Introduction
In Scotland in 2011/12, the ambulance service responded to approximately 8900 adult out-of-hospital cardiac arrest (OHCA) calls, for 5% of which the patient survived to hospital discharge1. Many of these survivors experienced some form of cognitive impairment2,3. Chances of OHCA survival are most affected by early recognition, prompt and good quality cardiopulmonary resuscitation (CPR), and early defibrillation. Unfortunately, the window of opportunity to influence outcome is a matter of minutes4,5 – an even greater challenge in more rural areas.
In 2015, the Scottish Government set out a strategy for improving the survival rates for OHCA. The aims of the strategy were to save 1000 more lives overall by 2020 and ‘to strive to ensure that communities in remote and rural locations have equity of treatment for OHCA’1. A study into OHCA in Norway demonstrated that a survival rate of 25% is achievable and found a positive correlation between survival and whether bystander CPR was delivered6. Therefore, targeted efforts to increase CPR training and improve bystander CPR in rural communities, where the survival rates are currently lowest, could have a significant effect4.
A significant barrier to the delivery of effective bystander CPR is the lack of education in basic life support skills7. Given approximately 18% of the Scottish population live in remote and rural areas8, the need for effective bystander CPR is even greater due to longer emergency service response times. Limited access to training due to cost or location has been identified as a significant problem for the provision of classroom-based bystander CPR training9. This raises the question of whether non-classroom-based methods would be equally effective, and could improve access to courses and increase the number of people trained in CPR. The implications of this could be significant in reducing training costs and subsequently increasing the reach of training programs and numbers of people being trained. An increased number of trained responders could directly improve survival rates of OHCA for those living in rural areas.
The aim of this systematic review was to analyse articles that compare traditional classroom-based CPR training with non-classroom-based methods of training, in order to find out if non-classroom-based methods are as effective as or superior to classroom-based CPR training. The research question was, ‘Is non-classroom-based CPR training for bystanders as effective as classroom-based training, as defined by hand positioning, chest compression depth and compression rate?’
Methods
Eligibility
For studies to be included in this review they had to meet the following criteria. The participants had to be non-healthcare professionals (bystanders), including both adults and children. The intervention was any method of non-classroom-based CPR training, for example using videos. The comparator had to involve classroom-based CPR training. Trials that compared one method of non-classroom-based training with another were excluded. Trials where either the intervention and/or comparator group studied paediatric basic life support, automated external defibrillation only training, more advanced life support training or training in in-hospital cardiac arrest were excluded. Trials had to use mannequins to assess CPR performance, and report at least one of the following outcomes: ‘hand positioning’, ‘chest compression depth’ or ‘compression rate’. These outcomes have proven to be important measures of CPR effectiveness; chest compression rate10 and depth11 have been associated with improved survival rates, and correct hand positioning on the lower third of the sternum has been associated with improved physiological outcomes12. It was also required that studies be randomised controlled trials in order to select the highest quality evidence13.
Search strategy
A database search was carried out systematically in both the Ovid Medline (1946 to May week 1 2017) and Embase (1974 to 2017 week 20) databases. MeSH terms, where they existed, were combined with ‘text word’ options that limited the keyword to the title or abstract. Search terms included:
- training
- (cardiopulmonary resuscitation, cardiac arrest, heart arrest) combined with OR
- (video recording, video-audio media, video, mobile app, mobile application, mobile phone, cell phone, DVD, telemedicine, distance education, face to face, classroom, self-instruction) combined with OR
- (Bystander, layperson, community, workplace, office, school, public) combined with OR.
1, 2, 3 and 4 were combined with AND, then limited to randomised controlled trials.
Common journals that appeared in the search results were then searched manually for relevant articles using that journal’s website search engine. The reference lists of papers obtained from the original database search were also scoured for further articles. These hand-searching methods resulted in five articles, two of which were included in the final review. Articles were screened independently by two authors for inclusion/exclusion using the criteria outlined, and any disagreements were resolved amongst all the authors.
Critical appraisal
Full texts were obtained and distributed amongst the authors so that each study was independently appraised twice. The Scottish Intercollegiate Guideline Network checklist14 for randomised controlled trials was used to assess the internal validity of each study and any discrepancy between the authors’ findings were noted, discussed and resolved either between the two authors or within the whole group if necessary. Cochrane guidance15 for systematic assessment of bias was used to allow the authors to determine the type and extent of bias each study was at risk of.
Data extraction and interpretation of outcomes
Outcomes of baseline and post-intervention testing for both the intervention and comparator groups were reviewed independently by two authors, along with demographics of the study groups and information about the type of intervention. These included video length, mannequin type and time at which the testing took place.
Results
The search identified 47 articles. A total of 39 articles were excluded manually from the study, 36 after screening abstracts and three after screening full texts. Reasons for exclusion are shown in Figure 1. After excluding irrelevant articles, eight full texts were included in the study.
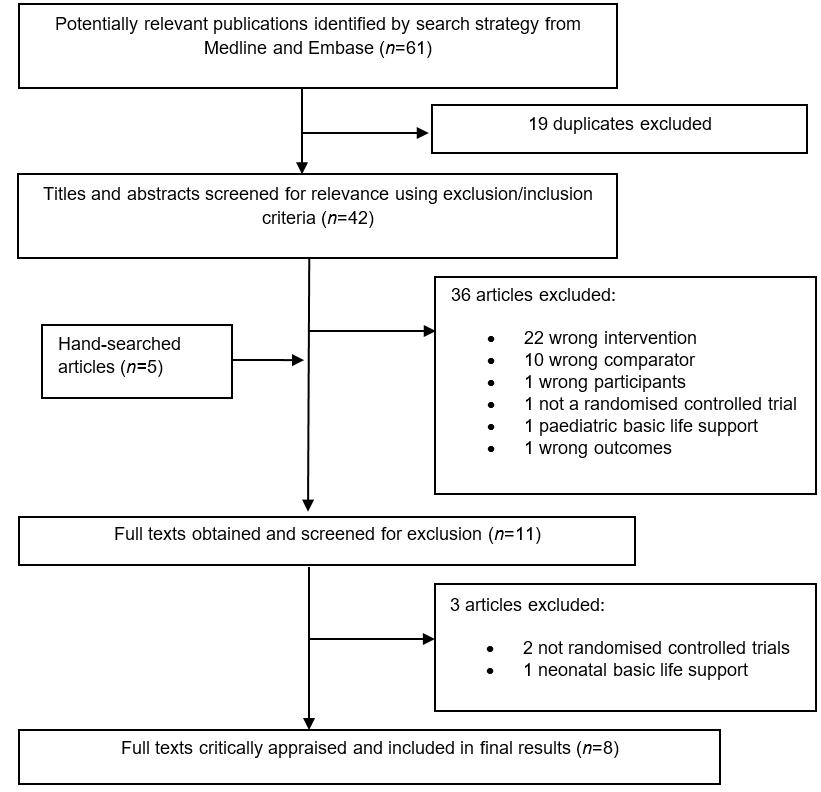 Figure 1: Database search strategy.
Figure 1: Database search strategy.
Population and demographics
Participant demographics are shown in Table 1. Combining all eight papers, the total study population before randomisation was 1910. However, 731 participants (38%) dropped out of the studies at various stages, leaving a final cohort of 1179 participants. Participant dropout varied from 0% to 72% amongst the different studies. Therefore, the risk of attrition bias within the entire population was deemed to be high.
Four studies reported mean age for both intervention and comparator groups16-19. Three studies20-22 did not report mean age, however both Mancini et al21 and Van Raemdonck et al22 did report age ranges, which were 25–65 years and 15–16 years, respectively. Einspruch et al20 did not provide demographic data as their study followed up previous research by Lynch et al23. However, because 63 participants dropped out between studies, it was deemed inappropriate to use the same demographic data for the Einspruch study in the review.
Within the studies that did provide gender demographics, distributions of females between intervention and comparator groups were similar16-18,21-23. Mancini et al21 could not fully report gender distributions within their population because 16% of individuals failed to share this information. Van Raemdonck et al22 excluded female participants because of wide variation within this group.
Todd et al noted that significantly more individuals in the comparator group had previous CPR training than in the intervention group17, creating potential bias against the intervention group. Three studies20,21,23 reported that participants had no CPR training within the previous 5 years; however, they did not give details about whether the participants had ever been given CPR training. Van Raemdonck et al did not assess previous CPR training in their population of school children aged 15–16 years22, but it may be less likely that they would have had prior CPR training due to their age.
Table 1: Descriptive statistics for the eight selected studies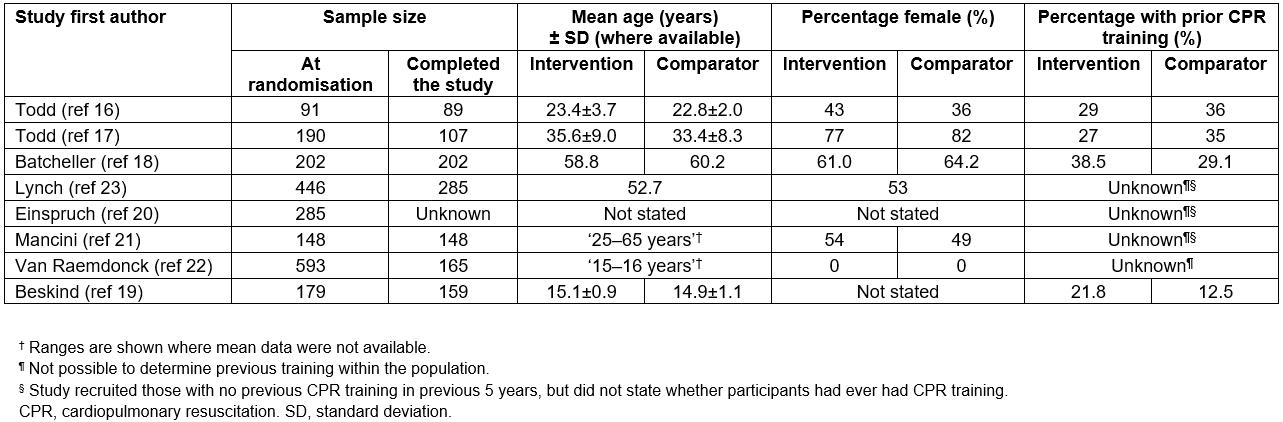
Intervention
There was variation between the studies of both video duration and the type of mannequins used (Table 2). Five out of eight studies used variations of video self-instructed (VSI) CPR training. Video duration varied between these studies, ranging from 22 minutes20,23 to 34 minutes16-18. Lynch et al23 and Einspruch et al20 used Mini Anne mannequins, differing from the Laerdal Family Trainer cardboard mannequins used by Todd16,17 and by Batcheller18. Mancini et al used Mini Anne mannequins but employed both online tutorials and a DVD-based, self-directed practical skills session21. Van Raemdonck et al22 and Beskind et al19 did not record which mannequins they used. Beskind et al varied from other studies in that they used chest compression only CPR training via a brief 90-second video with no skills practice19.
Table 2: Description of the eight selected studies (based on the PICO framework for this study)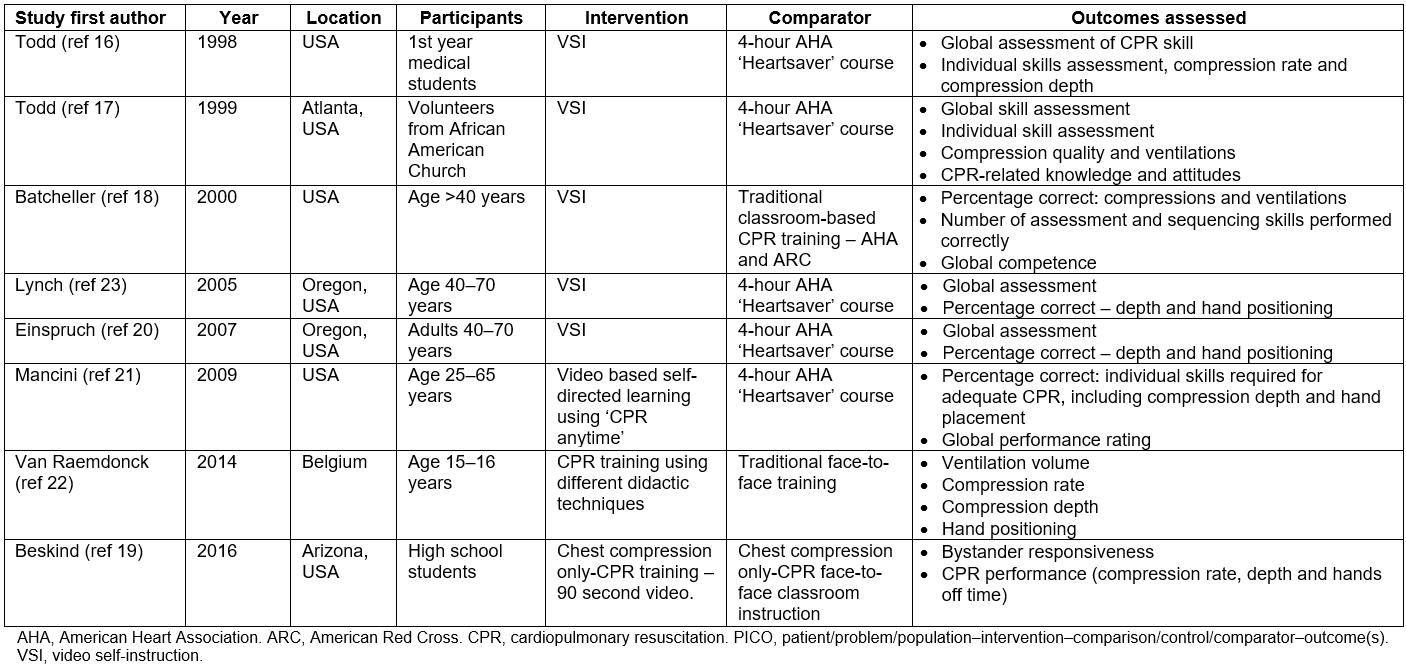
Comparator
All comparators were classroom-based training courses. Six of the courses used the 4–4.5 hour American Heart Association Heartsaver course as the standard classroom-based training (Table 2). Each of these courses used Resusci Anne mannequins for the practical skills aspect of the course. Van Raemdonck et al employed a teacher-led course; however, details of what this involved were not provided22. Unlike the other studies, Beskind et al provided a 20-minute chest compression only CPR session19.
Outcomes
As the studies differed significantly in their methods, pooling the data using meta-analysis was deemed inappropriate. However, general comparisons could be made between intervention and comparator groups. Outcome measures and the presence or absence of statistical differences between intervention and comparator groups are shown in Table 3.
Regarding percentage of participants with correct hand position, five studies demonstrated no significant differences between intervention and control groups (Table 3). Todd found that 55% of VSI trainees had correct hand position compared with 25% in the traditional trainee group (p<0.05)17, while Batcheller reported the largest difference between groups17, with 90.1% of the intervention group getting the correct hand position, compared to 35.8% in the comparator group (p<0.00001).
Four studies showed no difference in compression depth20-23. Lynch et al found 48% of those who were VSI trained achieved correct depth23, which was similar to the traditionally trained group, which scored 49%. Mancini et al21 recorded higher percentage correct scores, with 68±6% of video learners achieving the correct depth, compared with 80±4% for the traditional training, although this was not a statistically significant difference. In contrast, Beskind et al reported compression depth as metric data19, with video trainees achieving mean depths of 32.3 mm immediately post-intervention, and 31.1 mm when re-tested at 2 months. Mean depths for each group were shallower than European Resuscitation Council guideline recommendations24 of 5–6 cm. Similar issues were found with the study by Van Raemdonck et al where, although no significant difference existed between groups, neither group achieved adequate compression depths22.
Four studies assessed compression rate. Although Todd et al found no difference between groups for median compression rate (81 bpm v 79 bpm, respectively)16, both groups scored below the acceptable rates recommended by the European Resuscitation Council24. While Mancini et al reported a lower mean compression rate in their intervention group compared with their traditionally trained group (99±3 bpm compared with 108±2 bpm (p<0.05))21, Van Raemdonck et al22 and Beskind et al19 found no significant differences between rates in their intervention and comparator groups.
Table 3: Outcomes interpretation for the eight selected studies†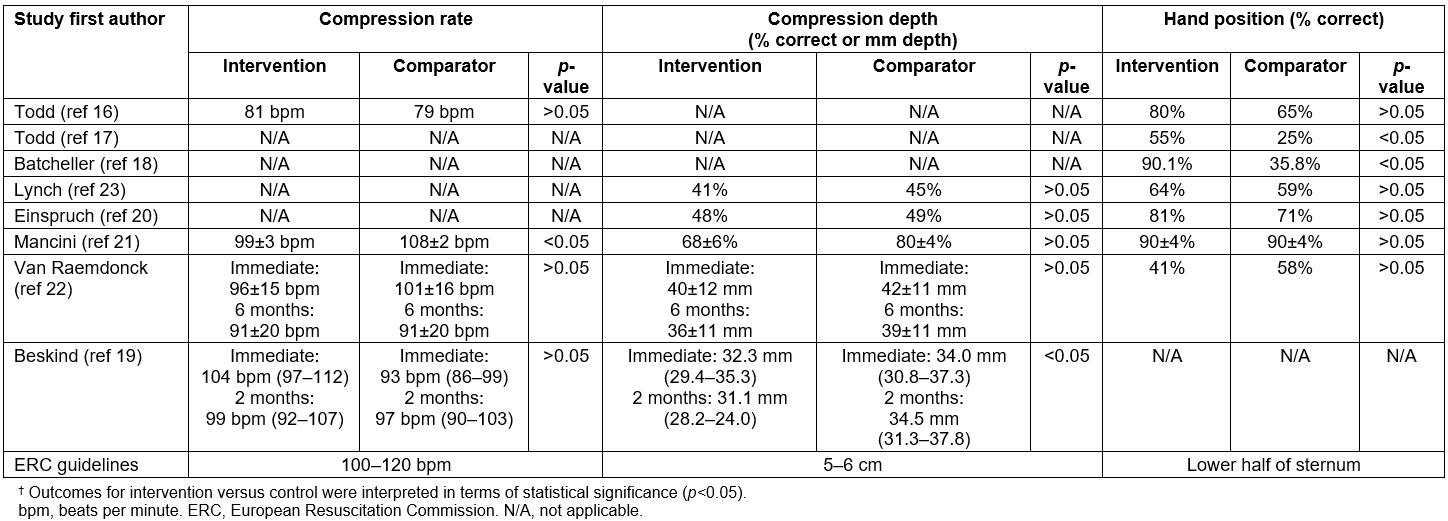
Bias assessment
Outcomes of study bias assessments are described in Table 4. Six studies did not clearly specify randomisation methods. Two studies16,17 used random number tables. Six of the studies did not clearly specify how the allocation of subjects was concealed. Todd et al16 concealed the type of training they would receive from the subjects and Todd et al gave study staff envelopes containing assignments at the time of enrolment17, meaning that there was a low risk of inadequate allocation concealment.
Six studies17-21,23 were assigned a high risk of performance bias due to the nature of the intervention – it was impossible to completely blind subjects to the CPR training delivered to them. Whereas Van Raemdonck et al22 failed to report blinding methods, making it difficult to determine bias risk, Todd et al were deemed to have the lowest risk of bias because assessors were blinded to subject assignments and were not involved in assigning subjects to groups16.
All studies measured the selected outcomes objectively using computer software linked to a mannequin, and were therefore at low risk of bias. Furthermore, Beskind et al19 was the only article that blinded the statistician, adding another level of protection against bias.
Three studies were deemed to be at high risk of attrition bias due to dropout rates of greater than 20%: Lynch et al23 reported 36% of their initial sample dropping out, while Todd et al17 and Van Raemdonck et al22 reported higher dropout rates of 44% and 72%, respectively. Van Raemdonck et al removed all female participants due to a high level of variance within the sample22. A further three studies did not give enough information to make an appropriate assessment of attrition.
Four studies were rated as having a high risk of reporting bias: Van Raemdonck et al22 removed all female participants and three other studies16,17,21 did not report all outcomes equally. Batcheller did not state a clear hypothesis18, making it difficult to ascertain if outcomes were being selectively reported.
Other potential sources of bias included the influence of previous CPR training on performance16,17, differences between types of classroom-based training used within comparator groups18, and different mannequins used for training and assessment18,21. Questions were also raised about the applicability of results seen in a medical student population to the wider population16.
Table 4: Bias assessment (conducted using the Cochrane Bias Assessment Tool15) for the eight selected studies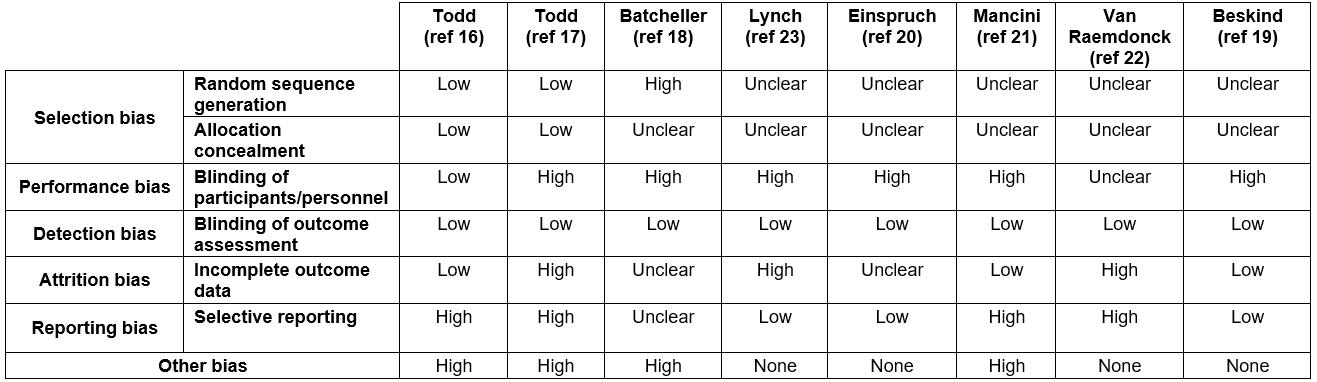
Discussion
This is the first systematic review of randomised controlled trials of non-classroom-based versus classroom-based CPR training for bystanders. Eight randomised controlled trials comparing non-classroom to classroom-based CPR training in bystanders were reviewed. Across these studies 13 out of a total of 15 outcomes showed non-classroom-based CPR training to be as effective or more effective than classroom-based CPR training. However, there was broad variation in how these outcomes were measured and the type of non-classroom and classroom-based CPR training used.
Outcome measurement
Seven studies used Laerdal reporting software (Laerdal Medical; https://www.laerdal.com/au/products/simulation-training/resuscitation-training) to measure compression depth, rate and hand position although the software and equipment to which they referred varied (‘Skillreporting’19,22,23, ‘Skillmeter’16-18 and ‘software programme’21). Einspruch et al20 did not identify what reporting software was used to measure outcomes. The studies were published at different times, and less accurate software may have been used in the older studies. However, the use of objective computer measurements to assess competency in these outcomes adds strength by both reducing risk of bias and improving accuracy.
Six of the seven studies that assessed hand position found that non-classroom-based training was equal to or more effective than classroom-based training16-18,20,21,23. Batcheller combined compression depth and position to give an overall percentage score for ‘compressions delivered correctly’18. As such, hand position was not individually assessed, although when analysed the intervention group was more effective than the comparator.
Only four of the studies measured compression rate16,19,21,22, despite demonstration of this outcome as crucial to survival10. Three non-classroom-based training groups16,19,22 performed as well as the classroom-based groups whereas the groups of Mancini et al demonstrated poorer performance21.
Five studies reported compression depth. Four studies20-23 found the non-classroom-based training group as effective as the classroom-based group, and one found them less effective19. Batcheller measured ‘compressions delivered correctly’18 and as such compression depth was not individually assessed.
During testing, a variety of guidelines were used as a benchmark for determining target outcomes, thus comparison should be conducted with caution. Five studies used American Heart Association16-18,21 or previous European Resuscitation Council22 guidelines, while Einspruch et al20, Lynch et al23 and Beskind et al19 did not specify which guidelines were used. This meant that what was considered to be the correct range for compression depth, compression rate and hand position was not universal for all the studies. For example, Mancini et al21 recorded a wider range of chest compression depths as correct than Van Raemdonck et al22.
Study design
Whilst all studies were required to involve CPR training on mannequins, the type of mannequins used varied. Some studies used a cheaper, lightweight mannequin for the non-classroom-based training group16,18,21. Whilst this can be regarded as part of the ‘distance training’ intervention, it is important to note that effects are likely to be due not only to video training, but also to differences in mannequins.
Although the present study’s methodology was designed to encompass all forms of non-classroom-based CPR training, many studies specifically used video-training while only one used an interactive DVD21. Amongst the video-training interventions, there were disparities in the duration of the videos as well as variety in time allowance for hands-on practice. This made it difficult to reliably compare the studies, although they could still provide insight into what constitutes an optimum video training program.
Beskind et al were specifically interested in determining whether brevity of training affected CPR outcomes19, the intervention group being provided with a 1.5-minute instruction video but given no time for hands-on practice. This group performed poorly on compression depth, which may be attributed to lack of psychomotor training – practice time was restricted in the Van Raemdonck study and participants again performed poorly on compression depth22.
Intervention groups whose videos had either been specifically designed to provide comprehensive CPR information18 or who allowed for unlimited practice time on the mannequin20,23 performed compression depth comparable to those who were classroom trained. Whilst the length of time participants chose to practise for throughout their training may have varied, this suggests that having more time to practise is of benefit and should be encouraged. The impact of practising whilst simultaneously receiving instruction16,17,20,23 may also have influenced outcome to some extent, and may be a future direction for research.
Non-classroom-based training methods that involved face-to-face training with an instructor were excluded from the study as this would have constituted a classroom-based approach. Although two studies did include elements of non-video instruction, in the form of peer-to-peer discussion analysis23 and a plenary feedback session22, they were deemed appropriate for inclusion. All study participants took part in the plenary session regardless of study arm assignment, thus removing risk of bias from the outcomes, and the peer-to-peer feedback did not conflict with the concept of a non-classroom-based training program.
Bias
Of the eight papers reviewed, all were deemed at high risk of at least one type of bias. Except for both studies by Todd et al16,17 none gave adequate information regarding randomisation and allocation of subjects, and were all therefore at risk of allocation bias. Due to the nature of these studies it was difficult to blind participants to study group. However, bias could have been reduced by limiting participants’ knowledge of the study as far as possible. Todd et al strove to do this by blinding subjects to the study question and the different training being given16.
For all studies, the outcomes were recorded directly from electronic mannequins so risk of detection bias was low. Although an external assessor was often present, the mannequins measured all the specified outcomes so it is unlikely that this had any bearing on the studies.
Both Lynch et al23 and Van Raemdonck et al22 had a high risk of attrition bias due to high dropout rates. Van Raemdonck et al risked further bias because all females were removed from the final analysis because results showed too much variance, without good justification22. Einspruch et al20, a follow-on study from Lynch et al23, had an acceptable dropout rate of <20%; however, the study began with 63 fewer participants than were reported to have completed the study by Lynch et al, with no explanation given.
Poor reporting was not only a problem in the methodologies when describing randomisation, but also when presenting results of outcomes set out to be measured. Todd et al were deemed to be at high risk of reporting bias, as stated outcomes were reported incompletely17, whereas Mancini et al lent more weight to their subjective questionnaire than to the objective outcomes extracted by this review, giving more positive conclusions than the objective results might suggest21.
Limitations of methodology
Useful research may have been excluded because of the present study’s strict exclusion criteria. Although the study research question aimed to evaluate non-classroom-based CPR training to laypersons, only trials comparing video training to classroom-based training were found. Broadening the inclusion criteria to include non-randomised controlled trial studies might allow other relevant studies with other training methods to be analysed. Furthermore, a more extensive literature search might find a greater variety of studies that could be included.
Conclusion
On the basis of research so far, there is generally no difference between the efficacy of teaching bystanders CPR through non-classroom-based training and classroom-based methods; however, limitations in the included studies means it is difficult to come to a definitive conclusion at this stage. Conclusions are limited to the objectively measured outcomes of quality of chest compression rate, chest compression depth and hand positioning, but there may have been improvements or decline in other aspects of CPR quality that were not recorded. No randomised controlled trials met this review’s inclusion criteria on other types of non-classroom training, such as through mobile phone applications or interactive video games, so further research into these could be of value. CPR is a critical link in the chain of survival and can be performed by almost anyone. However, as these reported studies show, even after training, efficacy was often suboptimal in both groups when compared to ERC guidelines. It is clear that there is still room for improvement in delivering effective CPR training. This review suggests that a program of video training merits further study and perhaps widespread implementation. This could help further the Scottish Government’s plan to improve OHCA survival rates, especially in rural areas.

