13 carcinogens: asbestos, benzene, cadmium, chromium IV, crystalline silica, diesel engine exhaust, lead, nickel, pesticides, polycyclic aromatic hydrocarbons (PAHs) other than from vehicle exhausts, solar radiation, trichloroethylene and wood dust. Results are presented for the 11 carcinogens for which five or more farmers were exposed (fewer than five farmers were exposed to asbestos and/or cadmium).
Exposure assessment
OccIDEAS provided automatic assessments of the probability of exposure (‘none’, ‘possible’ or ‘probable’) and level of exposure (‘low’, ‘medium’ or ‘high’) to each carcinogen depending on the answers to relevant questions. The assessments were qualitative and do not necessarily correlate to exposure standards. Algorithms linking answers to assessments were developed on the basis of expert opinion. The use of control measures was considered and the exposure assessments were adjusted automatically to take their use into account. For example, a participant who wore a respirator whilst power-sanding wood was assigned a low-level exposure whereas a participant who did not wear a respirator whilst undertaking this task was assigned a medium-level exposure to wood dust. All automatic assessments were reviewed by project staff for consistency.
Statistical analysis
All statistical analyses were conducted using Stata v14 (StataCorp, http://www.stata.com). Prevalence of exposure was calculated by dividing the number of exposed farmers by total farmers (within subgroups where applicable). Chi-squared tests were used to test for significant differences between prevalence of exposure by farm type, sex, education, age group and socioeconomic status and Fisher’s exact tests were used when there were fewer than five individuals in each specified group. Statistical significance was determined using 5% significance level.
Ethics approval
Ethics approval for this study was obtained from the human research ethics committee of the University of Western Australia (RA/4/1/4802).
Results
Of the 22 590 numbers telephoned in both the main AWES study and AWES-WA, a total of 5498 interviews were completed with sufficient information for analysis. The main reasons for not participating were ineligibility (n=12 081), no response after 10 different call attempts (n=3033) and refusal to participate (n=1948). This resulted in an overall response fraction (completed interviews/eligible and unknown households) of 53% and a cooperation fraction (completed interviews/eligible households) of 74%.
Farming ANZSCO codes were assigned to 166 participants who made up the final study population. The majority of farmers in the study were men (76%), aged 35–54 years (51%) and were born in Australia (94%) (Table 1). Sixty-eight percent of the study participants reported their highest education level as secondary school or less, and a majority fell into the second (37%) and third (25%) lowest quintiles for socioeconomic status. A majority resided in inner and outer regional areas (81%). The most common farm type was mixed crop and livestock farms, followed by livestock only and crop only.
All of the 166 farmers were assessed as being exposed to at least one of the 38 carcinogens. On average, farmers were exposed to 5.1 different carcinogenic agents, with men (5.3) having more exposures than women (4.3). Mixed crop and livestock farmers were exposed to more carcinogens on average (5.6) than both crop-only (4.4) and livestock-only (4.6) farmers.
The most prevalent exposures were to solar radiation, diesel engine exhaust, benzene, PAHs other than from vehicle exhausts and wood dust (Table 2). Pesticide use was reported by 117 (70%) participants; of those, 92% (n=108) used herbicides, 64% (n=75) used insecticides and 62% (n=72) used both. For all exposures considered separately, 75% or more of the farmers were exposed for greater than 30 hours per week. The exposures with the highest mean frequency in terms of weeks per year were lead, PAHs other than from vehicle exhausts, solar radiation, wood dust and diesel engine exhaust.
Table 1: Demographic characteristics and farm type of study population (N=166)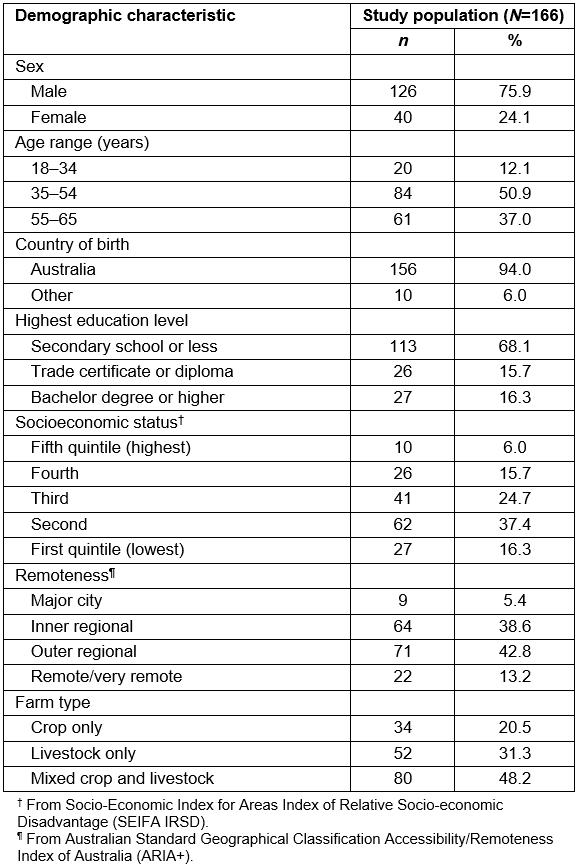
Table 2: Carcinogens in which farmers are potentially exposed, their International Agency for Research on Cancer classification, the tasks determined to cause probable exposure and the number, percentage exposed, frequency and duration of exposure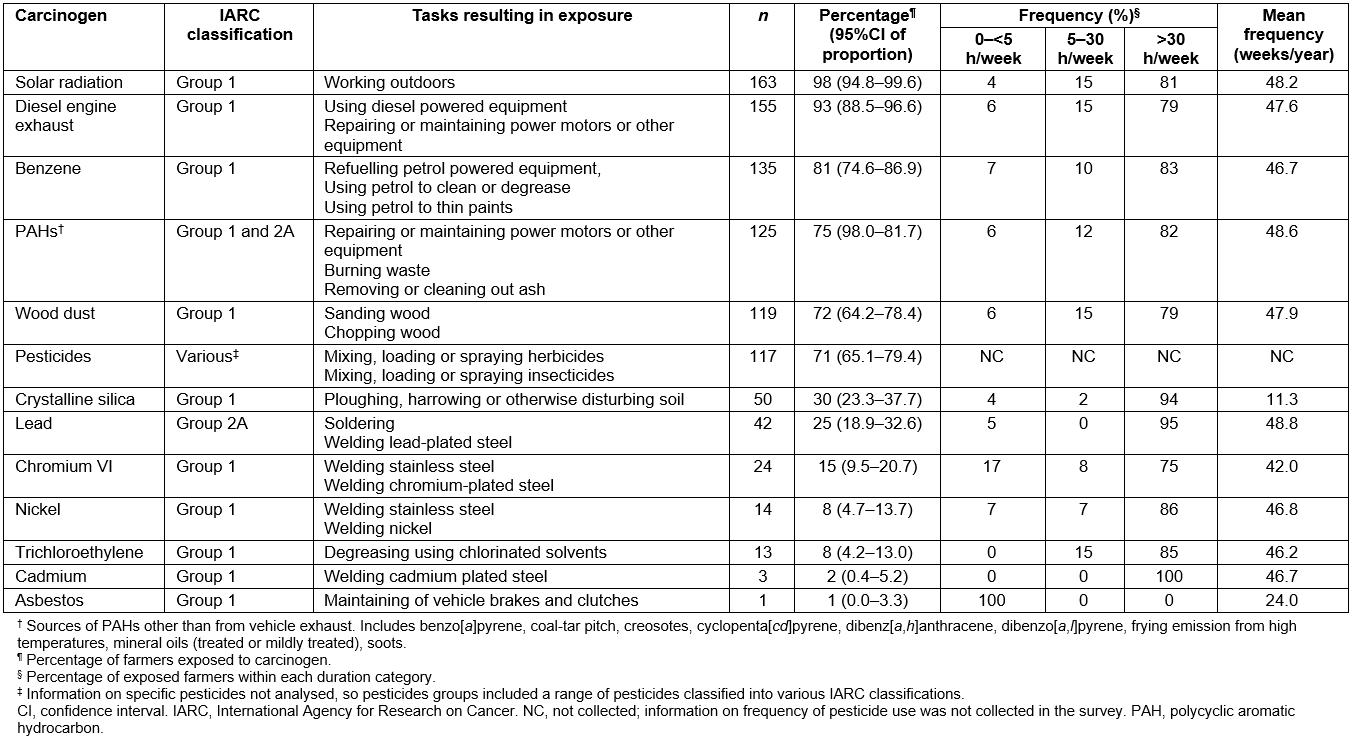
The most common exposure circumstance for solar radiation exposure was working outdoors, with most farmers assigned a high level of exposure (Table 3). Four types of sun protection were considered: wearing a hat, protective clothing, sunscreen use and working in the shade (Table 4). The most common sun protections used were wearing a hat and protective clothing and they were worn more than half the time when working outdoors by 91% and 79% of farmers respectively. Only 35% of farmers worked in the shade and 33% wore sunscreen for more than half the time they worked outdoors.
Common tasks that incurred exposure to diesel engine exhaust were using diesel powered equipment (n=148, 89%) and repairing or maintaining power motors or other equipment (n=97, 58%). Refuelling petrol powered equipment was the most common task resulting in benzene exposure (n=134, 89%).
Of the farmers who ploughed, harrowed or otherwise disturbed soil (n=48), 88% (n=42) did so in an enclosed cab and were assigned a medium level of exposure to crystalline silica, whilst those who did not use an enclosed cab were assigned a high level of exposure (Tables 3, 4).
Table 3: Most common circumstances for each carcinogen exposure, and level of exposure†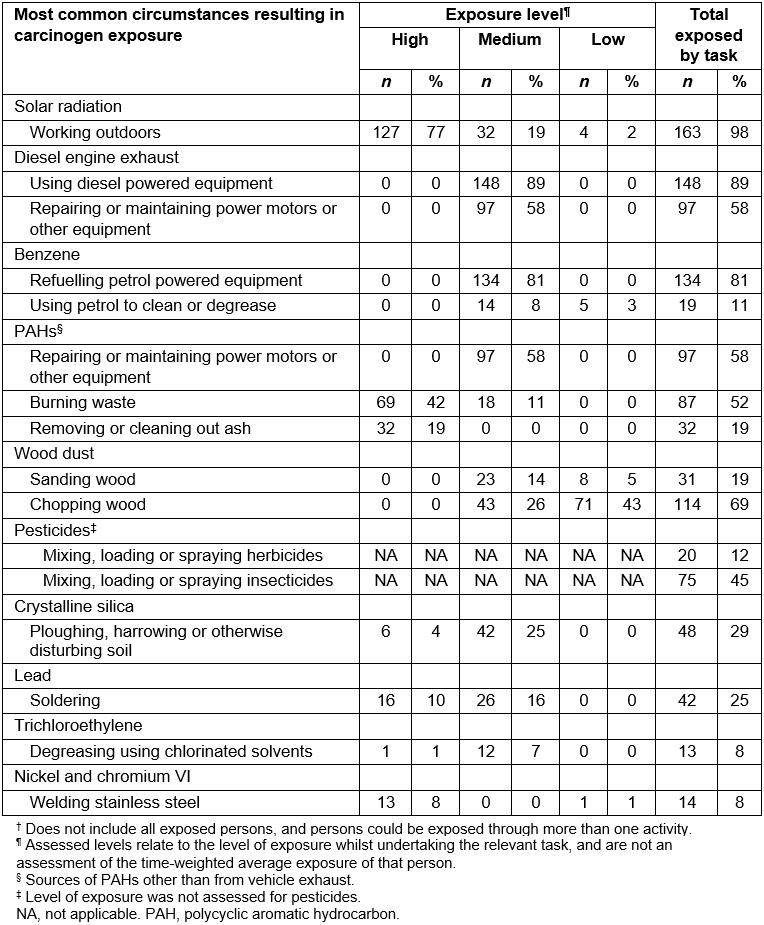
Table 4: Number and percentage of participants who used specific control measures for common exposure circumstances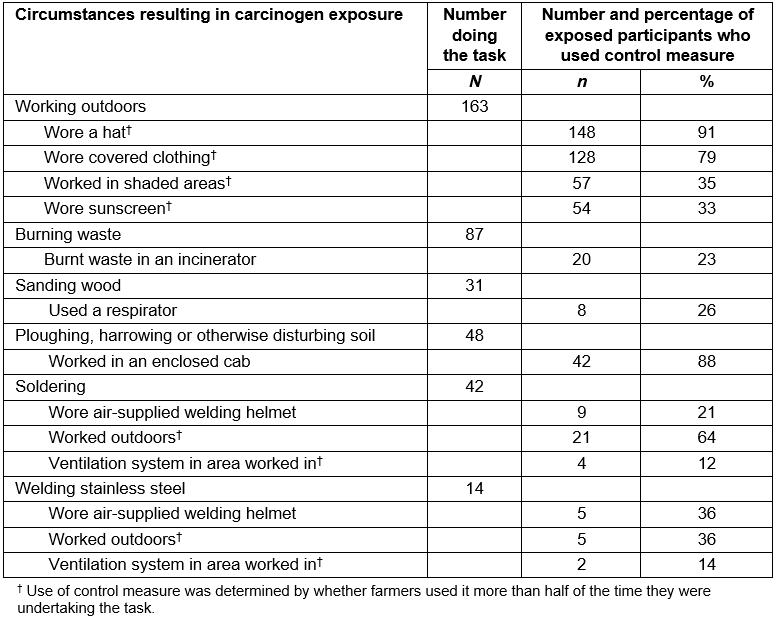
Men had considerably higher exposure prevalence than women for lead, PAHs other than vehicle exhausts, pesticides and wood dust (Table 5). The prevalence of exposure to crystalline silica was significantly higher in those farmers with a bachelor degree or higher compared with those with a lower level of education. No statistically significant differences were found for exposure prevalence by age or socioeconomic status.
Farmers working on different farm types (crop, livestock and mixed) were found to have important differences in their prevalence of exposure to seven of the carcinogens (Table 6). Prevalence to PAHs other than from vehicle exhaust, lead and pesticides were significantly higher for the mixed farm group compared with the crop-only or livestock-only groups. Crystalline silica and trichloroethylene were less common exposures for the livestock-only group compared with the other groups. The livestock and mixed groups had a higher prevalence of exposure to benzene and wood dust compared to the crop-only group.
Table 5: Number and percentage of study population (n=166) exposed to each carcinogen in total and by gender (men, n=126; women, n=40)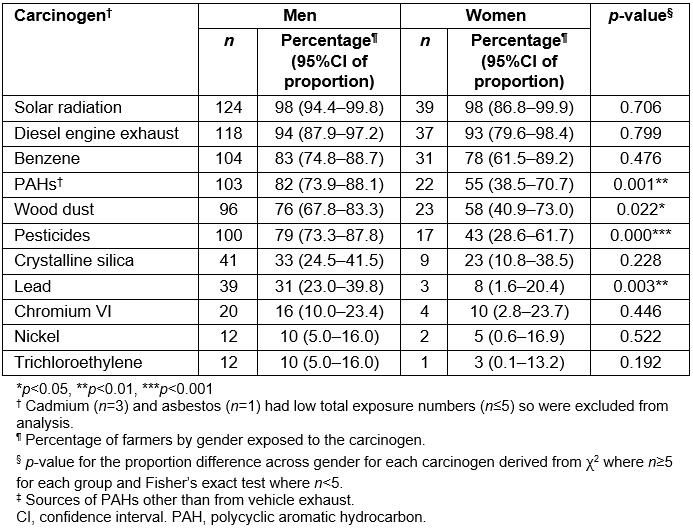
Table 6: Number and percentage of study population (n=166) exposed to each carcinogen by farm type (crop, n=34; livestock, n=52; mixed, n=80)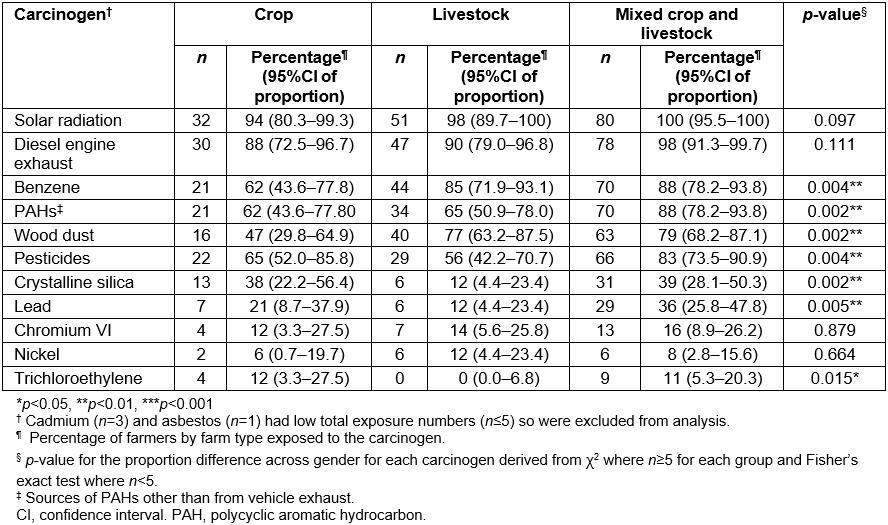
Discussion
This study found that farmers undertook a wide range of tasks and consequently were exposed to a wide range of carcinogens, including solar radiation, diesel engine exhaust, benzene, PAHs other than from vehicle exhaust, wood dust, pesticides, crystalline silica, lead, chromium VI, nickel and trichloroethylene. For six of the carcinogens, over 70% of farmers reported exposure: solar radiation, diesel engine exhaust, benzene, PAHs other than from vehicle exhausts, wood dust and pesticides. Generally, exposure was more common in male farmers than female farmers and among mixed-crop and livestock farmers than both crop-only and livestock-only farmers.
Although common (70% prevalence), pesticide use was not the most common carcinogen exposure in farmers. Like this study, the Agricultural Health Study conducted in the USA found a high prevalence of exposure to diesel engine exhaust (93%), metals (68%) and solvents (25%) among farmers22, and the Canadian CAREX study found a high prevalence of solar radiation (75%) exposure among farmers23.
Even though women had a significantly lower exposure prevalence than men for several carcinogens, their exposure prevalence was still high, with six of the carcinogens having a prevalence of greater than 40%. Most studies on carcinogen exposure in agriculture have paid particular attention to men5,24,25 with many of those that included women only investigating those living on farms, rather than those undertaking farm work. This study shows that carcinogenic exposures among women working on farms are common and should be considered when conducting studies in farmer populations.
Exposure prevalence across carcinogens varied by farm type. Solar radiation and diesel engine exhaust were the most common exposures on all types of farms. Crop-only farmers tended to be additionally exposed to pesticides, crystalline silica and lead, while livestock-only farmers were more often exposed to benzene and wood dust. Workers on mixed farms tended to be exposed to a larger combination of the carcinogens, resulting in them having the highest prevalence of exposure for most agents. For example, the prevalence of lead exposure was considerably higher (36%) in mixed-crop and livestock farmers than in crop-only farmers (21%) or livestock-only farmers (12%). Studies in the USA and Finland have found differences in mortality for some cancers between livestock farmers and crop farmers7,26,27. For example, the US study found that only livestock farmers had an excess mortality risk of non-Hodgkin lymphoma and cancers of the brain, prostate and pancreas compared with the general population, whereas crop farmers had an excess mortality risk of multiple myeloma, chronic lymphoid leukaemia and cancers of the lips and skin (excluding melanoma)7. The US study did not include a mixed-crop and livestock classification.
Australian farmers have particularly high exposures to solar radiation because of Australia’s equatorial proximity and its clear atmospheric conditions, so their use of sun protection is extremely important28,29. The findings of this study are consistent with a review of sun safety in farmers conducted in 2015 that showed that farmers commonly wear hats and long trousers as sun protection methods; however, the use of sunscreen was less frequent30.
The use of respiratory protective methods was much less frequently used by farmers than sun protection, with only 26% of participants reporting the use of a respirator. A study conducted in the USA found a significant decrease in respirator use among Californian farmers from 54% in 1993 to 37% in 2004, and additionally found that the use of dust masks or respirators was related to personal factors such as smoking history, education and respiratory risk concern31.
A major strength of the present study was the use of a task-based questionnaire to determine exposure to carcinogens. Participants were required to self-report on tasks they performed at work, and exposure assessments were based on the information given. Therefore there is less potential for misclassification bias than when exposure is attributed from a job exposure matrix or when individuals are asked to self-report their exposures32. Additionally, using a task-based approach allowed the investigation of the use of control measures used when participants completed specific tasks.
The approach used in this study had some limitations. Because the study used telephone interviews it was important to minimise interview time to maintain the participants’ willingness to cooperate. To account for this, the study restricted questions to those that were specific to the main study purpose and to relatively common activities. Farmers undertake many different tasks so it is possible that some specific tasks were not covered, and therefore some exposures may have been missed. This may have resulted in the omission of a carcinogen exposure, for example to oncogenic viruses, or an underestimate of the prevalence of exposure. However, the authors are confident that the study covered the most common farming tasks and therefore the majority of important carcinogen exposures among farmers. Another limitation was the lack of in-depth information on duration and frequency of exposure. Frequency was collected in categories of broad hours per week. No information on duration (ie number of years) for which the farmer undertook each task was collected in this survey as the emphasis was on current exposure.
The farmer sample was taken from a larger cross-sectional study that examined workplace exposures in a range of jobs, not farmers specifically, and therefore the sample size for this particular study was limited. Larger studies of farmers are needed to provide a more rigorous estimate of the prevalence of exposure to carcinogens in Australia, to determine the prevalence of less common exposures such as cadmium and asbestos and to provide further investigation of the factors influencing the use of control measures33.
Another limitation is the use of postal area as a proxy for socioeconomic status. Although commonly used, there are problems associated with the use of postal area as a socioeconomic measure in that it may be imprecise34; however, for the purposes required for this study, its use is unlikely to introduce bias.
Since the development of the priority carcinogen list in 201216, IARC has classified the insecticide lindane as a Group 1 carcinogen and the insecticides malathion, diazinon and dichloro-diphenyl-trichloroethane (DDT) and the herbicide glyphosate as Group 2A carcinogens35,36. Use of DDT was banned in Australia in 1987 but the remaining pesticides are likely to be used by a proportion of the study population37,38. Although information was collected bout whether insecticides or herbicides were used by the participants, the use of specific chemicals was not assessed as the sample size was too small.
Conclusions
Farmers are an occupational group with a high prevalence of exposure to carcinogens. The variation in tasks that they undertake results in exposures to a wide variety of different carcinogens that require similarly varied control measures.
Acknowledgements
The authors wish to acknowledge Renae Fernandez for her role in preparing the questionnaires for this study and Troy Sadkowsky for his role as data scientist. This work was supported by a National Health and Medical Research Council (NHMRC) project grant (#1056684), the Cancer Council Western Australia and Safe Work Australia.
