Introduction
Deprivation of sensory functions is identified as one of the most significant negative implications of ageing1, and it is one the most common chronic conditions of later life. Hearing loss disorders are projected to be among the top 10 causes of disease burden, with disabling hearing loss affecting approximately a third of people over 65 years2. Similarly, age-related vision disorders and cataracts are projected to move up the WHO disease burden rankings3. About 65% of all people who are sight impaired are aged 50 years and older; this age group makes up about 20% of the world’s population4. Dual sensory loss or deaf-blindness, which is concurrent loss of both sight and hearing, is estimated to affect 22.5% of adults aged 65 years and older5 and approximately a third of Europeans aged over 50 years have difficulties either with hearing or seeing or both6. Given this strong correlation between sensory impairment, older age and the ageing population, the prevalence of sensory impairment will continue to rise.
Epidemiological projections of sensory impairment are a significant health concern, as evidence demonstrates that sensory impairment and associated disability increases with age7. Sensory impairment interferes with an individual’s functional ability and their everyday competence and capacity to carry out activities of daily living8-11. Additionally, sensory difficulties are strongly associated with social inactivity6 and cognitive decline12,13. It is not surprising, therefore, that sensory impairment in older people reduces quality of life11,14 and is a predictor of accidental injury or harm, for example an increased falls risk15. Sensory impairments can pose a threat to older people’s sense of dignity, for example through loss of autonomy, isolation and independence16. Given the potential association between hearing loss and social isolation in older adults, greater attention to the sensory healthcare needs of rural older adults is an important consideration.
Interventions that prevent or treat the debilitating effects of hearing loss and sight impairment in older people have been shown to have a positive impact to maintain independence and quality of life. Liaising with vision agencies or local patient support groups provides a means of additional help and support to improve a person’s quality of life17,18, and rehabilitative actions targeting sensory functions in older people can enhance their social activity6. Individuals who use low-vision services have high levels of satisfaction with such services19. Older adults who accessed different preventive and rehabilitative actions successfully adapted to sight loss with use of optical aids and assistive devices, and experienced more supportive interactions with professionals, family and friends20. It is not surprising, therefore, that recommendations for sensory care include regular screening and provision of accessible care5,11, and access to information and local services21,22. However, accessing information on rehabilitation services and referral processes can be difficult23 and rural residents’ contact with visual healthcare facilities may be even more limited than it is for those without a sight impairment24.
Barriers to sensory care are complex and multifactorial25. Hearing loss in ageing is insidious and progresses slowly, with affected individuals considering it as a normal part of ageing11. Healthcare professionals may also share this assumption. In a study on attitudes to hearing rehabilitation for older adults, 60% of medical practitioners agreed with the statement that hearing loss is a normal part of ageing that does not require treatment25. In another study, 85% of 91 older patients reported receiving no spontaneous advice from their primary care providers regarding hearing, and that patient-directed enquiries were sometimes dismissed by the practitioners12. Lack of knowledge among healthcare professionals concerning the availability of vision and hearing rehabilitation programs26, and lack of knowledge about service provision17, have been identified as barriers to seeking help for sensory impairment, yet awareness of rehabilitation services is an important predictor of the use of these services27.
One key strategy for improving access and uptake of sensory services includes targeting healthcare providers who serve older adults, with the goal of increasing regular sensory screening7. Practitioners are in a unique position to play a significant role in decision making around hearing rehabilitation25. Nurses can play a significant part in advancing this strategy through their practice in primary and community health care28. For example, nurses have a key role in recognising sensory behaviours and in maximising communication22. They can be pivotal in the assessment of hearing and in the identification of hearing loss, so individuals are appropriately referred for further testing and possible early intervention12. Despite these recommendations and the overwhelming evidence that the majority of older patients will have some degree of sensory impairment, little is known about community nurses’ awareness of impairment and the impact of that awareness, if any, on their patients.
The aim of this study was to evaluate the impact of a brief educational intervention on sensory impairment, in the form of training workshops with community nurses on their knowledge, attitudes and practice pre- and post-intervention.
Methods
Research design
Kirkpatrick’s model of training evaluation29 provided an overarching framework to evaluate the educational intervention. Conceptualised as a hierarchy of outcomes, the model has four levels. The first level of the hierarchy was ‘reactions’, and considered how well the training was received, and participants’ views of the workshops. The second level, ‘learning’, studied how and if participants’ knowledge had increased, and considered changes in attitudes and perceptions. The third and fourth levels, ‘behaviours’ and ‘results’ respectively, explored how, or indeed if, the experience changed the participants’ approach to practice and any reported practice outcomes29. Consideration of each of these levels in this study contributed to a more complete understanding of the relevance and impact of the educational intervention.
The study used a longitudinal pre-test–post-test design implemented in three phases. Pre-test–post-test designs are widely used in behavioural research, for example to compare groups or, as used in this study, to measure change following an intervention30.
Recruitment
Purposive sampling was used, and all nurses who work in community settings in the Western Isles of Scotland were invited to participate both in the workshops and in the research. Invitations for participation were distributed to each of the five locality teams across four islands in the Western Isles to obtain geographical representation of community nursing teams. If nurses chose not to participate in the research, they were still able to attend the workshops. No exclusion criteria were applied.
Educational intervention – sensory training workshops
Sensory training workshops were held with community staff in five localities in the Western Isles of Scotland and were facilitated by sensory services staff (GM, JG) with expertise in sensory training and supporting people with sensory impairment. The duration of each workshop was 3–4 hours. Workshop content included simulation practice, information on assessment and referral pathways (box 1). The workshops were interactive and simulation scenarios gave participants the opportunity to experience examples of sight and hearing impairments and their impact on aspects of daily living. Simulation is a ‘technology to replace or amplify real experiences with guided experiences that evoke or replicate substantial aspects of the real world in a fully interactive manner31. Low-tech equipment, everyday tasks and post-simulation debriefing32,33 formed the basis of simulation in the workshops. For example, wearing sight impairment simulation spectacles, participants attempted to perform simple everyday tasks such as filling out forms, opening and closing clothing buttons and managing medication.
Box 1: Sensory training workshop content
Data collection
Data for this project were collected in three phases. In phase 1, pre- and post-workshop questionnaires assessed participants’ perceptions of workshop participation and knowledge, confidence, and awareness of sensory services including referral processes to support people with sensory impairment. Participants who attended the sensory workshops (n=41) were invited to complete the questionnaires and to rate their level of knowledge on three specific areas – hearing impairment, sight impairment and referral mechanisms – on a five-point Likert scale from 1 (low) to 5 (high). There were opportunities for free-text responses about the experience of workshop participation. In phase 2, a postal questionnaire (box 2), which focused on all levels of Kirkpatrick and Kirkpatrick’s hierarchy29, was sent to all participants 3 months post-workshop to gain their views of the longer term impact of workshop participation on their practice. Open-text responses were invited from participants about any changes with their approach to communication, assessment, information provision and referral advice. In phase 3, a focus group interview was conducted with a sample of participants, 6 months post-workshop, to elicit the longer term impact of participating and perceptions of referral processes, including an appraisal of barriers or facilitators. The interview was audio-recorded and transcribed verbatim.
Box 2: Postal questionnaire content
Data analysis
The pre- and post-workshop evaluation data were analysed using descriptive statistics for each response as shown in Tables 1–3. The tables show the number and percentage of respondents to each question on the five-point Likert scale at two time points, pre and post workshop. Data were grouped into five categories: (1) low, (2) low–medium, (3) medium, (4) medium–high and (5) high. Free-text responses to questions from the postal questionnaire and data from the focus group interview were analysed using a framework approach (AS, KM), which is a deductive approach to qualitative research that is informed by a priori reasoning34,35. Responses were coded, distilled and organised as evidence related to the a priori framework29 with sections of relevant text categorised into themes and agreed by the researchers (AS, KM, AS).
Ethics approval
The study was approved by the Ethics Committee, School of Health Sciences, University of Stirling (SREC 13/14 paper no. 99). Information sheets about the study were distributed to all potential participants inviting participation, and consent was obtained from all study participants.
Results
Sensory training workshops: In total, 41 participants took part in the workshops with every participant completing the pre-workshop questionnaire and 36 participants completing the post workshop questionnaire. Participants were registered nurses working in the community (n=27), student nurses (n=4), healthcare assistants (n=8), a medical student (n=1) and a social care assessor (n=1).
Pre- and post-workshop data: Participants’ responses on hearing and sight impairments and referral processes are presented in Tables 1–3. The tables present respondents’ answers pre- and post workshops to questions pertaining to their knowledge of hearing impairment (Table 1), visual impairment (Table 2) and referral processes to sensory services (Table 3).
Postal questionnaires: A total of 41 postal questionnaires were sent to all participants who attended the workshops and 19 were returned, an overall response rate of 46%.
Focus group: A focus group interview with seven workshop participants, comprising registered nurses (n=6) and a healthcare assistant (n=1), took place 6 months’ post-workshop and lasted approximately 50 minutes.
Table 1: Knowledge relating to hearing impairment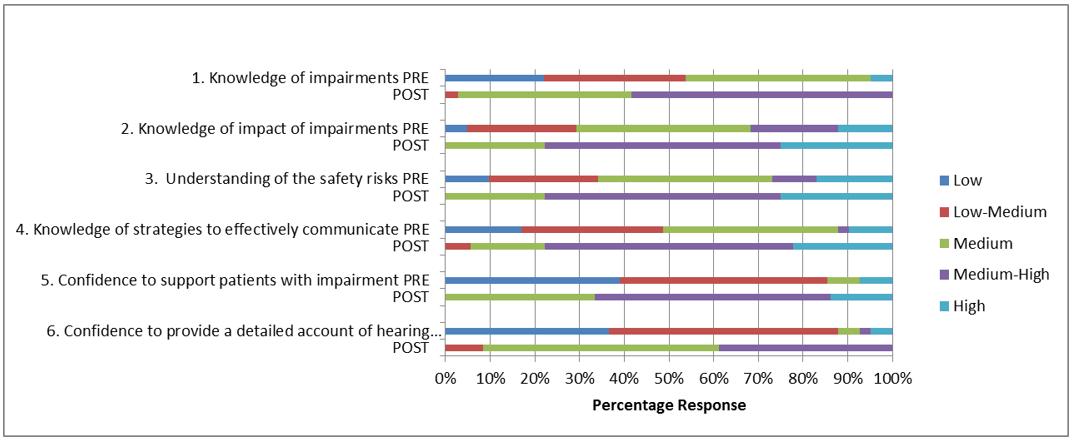
Table 2: Knowledge relating to visual impairment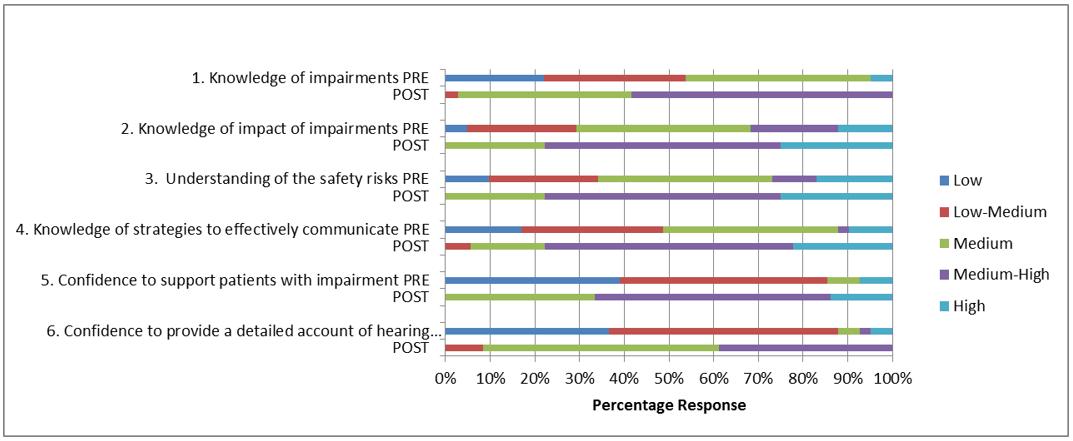
Table 3: Knowledge relating to referral processes to sensory services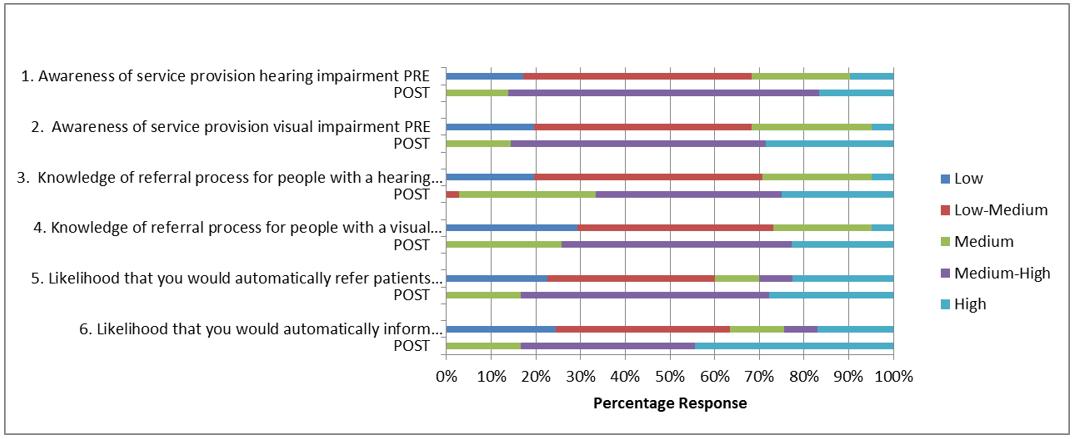
The overall findings from the pre- and post-workshop questionnaire postal questionnaire and focus groups were synthesised and are presented (reflecting Kirkpatrick and Kirkpatrick’s framework29) and categorised as follows.
Participants’ views of the workshops: Stage 1 of the hierarchy considered participants’ reactions to the workshops and how well the workshop information was received. There was consensus that participants benefited from undertaking the training workshop, stating that they found it ‘useful for practice’, ‘very helpful’, ‘interesting’, ‘informative’, ‘worthwhile’. All postal respondents indicated that their knowledge of sensory impairments improved following the workshops, including enhanced knowledge about the spectrum of sensory impairments, access to information, improved awareness of assistive devices, and increased confidence and competence to advise patients and carers.
The delivery methods, workshop duration and the experience of those undertaking the training were evaluated positively and this finding was particularly salient when reference was made to participation in the simulation activities. In the post-workshop questionnaire (PWQ), postal questionnaire (PQ) or focus group (FG), participants described an enhanced understanding of the experience of living with a sensory impairment:
Especially patients with visual difficulties and exercises with glasses helped me to understand full impact on patients. (PWQ)
Wearing the different glasses makes you empathetic and understanding of the difficulties of loss of sight and hearing. (PWQ)
The practical sessions were very informative and greatly improved the level of service I now provide to sensory impaired patients. (PQ)
The sensory training session was extremely valuable in relation to improving our interactions with sensory impaired patients. (FG)
Participants’ knowledge of sensory impairment: Stage 2 of the hierarchy considered how and if participants’ knowledge had increased, and considered changes in attitudes and perceptions. When asked about their knowledge of hearing impairments pre-workshop, only two (4.9%) participants rated this as medium–high or high. This increased to 21 (58.3%) post-workshop (Table 1). Similar findings were noted for knowledge of sight impairments, which increased from two participants (5.4%) pre-workshop to 24 (70.5%) post-workshop (Table 2). Those who rated their knowledge of the potential impact of sensory impairments on individuals’ daily lives as medium–high to high increased from 13 (31.7%) pre-workshop to 28 (77.8%) post-workshop for hearing impairment (Table 1) and from 13 (32.4%) to 26 (76.5%) for sight impairment (Table 2). Participants described their understanding of the impact of sensory impairment on patients and in doing so referred to both the physical limitations and psychosocial implications of sight and/or hearing loss:
Being more sensitive to a patient with hearing problems and how it affects their life. (PWQ)
Be more aware of how frustrating failing sight, deafness is for people on a daily basis. (PWQ)
I am more sensitive to their needs and put more input into helping to improve their activities of daily living by advising them and their relatives. (PQ)
Participants described situations where patients’ confidence and independence were compromised. Difficulties in carrying out tasks such as managing medications were noted. Most significant was the impact of social isolation, which participants suggested manifested in several ways. Loss of a driving license was described as ‘disheartening’, sight loss that affected patients who could no longer read was perceived as ‘isolating’ and made one participant ‘sad – that [she] can no longer read’.
If people have impairment they can’t drive, can’t make phone calls because they can’t hear, it means that they have to ask someone else and that’s the problem because they have lost their independence and they don’t want to be more dependent by asking people to make arrangements for them. (FG)
Hearing loss was noted to limit people’s ability to interact in groups, and background noise compromised patients who wore hearing aids. Participants noted that patients become even more isolated as friends and family members struggled to overcome communication difficulties:
Much more aware of hearing sight impairments and effect on the individual. (PWQ)
People find it difficult to be with her and not quite knowing what to do. (FG)
Participants described how workshop participation provided with a more empathetic and compassionate understanding of the impact of sensory impairment:
Increased awareness, heightened compassion/sensitivity. (PWQ)
Made us strongly aware of how diminished people’s lives are when these senses are taken away from them. (FG)
Yes, that is what the training really did – gave us empathy, whereas before we did not always understand the problems and frustrations they were actually facing. (FG)
We sympathised but didn’t really have empathy. (FG)
Change in participants’ practice: Stage 3 of the hierarchy detailed participant reported changes, if any, from their previous practice. Very few participants pre-workshop felt confident to provide a detailed account of either hearing or sight requirements in their patients’ care plans (n=3, 7.3% and n=3, 8.1%, respectively). Although there was an increase in confidence post-workshop, these figures were still low (n=16, 44.4% and n=14, 41.4% respectively), as seen in Tables 1 and 2. However, responses from the postal questionnaire indicated that attendance at the workshops had influenced participants’ (n=18) overall approach to patient assessment and there was evidence of greater awareness of the potential for sight and hearing impairments:
When patients make a little comment about hearing or seeing, I look into it more. (PQ)
Now more careful observation of hidden problems. (PQ)
I am now able to identify sensory impairment more effectively. (PQ)
I am more aware and observant of barriers. (PQ)
Participants provided examples of ways in which they had changed their practice; this included obtaining more detailed information about the nature of the patients’ impairment, strategies for support and use of aids:
I am more likely to spend more time discussing with [the] patient what the problem is and what we can do to help. (PQ)
I now ask direct questions regarding their sight and/or hearing as I feel I now know where to refer them to or what to offer regarding these problems. (FG)
The majority of postal respondents (n=17) indicated that documentation of patients’ sensory impairment, use of hearing aids and other assistive devices and specific communication strategies employed had improved. One participant who indicated that practice had remained unchanged had not come across a patient with sensory impairment since attending the workshop.
Respondents noted the value of sharing relevant information with colleagues who had not attended the workshops:
I feel I can now advise appropriately and will be advising student nurses and new staff members of the importance of addressing sensory impairment in nursing assessments. (PQ)
I have had a discussion with social care workers and highlighted the awareness of these impairments when dealing with clients and for them to relay any concerns. (PQ)
Promote the sensory service both with community teams and patients. (PWQ)
Outcome and referral to sensory services: The final stage of the hierarchy provided evidence of outcome and in particular whether participants were more likely to refer patients to sensory services. Awareness of sensory service provision increased from four participants (9.8%) rating their knowledge for hearing services as medium–high to high pre-workshop to 31 (86.3%) post-workshop and two participants (2.9%) rating their knowledge of visual services as medium–high to high pre-workshop to 30 (85.7%) respectively (Table 3). The likelihood that participants pre-workshop would refer patients with either a hearing or visual impairment for more specialist care was low with only 12 participants (29.0%) stating there was a medium–high or high chance of this happening. This increased to 30 (83.4%) after the workshop. Automatic referral to sensory services increased from 10 participants (24.4%) pre-workshop to 30 (83.3%) post-workshop (Table 3). Most participants felt they were in a better position to advise patients and others about service availability:
Much more likely to signpost people towards the services that may help. (PWQ)
Will inform patients of these services. (PWQ)
Increased knowledge of how to refer. (PWQ)
More empathy for the patient and I will encourage referral. (PWQ)
Being more aware of how to effectively refer patients to the sensory centre. (PWQ)
Yes, now much more likely to inform. It’s useful knowing they [sensory services] will do a home visit because often people who are severely disabled by problems are often older and can’t easily travel. (FG)
Participants were asked if they had informed or referred patients to sensory services post-workshop. While 12 participants indicated that they had informed patients about services, seven had not in the 3 months post-workshop. Reasons for not informing of sensory services included the need not having arisen (n=4), with participants indicating that they would inform future patients if such a need arose; some patients had previously accessed services and assistive equipment; and one of the student nurse participants did not see this as a student’s responsibility. Conversely, another student responded that they ‘felt confident enough to advise patients and carers with information’. One participant indicated that most patients were older and housebound and favoured a general practitioner or optician appointment over other services.
The majority of participants had taken the opportunity to inform patients about specialist services:
Relayed information to a housebound patient with senile macular degeneration and her daughter, discussed the sensory services with them. (PQ)
A small number (n=3) who had passed on information about services were able to identify some impact of the information on patients and carers:
Patient and daughter attended the local drop in clinic and accessed aids to help assist in daily living. (PQ)
Some have now had their hearing aids renewed. Some have sought advice for other ailments and for aids to help them. (FG)
Barriers to sensory services included reduced awareness of sensory impairment and service provision by other care providers who had regular patient contact. Participants also noted that patients themselves could be reluctant to access sensory services even when informed about the help and support available:
Some people are reluctant but mostly positive reactions. (FG)
Older ones a little reticent at first, they don’t want to put anyone at any trouble, … they will ‘oh well if it will help I will give it a try’. (FG)
Some people have been like that for so long, their impairment is what they know – and they can be resistant to change. (FG)
Discussion
With an increasing older population, the number of people living at home with sensory impairment will rise. Community nurses are ideally positioned to not only recognise these impairments in patients but also refer them to appropriate services for early intervention. This study examined the use of educational intervention to highlight the potential effects of sensory impairment on the individual and to raise awareness of services that are available.
The workshops constituted a brief educational intervention that was specifically designed to maximise the limited time available to achieve the most relevant outcomes for participants, who were mainly community nurses. Pragmatic decisions were taken about the length of workshops, which had to accommodate participants’ clinical work and travel to the workshop, with any possible infringement on personal time minimised to maximise attendance. Consideration of these factors was important as deterrents for attending continuing education included family responsibilities, travel distance and inability to get time away from work35, which can be further exacerbated in a remote and rural context36.
One important element of the workshop was the opportunity for participants to experience simulated scenarios that re-created common potential challenges for people with sensory impairment. Simulation in nursing education is often associated with skill acquisition37 and an aid to clinical decision-making38. In the workshops, low-tech solutions such as simulation spectacles helped to create an environment that supported the development of more affective aspects of nursing care39 through enhanced empathy and understanding of the disabling impact of sight and/or hearing loss. Opportunities for debriefing, considered the most important stage of simulation40, supported individual and group reflection about the community nurses’ role in recognising the impact of sensory impairment.
It was notable from the findings of the pre-workshop questionnaire that participants’ awareness of the incidence of sensory impairment was low; this is significant as it is highly probable that most patients cared for in rural communities are older and hence are more likely to experience a sensory impairment. This was not a surprising finding as the incidence and impact of hearing and sight impairment is underestimated in health care22. However, there was an improvement in participants’ knowledge of both sensory impairments and associated disability post-workshop, with evidence that this was sustained even at 6 months post-workshop, positively impacting on participants’ practice.
Participants described increased awareness of the potential for sensory impairment in their patients. Given the high occurrence of sensory impairment in older adults, and the strong associations between sensory impairment and cognitive decline8,13, some of the negative consequences of sensory impairment may be alleviated if professional caregivers recognise behaviours indicative of sensory impairment22. Additionally, participants described greater understanding and empathy with patients who experience sensory impairment, a more robust approach to patient assessment to identify impairment, and increased likelihood to inform of, and refer to, sensory services. These are important outcomes as reports from people with sight impairment and/or hearing impairment suggest that healthcare professionals often lack adequate awareness, sensitivity and skill for accommodating sensory impairments in daily practice41,42.
Pre-workshop, few participants felt confident to assess patients with either a hearing or sight impairment, and this uncertainty remained post-workshop. This was not a surprising finding as hearing and visual assessments were not included in the workshops and are best provided by the relevant sensory specialist. However, what was more relevant for the majority of community nurses was a change in their approach to patient assessments, with greater evidence that they increasingly considered the potential for sight and hearing impairments, were more likely to discuss sensory impairments with their patients and document that assessment. This is an important outcome as early detection of sensory deterioration and appropriate interventions may help to mitigate the detrimental outcomes related to both hearing and sight impairment42,43. Additionally, the importance of other care workers having the knowledge to provide similar support for people with sensory impairment was emphasised by participants. Nurses and care assistants can have key roles in regular screening of older patients, and in referring them to sensory services22.
Within Scotland and the UK, access to information and specialist services have been recommended as important aspects of service provision to support people with sensory impairments21,44 along with the need to redirect resources towards more targeted preventative strategies that include the provision of information and advice in relation to specific conditions21. During the workshops, participants were provided with information about sensory services and referral pathways into services. This information was inclusive of clinical services that support sight and hearing loss, and third sector agencies that provide specialist advice and support. Subsequently, most participants stated that they were more likely to refer patients, and provided examples where referral had occurred. Similar findings have been reported elsewhere where study participants felt more confident detecting hearing difficulties and were more empowered in seeking referrals45. Referral information was an important aspect of the workshops as provision of effective and accessible eyecare services is key to effectively controlling sight impairment, including blindness46.
Only a small minority of participants indicated that they would not be likely to refer, because, for example, they viewed this as the doctor’s role. This perspective is contrary to guidance that advocates for a partnership approach and the active engagement of a wide range of statutory and third sector agencies, which are considered central to the success of good sensory care17. Importantly, to offer advice and direct to patients to sensory services, community nurses and other healthcare professionals need to be aware of the services and the referral pathways that are available.
Participants in this study suggested that some patients may have become resigned to their condition and are therefore reluctant to seek advice about their impairment. There may be a reluctance by patients themselves to acknowledge their own hearing or sight impairment47,48, possibly because they consider impairment as a normal consequence of ageing49 or because they may be embarrassed to admit to that impairment, and any perceived associated stigmatisation47,50. Furthermore, older adults in rural communities perceive several barriers to general healthcare access, including problems with transportation, limited healthcare supply, lack of quality care, social isolation, financial challenges and fear of loss of independence51,52. Raising the general profile of sensory impairment and its impact may help to develop better awareness; for example, recommendations that eye health needs to be included in broader non-communicable and communicable disease frameworks46 might be appropriate.
The clear association between population ageing, sensory loss, cognitive and physical decline and associated disability cannot be ignored. With greater understanding and knowledge of these associations, a multi-faceted approach to interventions, which includes holistic assessment, can be helpful53. Nurses can make an important contribution to that approach including referring patients to services that can help them to adjust and compensate for their sensory loss. Through better awareness, creation of new policies and services to support individuals and their families, there is significant potential to improve their capacity to be independent and to optimise their quality of life54.
Conclusions
The results of this study begin to address the gap in sensory education for healthcare professionals in general and community nurses in particular. Accessible training programs for healthcare workers that focus on sensory impairment challenges including simulation and relevant interventions can help support improved patient outcomes. This study was carried out in an area where accessible service provision, including referral pathways for people with sensory impairment, is well established, which perhaps influenced workshop participants’ perceptions and confidence. The sample was drawn from a single rural island Health Board within Scotland and included mainly community nurses rather than other healthcare providers. The views of other health and social care professionals are equally valid and may help to identify further education needs and services gaps that can help to inform a multidisciplinary approach to address the needs of older people with sensory impairment in the community.
The study helps to demonstrate the importance of raising awareness of sensory impairment with healthcare workers and community nurses. From a preventative standpoint, there is good evidence that correcting hearing and sight impairments can lead to improvement in the quality of life and functional status of older people13 and this evidence in itself supports the importance of awareness raising and education about sensory impairment. Even mild impairments exert a toll on older adults42, yet most sensory problems are potentially treatable or relieved by interventions and environment adjustments44. Community nurses are often well placed to identify sensory impairment, associated disabilities and patients at risk of injury, and nurses usually have high public visibility in small communities54. Accessible and relevant education about sensory impairment for all health and social care professionals who deliver direct care to older people across all care settings is therefore highly relevant to facilitate both recognition of that impairment and access to appropriate interventions. With the population of older people ever expanding, the impact of sensory impairment is likely to become an increasingly significant health and social care burden without due attention to appropriate training of health and social care professionals.
Acknowledgments
We are grateful for the support of Gillian Mitchell (GM) and John Gill (JG) from Sight Action services who helped inform the development and delivery of the simulation workshops. This work was supported by the Queen’s Nursing Institute, Scotland who funded this project as part of the Delivering Dignity Programme (ENASI01).



