Introduction
In the second half of the 20th century, the number of children in childcare centers (CCCs) in several countries increased rapidly due to increasing numbers of mothers taking up employment1-4. The quality of care provided to young children has impact on the development and learning abilities of children including in the areas of language, literacy and mathematics5,6. Higher quality child care has been shown to predict greater school readiness for children aged 4.5 years, reflected in standardized tests of literacy and number skills6,7. However, previous studies reported that children in CCCs were at higher risk for infections due to low resistance2,8. Sickness in children aged less than 5 years impacts on their health, growth, optimal development and may cause serious complications without timely and proper care. Children’s sickness also increases family expenses and parents’ absence from work or other duties. The standard of care for children in CCCs should therefore be a concern for the management of the CCCs.
CCCs in Thailand were established by several different organizations. For example, CCCs have been established by the Local Administrative Organization (LAO), part of the Bureau of National Board for Primary Education; by the Department of Community Development, under the Ministry of Interior; and by the Department of Religions, located in the areas around temples and mosques. The decentralizing of government organizations in 1999 resulted in the transfer of authorities in line with the new National Education Act. Since 2002, all CCCs have been under the Department of Local Administration, authorized by the LAO. The CCCs are supported with academic guidelines, budget and training, and their purpose is to prepare children aged less than 5 years for primary school. CCC management is the responsibility of local administrators(s) and center heads. Management includes setting administrative structures and authority lines, and budget allocation9,10,10,11.
To standardize the quality of all CCCs in Thailand, quality standards for CCCs were set by two ministries, the Ministry of Interior and the Ministry of Public Health. Through the Department of Local Administration, the Ministry of Interior looks after six of the criteria: management of CCCs, personnel, building and environmental safety, academic program and activities, stakeholder participation and network promotion with child development organizations. The Department of Disease Control and the Department of Health, under the Ministry of Public Health, take care of disease prevention and control, physical checks of caregivers, sanitation and environment, instruments and supplies for disease prevention and control, growth monitoring, and overall health and food arrangements. There is a checklist for assessment of each criterion11. The most recent survey is from 2011. This survey shows 20 043 CCCs across Thailand. The highest numbers of CCCs are in Ubonratchathani, Udonthani and Chonburi provinces9. A 2009 survey showed that 9% of CCCs in Thailand could achieve the quality standards of child development centers set by the Department of Health at the excellent level and 34% could achieve the good level. The excellent and good levels reflect higher control of infectious diseases10,10.
Chonburi Province, with the third highest numbers of CCCs in Thailand and the highest number in the eastern region, has 210 CCCs under its LAO12. A study by Chonburi Provincial Health Office (CPHO) and Regional Health Promotion Center in 2011 found that 50% of these CCCs did not meet the quality standards of child development centers13. The 2007–2012 diseases surveillance report from CPHO revealed that the common infectious diseases in children nationwide aged less than 5 years were the common cold; hand, foot and mouth disease (HFMD); chickenpox; diarrhea; conjunctivitis; and mumps14. These diseases and symptoms were most commonly found in CCCs, where many children were together in the same place. A 2011 survey by CPHO found that, at the district level, Phanatnikhom had the highest number of CCCs in Chonburi Province and 68.8% (33/48) of these did not meet the quality standards of child development centers12. The common problems found in some CCCs were toilets in poor sanitary condition, meals/food given not being nutritionally sound, and inadequate budget allocation.
The two most common symptoms found in these CCCs were the common cold and diarrhea. These results, and others, suggest there is a strong need for improvement in Thai CCCs. One way to this is through a well-designed capacity building program. The present study aimed to test the effects and impacts of the capability development program of the LAs and CCC heads.
To understand the quality issues in CCCs, before conducting the main study, the principal investigator and CPHO staff conducted two group interviews with 30 CCC caregivers for situation analysis. The results indicated that there was no participation in CCC planning from stakeholders, a lack of understanding of the quality assessment by LAs, inadequate budget and materials from local government, poor morale among caregivers due to workload and insufficient income, and poor cooperation from the children’s parents. Most problems were related to management skills of LAs and CCC heads. These results were reported to Chonburi Provincial Health Office13.
In this study a participatory capacity building approach, adapted from a method used by the United Nations Development Program15,16 , was implemented. The program targeted LAs and heads of CCCs and aimed to improve the quality of CCCs and reduce the period prevalence of three diseases and two symptoms. The focus diseases and symptoms are those required by the quality standards of child development centers to be controlled. Capacity has been defined as the motivation and ability to identify, prioritize, plan, implement, evaluate and sustain health interventions17. For this study capacity building was defined as the process by which LAs and heads of CCC would develop their abilities to perform managerial tasks, together with increasing their knowledge of the quality standards for CCCs (QCCC). Although the focus was on LAs and CCC heads other stakeholders were included to increase the success of the intervention program. This study aimed to describe the effects and impacts of the participatory capacity building development for improving the quality of CCCs in Chonburi Province.
Methods
This study employed a quasi-experimental, one group pretest–post-test design. The program aimed to improve CCCs’ abilities to meet the quality standards of the Department of Health by building the capacities of LAs and heads of CCCs. The capacities focused on knowledge of the QCCC and management skills. The approach was a modified version of the United Nations Development Program’s (UNDP’s) five-step participatory approach to capacity development15,16. The program ran between February 2014 and February 2015.
The study site was Phanatnikhom District, the district with the most CCCs in Chonburi Province. All study CCCs were located outside the municipal area, as shown in Figure 1. Example pictures from study CCCs are presented in Figures 2–5. The study population was purposively selected. A total of 48 CCCs represented by 21 LAs were selected. The inclusion criterion for heads and LAs was that that they had been in the position for at least 1 year. Anyone who took extended leave, for any reason, during the study period was excluded.
 Figure 1: Map of Chonburi Province, showing the location of Phanatnikom District, Thailand.
Figure 1: Map of Chonburi Province, showing the location of Phanatnikom District, Thailand.
 Figure 2: Childcare center established by a temple.
Figure 2: Childcare center established by a temple.
 Figure 3: Childcare center established by a Local Authority Organization.
Figure 3: Childcare center established by a Local Authority Organization.
 Figure 4: Some childcare centers are crowded, without enough space per child for some activities.
Figure 4: Some childcare centers are crowded, without enough space per child for some activities.
 Figure 5: Children taking a 1 h nap in the afternoon.
Figure 5: Children taking a 1 h nap in the afternoon.
The process for improving the capacity of participants in this study was composed of six steps modified from the five-step UNDP framework15,16. Reinforcement was added as a step up before the final evaluation step (Fig6). All activities were divided into four phases: preparation, implementation, reinforcement and evaluation.
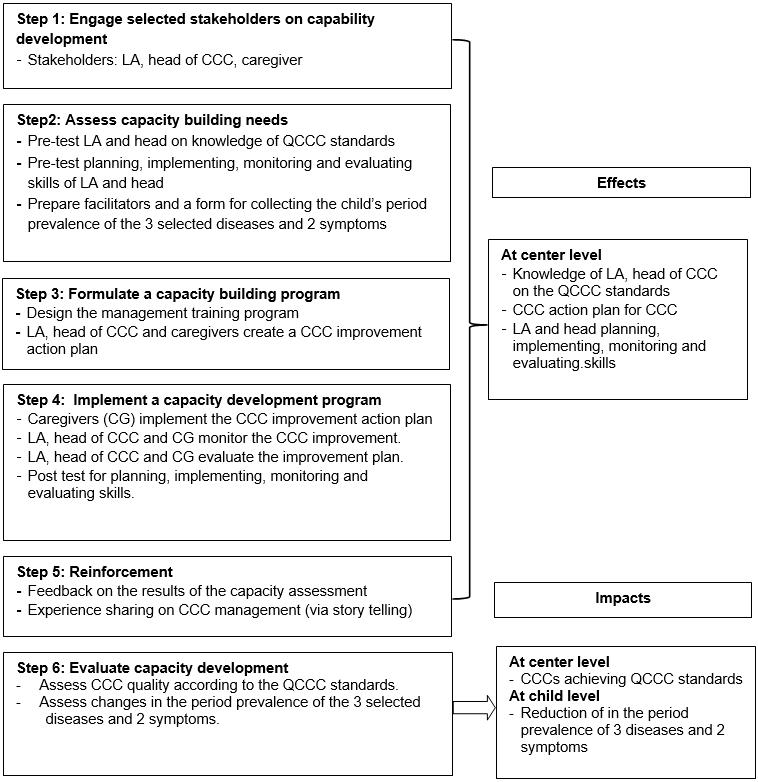 Figure 6: Participatory childcare center capacity building framework for local administrative organization.
Figure 6: Participatory childcare center capacity building framework for local administrative organization.
Phase 1: Preparation (2 months)
Step 1: Engage selected stakeholders on capability development: The stakeholders chosen for this study were (1) three district health personnel, who were individually in charge of the district’s health promotion, disease control and dental public health personnel (purposively selected to be training facilitators) and (2) six LAs and 48 heads of CCCs.
Step 2: Assess capacity needs: All participants’ capacity was pretested using questionnaires developed by the Department of Health0. They comprised a self-assessment questionnaire on knowledge of QCCC, planning, implementing, monitoring and evaluating; and a 20-item questionnaire for self-assessment of managerial skills. A form for collecting information about each child’s occurrence of three diseases and two symptoms was prepared for the next phase.
Phase 2: Implementation (8 months)
Step 3: Formulate a capacity building program: The management training program was designed based on the pretest results. The program aimed to increase knowledge of QCCC and managerial skills. The key activities were the three workshops:
- 3.1: The first 3-day workshop aimed to increase knowledge of the QCCC and problem analysis, priority setting and planning skills. On the last day of the workshop, LAs and heads of CCCs as well as caregivers from each CCC collaboratively developed an action plan for their CCCs. The focus of the action plan was meeting the QCCC.
Step 4: Implement a capacity development program:
- 4.1: Action plan in place for 3 months after the first workshop.
- 4.2: The 48 CCCs were assessed according to the QCCC. Data concerning the children’s period prevalence of the common cold, HFMD, chickenpox, conjunctivitis and diarrhea was gathered from CCC health records.
- 4.3: The second 1-day workshop aimed to increase capacity concerning supervision and monitoring. During the workshop, the action plans for CCCs were reviewed and their level of implementation discussed and noted. Any activities that had not yet been implemented were revised as appropriate.
- 4.4: The revised action plan was implemented for another 3 months.
- 4.5: The third 1-day workshop aimed to increase participants’ ability to carry out evaluations. The CCC action was revised again.
- 4.6: At the end of the third workshop, the participants completed a self-assessment of their knowledge of the QCCC and their managerial skills.
Phase 3: Reinforcement (1 day)
Step 5: Reinforcement activity: This step was added to the UNDP steps to empower, using positive reinforcement, LAs and heads of CCCs who had not been able to implement their action plans. The storytelling from LAs and heads of CCC who had successfully implemented their action plans in their CCCs provided positive examples and inspiration.
Phase 4: Evaluation (1 month)
Step 6: Evaluate capacity development: After the reinforcement phase, two evaluations were conducted:
- 6.1: A total of 48 CCCs were evaluated according to the QCCC. Results before and after implementing the capacity building were compared.
- 6.2: Secondary data, before and after implementing the action plan, regarding the period prevalence of the selected five diseases (common cold, chickenpox, HFMD, diarrhea and conjunctivitis), were evaluated and compared. Disease data were collected from May 2013 to April 2014 and from May 2014 to April 2015.
Measurements
Checklist of QCCC: The checklist was developed by the Department of Health0. There are 109 items across six criteria. The maximum total score is 100. The points are divided in the following way: personnel, 8 items, 20 points; growth monitoring, oral health and food arrangement, 42 items, 20 points; development and learning according to children’s age, 15 items, 25 points; arrangement of the inside and outside environment, 25 items, 15 points; infectious disease prevention and control, 12 items, 10 points; and participation of parents, community, local organizations and others, 7 items, 10 points. The checklist uses dichotomous questions in a yes/no format. To achieve the QCCC standard a CCC must reach at least 80% in both their total score and in their score for each criterion.
Knowledge of QCCC: A self-assessment questionnaire on knowledge of the QCCC0 was used. The same six criteria as the checklist were used. There were 44 yes/no questions. A score of 1 was given for a correct answer and 0 for an incorrect answer. A total score of 0–25 was classified as ‘need for improvement’, 26–34 as ‘fair’ and 35–44 as ‘good’. The Cronbach’s alpha coefficient was 0.82.
Managerial skills: Managerial skills were evaluated with 20 self-assessment questions0. Examples include: ‘you are able to create goals in line with your areas of responsibility’; ‘you are able to identify problems in your areas of responsibility’; ‘you are able to conduct problem analyses’; ‘you are able to set priorities’; and ‘you use a participatory management approach’. Responses were rated on a four-point rating scale: 0 = ‘not able to do at all’; 1 = ‘able to do but need close supervision’; 2 = ‘able to do with some supervision’ and 3 = ‘able to do without supervision’. A total score of 0–35 was classified as ‘need for improvement’, 36–47 as ‘fair’, and 48–60 as ‘good’. The Cronbach’s alpha coefficient was 0.78.
Diseases record form: The form is used to monitor incidents of the five diseases that are required to be controlled in CCCs: diarrhea, conjunctivitis, chickenpox, HFMD and the common cold0.
Statistical analysis
Number, percentage, mean, median and standard deviation were used to describe the characteristics of the CCCs and the study population. Wilcoxon signed rank test was used to compare knowledge of the QCCC and managerial skills before and after capacity building and the disease period prevalence before and after implementing CCC improvements. The McNemar test was used to compare QCCC results before and after implementing CCC improvements. Significance was set at p<0.05.
Ethics approval
The Ethics Committee of the Faculty of Public Health, Mahidol University approved the research protocol (COA No. MUPH 2013-042; 22 January 2013). All participants were clearly informed of their rights and any risks associated with participation. Verbal consent was obtained from all interview participants.
Results
Baseline characteristics of participants
The six participants were female and aged 30–39 years, all had completed a bachelor degree and 50.0% had been in the management position for at least 5 years. All reported previously receiving managerial skills training: 50.0% in planning, 16.7% in planning and problem analysis and 33.3% in monitoring and evaluation.
The 48 heads of CCC were female. A total of 54.2% were aged 30–39 years and 91.7% had completed a bachelor degree. A total 60.5% had been in the position for at least 5 years. All reported previously receiving managerial skills training: 50.0% in planning, 27.1% in problem analysis and planning, and 22.9% in monitoring and evaluation.
Effects of capacity building at center level
After implementing the program, the overall knowledge of QCCC among LAs and CCC heads was significantly increased (p<0.05). The overall managerial skills of CCC heads was also increased (p<0.05). However, although overall managerial skills of LAs at a good level increased from 66.7% to 100% (Table 1), the change was not significant (p=0.107). Looking further at overall knowledge of QCCC among six LAs, the criteria for which all participants could not reach 100% at a good level of capacity were personnel (caregivers’ qualifications, physical and mental health, training and development, and child/caregiver ratios, only 66.7% reached the level of ‘good’), infectious disease prevention and control (66.7%), and development and learning according to children’s age (83.3%). Among the 48 heads of CCCs, the criteria with a low proportion of participants reaching ‘good’ were growth monitoring, oral health and food arrangement (68.8%), personnel (child/caregiver ratios, 75.0%), and infectious disease prevention and control (83.3%) (Table 2).
For LAs’ managerial skills after capacity building, 83.3% reported they were ‘able to do with some supervision’ or ‘able to do without supervision’ for most skills in the list (data not shown). For CCC heads’ managerial skills after capacity building, 4.2% reported ‘not able to do at all’ for developing an implementation plan to fit the strategic plan, and 10.4% reported ‘able to do but need close supervision’ for the following items: ‘analyze strengths and weaknesses of the organization’; ‘use analysis of organizational strengths, weakness, opportunities and threats to develop a strategic plan for solving problems’; and ‘use a participatory management approach’ (Table 3).
Table 1: Local administrator and childcare center head overall knowledge of quality standards of childcare centers and their overall managerial skills before and after implementing the capacity building program 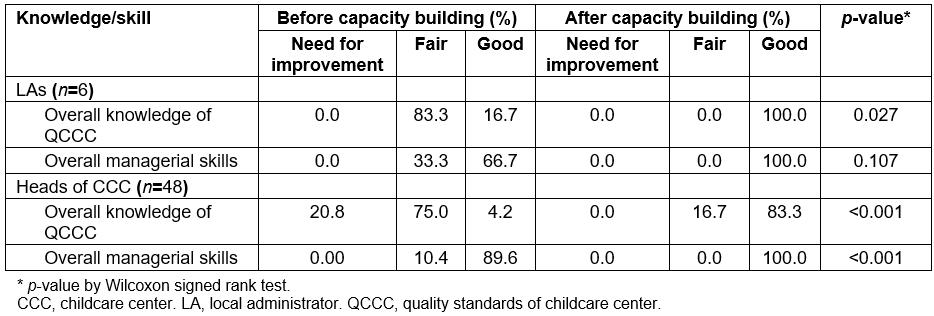
Table 2: Local administrator and childcare center head knowledge of six criteria of quality standards of a childcare center (n=48)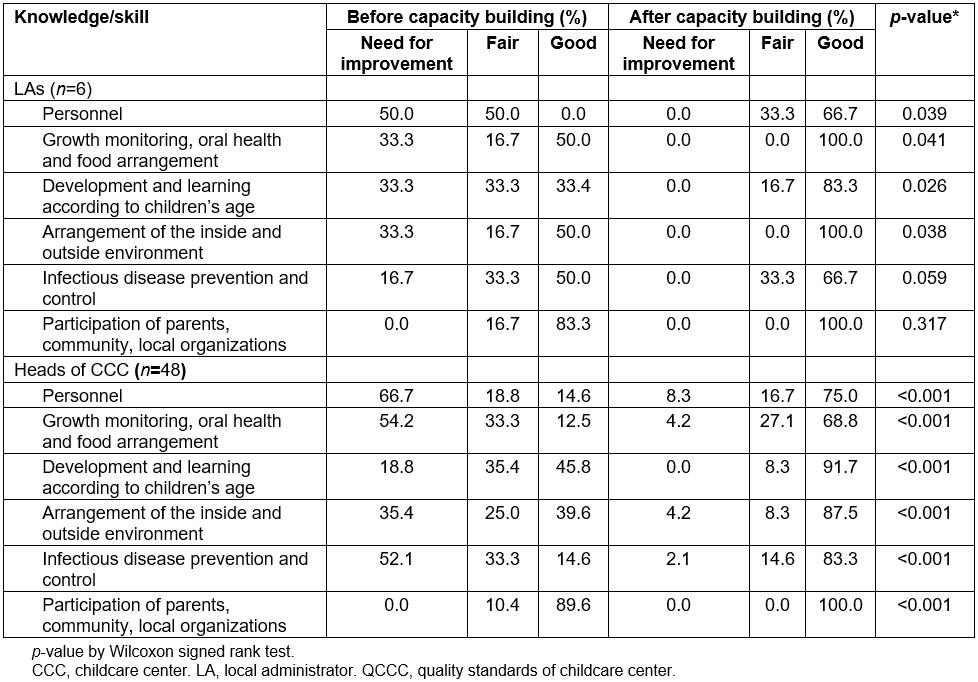
Table 3: Heads of childcare center managerial skills before and after implementing capacity building (n=48)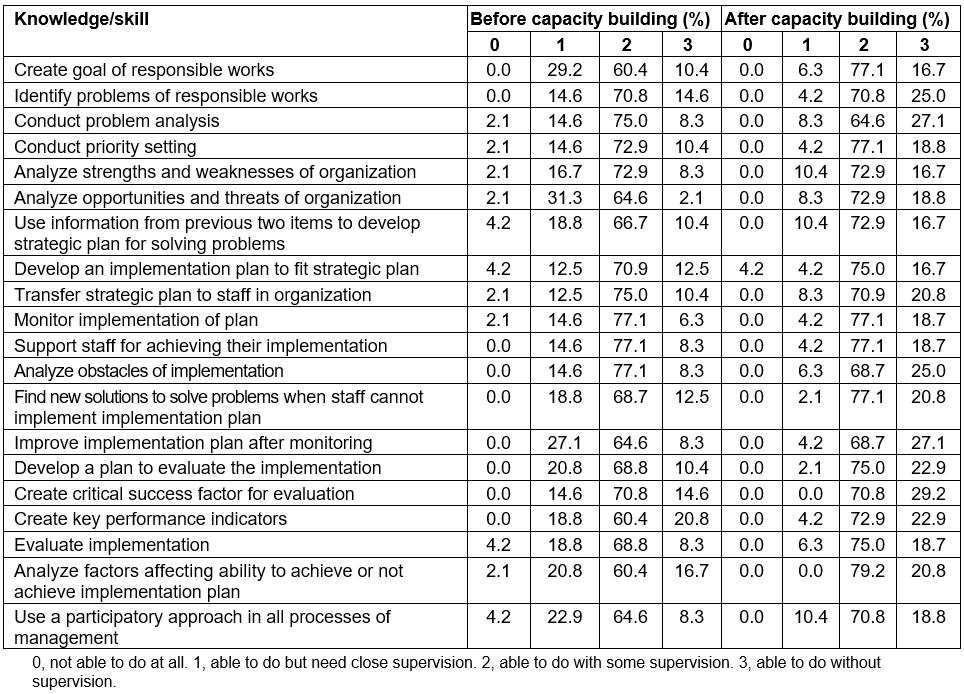
Impacts of capacity building at center and child levels
After implementing the capacity building program, the number of CCCs achieving the quality standards significantly increased (p<0.001) for both individual items and all criteria. The proportions of CCC achieving the QCCC standard in all criteria increased from 2.1% to 64.6%. The criterion with the highest proportion of CCCs achieving the QCCC standard was ‘arrangement of the inside and outside environment’ (87.5%), while the criterion with the lowest proportion was ‘participation of parents, community, local organizations and others’ (64.6%), as shown in Table 4. At the child level, only the period prevalence of chickenpox and diarrhea was reduced (Table 5).
Table 4: Proportion of CCC achieving the quality standards of a childcare center before and after implementing capacity building for local administrator and head of childcare center (n=48)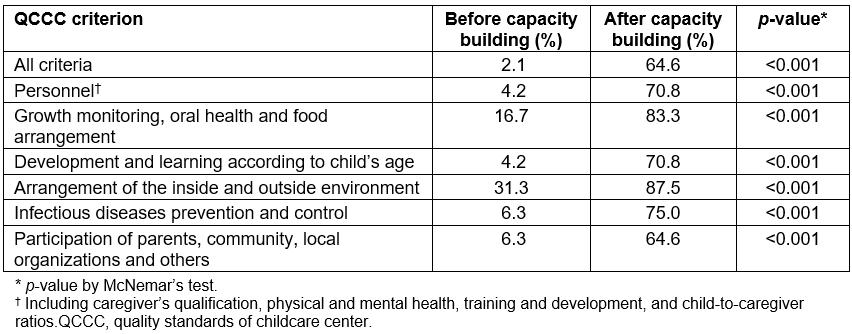
Table 5: Period prevalence of the infectious diseases required to be controlled in childcare centers, before and after implementing the capacity building program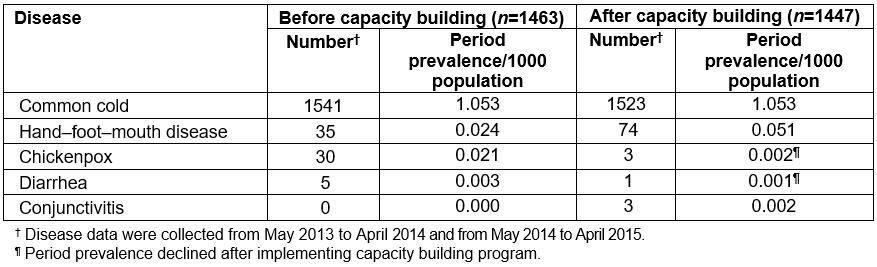
Discussion
This capacity building training program is an intervention using a participatory approach adapted from the UNDP framework. It aimed to increase the capacity of LAs and heads of CCCs in order to improve the quality of CCCs in Phanatnikhom District, Chonburi Province. This study found CCCs under LAO management lacked caregivers. About 65% of the CCCs in the study reported child-to-caregiver ratios around 20:1. This does not meet the quality standard of a maximum of 10 children to one caregiver. This is similar to the finding of Sueluerm et al5 who reported the child-to-caregiver ratio in Chonburi Province to be 20:1. This is considered a heavy workload for caregivers. An explanation for the low numbers of caregivers is that there is no career ladder for the caregivers as they affiliated to the local authority and restricted by its organizational structure.
Capacity building
After implementing the program, LAs’ managerial skills were not significantly improved (p=0.107). A possible explanation was that, before implementing the program, 83.3% of LAs reported they were already ‘able to do with some supervision’ or ‘able to do without supervision’ for most skills. In addition, there were only six s, a small study sample. Although 100% of LAs had overall managerial skills scores at the ‘good’ level there was no significant change. In contrast, before implementing capacity building, heads of CCCs rated many skills items as ‘able to do but need close supervision’ and some skills as ‘not able to do’. This means there was greater room for improvement, and a significant change in managerial skills items was seen in this group (p<0.001). The reason for the positive results might be the addition of the positive reinforcement step. Some heads of CCCs reported that the experience sharing activities in the reinforcement step helped them learn the ‘hows and whys’ of improvement. They felt the practical experiences shared were not difficult to perform and could be applied in their CCC. This was similar to the finding of Lamkar et al18. Participatory workshops focus on more practice than lectures and are seen to strengthen the ability and skills of participants, increase working efficacy and increase problem solving19.
Impacts of capacity building
At center level: The number of CCCs achieving the QCCC standard significantly increased (p<0.001) both in individual items and overall criteria. Experience sharing in the reinforcement step helped LAs and CCCs to apply the knowledge gained to improve their CCC before the final evaluation step. This was similar to the finding of Sripen and Noichun20 where the results of CCC management by the LAO were at a good level due to participation of caregivers in problem solving. A total of 81.2% of the CCCs did not achieve the targets relating to toilet use. It was revealed for these CCCs that the toilets-to-children ratio and the size of toilet were not in accordance with the standard criteria. This is because most CCCs were primary school classrooms previously. They are still located within primary schools and share toilets with the school. This was also a finding of Pongsanit et al21 in Saimoon District-Municipality, Yasothon Province.
At child level: After implementing the capacity building program, only the period prevalence of chickenpox and diarrhea symptom were reduced. The period prevalence of the common cold symptom was still high. This is likely because the children stay together all day. There is little control once a child is sick. Training and support should be given to encourage caregivers to perform health screening before accepting children into the CCC in the morning. In addition, hand washing should be monitored to observe whether it is done correctly and if the children understand the guidelines on hand washing.
Lessons learned
The quality standards of CCCs are important and the guidelines allow administrators, heads and caregivers to know what to do and how to do it. The guidelines focus on the health of the children, including their growth and learning. However, the guidelines are not as clear as they could be and between the Ministry of Interior and Ministry of Public Health many criteria are repeated. Therefore, it is important to let local authorities set up the criteria that measure what happens in reality and meet the quality standards of both ministries. This is an opportunity for collaboration and avoids confusion when a CCC is evaluated.
The approach of having participation from both ministries, including using skilled workshop facilitators from the Ministry of Public Health, is acceptable. The two ministries can work closely with the local administrators and heads of CCCs. From the dialogues with several participants, the action plans drawn up met the needs of the implementers (the caregivers) and served the needs of the parents and community afterwards. This study made it clear that the local authority’s capacity should be continuously enhanced, in particular in situation analysis and monitoring and evaluating. To make a program sustainable, involvement from all stakeholders and strong support from the local authorities are needed22,23.
Strengths and limitations
By involving local administrators from the very beginning of the process the authors strengthened the program. It is the local administrators who are authorized to make policy and allocate budget to improve the CCCs. By involving the local administrators they had a greater engagement with the plans for improvement.
This study had three limitations. First, there was no comparison group in this study. This was because the other districts had few CCCs and thus a different set of issues. Second, parents, health personnel and other groups in the community were not included as participants in the three workshops. This was because the authors felt there would be a lack of trust between the LAs and heads and the other stakeholders. Third, the assessment of the LAs and heads involved only self-reporting. Some participants with low confidence may underestimate themselves. Some may overestimate themselves as they do not want to look unqualified for their job. However, participants were reminded that the assessment results would not be shared with their supervisors. During the study period, there were not any other programs or interventions in the study CCCs. Therefore, the results of this study are likely to be due to the program only. As the context of local administration is particular to local and national governance, it can be difficult to generalize conclusions to include other countries. However, the approaches can be applied in Thailand. The finding that stakeholder participation at all levels makes programs sustainable can be applied to a wider range of contexts.
Conclusion
This study has shown that enhancing the managerial skills of the administrators and heads of CCCs is needed for CCCs to meet the quality standards set by the local authority and the Ministry of Public Health. Participatory capacity building is an appropriate way to enhance the managerial skills of LAs and heads of CCCs for improving quality of childcare centers.
Acknowledgements
This study was supported by the Praboromarajchanok Institute of Health Workforce Development and Sirindorn College of Public Health, Chonburi. China Medical Board and the Faculty of Public Health, Mahidol University financially supported the publication of the study. This article is a partial fulfillment of the requirements for Doctor of Public Health, Mahidol University for Mrs Hataya Petcharoen.





