Introduction
Rural and remote populations in Australia experience higher rates of disease, obesity, substance abuse and injury than their metropolitan counterparts. These factors contribute to lower life expectancies with increasing remoteness: by 1–2 years for regional populations and up to 7 years for remote populations1 .
Throughout Australia, the majority of specialist health services are within tertiary hospitals located in major metropolitan centres, making access for regional, rural and remote populations difficult2. In addition, these populations have fewer general practitioners (GP) per 100 000 and fewer after-hours attendances compared to those living in metropolitan centres, resulting in as little as half the access to GP services in remote areas3. Similarly, access to medicines is further restricted by community pharmacists being more sparsely distributed per head of population in these remote regions, compounded by the low population density4. In these environments the Royal Flying Doctor Service (RFDS) provides essential medical support for general medical and emergency situations. In order to further overcome the remote access to treatment, the RFDS introduced its medical chest program in 1942 and it is now a major component of the support offered to Australia’s rural and remote populations with medical chests located in more than 3000 rural and remote communities and towns across the country5. Each medical chest contains a standardised range of medical supplies and pharmaceuticals, including ‘prescription only’ pharmaceutical items, which can be dispensed on the advice of an RFDS medical practitioner in the absence of a pharmacist.
The medical chest program operates in conjunction with the RFDS medical advice line for the local area of operation, which people can call when they require medical assistance. Their call is transferred to a doctor who will diagnose their condition over the telephone. If the condition requires treatment the doctor can remotely prescribe medications from the chest using the chest cataloguing system and provide instructions for its administration. At the conclusion of the consultation the patient is provided with a consultation number that can be used to re-order the drug if further quantities are needed5. In the event of an emergency, when a patient is unable to communicate effectively, the custodian of a medical chest can access an RFDS doctor by telephone. The custodian may also use the medical chest to assist in the treatment of the patient while other medical personnel and resources are dispatched5.
The medical chest program is administered by RFDS areas of operation, usually defined by state boundaries. By examining the use of the medical chest in association with the nature of the RFDS consultations, it may be possible to gain some insight into rates and patterns of disease amongst remote populations. This study analysed the categories of items dispensed from the RFDS medical chests and ‘mini-chests’ and the conditions they were used to treat for the state of Queensland over the year 2013–14. The data were compared with an earlier review of the Queensland section medical chest program for the year 2005–066, to assess any change in the distribution of conditions treated and the quantity and nature of items dispensed. In addition, this study examined the demographics of the patients treated within the medical chest program, for the first time in the history of the program providing age, gender and ethnicity of patients served.
Methods
Use of the medical chest
During every telehealth consultation within the Queensland section of the RFDS a doctor records their notes in paper form. At the conclusion of the consultation the patient’s medical information is entered into the electronic Health Consultation Record (HCR) and the items dispensed from the medical chest are entered into the Health Aeromedical Logistics (HAL) database. The Queensland RFDS recently introduced ’mini-chests’, which are smaller versions of the medical chest and are used in the same telehealth format as the traditional medical chests. The data associated with their use are recorded in the same manner as data from the traditional medical chests, and the two were combined for this study.
In addition to tele-consultations, the Queensland RFDS runs clinics in remote communities where RFDS personnel travel to the area. These clinics have access to the RFDS medical chests if required; however, they are usually run in facilities that separately stock the required medical supplies. During these clinics the patients’ notes and record of the supplies used for each consultation are entered into the electronic MD3 Medical Director program.
The de-identified data for this report were taken from the HAL database for the period of 1 July 2013 – 30 June 2014. These dates were chosen to permit comparison with a previously published report on the medical chest covering the period 2005–066. No data were retrieved from the MD3 Medical Director program, as the RFDS clinics rarely use supplies from the medical chests. Data was de-identified by a third party not involved in the research.
The items dispensed from the medical chests throughout the review period were recorded from the HAL database and grouped into categories before being tallied.
The number of telehealth consultations involving an RFDS doctor during the review period was recorded from the electronic HCR. These consultations were grouped into diagnostic categories according to the WHO’s International statistical classification of diseases and related health problems7. The results included the total number of telehealth consultations, those where the medical chest was used and those where it was not used. These data were compared with the WHO International Classification of Disease (ICD) diagnostic category data from 2005–066. A χ2 with Fisher’s exact test was applied to each diagnostic category to compare the percentage use of the medical chests in telehealth consultations in 2013–14 compared to that in 2005–06 6. Statistical significance was accepted at p<0.05.
Ethics approval
The University of Wollongong’s Human Research Ethics Committee approved the aims, objectives and methods of this research (GSM14/029).
Results
In total, 20 707 telehealth consultations were conducted in the 2013–2014 review period. The median age per consultation was 45 years (Table 1), ranging from newborn to 105 years. The male-to-female ratio was 56:44, and at least 22% of consultations concerned Indigenous people (32.6% undisclosed ethnic origin).
Table 1: Number of telehealth consultation episodes by patient age group, sex and ethnicity in 2013–14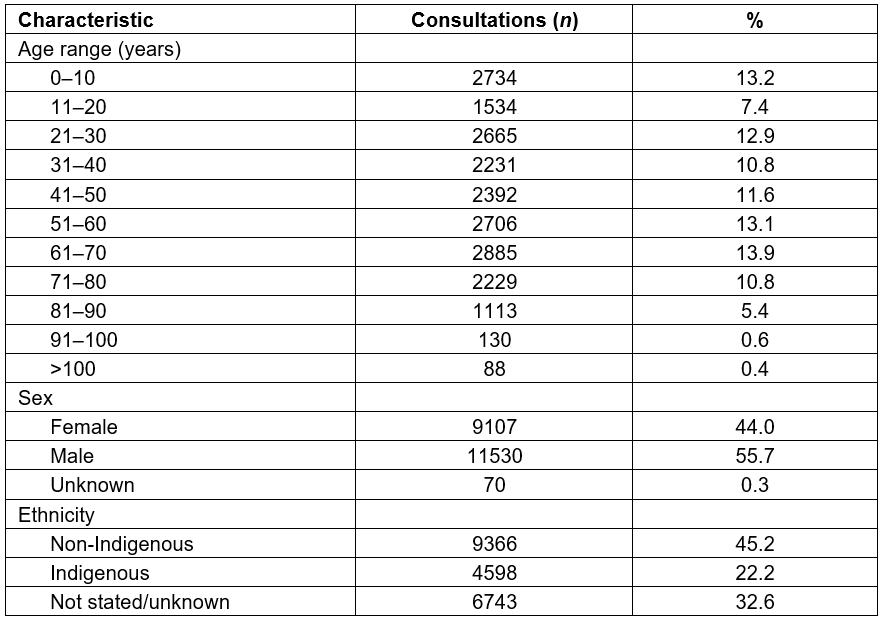
Items dispensed
A total of 3936 items were dispensed, amounting to less than 50% the number of items dispensed in 2005–06 (Table 2). Of those items dispensed during the review period, over 50% came from the categories of antibiotics, and burns and other dressings, which, together with analgesics and gastrointestinal medication, accounted for more than 75% of items amongst just four categories.
Most categories of item were dispensed significantly less than in 2005–06, with only burns and other dressings, and antihistamines, showing increased use (Fig1). As a proportion of total items dispensed, analgesics, burns and other dressings, and antihistamines, increased in use and antibiotic use remained unchanged. The remainder of categories were proportionately less used in the current review period (Table 2).
Table 2: Items dispensed from the medical chest, by category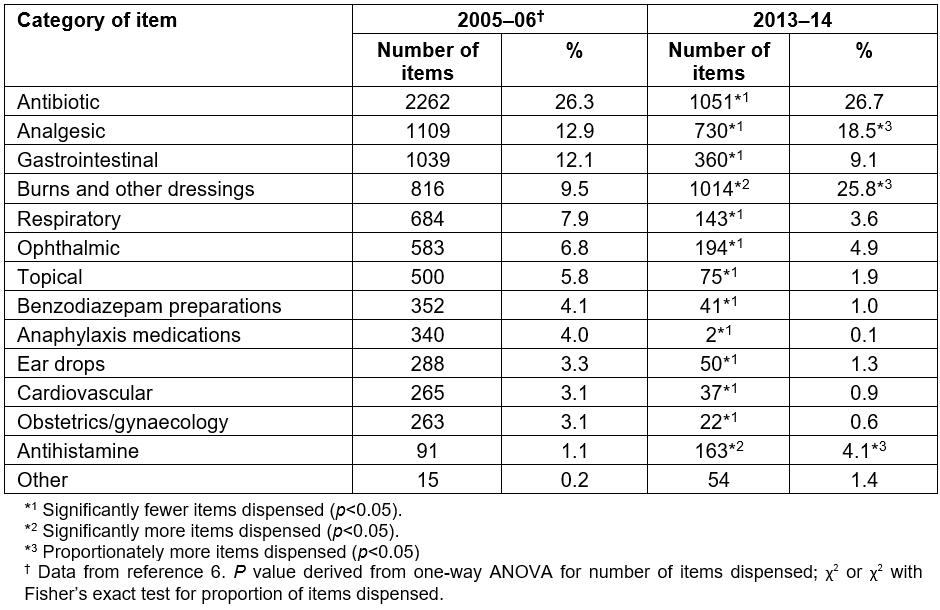
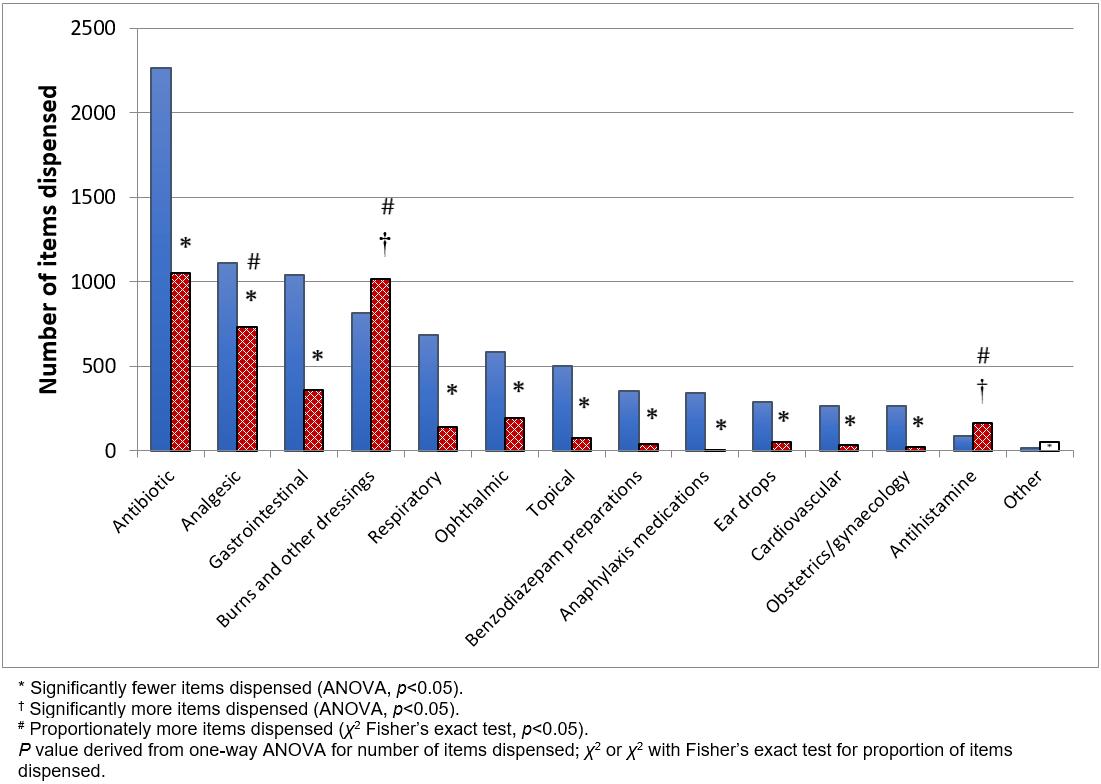
Figure 1: Number of items dispensed in each category for the year 2013–14, N=3936 items (cross-hatched columns); and 2005–06, N=8607 items6 (filled columns).
Diagnostic categories
During the review period a total of 20 707 consultations occurred, which was not significantly different to the 21 470 consultations during 2005–06 (Table 3). Three ICD diagnostic categories were involved in consultations significantly more often in 2013–14: circulation system, symptoms without a diagnosis and other contact with health service, with 10 categories used less often (Fig2).
Eight diagnostic categories had significant reductions in items dispensed from the medical chests (Table 3): circulation system, specific infectious disease, respiratory system, abdominal system, skin diseases, symptoms without a diagnosis, injury and other contact with health service. The category of genitourinary system, was the only diagnostic category to have a significantly greater use of the medical chest.
Table 3: Use of medications according to primary diagnostic categories of telehealth consultations 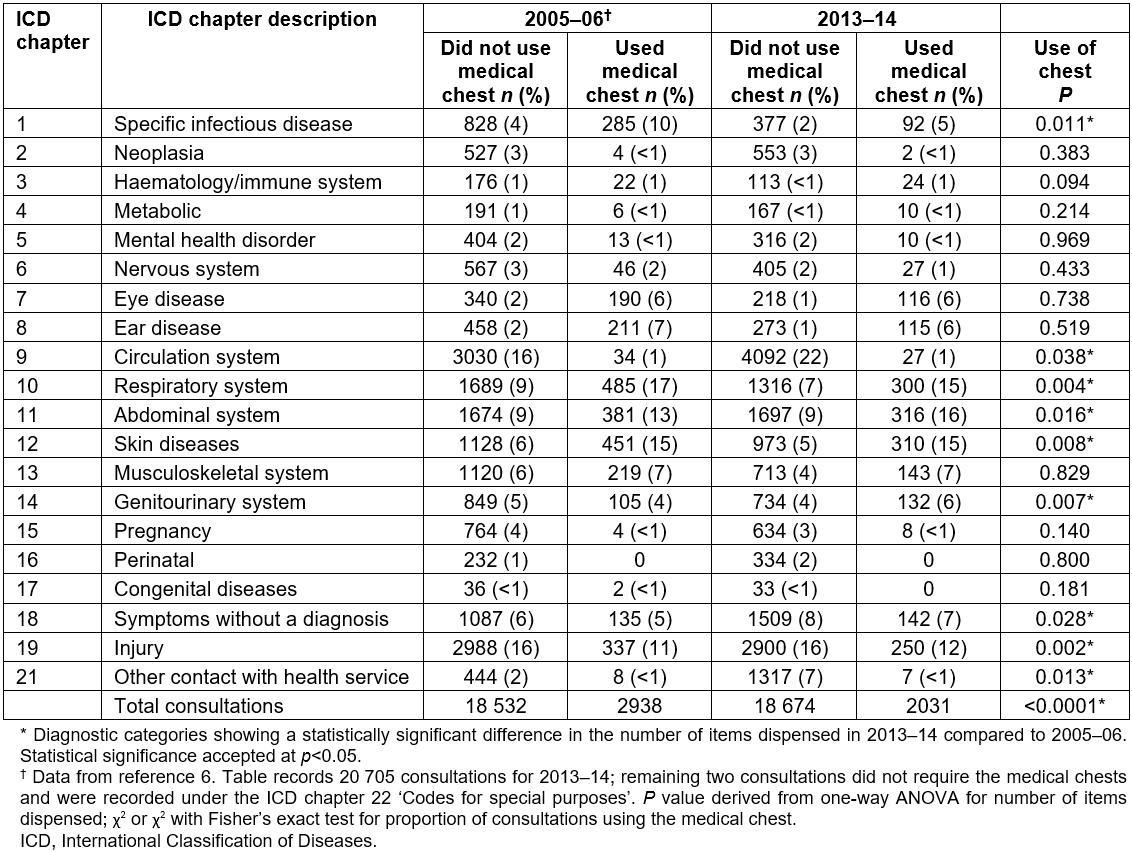
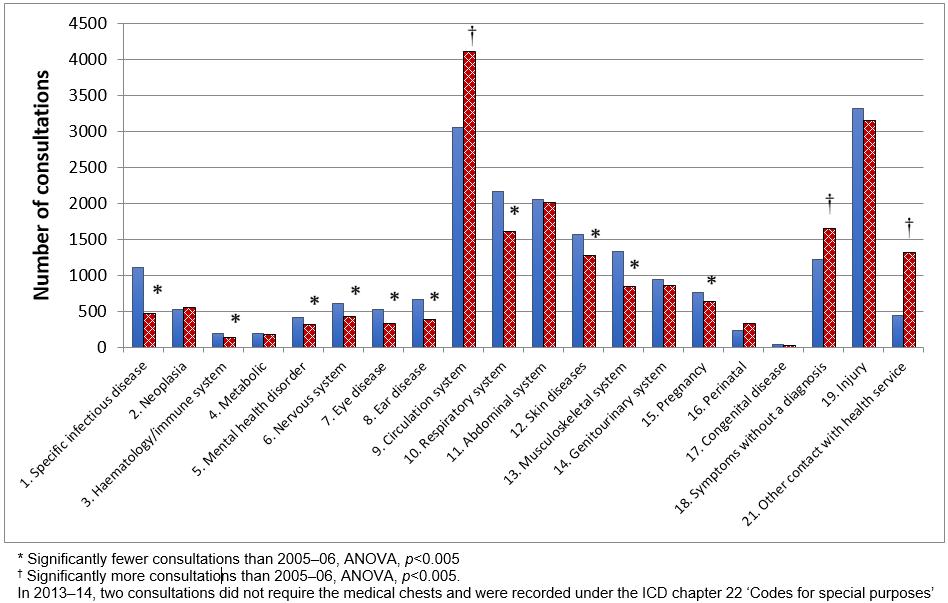 Figure 2: Number of telehealth consultations in each of the ICD primary diagnostic categories for the year 2013–14, N=20 705 consultations (cross-hatched columns); and 2005–06, N=21 470 consultations6 (filled columns).
Figure 2: Number of telehealth consultations in each of the ICD primary diagnostic categories for the year 2013–14, N=20 705 consultations (cross-hatched columns); and 2005–06, N=21 470 consultations6 (filled columns).
Discussion
Medical chest dispensing as a marker of rural health
The rates of injuries, road and workplace fatalities, poisonings, deaths from assault, childhood hospitalisations and deaths in remote Australia outweigh those in metropolitan and larger regional centres8. This is reflected in a higher rate of encounters for injuries in this study than is seen in general practice across Australia9, mostly reflecting urban living. Despite this, populations in remote locations have access to few medical professionals and fewer medical resources10. The RFDS medical chest program provides invaluable medical resources to these communities and its use offers a unique insight into the healthcare needs of remote Australian populations.
Items dispensed from the medical chests
Despite little change in the number of RFDS consultations over time, the number of items dispensed from the medical chests was significantly reduced between 2005–06 and 2013–14. This result was reflected in all categories of items except for burns and other dressings and antihistamines. The number of items categorised as burns and other dressings was originally lower and in line with the overall reduction across most categories; however, upon further investigation it became evident that many of the items that should fall within this category had not been recorded in the HAL database as most did not require a prescription from a doctor. To ensure this category of items was appropriately represented in the results the authors analysed a list of items ordered to replace used or out-of-date stock in the medical chests. The items fitting the category of burns and other dressings were tallied from the list of ordered items and included in the results in place of the HAL data for this category. This approach was taken because many of the items in the category do not have expiration dates and therefore normally require replacement only after being dispensed for use by a patient.
Injuries in general and thermal injuries specifically occur in rural and remote Australia at over twice the rate per 100 000 of population compared to major cities8. The increased use of items from the category of burns and other dressings could indicate an increase in the rate of burns and conditions requiring dressings, a greater emphasis placed on the treatment of these conditions, changes to the type of dressings and their recommended use or an anomaly based on the method of data collection. A review of burn and wound management across Australia is required to address this; however, there is little evidence of any increase in unintentional thermal injuries from 2005 to 2010 across Australia as a whole8. Notably, the number of consultations for the injury category was unchanged in 2013–14 yet fewer items were dispensed during those consultations. This could suggest that the increased use of items categorised as burns and other dressings was associated with greater severity of injury, resulting in multiple items dispensed per consultation or an increased use of dressings outside of the consultation process.
The rise in antihistamine use is in line with the increasing prevalence of allergic conditions such as food allergies11 and allergic rhinitis (hay fever)10,12,13 within the Australian population.
The overall reduction in the number of items dispensed represents a significant decline in the use of the medical chests from 2005–06 to 2013–14. This could be explained by the increase in government funding over the same period to address the shortage of rural and remote general practitioners9, although the number of RFDS consultations did not decline. Strategies to address the shortfall have included training more doctors, providing doctors and medical students with incentives to travel to the areas of need and requiring overseas-trained doctors to practise in rural and remote communities3. It could be argued that this investment in the health of rural populations could have caused the decreased dependence on the RFDS medical chests due to a diversification of rural health facilities and infrastructure.
Expansion of pharmacy support in rural and remote Queensland could also account for the decline in the use of the medical chests. Capacity building initiatives, including alternative delivery models, seasonal employment, outreach services and additional telehealth initiatives14 could provide further explanation for the reduced use. These initiatives have received increased support from the Australian Government since the establishment of the National Prescribing Service in 1998 and the National Medicines Policy in 200015. The National Medicines Policy is committed to the objectives of timely access to medicine which meet appropriate standards for quality safety and efficacy, at a cost the community can afford16. Both the National Medicines Policy and the development of the National Prescribing Service occurred between the periods of review.
Additional reasons that could account for the reduction in use of the medical chests include the improved accessibility to medications via online providers, reduction in price of medications available to communities through traditional pharmacies and the improved accessibility between rural and remote communities due to new or improved road infrastructure, and these points merit further research.
Diagnostic categories treated with the medical chests
The data show that a similar number of telehealth consultations occurred during this review period compared to the previous review period, indicating that the demand for RFDS telehealth consultations has not changed. Furthermore, the proportion of consultations for each diagnostic category has remained similar except for circulation system and other contact with health service, which both increased.
Mortality from coronary artery disease decreased per head of population from 2006 to 2014 yet remained the leading cause of death in Australia in males and females for both review periods13. Therefore, the increased incidence of circulatory system consultations could be attributed to better survival leading to increased prevalence, together with a greater community awareness of the signs and symptoms of coronary artery disease and the importance of treatment. This idea is supported by data in Table 3, which indicates the use of the medical chest treatments in the category of circulatory system disease was less than expected despite the total number of consultations increasing. This could indicate increasing levels of health literacy amongst rural populations; however, analysis is challenging without comparative data from metropolitan centres.
The increase in the category of other contact with health service is likely attributable to the increased funding towards medical support of rural and remote communities within Queensland14; however, further details or reasons for the increase are beyond the scope of this research.
The increase in the use of the medical chests to treat presentations in the genitourinary system category could relate to the incidence of urinary tract infections (UTI) which are considered to be the most common bacterial infections17. It would be reasonable to expect UTIs to form a significant percentage of genitourinary system presentations and the treatment of these presentations could be complicated by the increasing number of UTIs resistant to most antibiotics18. This data could indicate increasing rates of UTIs in rural Australian populations; however, it could also suggest that people with signs and symptoms of a UTI were more easily able to access care through the RFDS medical chest program than through more conventional medical services located in their region.
The reduced use of the medical chest in some categories may relate to a change in prescribing habits for conditions within each diagnostic category or a variation in the style of presentations within each category. Although this information could be used to adjust the resources in the RFDS medical chests to optimise the limited space to best meet patient need, the authors urge caution until a greater understanding for the observed differences is achieved.
Patient demographics
No data has previously been published on the demographics of the patients treated with the medical chest program. In the present study, data on the age of patients treated show a relatively uniform pattern of distribution in line with current Australian life expectancies19. Of the 2734 patients in the age category of 1–10 years, more than 2000 were aged 0–5 years. This suggests the greatest proportion of children treated with the medical chest program were aged less than 5 years. Together with the lower use of the medical chest in the 10–20-year category, this aligns with the similarly high number of paediatric presentations in general practice across Australia for this age group compared to the 5–15-year age group, which is also amongst the lowest of any 10-year group9. It indicates the importance of the RFDS medical chest program in providing care to patients below school age in rural Australia.
At 45 years, the median age of those consulted was higher than the Queensland state and Australian population median age of 37 years in 201420. Moreover, a higher number of medical consultations involved male patients. This could simply indicate a greater proportion of males in rural populations or more likely reflects an increased risk of disease and trauma amongst males in those areas21. This is particularly evident in cardiovascular disease amongst men in rural Australia21 and reflected in the high incidence of cardiovascular consults with the RFDS in the review period.
At least 22% of the patients that underwent a telehealth consultation with an RFDS doctor identified as Indigenous. The last Australian Bureau of Statistics Census in 2011 indicated that 4.2% of the Queensland population identified as Indigenous22. Whilst a high proportion of Indigenous Australians live outside major cities or regional centres in Australia (21.4% of Indigenous population compared to 1.7% of non-Indigenous22), when applied to the Queensland state population20 this amounts to about 73 000 non-Indigenous and 40 000 Indigenous citizens living remotely or 35% of the remote population being Indigenous. This suggests that Indigenous people in remote Queensland have a disproportionately low likelihood of requesting medical assistance from the RFDS compared to the non-Indigenous population. This finding is despite the well-documented poorer health outcomes for Indigenous Australians23,24, including greater incidence of smoking and obesity and greater incidence of chronic kidney disease or diabetes and less likelihood of effectively managing diabetes, and suggests the Indigenous access to RFDS consultations is less than optimal.
Normative data about general practice presentations in Queensland for the period of review reveal that circulatory disorders are amongst the most frequent problems managed9, as they are for the RFDS consultations. However, in general practice, presentations for musculoskeletal, skin and respiratory disorders are equally prevalent. This may reflect a greater sense of urgency relating to cardiac problems in remote areas and the convenience factor for less urgent or debilitating conditions to be attended in general practice.
Limitations
The data collected over the review period were compared to the previous data collected in 2005–066 in order to assess trends in clinical presentations and treatment practices. The 2005–06 data extracted from that publication could not be confirmed by RFDS Queensland staff with access to the HAL, HCR and MD3 Medical Director program because details of the data collection methods were not provided6.
The medical chests are designed to fit the clinical needs of patients in rural and remote communities and their contents have been adjusted over time to best meet the demands of those communities. The changes to the contents of the medical chest since the 2005–06 review period6 were not assessed and so could influence these findings.
Conclusions
The RFDS medical chest program remains an invaluable resource for remote Australian populations. Within Queensland, the program continues to serve thousands of Australians annually through both telehealth consultations and distribution of items from the medical chests. The demand for telehealth consultations remains unchanged over the period 2005–14 but fewer items are being dispensed from the medical chests annually. The expected use of the medical chests for each diagnostic category of consultation has shown some variation over time.
The results of this study highlight the demand for the RFDS medical chest program in rural and remote Australia. It is hoped these results demonstrate the healthcare needs of Australians living in remote communities and can be used to improve the future capacity of the medical chest program. Further research is needed to assess if the changes observed since the previous review of the medical chest program are transient or progressive.
